Abstract
Glycoproteins of enveloped viruses replicating in nonprimate mammalian cells carry α‐1,3‐galactose (α‐Gal) glycans, and can bind to anti‐Gal antibodies which are abundant in humans. The antibodies have protected humans and their ancestors for millions of years, because they inhibit replication of many kinds of microbes carrying αGal glycans and aid complements and macrophages to destroy them. Therefore, severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) replicating in nonprimate mammalian cells (eg, PK‐15 cells) carry αGal glycans and could be employed as a live vaccine for corona virus 2019 (COVID‐19). The live vaccine safety could be further enhanced through intramuscular inoculation to bypass the fragile lungs, like the live unattenuated adenovirus vaccine safely used in US recruits for decades. Moreover, the immune complexes of SARS‐CoV‐2 and anti‐Gal antibodies could enhance the efficacy of COVID‐19 vaccines, live or inactivated, carrying α‐Gal glycans. Experiments are imperatively desired to examine these novel vaccine strategies which probably have the critical advantages for defeating the pandemic of COVID‐19 and preventing other viral infectious diseases.
Keywords: anti‐Gal antibodies, COVID‐19, immune complex, SARS‐CoV‐2, vaccine
Research Highlights
Severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) replicating in nonprimate mammalian cells carries α‐1,3‐galactose (α‐Gal) glycans which can bind to anti‐Gal antibodies abundant in humans.
Anti‐Gal antibodies inhibit replication of various α‐Gal‐carrying pathogens and aid complements and macrophages to destroy them.
α‐Gal‐carrying SARS‐CoV‐2 could be used as a live vaccine for corona virus 2019 (COVID‐19).
The live vaccine safety could be enhanced through intramuscular inoculation to bypass the fragile lungs.
Live and inactivated COVID‐19 vaccines could be more effective if produced using PK‐15 rather than Vero cells.
1. BACKGROUND
Corona virus 2019 (COVID‐19) caused by the novel coronavirus severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) was first identified in December 2019 in Wuhan, China, and has resulted in an ongoing pandemic. As of 13 July 2020, over 12.9 million cases have been reported across 188 countries and territories, resulting in over 560 000 deaths. 1 , 2 So far, particularly effective antiviral agents against COVID‐19 have not been identified. 3 It is thus imperatively desired to develop safe and effective vaccines for the disease, and accordingly, various vaccines for COVID‐19 have been under development with unprecedented rapidity. 4 , 5 , 6 , 7 , 8 , 9 These vaccines can be largely divided into whole‐virus vaccines and subunit vaccines. 4 , 5 , 6 , 7 , 8 , 9 Whole‐virus vaccines include live vaccines and inactivated vaccines, and subunit vaccines are those based on proteins, DNA, messenger RNA, or viral vectors.
Through decades of competition, live vaccines, inactivated vaccines, and subunit vaccines are employed for prevention of 13, 6, and 4 human viral infectious diseases, respectively (Table 1). 10 Therefore, it is of great significance to develop whole‐virus vaccines, particularly live vaccines which are usually more efficacious and less costly than other vaccines, for COVID‐19. 11 Currently, several inactivated vaccines for COVID‐19 have entered clinical trials, 8 , 9 but progress of live vaccine development for COVID‐19 has yet to be reported.
Table 1.
Types of vaccines currently used for human viral diseases
| Vaccines | Diseases prevented by the vaccines |
|---|---|
| Live vaccines | Adenovirus‐associated respiratory disease (only used in US recruits), dengue, hepatitis A, influenza, Japanese encephalitis, measles, mumps, poliomyelitis, rabies, rotavirus‐associated diarrhea, rubella, Shingles, varicella, yellow fever |
| Inactivated vaccines | Hepatitis A, influenza, Japanese encephalitis, rabies, poliomyelitis, tick‐borne encephalitis, hand foot mouth disease |
| Subunit vaccines | Viral vector‐based: dengue; protein‐based: hepatitis B, hepatitis E, HPV infection |
The inactivated vaccines for COVID‐19 currently under development are produced using Vero cells. 8 , 9 It has been found that SARS‐CoV‐2 replicates in PK‐15 cells as efficiently as in Vero cells, and can reach to the titer of 1011 PFU/mL. 12 As elucidated below, SARS‐CoV‐2 replicating in nonprimate mammalian cells, including porcine PK‐15 cells, probably has critical advantages for inactivated and live vaccines for COVID‐19, due to interaction of the glycans of α‐1,3‐galactose (Galα1‐3Galβ1‐4GlcNAc‐R, αGal) and anti‐Gal antibodies.
2. α‐GAL GLYCANS (GAL‐GS) ON VIRUSES
Glycans at the N‐linked glycosylation sites on enveloped viruses including coronaviruses are synthesized by the relevant cellular enzymes in host cells. 13 , 14 , 15 , 16 , 17 , 18 Accordingly, enveloped viruses, such as influenza virus, vesicular stomatitis virus (VSV), eastern‐equine‐encephalitis virus (EEEV), replicating in cells of nonprimate mammals, lemurs, or New‐World monkeys, including murine 3T3 fibroblasts, canine MDCK, and porcine PK‐15, carry Gal‐Gs, because these cells express active α‐1,3‐galactosyltransferase (α‐1,3‐GT). 13 , 14 , 15 , 16 , 17 , 18 These cells also decorate their surface glycoprotein and glycolipids with many Gal‐Gs synthesized within the cells. In contrast, enveloped viruses replicating in cells of humans, apes, Old‐World monkeys, including human Hela cells and African green monkey Vero cells, lack Gal‐Gs, because nucleotide mutations inactivated the enzyme α1,3GT in these cells. 13 , 14 , 15 , 16 , 17 , 18 The surfaces of these cells also lack Gal‐Gs. Many bacteria (eg, Serratia marcescens) and protozoa (eg, Trypanosoma cruzi) synthesize and present Gal‐Gs on the glycoproteins and glycolipids. 13 , 18 , 19
3. ANTI‐GAL ANTIBODIES (ANTI‐GAL‐ABS)
Nonprimate mammals, lemurs, or New‐World monkeys do not produce anti‐Gal‐Abs due to immune tolerance to self‐antigens. 14 In contrast, humans, apes, and Old‐World monkeys produce anti‐Gal‐Abs throughout life because of frequent antigenic stimulation by many gastrointestinal bacteria carrying Gal‐Gs. 19 Anti‐Gal‐Abs are abundant in humans, constituting ~1% of serum IgG, IgM, and IgA immunoglobulins. 18 , 20 Anti‐Gal‐Abs also exist as IgA and IgG in milk, colostrum, saliva, and bile. 20
Beyond anti‐Gal‐Abs specifically binding to Gal‐Gs, there are other natural anti‐glycan antibodies in human serum which bind to over 100 types of glycans, including anti‐A and anti‐B antibodies produced against blood‐groups A and B glycans in the ABO system. 21 The natural anti‐glycan antibodies of anti‐A and anti‐B are produced due to stimulation of gastrointestinal bacteria carrying blood‐groups A or B antigen. 13 , 22 It remains unknown whether anti‐A and/or anti‐B antibodies are responsible for the observations that blood group O humans are probably less susceptible to COVID‐19 and group A humans are probably the most susceptible to COVID‐19. 23 , 24 , 25
Anti‐Gal‐Abs induce immune rejection of xenografts (eg, porcine organs) carrying Gal‐Gs transplanted into humans. 13 , 26 However, their major contribution to humans is to help the immune system to eliminate many kinds of zoonotic viruses carrying Gal‐Gs synthesized by the source animals, and fight bacteria and protozoa carrying Gal‐Gs. 13 , 14 , 15 , 16 , 17 , 18 In terms of evolution and immunology, anti‐Gal‐Abs have contributed greatly to protection of humans and their ancestors from infectious diseases for millions of years. 13 , 27 The protection of anti‐Gal‐Abs against viruses is based on the following three mechanisms:
First, anti‐Gal‐Abs can prevent the virus from attaching to the viral receptors, and thus block the entry and replication of the virus. 13 , 23 , 28 This is because when anti‐Gal‐Abs bind to Gal‐Gs on the viral surface glycoproteins, the binding can present a spatial obstacle to prevent the virus from attaching to the viral receptors on host cells. In‐vitro incubation of EEEV carrying Gal‐Gs with purified human anti‐Gal‐Abs blocked the replication of ∼50% of the virions in Vero cells, whereas such inhibition was not detected with EEEV lacking Gal‐Gs. 13 , 17 It is noteworthy that anti‐Gal‐Abs may be unable to neutralize or block all virions carrying Gal‐Gs. 13 , 17
Second, the immune complexes of anti‐Gal‐Abs and Gal‐Gs on a virus can target the virus to the complement system and activate the system to destroy the virus. 13 , 29 , 30 , 31 , 32 , 33 Through this complement‐mediated mechanism, anti‐Gal‐Abs have been found to be able to facilitate destruction of Gal‐Gs presenting lymphocytic choriomeningitis virus, measles virus, Newcastle disease virus, porcine endogenous retrovirus, pseudorabies virus, Sindbis virus, Type C retrovirus, vaccinia virus, and VSV. 13 , 29 , 30 , 31 , 32 , 33 An in‐vitro study showed that anti‐Gal‐Abs enhanced complement‐mediated killing of measles virus by over three folds compared with killing of the virus lacking Gal‐Gs. 31 Another in‐vitro study showed that anti‐Gal‐Abs could enhance complement‐mediated killing of VSV over 10‐fold compared with killing of the virus lacking Gal‐Gs, and over 99.99% VSV virions could be destroyed through this approach. 16
Third, anti‐Gal‐Abs can target a Gal‐Gs‐carrying virus to macrophages and other antigen presenting cells (APCs), through the interaction of their Fc tails and the Fc receptors on APCs, and aid these immune cells to destroy the virus and present relevant antigenic epitopes to T and B cells. 13 , 34 , 35 , 36 , 37 This process is termed immune opsonization which reduces the virus pathogenesis and induces higher protective immunity as compared with the virus alone (ie, lacking a‐gal epitopes). Mice in which the α1,3GT gene was knockout (GT‐KO mice) and which produce anti‐Gal‐Abs have been used for investigation of the effect of anti‐Gal‐Abs. 35 , 36 , 37 Compared with GT‐KO mice immunized with inactivated influenza virus lacking Gal‐Gs, GT‐KO mice immunized with inactivated influenza virus carrying Gal‐Gs produced anti‐influenza virus antibodies ~100‐fold higher in titers, and the mice demonstrated eightfold higher survival after intranasal challenge with a lethal dose of live influenza virus lacking Gal‐Gs. 35 For the same reason, immunogenicity of recombinant HIV viral glycoprotein gp120 and bovine serum albumin carrying α‐Gal‐Gs increased by over 4 to 30 folds in GT‐KO mice compared with these glycoproteins lacking Gal‐Gs. 36 , 37
Although anti‐Gal‐Abs are abundant in human bodies, their activity varies among individuals. 13 , 38 Meanwhile, immunization with an antigen carrying Gal‐Gs (eg, mouse cells) could result in rapid elevation in anti‐Gal‐Ab titer by 8 to 200 folds. 13 , 39 Increased anti‐Gal‐Abs are beneficial to mediate complements and APCs to destroy zoonotic viruses, bacteria, and protozoa carrying Gal‐Gs, and they thus provide better protection for humans against infectious diseases caused by these microbes including SARS‐CoV‐2 from animals. 13 , 23 , 40 Increased anti‐Gal‐Abs has displayed more effective in mediating complements to destroy Trypanosoma cruzi, the protozoan pathogen of Chagas disease in humans. 41
4. PROPOSALS FOR COVID‐19 VACCINES
From the information and evidence given above, SARS‐CoV‐2 replicating in nonprimate mammalian cells (eg, porcine PK‐15 cells), rather than simian Vero cells, carries Gal‐Gs on the viral spike (S) glycoprotein, which usually comprises 22 N‐linked glycosylation sites for adding Gal‐Gs. 23 , 28 SARS‐CoV‐2 carrying Gal‐Gs can bind to anti‐Gal‐Abs abundant in humans.
The first application of anti‐Gal‐Abs is to replace Vero cells with PK‐15 cells for the inactivated vaccines under rapid development for COVID‐19. This replacement shall probably enhance the vaccine efficacy through immune opsonization elicited by the complexes of anti‐Gal‐Abs and Gal‐Gs on the virus. 13 , 34 , 35 , 36 , 37 This potential advantage is critical for providing longer immunity against SARS‐CoV‐2. It could also be valuable to enhance the levels of antiviral antibodies to circumvent antibody‐dependent enhancement (ADE), one of the major potential pitfalls for COVID‐19 vaccine development. 42 , 43 ADE is a mechanism through which dengue viruses, feline coronaviruses, SARS coronavirus, and HIV viruses take advantage of low‐levels of antiviral antibodies to infect host cells. 42
The second application of anti‐Gal‐Abs is the development of a live unattenuated or attenuated vaccine using SARS‐CoV‐2 replicating in PK‐15 cells or other non‐primate mammalian cells (Figure 1). The efficacy of this live vaccine could be higher than other live COVID‐19 vaccines due to immune opsonization elicited by the complexes of anti‐Gal‐Abs and Gal‐Gs on the virus. 13 , 34 , 35 , 36 , 37 The safety of this live vaccine could be from three mechanisms given below (Figure 1).
Figure 1.
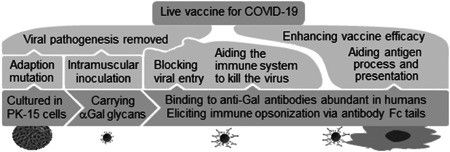
Logic for SARS‐CoV‐2 replicating in PK‐15 cells to be a live COVID‐19 vaccine. COVID‐19, corona virus 2019; SARS‐CoV‐2, severe acute respiratory syndrome coronavirus 2
First, anti‐Gal‐Abs can block the viral replication and aid complements and macrophages to destroy the virus, 13 , 16 , 17 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 making the virus less pathogenic. This safety mechanism could be standardized and strengthened through mixing the live virus and high‐quality anti‐Gal‐Abs during the vaccine production, to ensure the complexes of anti‐Gal‐Abs and Gal‐Gs are well formed in time in all vaccine recipients and those inhaling the vaccine virus unintentionally. 13 , 34 Production of high‐quality anti‐Gal‐Abs for the vaccine production is relatively inexpensive because anti‐Gal‐Abs are abundant in human blood.
Second, the live vaccine could be less pathogenic through intramuscular inoculation to bypass the pathogenesis site of the fragile lungs (Table 2). If the live vaccine is inoculated nasally, the live virus in the vaccine can attach directly to and replicate efficiently in its favorite cells. In contrast, if the live vaccine is inoculated intramuscularly, immune molecules and cells of the whole body, particularly those in the circulation system, could readily contact, identify and destroy the injected virus, a process that could be greatly facilitated by anti‐Gal‐Abs as elucidated above. Therefore, the live respiratory virions could have limited chances to replicate in humans, and their limited replication is also inhibited by innate immunity of the whole body. To test this mechanism, we recently inoculated mice with 106 50% egg‐infective dose of H5N6 subtype of avian influenza virus lacking Gal‐Gs through nasal and intramuscular administration. We found that all the mice inoculated nasally developed severe pneumonia and encephalitis with the mortality of 70%, while all the mice inoculated intramuscularly maintained health throughout the experiment and produced adequate immunity within 30 days after the inoculation and survived nasal challenge with 108 50% egg‐infective dose of the same virus (our unpublished data). The safety mechanism bypassing the pathogenesis site of the fragile lungs has also been employed in US recruits safely for 40 years for preventing adenovirus‐associated acute respiratory disease (ARD), using a live unattenuated vaccine inoculated enterally to bypass the lungs. 43 , 44 , 45 This live vaccine reduced adenovirus‐associated ARD cases in US recruits by 99.66%, and the live vaccine itself causes no more respiratory cases than the placebo. 43
Table 2.
Comparison of nasal and intramuscular inoculation of a respiratory virus
| Nasal inoculation | Intramuscular inoculation | |
|---|---|---|
| Immunity responded | Relatively few immune molecules and cells in respiratory tracts | Plenty of immune molecules and cells from the circulation system |
| Attachment & replication | The virus can directly attach to and replicate efficiently and continuously in its favorite cells | The virus should overcome immunity from the circulation system to reach and attach to its favorite cells |
| Progeny viruses | Many progeny viruses are generated for days or weeks | Few progeny viruses are generated |
| Viruses invading deeper tissues | Many progeny viruses invade the circulation system for days or weeks | Few progeny viruses invade the circulation system except the inoculated viruses |
| Viruses shed outside | Many progeny viruses are shed outside and spread to other people | Few progeny viruses are shed outside and spread to other people |
| Local pathogenesis | Local inflammation (pneumonia) is life threatening due to anoxia | Local inflammation is usually not that pathogenic |
Third, SARS‐CoV‐2 could become less pathogenic to humans due to mutations for adaption to non‐primate mammalian cells through serial passage. This traditional attenuation mechanism via serial passage of a virus in heterogenous host cells has been successfully applied in the development of live vaccines for rubella, types 1 and 3 polio, yellow fever, and measles. 10 , 46
The first two mechanisms given above could provide enough safety for the potential live COVID‐19 vaccine. If the third mechanism is needed, some cell lines, such as MDCK and BHK‐21, in which SARS‐CoV‐2 can replicate but replicates much less efficiently than in Vero or PK‐15 cells, 12 could be superior to PK‐15 cells for generating mutations for host adaption which could lead to attenuation of the virus. MDCK and BHK‐21 cells can also add Gal‐Gs to SARS‐CoV‐2.
It was estimated that inactivated vaccines for influenza require about 1010 virions per dose, and the cold‐adapted live vaccine for influenza with amino acid substitutions requires about 107 virions per dose, and the live vaccine for influenza using rare codons with no amino acid substitutions requires about 105 virions per dose. 47 If this scenario is the same to COVID‐19, production of the live vaccine using SARS‐CoV‐2 replicating in PK‐15 cells could be much more efficient than production of the inactivated vaccine using SARS‐CoV‐2 replicating in Vero cells. This is critical for rapidly manufacturing sufficient doses of COVID‐19 vaccines to curb the dreadful pandemic. 3 , 47 Such a live vaccine could even have the potential to eliminate the pandemic virus. 48
Like other live vaccines, the live vaccine proposed in this review should not be used for those not in good health or with immunodeficiency. 46 Those people with immunodeficiency could be inoculated with the inactivated vaccines carrying Gal‐Gs to help them to establish specific immunity against COVID‐19.
5. CONFIRMATION REQUIRED
Animal experiments and clinical trials are imperatively desired to confirm the potential critical advantages elucidated above for defeating COVID‐19.
First, it should be confirmed through experiments that SARS‐CoV‐2 replicating in PK‐15 cells stably carry Gal‐Gs and can thus bind to anti‐Gal‐Abs in humans. In this respect isolectin 1‐B4 from Griffonia simplicifolia (GS‐1‐B4) can be used as an immunodiagnostic reagent because of its high specificity for the glycan. 49
To confirm that SARS‐CoV‐2 replicating in PK‐15 cells can induce higher immunity, two inactivated vaccines can be prepared in the same way except that the cells for culturing SARS‐CoV‐2 are different. Then, two randomized groups of rhesus macaques are inoculated with these two inactivated vaccines, and the antibodies against SARS‐CoV‐2 are qualitatively evaluated using mini‐neutralization assay. 5 , 6
To confirm the potential that SARS‐CoV‐2 replicating in non‐primate mammalian cells could be employed as a safe and efficacious live vaccine for COVID‐19, the live vaccine can be prepared using SARS‐CoV‐2 replicating in PK‐15 cells. Then, three tested and one control groups of rhesus macaques are intramuscularly inoculated with the live vaccine or normal saline. Each macaque in the three tested groups is inoculated with 104, 106, and 108 PFUs of virions, respectively. All the macaques are challenged with nasal administration of the virus (106 PFU/macaque) replicating in Vero cells 28 days after the intramuscular inoculation. If all macaques in the control group develop pneumonia, and maintain a high viral load in throat and anal swabs 7 days after the virus challenge, 8 , 9 and all macaques in the three tested groups have neither developed pneumonia nor shed the virus via respiratory or digestive tracts, then the live vaccine is presumed safe and efficacious, and such vaccine could be considered for clinical trials in young volunteers who are more naturally resistant to the infection than the elderly. The safety and efficacy of the live attenuated vaccine prepared using SARS‐CoV‐2 adapted to another non‐primate mammalian cell line via serial passage may be preliminarily confirmed in the same way.
Notably, all relevant data should be collected from the above experiments and clinical trials to identify or exclude the possibility that the anti‐Gal‐Abs could weaken the immune response to the vaccine, and that anti‐Gal‐Abs have some potential limitations and disadvantages.
6. CONCLUSION
This review suggests with evidence that SARS‐CoV‐2 replicating in nonprimate mammalian cells, if employed as live or inactivated vaccines, may induce higher immunity against COVID‐19, with the aid of anti‐Gal antibodies abundant in humans. The safety of the live vaccine could be enhanced through intramuscular inoculation to bypass the fragile lungs. These novel vaccine strategies, if confirmed with experiments and clinical trials, provide a simple, rapid and powerful approach to defeating COVID‐19 and shed novel insight into prevention of other viral infectious diseases. Experiments are imperatively desired to examine the critical advantages of these vaccine strategies.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTION
Ji‐Ming Chen completed this work with the aid of Meng Yang, Jiwang Chen, and an anonymous scientist.
ETHICS STATEMENT
The article does not contain the participation of animals and humans other than the authors.
ACKNOWLEDGMENTS
The author thanks Meng Yang and Jiwang Chen for their helpful assistance, and thanks deeply an anonymous scientist for his very precious direction. This work was conducted at Qingdao Agricultural University and Qingdao Six‐Eight Nearby Sci‐Tech Company.
Chen J‐M. SARS‐CoV‐2 replicating in nonprimate mammalian cells probably have critical advantages for COVID‐19 vaccines due to anti‐Gal antibodies: A minireview and proposals. J Med Virol. 2021;93:351–356. 10.1002/jmv.26312
REFERENCES
- 1. World Health Organization . Coronavirus disease (COVID‐2019) situation reports. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/. Accessed July 13, 2020.
- 2.The Center for Systems Science and Engineering at Johns Hopkins University. COVID‐19 dashboard. https://coronavirus.jhu.edu/map.html. Accessed July 13, 2020.
- 3. Sahu KK, Kumar R. Preventive and treatment strategies of COVID‐19: from community to clinical trials. J Family Med Prim Care. 2020;9:2149‐2157. 10.4103/jfmpc.jfmpc_728_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sharpe HR. The early landscape of COVID‐19 vaccine development in the UK and rest of the world. Immunology. 2020;160(3):223‐232. 10.1111/imm.13222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zhang J, Zeng H, Gu J, Li H, Zheng L, Zou Q. Progress and prospects on vaccine development against SARS‐CoV‐2. Vaccines (Basel). 2020;8(2):E153. 10.3390/vaccines8020153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Corbett KS, Edwards D, Leist SR, et al. SARS‐CoV‐2 mRNA vaccine development enabled by prototype pathogen preparedness. bioRxiv. 2020. 10.1101/2020.06.11.145920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zhu FC, Li YH, Guan XH, et al. Safety, tolerability, and immunogenicity of a recombinant adenovirus type‐5 vectored COVID‐19 vaccine: a dose‐escalation, open‐label, non‐randomised, first‐in‐human trial. Lancet. 2020;395:1845‐1854. 10.1016/S0140-6736(20)31208-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gao Q, Bao L, Mao H, et al. Development of an inactivated vaccine candidate for SARS‐CoV‐2. Science. 2020;369(6499):77‐81. 10.1126/science.abc1932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wang H, Zhang Y, Huang B, et al. Development of an inactivated vaccine candidate, BBIBP‐CORV, with potent protection against SARS‐CoV‐2. Cell. 2020;182:1‐9. 10.1016/j.cell.2020.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization. Immunization, Vaccines and Biologicals. https://www.who.int/immunization/diseases/en/. Accessed July 13, 2020.
- 11. Chen JW, Chen JM. Potential of live pathogen vaccines for defeating the COVID‐19 pandemic: history and mechanism. J Med Virol. 2020;92. 10.1002/jmv.25920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chu H, Chan JF, Yuen TT, et al. Comparative tropism, replication kinetics, and cell damage profiling of SARS‐CoV‐2 and SARS‐CoV with implications for clinical manifestations, transmissibility, and laboratory studies of COVID‐19: an observational study. Lancet Microbe. 2020;1. 10.1016/S2666-5247(20)30004-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Galili U. Human natural antibodies to mammalian carbohydrate antigens as unsung heroes protecting against past, present, and future viral infections. Antibodies. 2020;9(2):E25. 10.3390/antib9020025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Galili U, Shohet SB, Kobrin E, Stults CLM, Macher BA. Man, apes, and Old‐World monkeys differ from other mammals in the expression of α‐Galactosyl glycans on nucleated cells. J Biol Chem. 1988;263:17755‐17762. [PubMed] [Google Scholar]
- 15. Galili U, Repik PM, Anaraki F, Mozdzanowska K, Washko G, Gerhard W. Enhancement of antigen presentation of influenza virus hemagglutinin by the natural anti‐Gal antibody. Vaccine. 1996;14:321‐328. [DOI] [PubMed] [Google Scholar]
- 16. Pipperger L, Koske I, Wild N, et al. Xenoantigen‐dependent complement‐mediated neutralization of LCMV glycoprotein pseudotyped VSV in human serum. J Virol. 2019;93(18):e00567. 10.1128/JVI.00567-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Repik PM, Strizki M, Galili U. Differential host dependent expression of α‐galactosyl glycans on viral glycoproteins: A study of Eastern equine encephalitis virus as a model. J Gen Virol. 1994;75:1177‐1181. [DOI] [PubMed] [Google Scholar]
- 18. Galili U, Swanson K. Gene sequences suggest inactivation of α1‐3 Galactosyltransferase in catarrhines after the divergence of apes from monkeys. Proc Natl Acad Sci USA. 1991;88:7401‐7404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Montassier E, Al‐Ghalith GA, Mathé C, et al. Distribution of bacterial α1,3‐galactosyltransferase genes in the human gut microbiome. Front Immunol. 2020;10:3000. 10.3389/fimmu.2019.03000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hamadeh RM, Galili U, Zhou P, Griffiss JM. Anti‐alpha‐galactosyl immunoglobulin A (IgA), IgG, and IgM in human secretions. Clin Diagn Lab Immunol. 1995;2:125‐131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Stowell SR, Arthur CM, McBride R, et al. Microbial glycan microarrays define key features of host‐microbial interactions. Nat Chem Biol. 2014;10(6):470‐476. 10.1038/nchembio.1525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Watkins WM. Biochemistry and genetics of the ABO, Lewis, and P blood group systems. Adv Hum Genet. 1980;10:379‐385. [DOI] [PubMed] [Google Scholar]
- 23. Breiman A, Ruvën‐Clouet N, Le Pendu J. Harnessing the natural anti‐glycan immune response to limit the transmission of enveloped viruses such as SARS‐CoV‐2. PLOS Pathog. 2020;16(5):e1008556. 10.1371/journal.ppat.1008556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Zhao J, Yang Y, Huang H‐P, et al. Relationship between the ABO blood group and the COVID‐19 susceptibility. medRxiv. 2020. 10.1101/2020.03.11.20031096 [DOI] [Google Scholar]
- 25. Leaf RK, Al‐Samkari H, Brenner SK, Gupta S, Leaf DE. ABO phenotype and death in critically ill patients with COVID‐19. Br J Haematol. 2020;189. 10.1111/bjh.16984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Xu Y, Lorf T, Sablinski T, et al. Removal of anti‐porcine natural antibodies from human and nonhuman primate plasma in vitro and in‐vivo by a Gal α 1‐3Gal β 1‐4 β Glc‐X immuneaffinity column. Transplantation. 1998;65:172‐179. [DOI] [PubMed] [Google Scholar]
- 27. Galili U. Evolution in primates by "Catastrophic‐selection" interplay between enveloped virus epidemics, mutated genes of enzymes synthesizing carbohydrate antigens, and natural anti‐carbohydrate antibodies. Am J Phys Anthropol. 2019;168(2):352‐363. 10.1002/ajpa.23745 [DOI] [PubMed] [Google Scholar]
- 28. Wang D. Coronaviruses' sugar shields as vaccine candidates. Curr Trends Immunol. 2020;21:17‐23. [PMC free article] [PubMed] [Google Scholar]
- 29. Takeuchi Y, Porter CD, Strahan KM, et al. Sensitization of cells and retroviruses to human serum by.α1‐3 Galactosyltransferase. Nature. 1996;379:85‐88. [DOI] [PubMed] [Google Scholar]
- 30. Welsh RM, O'Donnell CL, Reed DJ, Rother RP. Evaluation of the Galα1‐3Gal epitope as a host modification factor eliciting natural humoral immunity to enveloped viruses. J Virol. 1998;72:4650‐4656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Preece AF, Strahan KM, Devitt J, Yamamoto F, Gustafsson K. Expression of ABO or related antigenic carbohydrates on viral envelopes leads to neutralization in the presence of serum containing specific natural antibodies and complement. Blood. 2002;99(7):2477‐2482. 10.1182/blood.v99.7.2477 [DOI] [PubMed] [Google Scholar]
- 32. Rother RP, Fodor WL, Springhorn JP, et al. A novel mechanism of retrovirus inactivation in human serum mediated by anti‐α‐Galactosyl natural antibody. J Exp Med. 1995;182:1345‐1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hayashi S, Ogawa S, Takashima Y, Otsuka H. The neutralization of pseudorabies virus by anti‐α‐Galactocyl natural antibody in normal serum. Virus Res. 2004;99:1‐7. [DOI] [PubMed] [Google Scholar]
- 34. Wang X, Wang B, Wen Y. From therapeutic antibodies to immune complex vaccines. NPJ Vaccines. 2019;4:2. 10.1038/s41541-018-0095-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Abdel‐Motal UM, Guay HM, Wigglesworth K, Welsh RM, Galili U. Increased immunogenicity of influenza virus vaccine by anti‐Gal mediated targeting to antigen presenting cells. J Virol. 2007;81(17):9131‐9141. 10.1128/JVI.00647-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Abdel‐Motal UM, Wang S, Awwad S, Lu S, Wigglesworth K, Galili U. Increased immunogenicity of HIV‐1 p24 and gp120 following immunization with gp120/p24 fusion protein vaccine expressing α‐Gal epitopes. Vaccine. 2010;28(7):1758‐1765. 10.1016/j.vaccine.2009.12.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Benatuil L, Kaye J, Rich RF, Fishman JA, Green WR, Iacomini J. The influence of natural antibody specificity on antigen immunogenicity. Eur J Immunol. 2005;35:2638‐2647. [DOI] [PubMed] [Google Scholar]
- 38. Buonomano R, Tinguely C, Rieben R, Mohacsi PJ, Nydegger UE. Quantitation and characterization of anti‐Galα1‐3Gal antibodies in sera of 200 healthy persons. Xenotransplantation. 1999;6:173‐180. [DOI] [PubMed] [Google Scholar]
- 39. Maruyama S, Cantu E, DeMartino C, et al. Interaction of baboon anti‐α‐galactosyl antibody with pig tissues. Am J Pathol. 1999;155:1635‐1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. de la Fuente J, Gortázar C, Cabezas‐Cruz A, et al. Boosting anti‐alpha‐Gal immune response to control COVID‐19. R Soc Open Sci. 2020;7. 10.17605/OSF.IO/XHDPU [DOI] [Google Scholar]
- 41. Almeida IC, Ferguson MA, Schenkman S, Travassos LR. Lytic anti‐ α ‐galactosyl antibodies from patients with chronic Chagas’ disease recognize novel O‐linked oligosaccharides on mucin‐like glycosyl‐phosphatidylinositol‐anchored glycoproteins of Trypanosoma cruzi. Biochem J. 1994;304:793‐802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Wang SF, Tseng SP, Yen CH, et al. Antibody‐dependent SARS coronavirus infection is mediated by antibodies against spike proteins. Biochem Biophys Res Commun. 2014;451(2):208‐214. 10.1016/j.bbrc.2014.07.090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Cao X. COVID‐19: immunopathology and its implications for therapy. Nat Rev Immunol. 2020;20(5):269‐270. 10.1038/s41577-020-0308-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Couch RB, Chanock RM, Cate TR, Lang DJ, Knight V, Huebner RJ. Immunization with types 4 and 7 adenovirus by selective infection of the intestinal tract. Am Rev Respir Dis. 1963;88(Suppl):394‐403. 10.1164/arrd.1963.88.3P2.394 [DOI] [PubMed] [Google Scholar]
- 45. Choudhry A, Mathena J, Albano JD, Yacovone M, Collins L. Safety evaluation of adenovirus type 4 and type 7 vaccine live, oral in military recruits. Vaccine. 2016;34(38):4558‐4564. 10.1016/j.vaccine.2016.07.033 [DOI] [PubMed] [Google Scholar]
- 46. Graham BS, Crowe JE. Immunization against viral diseases. In: Knipe DM, Howley PM, eds. Fields' virology. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:487‐538. [Google Scholar]
- 47. Stauft CB, Yang C, Coleman JR, et al. Live‐attenuated H1N1 influenza vaccine candidate displays potent efficacy in mice and ferrets. PLOS One. 2019;14:e0223784. 10.1371/journal.pone.0223784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Chen JM, Sun YX, Chen JW. Potential for elimination of SAR‐CoV‐2 through vaccination as inspired by elimination of multiple influenza viruses through natural pandemics or mass vaccination. J Med Virol. 2020;92. 10.1002/jmv.26162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Tempel W, Tschampel S, Woods RJ. The xenograft antigen bound to Griffonia simplicifolia lectin 1‐B(4). X‐ray crystal structure of the complex and molecular dynamics characterization of the binding site. J Biol Chem. 2002;277(8):6615‐6621. 10.1074/jbc.M109919200 [DOI] [PMC free article] [PubMed] [Google Scholar]


