Dear Editor,
The ongoing emergency due to the widespread of a novel coronavirus called SARS‐CoV‐2 (severe acute respiratory syndrome coronavirus 2) causing a severe acute respiratory syndrome 1 forced a strong reduction of people's mobility since March 8 in the Veneto region of Italy, one of the most affected area after Lombardy. 2 Due to the rapid increase of contagions, the government also decided to restrict access to hospitals, limited to urgency‐only outpatient visits.
Such restrictions motivated us to find alternative ways to follow‐up our patients. During those weeks, we performed telephone calls to our scheduled patients with chronic conditions such as autoimmune blistering diseases, psoriasis and psoriatic arthritis, cutaneous lupus erythematous, scleroderma and other dermatological diseases in order to modulate their treatment on the basis of blood examinations and reported cutaneous conditions.
We also provided a direct telephone line for teledermatology for the exclusive use of general practitioners (GPs) and pediatricians. Since March 25, every day at scheduled time, including Sundays, a dermatologist of our department answered to all GPs' and pediatricians' calls of Treviso district (about 885 000 inhabitants, density 358 inhabitants/km2). 3 GPs and pediatricians were asked to send pictures of dermatological features of their patients by email and they received a formal answer with recommendations. After 2 weeks, to date, we received 32 calls: 26 from GPs and six from pediatricians (Figure 1). The dermatological conditions reported ranged from Gianotti‐Crosti syndrome, to bullous pemphigoid, burns, tinea corporis, psoriasis, eczema, intertrigo, photodermatitis, pityriasis rosea, pyogenic granuloma, site‐injection reaction to adalimumab and more (Figure 2). In 27 out of 32 teledermatology consultations, diagnosis and therapeutic indications could be provided and patients did not need to come to the hospital for an outpatient visit. Only in five cases, regarding mainly pigmented lesions and single nodular lesions, GPs were asked to refer patients because a proper diagnosis could not be made by pictures and reported history.
FIGURE 1.
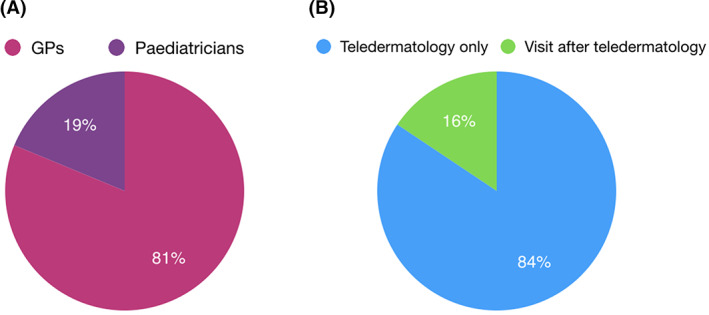
A, Percentage of patients referred by general practitioners and pediatricians. B, Percentage of typologies of visits
FIGURE 2.
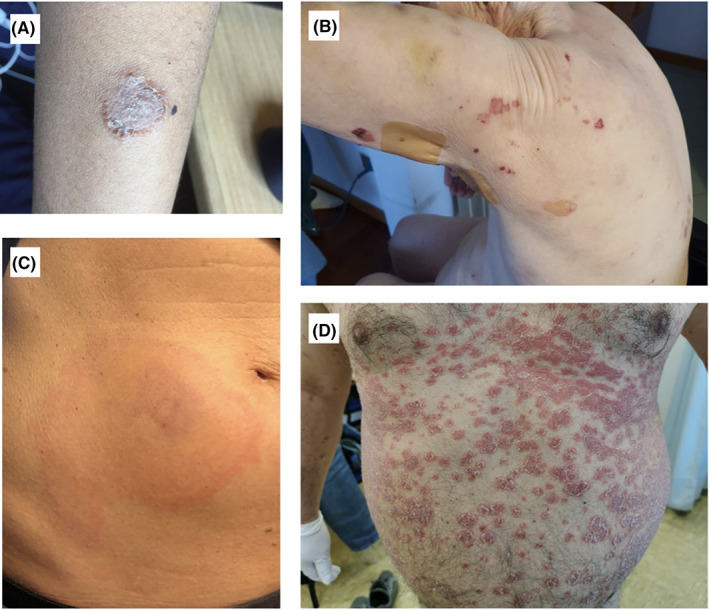
Examples of pictures received. A, Tinea corporis in a 12‐year‐old boy. B, Bullous pemphigoid in a 90‐year‐old woman. C, Reaction after adalimumab injection. D, Psoriasis
The aim of teledermatology is to provide diagnosis, treatment, follow‐up and education using communication technologies instead of a face‐to‐face visit. 4 Usually, teledermatology implies a direct communication between the patient and the dermatologist (primary teledermatology). 5 In such an emergency condition, we decided to apply primary teledermatology only to well‐known patients for follow‐up, whether we preferred implementing secondary teledermatology (communications between patients and dermatologists with the intermediation of GPs or pediatricians) for new consultations.
We found that secondary teledermatology was an immediate and easy access tool, helped patients avoiding useless movements and reduced the risk of contagion. For the elderly, it also provided an economic benefit in terms of national health system organization sparing unnecessary ambulance trips from home to hospital. Teledermatology contributed to create a network among dermatologists and GPs/pediatricians making a common practice of sharing pictures official, and it also helped GPs/pediatricians feeling connected to the central hospital in such an emergency situation.
Otherwise, the quality of the pictures sent was usually low and needs to be standardized. Dermatological diagnosis according to few photographs was challenging, lacking a proper physical examination: diagnosis is usually made by the use of five senses. Finally, GPs and pediatricians are not familiar with dermoscopy: every pigmented and nonpigmented lesion must be referred to a dermatologist in order not to miss a melanoma diagnosis. Teledermatology does not allow dermatologists to perform second‐level investigations (eg, swabs, biopsy and videodermoscopy) during the visit that can end in a diagnostic delay.
Data gathered during such a short period of time need to be expanded, although what we have experienced in a global emergency setting can possibly become a routine habit during ordinary work.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
REFERENCES
- 1. Park M, Cook AR, Lim JT, Sun Y, Dickens BL. A systematic review of COVID‐19 epidemiology based on current evidence. J Clin Med. 2020;9:967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gazzetta Ufficiale Della Repubblica Italiana Serie generale ‐ n. 59 8‐3‐2020.
- 3. https://www.istat.it/en/permanent-censuses/population-and-housing
- 4. Coates SJ, Kvedar J, Granstein RD. Teledermatology: from historical perspective to emerging techniques of the modern era: part I: history, rationale, and current practice. J Am Acad Dermatol. 2015;72:563‐567. [DOI] [PubMed] [Google Scholar]
- 5. Pasquali P, Sonthalia S, Moreno‐Ramirez D, et al. Teledermatology and its current perspective. Indian Dermatol Online J. 2020;11:12‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]


