1.
Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome, (formerly known as drug‐induced hypersensitivity syndrome) is an acute, idiosyncratic, and potentially life‐threatening drug reaction, characterized by fever (>38.5°C), skin eruptions, and haematological abnormalities. 1 The most frequently involved drugs are anticonvulsants, sulfonamides, allopurinol, and antibiotics, 2 while hydroxychloroquine has been rarely reported as causative agent.2, 3
CASE REPORT
A 37‐year‐old woman consulted the emergency department for itchy rash, facial edema, and fever (38.5°) developing in the course of 2 days. Physical examination revealed a maculopapular rash, predominantly in the face, periorbital angioedema, and purpuric rash with involvement of the trunk and limbs, but sparing of palms and soles (Figure 1A). Bilateral cervical lymphadenopathy and oral mucosa enanthema were present. The patient had been treated in the previous 2–3 weeks for bilateral pneumonia as manifestation of suspected, but not confirmed, COVID‐19, with hydroxychloroquine 200 mg and lopinavir‐ritonavir 200/50 mg/12 hours and azithromycin 250 mg/day for 5 days.
Laboratory tests showed leukocytosis with eosinophilia and elevated transaminases. Abdominal ultrasound was normal, and no atypical lymphocytes were found. Bacterial cultures and viral serologies, including SARS‐CoV‐2, were negative except for IgG for cytomegalovirus, parvovirus B‐19, Epstein–Barr virus, chickenpox, and measles, which were positive.
After 8 weeks, patch tests were performed with lopinavir/ritonavir, hydroxychloroquine, and azithromycin (each 20% aq. and pet.), which were positive for hydroxychloroquine on day (D) 4 (Figure 1B). Therefore, DRESS was diagnosed in accordance with RegiSCAR group criteria, 4 and an atypical DRESS according to SCAR‐J's criteria, caused by hydroxychloroquine (Figure 1A and B).
FIGURE 1.
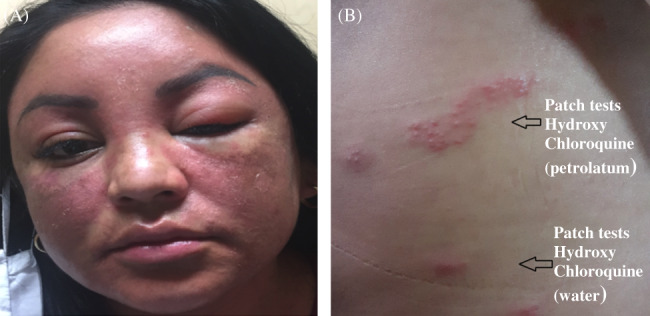
(A) Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome due to hydroxychloroquine. Periorbital edema and maculopapular rash on the face. (B) Patch tests with hydroxychloroquine (petrolatum and water) were positive
DISCUSSION
Hydroxychloroquine has been used as an antimalarial. Nowadays, it is used in autoimmune diseases such as lupus and rheumatoid arthritis. The growth of many different viruses can be inhibited in cell culture by chloroquine and hydroxychloroquine, including SARS‐CoV‐2. 5 Therefore, it had been prescribed to our patient with suspected COVID‐19.
Hydroxychloroquine is considered to be safe and side‐effects are generally mild and transitory. 5 The most common adverse effect of hydroxychloroquine is a a skin rash; however, in our patient, DRESS syndrome caused by hydroxychloroquine was diagnosed, based on patch testing that proved useful for identifying the causative drug in this patient. 6 In conclusion, we have presented the first case of DRESS syndrome due to hydroxychloroquine with a positive patch test.
2. CONFLICTS OF INTEREST
The authors dclare no conflict of interest.
AUTHOR CONTRIBUTIONS
Mª Araceli Castro Jiménez: Conceptualization; data curation; resources; software; supervision; writing‐original draft; writing‐review and editing. Nuria Navarrete Navarrete: Conceptualization; data curation; supervision. Alejandro Raul Gratacos Gomez: Writing‐review and editing. Fernando Florido López: Conceptualization; data curation; software. Rosa Garcia Rodriguez: Writing‐original draft; writing‐review and editing. Gomez Elisa: Conceptualization; project administration; supervision; validation; writing‐original draft; writing‐review and editing.
Castro Jiménez A, Navarrete Navarrete N, Gratacós Gómez AR, Florido López F, García Rodríguez R, Gómez Torrijos E. First case of DRESS syndrome caused by hydroxychloroquine with a positive patch test. Contact Dermatitis. 2021;84:50–51. 10.1111/cod.13657
REFERENCES
- 1. Taweesedt PT, Nordstrom CW, Stoeckel Y, Dumic I. Pulmonary manifestations of drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome: A Systematic Review. Biomed Res Int. 2019;2019:1‐10. 10.1155/2019/7863815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Grandolfo M, Romita P, Bonamonte D, et al. Drug reaction with eosinophilia and systemic symptoms syndrome to hydroxychloroquine, an old drug in the spotlight in the COVID‐19 era. Dermatol Ther. 2020:1‐2. e13499. 10.1111/dth.13499. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Volpe A, Marchetta A, Caramaschi P, Biasi D, Bambara LM, Arcaro G. Hydroxychloroquine‐induced DRESS syndrome. Clin Rheumatol. 2008;27(4):537‐539. [DOI] [PubMed] [Google Scholar]
- 4. Cabañas R, Ramírez E, Sendagorta E, et al. Spanish guidelines for diagnosis, management, treatment and prevention of DRESS syndrome. J Investig Allergol Clin Immunol. 2020. 30(4):229–253 [DOI] [PubMed] [Google Scholar]
- 5. Touret F, Lamballerie X. Of chloroquine and COVID‐19. Antiviral Res. 2020;177:1‐2.104762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Carneiro‐Leão L, Gomes I, Freitas C, Costa e Silva M, Viseu R, Cernadas J. Multiple drug hypersensitivity syndrome to antituberculosis drugs: a case report. J Investig Allergol Clin Immunol. 2020;30(1):70‐71. [DOI] [PubMed] [Google Scholar]


