To the Editor:
The coronavirus disease of 2019 (Covid19) was first reported to be responsible for a cluster of cases of viral pneumonia in December 2019 in the Chinese city of Wuhan. 1 In consultation with World Health Organization (WHO), different degrees of lockdown, social distancing measures, travel restrictions, and restructuring of health services were enforced in different parts of the world, depending upon where the regions were on the pandemic curve. 2 There is increasing evidence on the unintended consequences of pandemic‐related lockdown restrictions such as delayed diagnosis and increased morbidity and mortality at the time of initial presentation. 3 , 4
We retrospectively reviewed all of our outpatient activity and new patients admitted to the pediatric oncology and hematopoietic stem cell transplant (HSCT) service from December 2019 to May 2020, the last 3‐month period corresponding to coronavirus lockdown. In addition to the numbers and types of malignancies, we looked at the pattern of presentation, need for nonelective pediatric intensive care unit (PICU) stay at presentation, and morbidity or mortality within the first week after presentation.
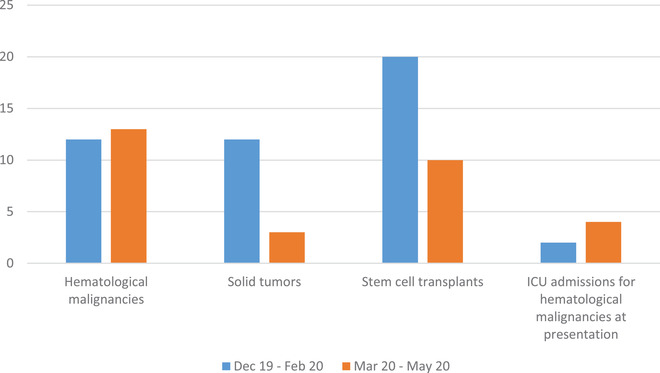
There were 24 new patients admitted to the pediatric oncology service from December 2019 to February 2020, 12 each of hematological malignancies and solid tumors. From March to May 2020, there were 16 new cases, 13 with hematological malignancies and three with solid tumors, corresponding to a 33% overall reduction (Figure 1). There were two patients with hematological malignancies who required PICU admission at the time of initial presentation from December 2019 to February 2020, while there were four such admissions from March to May 2020 (Figure 1). In the solid tumor subgroup from December 2019 to February 2020, there were four PICU admissions (three of which were elective) at the time of initial presentation and none from March to May 2020.
FIGURE 1.
Impact of Covid19 on pediatric oncology and stem cell transplant service
A total of 20 allogeneic and autologous stem cell transplants were carried out from December 2019 to February 2020 as compared to 10 in the following 3 months corresponding to Covid19‐related lockdown restrictions (Figure 1). In our outpatient clinics, there were a total of 1816 outpatient visits in the first 3 months that reduced to 1073 in the last 3 months.
In our study, we did not find any significant difference in the number of new hematological malignancies but there was 75% reduction in the number of new solid tumor cases between the two time intervals. It raises the concern that these missed solid tumor patients will present later, possibly with advanced‐stage disease impacting their curability, an experience observed by Ferrari at al. 5
With respect to severity of disease, we noticed a significant increase in the incidence of PICU admissions at the time of presentation for hematological malignancies during the time of pandemic‐related lockdown. There was a significant delay in presentation in a 5‐month‐old infant with high‐white‐count acute lymphoblastic leukemia who presented with an intracranial bleed and multiorgan failure. She required prolonged ventilation and intensive care support and is fortunately alive but the impact of her initial resuscitation and potential hypoxic brain damage to brain is difficult to quantify now and could eventually impact her neurological outcome.
There was only one death during the first week after presentation, also occurring during the second half of the study. A 6‐year‐old girl with advanced Burkitts lymphoma who developed tumor lysis syndrome, severe sepsis and unfortunately succumbed to her disease within first week of presentation. Within solid tumors, there was no increase in PICU admissions at the time of presentation but that is not surprising considering the significant reduction in their numbers during the lockdown.
All elective stem cell transplants for benign hematological conditions were put on hold during the months of March to May 2020 and the transplant workload was limited to high‐risk or relapsed hematological malignancies and autologous stem cell infusions for solid tumor patients, which was in line with international practice. 6 , 7 Difficulties in approaching unrelated donor registries because of donors’ unavailability or travel bans led to transplanting only from matched related donors or haplo‐identical family members. 6 , 7 , 8 The startling decrease in the number of outpatient clinic visits during the lockdown months did not affect chemotherapy administration for patients on active treatment and virtual clinics were introduced where practical. This is something worth considering as a standard practice, even after the pandemic is over, for better utilization of outpatient clinic services.
Despite the concerns that chemotherapy‐related immunosuppression is a risk factor to develop severe disease with Covid19, there is growing evidence that coronavirus‐related mortality is extremely rare in pediatric cancer patients. 5 , 9 , 10 Minotti et al, in a systematic review, postulated that cancer treatment‐related immunesuppression may be a protective factor against the development of cytokine release syndrome, which is highly associated with coronavirus‐related mortality. 11 Further research is needed, but the deleterious effects of delayed diagnosis and treatment in pediatric cancer patients warrants that we reconsider our approach to the design of pediatric cancer services in the event of a second peak of Covid19 and future such pandemics. 12
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
ACKNOWLEDGMENTS
We acknowledge the contribution of our clinical and administrative staff within the department who take the responsibility of managing the departmental data of new patients and outpatient clinic visits.
REFERENCES
- 1. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497‐506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. WHO . WHO Director General's opening remarks at the media briefing on COVID19. 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19. Accessed March 11, 2020.
- 3. Piccininni M, Rohmann JL, Foresti L, et al. Use of all‐cause mortality to quantify the consequences of covid‐19 in Nembro, Lombardy: descriptive study. BMJ. 2020;369:m1835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Parasole R, Stellato P, Conter V, et al. Collateral effects of COVID‐19 pandemic in pediatric hematooncology: fatalities caused by diagnostic delay. Pediatr Blood Cancer. 2020:e28482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ferrari A, Zecca M, Luksch R, et al. Children with cancer in the time of COVID‐19: an 8‐week report from the six pediatric onco‐hematology centres in Lombardi, Italy. Letter to the Editor. Pediatr Blood Cancer. 2020:e28410 10.1002/pbc.28410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ljungman P, Mikulsk M, de la Camara R, et al. The challenge of COVID‐19 and hematopoietic cell transplantation; EBMT recommendations for management of hematopoietic cell transplant recipients, their donors, and patients undergoing CAR T‐cell therapy. Bone Marrow Transplant. 2020. 10.1038/s41409-020-0919-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sah KK, Siddiqui AD, Cerny J. COVID‐19 pandemic and impact on hematopoietic stem cell transplantation. Bone Marrow Transplant. 2020. 10.1038/s41409-020-0913-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. WMDA . WMDA guidance on COVID19 impact on registry operations. https://share.wmda.info/display/LP/COVID-19%2B-%2BImpact%2Bon%2BRegistry%2BOperations Accessed 16th June 2020
- 9. Andre N, Rouger‐Gaudichon J, Brethon B, et al. COVID‐19in pediatric oncology from French pediatric oncology and hematology centers: high risk of severe forms? Letter to the Editor. Pediatr Blood Cancer. 2020:e28410 10.1002/pbc.28410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cela E, Baragaño M, Galán V, et al. COVID‐19 infection in children and adolescents with cancer in Madrid. Letter to the Editor. Pediatr Blood Cancer. 2020;67:e28397 10.1002/pbc.28397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Minotti C, Tirelli F, Barbeiri E, et al. How is immunosuppressive status affecting children and adults in SARS‐CoV infection? A systematic review. J Infect. 2020;81:e61‐e66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Anonymous . Safeguarding cancer care in a post‐COVID‐19 world. Lancet Oncol. 2020; 21(5):603 10.1016/S1470-2045(20)30243-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


