To the Editor,
Reuters reported “The coronavirus mortality rate among some of the poorest Catalans is five times higher than among the wealthiest residents of the Spanish region, a study showed, in the latest evidence of how COVID‐19 hits the needy hardest” on 22 May 2020 (https://www.reuters.com/article/us-health-coronavirus-spain-study/virus-deaths-five-times-higher-among-poor-in-spanish-region-idUSKBN22Y23M). It has been suggested that outcomes of pandemic influenza are associated with socioeconomic status. 1 Socioeconomic characteristics also may affect prevalence and case fatality of coronavirus disease 2019 (COVID‐19). To screen potential risk and protective socioeconomic factors for COVID‐19 prevalence and fatality, meta‐regression of data from the top 50 U.S. large cities was performed.
From the “Population and Housing Unit Estimates (https://www.census.gov/programs-surveys/popest.html),” the top 50 U.S. large‐population cities (2019) were selected. The population estimate (2019) of each county to which the city belongs was abstracted from the “County Population Totals: 2010‐2019 (https://www.census.gov/data/tables/time-series/demo/popest/2010s-counties-total.html).” From the “Johns Hopkins Coronavirus Resource Center (https://coronavirus.jhu.edu/us-map),” the cumulative number of confirmed cases and deaths of COVID‐19 in each county was obtained on 22 May 2020. Socioeconomic characteristics of each county were extracted from the “2014‐2018 ACS 5‐Year Data Profile (https://www.census.gov/acs/www/data/data-tables-and-tools/data-profiles/)” and “SAIPE Program (2018) (https://www.census.gov/programs-surveys/saipe.html),” which included male (%), 65 years and over (%), Black/African‐American (%), Hispanic/Latino (%), never married in population 15 years and over (%), high school graduate or higher in population 25 years and over (%), households with a computer (%) and broadband Internet subscription (%), unemployment rate (%), median and mean (dollars) household income, civilian noninstitutionalized population with private health insurance (%), public coverage (%), and no health insurance coverage (%), and poverty rate (%) (Table S1). Random‐effects meta‐regression was performed using OpenMetaAnalyst (http://www.cebm.brown.edu/openmeta/index.html). We defined COVID‐19 prevalence and case‐fatality, respectively, as confirmed cases divided by population and deaths by confirmed cases. A meta‐regression graph depicted the COVID‐19 prevalence or fatality (plotted as the logarithm‐transformed prevalence or fatality on the y‐axis) as a function of a given factor (plotted as a socioeconomic characteristic on the x‐axis). Covariates with a significantly (P < .05) positive or negative coefficient in the univariable model were together entered into the multivariable model.
Results of the meta‐regression were summarized in Table 1. A coefficient (slope of the meta‐regression line) for COVID‐19 prevalence was significantly negative for male sex (P < .001; Figure 1A), education attainment (P = .011), computer (P < .001; Figure 1B) and Internet (P < .001) use, and private health insurance (P = .029), which suggests that COVID‐19 prevalence may decrease significantly as male sex, education attainment, computer and Internet use, and private health insurance increases. Whereas the coefficient was significantly positive for Black race (P < .001), never matrimony (P < .001; Figure 1C), unemployment (P = .003), and poverty (P < .001), which suggests that COVID‐19 prevalence may increase significantly as Black race, never matrimony, and poverty increases. In the multivariable model entering all these nine covariates, the coefficient was significantly negative for male sex (P = .036) and computer use (P = .024), and significantly positive for never matrimony (P < .001), which suggests that male sex and computer use may be independently and negatively associated with COVID‐19 prevalence and never matrimony may be independently and positively associated with COVID‐19 prevalence.
Table 1.
Meta‐regression summary
| Covariate | Prevalence | Case fatality | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Coefficients | P | Multivariable P | Coefficients | P | Multivariable P | ||||||
| Lower bound | Upper bound | Lower bound | Upper bound | ||||||||
| Male (%) | −0.587 | −0.831 | −0.344 | <.001 | .036 | −0.148 | −0.296 | 0.001 | .051 | … | |
| 65 y and over (%) | 0.067 | −0.090 | 0.224 | .401 | … | 0.138 | 0.064 | 0.212 | <.001 | .004 | |
| Black/African‐American (%) | 0.032 | 0.015 | 0.048 | <.001 | .395 | 0.004 | −0.005 | 0.014 | .391 | … | |
| Hispanic/Latino (%) | −0.005 | −0.021 | 0.010 | .508 | … | −0.004 | −0.012 | 0.004 | .355 | … | |
| Never married (%) | 0.104 | 0.071 | 0.138 | <.001 | <.001 | 0.019 | −0.044 | 0.042 | .099 | … | |
| High school graduate or higher (%) | −0.076 | −0.134 | −0.017 | .011 | .146 | −0.000 | −0.033 | 0.033 | .992 | … | |
| Households | With a computer (%) | −0.169 | −0.237 | −0.101 | <.001 | .024 | −0.029 | −0.072 | 0.014 | .183 | … |
| With a broadband Internet subscription (%) | −0.098 | −0.145 | −0.050 | <.001 | .31 | −0.017 | −0.045 | 0.011 | .241 | … | |
| Unemployment rate (%) | 0.245 | 0.086 | 0.404 | .003 | .878 | 0.111 | 0.025 | 0.197 | .011 | .141 | |
| Household income | Median (dollars) | −0.000 | −0.000 | 0.000 | .208 | … | −0.000 | −0.000 | 0.000 | .639 | … |
| Mean (dollars) | −0.000 | −0.000 | 0.000 | .744 | … | −0.000 | −0.000 | 0.000 | .947 | … | |
| Civilian noninstitutionalized population | With private health insurance (%) | −0.033 | −0.063 | −0.003 | .029 | .957 | −0.009 | −0.025 | 0.007 | .282 | … |
| With public coverage (%) | 0.024 | −0.002 | 0.051 | .071 | … | 0.018 | 0.004 | 0.031 | .011 | .622 | |
| No health insurance coverage (%) | −0.036 | −0.096 | 0.024 | .236 | … | −0.041 | −0.071 | −0.011 | .007 | .069 | |
| Poverty rate (%) | 0.095 | 0.039 | 0.151 | <.001 | .076 | 0.027 | –0.005 | 0.059 | .097 | … | |
Figure 1.
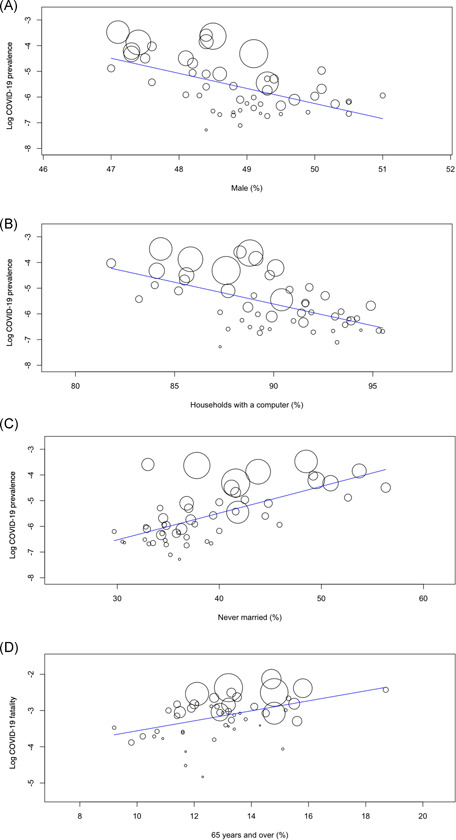
Meta‐regression graph depicting the coronavirus disease 2019 (COVID‐19) (A‐C) prevalence or (D) fatality (plotted as the logarithm‐transformed prevalence or fatality on the y‐axis) as a function of a given factor (plotted as a socioeconomic characteristic on the x‐axis)
A coefficient for COVID‐19 fatality was significantly negative for no health insurance (P = .007), and significantly positive for elderly (P < .001; Figure 1D), unemployment (P = .011), and public coverage (P = .011). In the multivariable model, the coefficient was significantly positive only for the elderly (P = .004), which suggests that the elderly may be independently and positively associated with COVID‐19 fatality.
The present results suggest an independent and negative association of male sex and computer use with COVID‐19 prevalence, an independent and positive association of never matrimony with COVID‐19 prevalence, and an independent and positive association of elderly with COVID‐19 fatality. Our findings never denote, for instance, that a subject having a computer is at a low risk of COVID‐19 prevalence, which should be noted. Because of the community‐level epidemiological study, the present results simply denote, for instance, that COVID‐19 prevalence is lower in a community in which there are more subjects having a computer. Further patient‐level clinical studies would be expected to determine, for instance, whether a subject having a computer is at a low risk of COVID‐19 prevalence. In meta‐regression being generally different from simple regression, the relationship between the outcome and explanatory variables is more influenced by larger samples (counties in case of the present analysis) than by smaller samples because the precision of each estimate weights samples. 2 Thus, to screen potential risk and protective socioeconomic factors for COVID‐19 prevalence and fatality, meta‐regression may be more valid than simple regression.
More expression of angiotensin‐converting enzyme 2, 3 receptors of which severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) binds to and uses in entering host cells, 4 in males' renin‐angiotensin‐aldosterone system could play an important role in COVID‐19 severity in males. 4 These molecular biological findings 3 , 4 and results of a systematic review 5 of clinical studies suggest that male sex is a risk factor of COVID‐19 severity, which does not accord with the negative association of male sex with COVID‐19 prevalence (ie, SARS‐CoV‐2 infection) and no correlation of male sex to COVID‐19 fatality indicated in the present community‐level epidemiological analysis. Mechanisms of SARS‐CoV‐2 infection may differ from those of COVID‐19 severity including fatality. Immunosenescence could expound the positive association of elderly with COVID‐19 fatality. 6 Marriage status as well as other sociodemographic characteristics predicting help‐seeking behavior 7 might be correlated to the positive association of never matrimony with COVID‐19 prevalence. Furthermore, computer users could obtain more information about COVID‐19 prevention via the Internet, which may explain the negative correlation of compute use to COVID‐19 prevalence.
In conclusion, the present community‐level epidemiological analysis indicated that COVID‐19 prevalence was lower in a city with more males and computer users, the prevalence is higher in an urban including more never‐married subjects, and the fatality was higher in a community with more proportion of elderly, which suggests that male sex (negatively for prevalence), elderly (positively for fatality), never matrimony (positively for prevalence), and computer use (negatively for prevalence) may be associated with COVID‐19.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
All authors have seen the manuscript and agree to the content and data. All the authors played a significant role in the paper.
Supporting information
Supporting information
REFERENCES
- 1. Mamelund SE, Shelley‐Egan C, Rogeberg O. The association between socioeconomic status and pandemic influenza: protocol for a systematic review and meta‐analysis. Syst Rev. 2019;8:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Higgins JPT, Thomas J, Chandler J, et al., eds. Chapter 10: analysing data and undertaking meta‐analyses. Cochrane Handbook for Systematic Reviews of Interventions Version 6.0. Cochrane; 2019. [Google Scholar]
- 3. Hoffmann M, Kleine‐Weber H, Schroeder S, et al. SARS‐CoV‐2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271‐280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Komukai K, Mochizuki S, Yoshimura M. Gender and the renin‐angiotensin‐aldosterone system. Fundam Clin Pharmacol. 2010;24:687‐698. [DOI] [PubMed] [Google Scholar]
- 5. Galbadage T, Peterson BM, Awada J, et al. Systematic review and meta‐analysis of sex‐specific COVID‐19 clinical outcomes. Front Med. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kadambari S, Klenerman P, Pollard AJ. Why the elderly appear to be more severely affected by COVID‐19: the potential role of immunosenescence and CMV. Rev Med Virol. 2020. 10.1002/rmv.2144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lai R, Tan L, Lai X, Zhang X, Zhou Q. Help‐seeking behavior of returning to work in healthcare workers and its influencing factors during COVID‐19 subsiding. J Occup Environ Med. 2020. 10.1097/JOM.0000000000001959 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information


