Abstract
Objectives
The purpose of this article was to determine the change in the volume of pacemaker implantations with the COVID‐2019 pandemic and to assess the change in the number of pacemaker implants according to etiology during the pandemic.
Background
The establishment of a mandatory social isolation have generated a decrease in activities in cardiology units.
Methods
Descriptive, cross‐sectional study that used a database of a Peruvian Hospital. Time was divided into three categories: Before COVID period and COVID period including Previous to Social isolation (SI) and Social Isolation. The number of pacemaker implantations were compared per the same amount of time.
Results
A reduction in the pacemaker implant of 73% (95% CI: 33‐113; P < .001) was observed during the COVID‐19 pandemic period, and a reduction of 78% of patients with the diagnosis of complete or high‐grade atrioventricular block and a reduction in the de‐novo pacemaker implant was observed, regardless of the etiology.
Conclusions
Our results indicate a very significant reduction (73%) in de‐novo pacemaker implantation during the months of the COVID‐19 pandemic. The reduction in the number of de‐novo pacemaker occurred independent of the etiology.
Keywords: atrioventricular block, COVID‐19, pacemaker
This article reports the reduction of de‐novo pacemaker implants in a Peruvian hospital due to the COVID‐19 pandemic. The reduction in the number of de‐novo pacemaker occurred independently of the etiology.
1. INTRODUCTION
Since the appearance of the new SARS‐CoV‐2 coronavirus (severe acute respiratory syndrome coronavirus 2) in December 2019, in Wuhan, China; patients were admitted with symptoms of pneumonia, named coronavirus disease 2019 (COVID‐19); the virus spread, affecting different provinces in China and, after a few months, it is now present in more than 150 countries around the world. World Health Organization (WHO) has declared the novel coronavirus (COVID‐19) outbreak a global pandemic on March 11, 2020. 1
In Peru the first case was diagnosed on March 6th and from March 16th the government established a mandatory social isolation to prevent the COVID from further spreading in the country.
COVID‐19 has impacted and determined substantial changes in health systems in all countries; emergency, intensive, or intermediate care units carry the greatest burden, but several hospital wards have also been converted to COVID units, to face the growing wave of the disease. Many units of the different services, including cardiology, have redistributed their spaces and personnel dedicating them to become COVID‐19 units.
The resource allocation and priority setting measures, such as redirecting the personal protective equipment and hospital beds for patients with COVID‐19 and the delay of elective cardiac procedures, 2 as recommended by the Centers for Disease Control and Prevention as well as the guidelines from the Electrophysiology section of the American College of Cardiology and the Arrhythmia Committee of the American Heart Association, 3 were implemented in Peru.
Electrophysiology units are not exempt from these changes; therefore, the impact of the COVID‐19 pandemic on the implantation of cardiac pacing devices such as pacemakers was investigated.
2. METHODS
Cross‐sectional descriptive study used the pacemaker implant database of the Department of Cardiology of the Edgardo Rebagliati Martins National Hospital (HNERM), the national reference hospital, the largest in the country, where an average of 600 procedures are performed per year including de‐novo pacemaker implants and pacemaker replacements. The hospital has two emergencies, one of which was dedicated to receiving COVID patients and the other to non‐COVID patients. The admission of any patient has not been restricted.
In the present study, we only considered de‐novo pacemaker implants (DNPI) performed from January 2017 to April 30, 2020, generator replacements were excluded from the analysis as they are generally elective procedures; The data of the de‐novo pacemakers implanted between January 1st to April 30th from 2017 to 2020 were used and compared with each other. Likewise, the average number of DNPI in the last 12 months prior to the start of the COVID‐19 pandemic in Peru was calculated and compared with the average number of DNPI in the COVID‐19 pandemic in Peru.
Until the time of the present study, the HNERM was not designated as an exclusive Hospital for the care of COVID‐19 patients, so it continued admitting patients with any pathology; in the cardiology area, electrophysiologists continued to be programmed for the emergency pacemaker implant. All the patients admitted with a pacemaker indication underwent the respective implant. The number of DNPI was described according to etiology.
The objectives of the study were: (a) to determine the change in the volume of pacemaker first implants during the pandemic, (b) to assess the change in the number of pacemaker implants according to etiology during the pandemic.
For the purposes of this study, time has been divided into two periods: "before COVID" (BC) and "COVID". The BC period is comprised of the 14 months prior to the pandemic in Peru (from January 1st, 2019 to February 29th, 2020); March 6th, 2020, was identified as the beginning of the COVID period, the date on which the first COVID‐19 case was reported in Peru and substantial changes began in the health system, until April 30, 2020 (date the study ended). In addition, the COVID period was subdivided into: “presocial isolation” period (COVID‐preSI, from March 6th to March 15th) and “social isolation” period (COVID‐SI, from March 16th to 30th April). We compared the total number of DNPI and the number of pacemaker implants according to etiology in the last 4 years, considering the same time interval.
We compare the monthly total of DNPIs from January 2019 to April 2020. We also compare the average DNPI per month between BC and COVID periods. The “t‐student” test was used to estimate the change in the average DNPI between both periods.
3. RESULTS
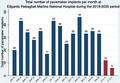
The total number of pacemaker implants per month in Rebagliati hospital was lower in March and April 2020 compared to the months prior to the start of the COVID‐19 pandemic (Figure 1).
FIGURE 1.
Total number of pacemaker implants per month at Edgardo Rebagliati Martins National Hospital during the 2019‐2020 period. Absolute number of de‐novo pacemaker implantation. The total number of monthly implants is reduced in the months during the COVID 19 pandemic (red)
An average of 33.1 pacemakers per month were implanted per month in the BC period; in contrast, only nine pacemakers per month were implanted on average in the COVID period. A reduction in the pacemaker implant of 73% (95% CI: 33‐113; P < .001) was observed during the COVID‐19 pandemic period.
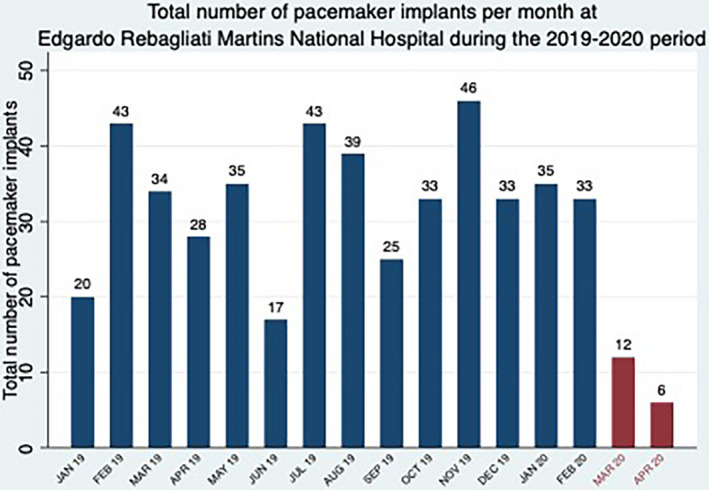
On the other hand, when comparing the number of implants after the start of the period of social isolation with the number of implants in the previous 3 years, in the same period of time, a significant reduction of 82% was evident. However, there was no evidence of variation in the pre‐social isolation period of COVID compared to previous years, in the same time periods (Figure 2).
FIGURE 2.
Number of de‐novo pacemaker implants per the same amount of time in the last 4 years. *Previous to social isolation period. **Social isolation period
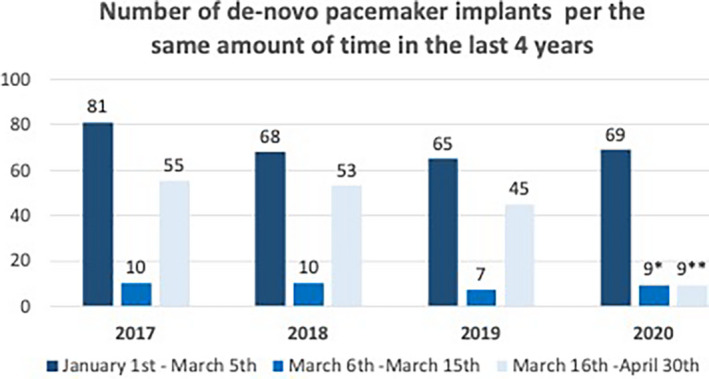
When evaluating the DNPI, a reduction in their number was observed, regardless of the etiology (complete atrioventricular block high grade block, atrial fibrillation or atrial flutter with atrioventricular node disease, sinus node dysfunction), in the period of social isolation (Figure 3).
FIGURE 3.
De‐novo pacemaker implants according to etiology. Complete AV block: complete atrioventricular blocks, AFib: atrial fibrillation, Aflutter: atrial flutter
Most of the complete atrioventricular blocks (AVB) or high‐grade blocks are emergencies and, depending on the escape rhythm, are symptomatic and require a short pacemaker implantation. It was observed that during the period of social isolation the number of cases of DNPI for complete AVB and high‐grade blocks has also decreased significantly compared to the BC period, as well as in relation to previous years in the same period, with a 78% reduction on average compared to previous years (Figure 3).
4. DISCUSSION
The present study was carried out at HNERM, which is the hospital center that performs the largest number of pacemaker implants per year (de novo pacemaker implant and replacement).
In the present investigation we observe a great reduction in the number of pacemaker procedures and implants during the months of the COVID‐19 pandemic in Peru, especially during the period of social isolation decreed by the Peruvian state, this finding is similar to the Reduction in ST‐Segment Elevation Cardiac Catheterization Laboratory Activations. 4 It is evident that the decrease occurs in all the etiologies for the indication of DNPI.
And if we consider the number of pacemaker implants for complete or high‐grade atrial ventricular block, which are usually the most symptomatic patients, it has also decreased.
We hypothesized that the decrease in the number of DNPI is because of multiple factors, such as the fear of getting COVID because of going to the hospital, a hypothesis suggested by us and other authors previously, both in cardiovascular pathologies 5 , 6 , 7 and other disciplines. 8 , 9 , 10 , 11 The fear of infection has already been reported in a study of psychological responses to emerging outbreaks of infectious diseases. 12
We consider as possible causes of this decrease, the difficulty in getting around that limits timely access to the hospital. Another question asked is whether, in addition, patients underestimate their symptoms and prefer to stay home. 5 , 6 , 10 All of the above can have a deleterious impact on the health of the population, with an increase in morbidity and mortality, not only today, but also in the coming months.
The findings found are an early sign of an impending problem, which we must be prepared for. We must start educating patients with a cardiac pathology to go to cardiology services in the event of the onset or worsening of the disease or use digital means for remote orientation, remote monitoring, among other tools, and thus avoid fatal outcomes.
On the other hand, strategies must be developed on the management of patients with cardiac pathology during admission to medical units or emergencies. In this context, these units must be implemented with full biosafety protection for health professionals, patients, family members and companions, as well as considering the isolation of patients who require DNPI and are diagnosed with COVID‐19 infection, previous reports have explained how to implement these strategies as well. 3
In general terms, the cause of the reduction in the number of DNPI is considered to be multifactorial; the Figure 3 showed a marked decreased in peacemaker implants in the isolation period, and as the emergency room was open to any patients 24/7, the attendance of patients to the emergency probably was affected by the decision of the patients, so it is believed that what determines the patient not to go to the emergency would be the fear of getting COVID. Even so, this fear can be controlled to avoid fatal cardiovascular outcomes.
5. CONCLUSIONS
Our results indicate a very significant reduction (73%) in de‐novo pacemaker implantation during the months of the COVID‐19 pandemic. The reduction in the number of de‐novo pacemaker occurred independently of the etiology.
5.1. Limitations
A single hospital center in Peru was considered; although it is true that a single center experience may not represent the entire national situation, this hospital has the peculiarity of receiving patients from all over the country and being the one that implants the largest number of pacemakers per year.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest and have not received a financial grant to carry out this study.
Gonzales‐Luna AC, Torres‐Valencia JO, Alarcón‐Santos JE, Segura‐Saldaña PA. Impact of COVID‐19 on pacemaker implant. J Arrhythmia. 2020;36:845–848. 10.1002/joa3.12411
REFERENCES
- 1. Sahu K, Mishra A, Lal A. Comprehensive update on current outbreak of novel coronavirus infection (2019‐nCoV). Ann Transl Med. 2020;8(6):393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. CDC . Healthcare Facilities: Preparing for Community Transmission [Internet]. 2020. https://www.cdc.gov/coronavirus/2019‐ncov/hcp/guidance‐hcf.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019‐ncov%2Fhealthcare‐facilities%2Fguidance‐hcf.html
- 3. Lakkireddy DR, Chung MK, Gopinathannair R, Patton KK, Gluckman TJ, Turagam M, et al. Guidance for cardiac electrophysiology during the COVID‐19 pandemic from the heart rhythm society COVID‐19 task force; Electrophysiology section of the american college of cardiology; and the electrocardiography and arrhythmias committee of the council on clinical cardiology, American heart association. Heart Rhythm. 2020; 10.1016/j.hrthm.2020.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Garcia S, Albaghdadi M, Meraj P, Schmidt C, Garberich R, Jaffer F, et al. Reduction in ST‐segment elevation cardiac catheterization laboratory activations in the United States during COVID‐19 pandemic. J Am Coll Cardiol. 2020;75(22):2871–2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zaleski AL, Taylor BA, McKay RG, Thompson PD. Declines in acute cardiovascular emergencies during the COVID‐19 pandemic. The American Journal of Cardiology. 2020; 10.1016/j.amjcard.2020.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. De Rosa S, Spaccarotella C, Basso C, Calabrò M, Curcio A, Filardi P, et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID‐19 era. Eur Heart J. 2020;41(22):2083–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Masroor S. Collateral damage of COVID‐19 pandemic: delayed medical care. J Card Surg. 2020;35(6):1345–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kansagra AP, Goyal MS, Hamilton S, Albers GW. Collateral effect of covid‐19 on stroke evaluation in the United States. New England Journal of Medicine. 2020; 10.1056/nejmc2014816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tartara F, Cofano F, Zenga F, Boeris D, Garbossa D, Cenzato M. Are we forgetting non‐COVID‐19‐related diseases during lockdown? Acta Neurochir (Wien). 2020;162(7):1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Enache B, Claessens Y‐E, Boulay F, Dor V, Eker A, Civaia F, et al. Reduction in cardiovascular emergency admissions in Monaco during the COVID‐19 pandemic. Clinical Research in Cardiology. 2020; 10.1007/s00392-020-01687-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Feral‐Pierssens A‐L, Claret P‐G, Chouihed T. Collateral damage of the COVID‐19 outbreak: expression of concern. Eur J Emerg Med. 2020;27(4):233–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chew Q, Wei K, Vasoo S, Chua H, Sim K. Narrative synthesis of psychological and coping responses towards emerging infectious disease outbreaks in the general population: practical considerations for the COVID‐19 pandemic. Singapore Med J. 2020;51:1–31. [DOI] [PMC free article] [PubMed] [Google Scholar]


