Since the COVID‐19 (SARS‐COV‐2) pandemic began, a number of facial dermatoses, such as acne, rosacea and seborrhoeic dermatitis, secondary to prolonged use of personal protective equipment (PPE) have been reported in frontline healthcare workers.1 By contrast, when we performed a retrospective report on 4 May 2020 of ‘emergent’ diagnoses during the lockdown period in our Dermatology Unit (Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Milan, Italy) we did not observe an increasing number of facial dermatoses among the general population.2 However, on this date, the Italian government moved to Phase 2 of the pandemic crisis, which allowed people to more freedom in daily life but with the obligation, in most Italian regions, to cover the mouth and nose with a facemask. Consequently, the usage time of PPE greatly increased and shortly afterwards, the first mask‐induced facial dermatoses in people who were not healthcare workers came to our attention.
Patient 1 was a 32‐year‐old woman, who developed a persistent bilateral erythematous rash on her cheeks 2 weeks after the end of lockdown (Fig. 1a). She reported a history of facial flushing and a usage time of an N95 mask for 6 h/day because she shared a workplace with two other people. We made a clinical diagnosis of rosacea and prescribed doxycycline 40 mg for 12 weeks, which provided clinical benefit.
Figure 1.
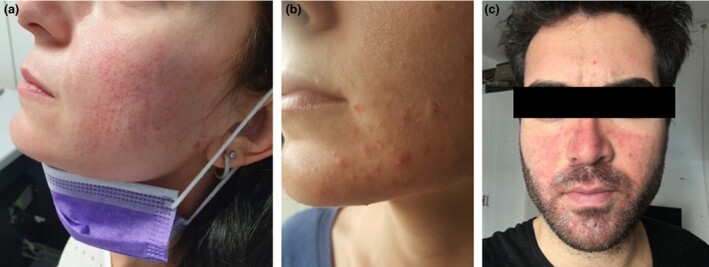
Common facial dermatoses in general population, induced by protective mask: (a) rosacea; (b) acne; (c) seborrhoeic dermatitis.
Patient 2 was a 24‐year‐old woman diagnosed with occlusive acne. Clinical examination showed numerous inflamed papules, pustules and microcomedones located on the chin and jaws bilaterally (Fig. 1b). She had a history of facial seborrhoea but she had never developed similar acne lesions. She worked as barmaid and used a facial mask and goggles for the entirety of her 8‐h work shift. Treatment consisted of daily application of adapalene 0.1% plus benzoyl peroxide 2.5% gel for 8 weeks, with zinc gluconate 175 mg and nicotinamide 27 mg daily for 3 months.
Patient 3 was a 29‐year‐old man with acute exacerbation of seborrhoeic dermatitis. Erythema and greasy scales appeared on the patient’s nose, cheeks and beard (Fig. 1c), areas covered by the facial mask. He was treated with low‐potency steroid cream for 5 days followed by pimecrolimus 1% ointment daily application for another 10 days.
Facial dermatoses are common diseases for dermatologists; however, there are some challenging aspects to face with during the COVID‐19 pandemic. Even though it has been demonstrated that facial protections induce occlusion and consequently a damp and warm microenvironment, which can cause or exacerbate these conditions,3 physicians cannot suggest simply abandoning use of PPE; however, a surgical mask can be recommended instead of an N95 mask, if the work activity allows it. Suggested treatment should include recommendations on daily skin care, such as application of moisturizers before and after mask utilization. Treating these dermatoses may prevent also COVID‐19 contagion, because facial skin damage causes pruritus, which may induce the wearer to scratch the face and/or to remove the mask,4 with a consequent reduction in PPE effectiveness.
We report these cases to highlight that dermatologists must be aware of the risk of increasing incidence of facial dermatoses among the general population in Phase 2 of lockdown, due to occlusive effects of facial PPE.
Contributor Information
S. Giacalone, Department of Physiopathology and Transplantation Università degli Studi di Milano MilanItaly
A. Minuti, Dermatology Unit Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico Milan Italy
C. B. Spigariolo, Department of Physiopathology and Transplantation Università degli Studi di Milano MilanItaly
E. Passoni, Dermatology Unit Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico Milan Italy
G. Nazzaro, Dermatology Unit Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico Milan Italy
References
- Singh M, Pawar M, Bothra A et al. Personal protective equipment induced facial dermatoses in healthcare workers managing COVID‐19 cases. J Eur Acad Dermatol Venereol 2020; 34: e378–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giacalone S, Bortoluzzi P, Nazzaro G. Which are the “emergent” dermatologic practices during COVID‐19 pandemic? Report from the lockdown in Milan, Italy. Int J Dermatol 2020; 9: e269–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan Y, Chen H, Chen L et al. Consensus of Chinese experts on protection of skin and mucous membrane barrier for health‐care workers fighting against coronavirus disease 2019. Dermatol Ther 2020; e13310. 10.1111/dth.13310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szepietowski JC, Matusiak Ł, Szepietowska M et al. Face mask‐induced itch: a self‐questionnaire study of 2,315 responders during the COVID‐19 pandemic. Acta Derm Venereol 2020; 100: adv00152. [DOI] [PMC free article] [PubMed] [Google Scholar]


