Abstract
The coronavirus disease 2019 (COVID-19) pandemic is a rapidly changing circumstance with dramatic policy changes and universal efforts to deal with the initial crisis and minimize its consequences. To identify changes to organ donation and transplantation during this time, an anonymous web-based survey was distributed to 19 select organ procurement organizations (OPOs) throughout the United States comparing 90-day activity during March-May 2020 and March-May 2019. Seventeen OPOs responded to the survey (response rate of 89.5%). Organ authorization decreased by 11% during the current pandemic (n = 1379 vs n = 1552, P = .0001). Organ recovery for transplantation fell by 17% (P = .0001) with a further 18% decrease in the number of organs transplanted (P = .0001). Donor cause of death demonstrated a 4.5% decline in trauma but a 35% increase in substance abuse cases during the COVID-19 period. All OPOs reported significant modifications in response to the pandemic, limiting the onsite presence of staff and transitioning to telephonic approaches for donor family correspondence. Organ donation during the current climate has seen significant changes and the long-term implications of such shifts remain unclear. These trends during the COVID-19 era warrant further investigation to address unmet needs, plan for a proportionate response to the virus and mitigate the collateral impact.
KEYWORDS: clinical research/ practice, donors and donation, health services and outcomes research, infection and infectious agents—viral, organ procurement and allocation, organ procurement organization, organ transplantation in general
Abbreviations: AOPO, Association of Organ Procurement Organizations; COVID-19, coronavirus disease 2019; DBD, donation after brain death; DCD, donation after cardiac death; DSA, designated service area; ECD, extended criteria donor; MVA, motor vehicle accident; OPO, organ procurement organization; OPTN, Organ Procurement and Transplantation Network; SARS, severe acute respiratory syndrome; SOT, solid organ transplant; UNOS, United Network for Organ Sharing
1. INTRODUCTION
When coronavirus disease 2019 (COVID-19) was first described in Wuhan, China, in December 2019, it was difficult to envisage the global pandemic that would later ensue and the direct and indirect impact this rapidly progressing disease would have on all health systems.1 In contrast to previous disease pandemics of more recent times, such as the Ebola virus, swine flu, and severe acute respiratory syndrome (SARS), all of which demonstrated a substantial lethality, the fallout of these diseases seems minimal compared to the current international crisis.2 Notwithstanding the collateral impact on economic and social constructs, the strain on global healthcare systems has been devastating with growing concerns regarding asymptomatic person-to-person transmission, infected healthcare workers, a lack of appropriate personal protective equipment (PPE), and ventilator shortages.3, 4, 5 The paucity of high-quality level-I evidence has consequently placed a reliance on institutional experiences, expert opinions, and small series from the international medical community.
All health services have had to reconfigure the way care is delivered to patients and their families and the implications for surgical services during the current outbreak and in the subsequent “post-pandemic” era are concerning and equally unclear.6, 7, 8, 9 Organ transplantation is an exemplar model of complex major surgery with an additional challenge of managing immunosuppressed patients and the constant scarcity of organs. Organ procurement organizations (OPOs) have had to adjust to this challenging time and the current and long-term impact are an important facet to consider. Moreover, the transplant community has been vocal about the potential consequences of COVID-19 on services and a radical need to implement policy changes, but no study has adequately provided a quantitative assessment of organ donation practices during this time.10 , 11
Most existing studies on transplantation and COVID-19 have approached recipient related issues and medication challenges at a transplant center-level, however, little is known about the impact on OPOs and the donor service. It may be that existing social distancing measures and health policy recommendations play a role in their functionality and, on the basis of previous observations in the surgical literature, we hypothesized that the current COVID-19 crisis may have affected donor volume, organ yield, and service activity.12, 13, 14 One important question to ask is how this pandemic has altered the process of organ donation and how long it could take to address a potentially growing waiting list. Herein, we report on a consecutive cohort of organ donors and recipients during 2 similar time frames to comprehensively describe the effects of a global pandemic on donation and transplantation services within the United States. Specifically, we hope to define and capture the clinical significance of this new virus on organ transplantation during the initial wave and peak phase and raise questions regarding the potential consequences of the COVID-19 pandemic through measured OPO parameters.
2. METHODS
2.1. Survey design
A questionnaire (Supplement 1) was designed using a combination of open-ended and multiple-choice questions via an online web-based tool (Survey Monkey, http://www.surveymonkey.com). The focus of the study was to compare 2 specific 90-day periods from March-May 2019 and March-May 2020 and determine the impact of the COVID-19 virus on the organ donation process in response to the implementation of stay-at-home orders including limited or absent hospital visitation privileges and new recommendations proposed by the United Network for Organ Sharing (UNOS) during this time. Survey questions were designed and approved through the collaborative leadership of the Department of Abdominal Organ Transplantation at Washington University/Barnes-Jewish Hospital and Mid-America Transplant to purposely assess changes in solid organ transplant (SOT) activity, specifically for heart, lung, liver, and kidney organ authorization; organ recovery; and decline. Donor cause of death was assessed by defining the circumstance of death in all trauma cases and specifying the mechanisms of death in head traumas. We adopted the same nomenclature utilized by UNOS and the Organ Procurement and Transplantation Network (OPTN) for ease of comprehension and dissemination by the included OPOs. The survey assessed rates of donation after brain (DBD) and cardiac death (DCD) separately, considering all OPOs apply the same criteria for death as outlined by OPTN.15 The rates of extended criteria donors (ECDs) during both periods were also captured, defined as donors aged 60 years or older or over 50 years with at least 2 of the following conditions: death following a cerebrovascular accident, a history of hypertension, or a serum creatinine > 1.5 mg/dL. In addition, OPOs were asked what institutional practice modifications were made to the organ donation process in response to the virus.
2.2. Study participants
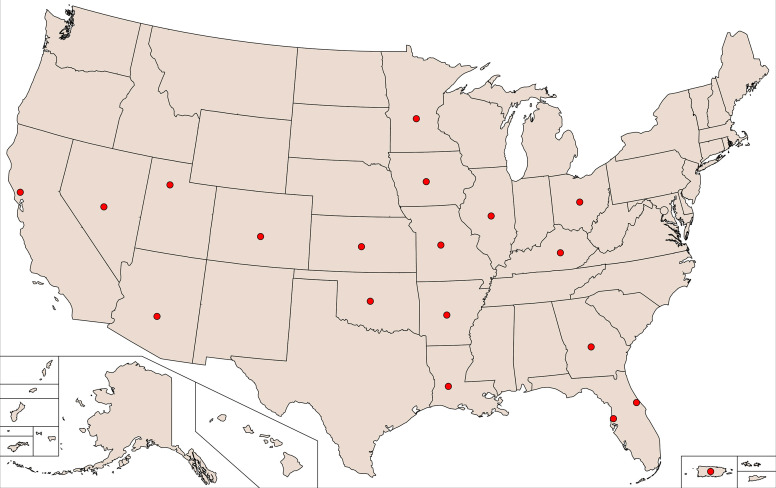
There are 58 OPOs in the United States and Puerto Rico, responsible for coordinating the donation process within their own designated service area (DSA).16 These DSAs may cover all or part of a state where an OPO will assess donor potential, convey relevant clinical information to transplant centers, and work closely with the deceased’s family to manage the authorization and donation process. The chief executive officer of the Association of Organ Procurement Organizations opened the survey to all 58 OPOs and the survey was distributed, via an email link, to 19 select OPOs who chose to submit their data capturing donor activity in midwestern, southern, and western states and Puerto Rico ( Figure 1). Specific OPO data were recorded by individual data collectors and procurement coordinators employed by OPOs. Responses were received by a central data supervisor who collated and subsequently reported data to the authors. Participation was voluntary with completion inferring informed consent. Compensation was not offered in exchange for participation.
FIGURE 1.
Locations of organ procurement organizations (OPOs) in the survey. Arkansas Regional Recovery Agency (AR); Nevada Donor Network (NV); Our Legacy (FL); Kentucky Organ Donor Affiliates (KY); Midwest Transplant Network (KS); Donor Network West (CA); Lifefeshare of Oklahoma (OK); Louisiana Organ Procurement Agency (LA); Donor Network of Arizona (AZ); Mid-America Transplant (MO); Donor Alliance (CO); LifeSource (MN); LifeBanc (OH); Gift of Hope (IL); LifeLink of Florida (FL); LifeLink of Georgia (GA); LifeLink of Puerto Rico; Iowa Donor Network (IA); Donor Connect (UT) [Color figure can be viewed at wileyonlinelibrary.com]
2.3. DATA collection
An email request with a link to the online survey was sent on April 15, May 1, and June 1, 2020 and participants were asked to complete data as comprehensively as possible. The survey was open for a 2-week period and email reminders to nonresponders were sent on day 10 to optimize the response.
2.4. DATA analysis
OPO responses were electronically recorded on a Microsoft Excel spreadsheet (Microsoft Corporation, Redmond, WA) and results were analyzed using GraphPad Prism 7 software (San Diego, CA) to compare events during the 2 study periods. Descriptive data are presented as absolute frequencies and percentages. Continuous variables are reported in mean (± SD) or median (range) values and compared using unpaired t tests. A significance level of 0.05 was used for all analyses and all P values are reported as 2 tailed.
3. RESULTS
A total of 17 OPOs responded to the survey with an overall response rate of 89.5%. All OPO responses were anonymized and no identifiable patient or OPO data was processed.
3.1. COVID-19 testing, donor authorization, and organ availability
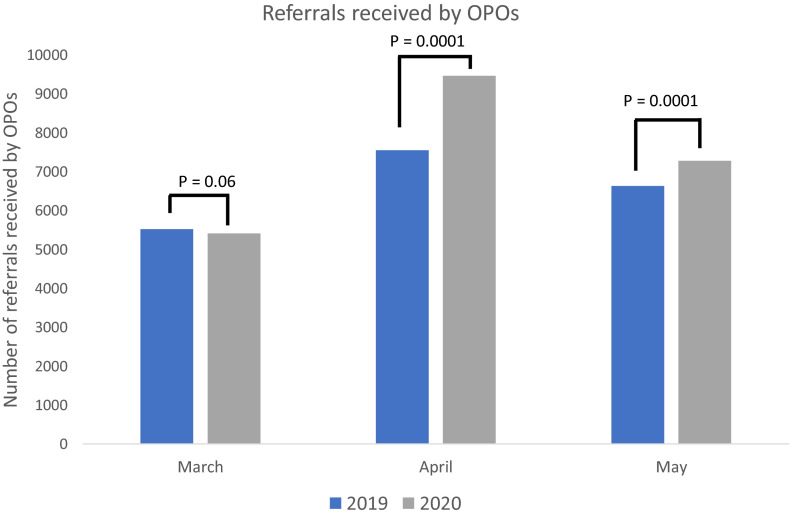
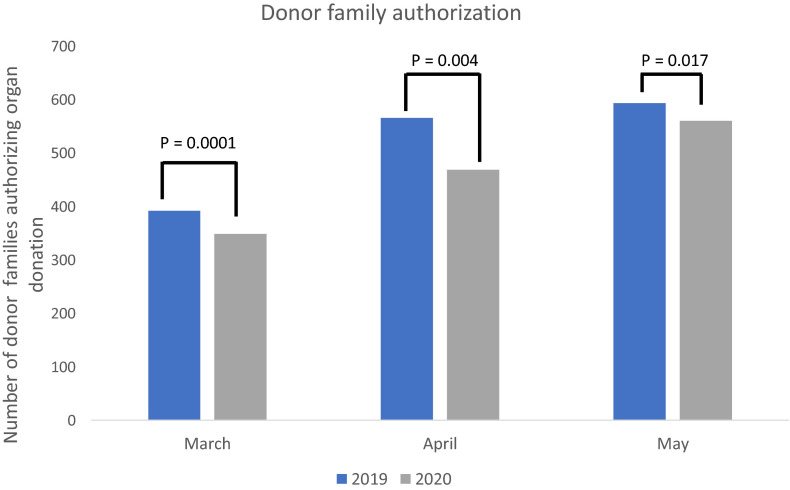
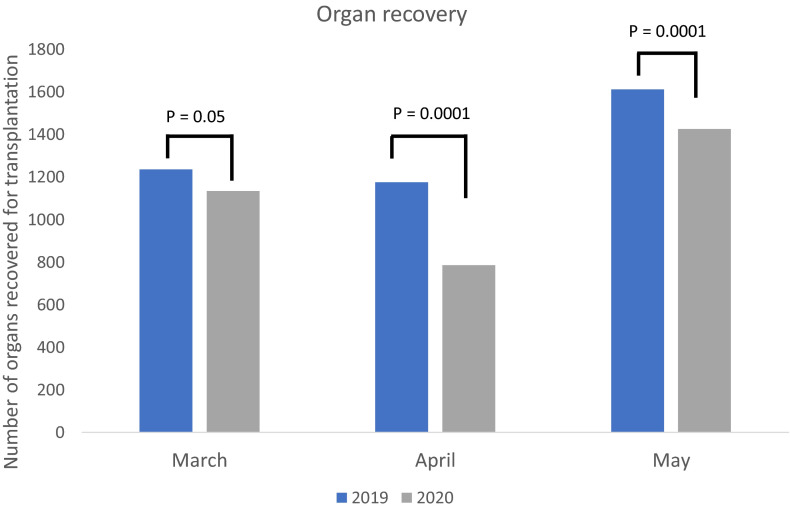
Individual OPOs were questioned on the number of organ referrals received from their own DSAs during the first 90-day period from March to May 2019 and second period from March to May 2020, with the latter period demonstrating a 12.4% increase in referral activity ( Table 1). The greatest difference was seen in the 2 corresponding April periods during which referrals increased by 25% in April 2020 (mean 445 ± 415 vs 557 ± 732, P = .0001) when compared to April 2019 ( Figure 2). COVID-19 testing was initially performed in only 170 (49%) potential organ donors in March 2020 but was extended to all potential donors by May 2020. Nasopharyngeal swabbing for nucleic acid testing was the most common diagnostic tool performed by 17 OPOs (100%) with additional confirmatory tests performed using bronchoalveolar lavage, oropharyngeal swab fluid analysis, and serum antibody testing by 7 (41%), 5 (29%) and 1 (6%) OPO, respectively. During March to May 2020, there was an 11% decrease in organ authorization by donor families when compared to the same 90-day period in 2019 (P = .0001). The sharpest decline was observed in the April data (April 2019 n = 566 vs April 2020 n = 469, P = .004) during which authorization rates decreased by 17% during the COVID-19 pandemic ( Figure 3). In addition, the total number of organs recovered for transplantation decreased by 17% during the 2020 study period (2019 n = 4021 vs 2020 n = 3344, P = .0001), presenting the most dramatic decline of 33% in organ recovery in April 2020 when compared to April 2019 (2019 mean 73 ±45 vs 2020 mean 49 ± 27, P = .0001) ( Figure 4).
TABLE 1.
OPO organ availability, authorization, and recovery
| March-May 2020 (n) | March-May 2019 (n) | P Value | |
|---|---|---|---|
| Referrals received by OPOs | 19724 | 22163 | .0001 |
| Donor families authorizing organ donation per OPO | 1379 | 1552 | |
| Organs recovered for transplant | 3344 | 4021 |
FIGURE 2.
Monthly trends in referral numbers received by studied organ procurement organizations (OPOs) during March to May 2019 and March to May 2020 [Color figure can be viewed at wileyonlinelibrary.com]
FIGURE 3.
Monthly trends in donor family authorization during March to May 2019 and March to May 2020 [Color figure can be viewed at wileyonlinelibrary.com]
FIGURE 4.
Monthly trends in organ recovery during March to May 2019 and March to May 2020 [Color figure can be viewed at wileyonlinelibrary.com]
3.2. Organ donation and transplantation
In total, 1162 and 953 organ donors were identified during the 2019 and 2020 study periods, a decline of 18% respectively (P = .0001). The total number of organs transplanted during the 90-day 2020 period fell by 18% (n = 2580 vs n = 3148 organs, P = .0001) when compared to the similar 90-day period in 2019. The greatest differences were reported in heart and lung transplantation ( Table 2). A decline in organ donation was apparent in the entire donor pool during 2020 when compared to 2019 (P = .0001), with lower rates of DCDs (12% decrease), DBDs (17% decrease), and ECDs (30% decrease). Overall organ discard declined by 11% during the current 2020 pandemic period (n = 452 vs n = 404, P = .0001).
TABLE 2.
Frequency of organ donation
| Percentage decline | March-May 2020 | March-May 2019 | P Value | |
|---|---|---|---|---|
| All organ transplantation (n) | 18% | 2580 | 3148 | .0001 |
| Solid organ transplantation (n) | .0001 | |||
| Heart | 24% | 247 | 324 | |
| Lung | 27% | 310 | 424 | |
| Liver | 19% | 603 | 748 | |
| Kidney | 15% | 1299 | 1522 | |
| Donor type (n) | .0001 | |||
| Donation after brain death | 17% | 629 | 758 | |
| Donation after cardiac death | 12% | 202 | 230 | |
| Extended criteria donor | 30% | 122 | 174 |
3.3. Donor cause of death and organ retrieval
Cause of death analysis demonstrated a 5% reduction in donor death by trauma (P = .03) during the 2020 study period compared to the similar 2019 period. Donor death by substance abuse increased significantly by 35% during the current pandemic period compared to 2019 study data. The overall changes in donor cause of death are detailed in Table 3 (Supplementary files 2 and 3).
TABLE 3.
Donor cause of death reported by OPOs
| Percentage decline | March-May 2020 (n) | March-May 2019 (n) | P value | |
|---|---|---|---|---|
| Trauma | 4.5% | 382 | 400 | .03 |
| Homicide | 14% increase | 66 | 58 | .11 |
| Suicide | 11% | 142 | 159 | .03 |
| Blunt injuries | 13% | 212 | 244 | .0001 |
| MVA | 25% | 144 | 193 | .0001 |
| GSW | 4.5% increase | 116 | 111 | .35 |
| CVA | 9% | 444 | 488 | .0001 |
| Substance abuse | 35% increase | 220 | 163 | .0001 |
| Natural causes | 1.7% | 2071 | 2106 | .31 |
| CNS tumor/seizure | 43% | 12 | 21 | .0001 |
| Anoxia | 0.7% | 968 | 975 | .69 |
Abbreviations: CNS, central nervous system; CVA, cerebrovascular accident; GSW, gunshot wound; MVA, motor vehicle accident; OPO, organ procurement organization.
Changes in organ recovery by transplant teams are described in Table 4. Out-of-town and local team recovery of organs decreased by 20% and 16% during the 2020 study period (P = .0001).
TABLE 4.
Organ recovery by transplant teams
| Percentage decline | March-May 2020 (n) | March-May 2019 (n) | P Value | |
|---|---|---|---|---|
| Local-team recovery | ||||
| Heart | 44% | 67 | 120 | .0001 |
| Lung | 20% | 84 | 105 | |
| Liver | 22% | 448 | 574 | |
| Kidney | 8% | 808 | 878 | |
| Out-of-town team recovery | ||||
| Heart | 16% | 166 | 197 | .0001 |
| Lung | 34% | 120 | 182 | |
| Liver | 13% | 158 | 181 | .0005 |
| Kidney | 17% | 125 | 151 | .0001 |
3.4. OPO policy changes
OPOs were questioned about institutional modifications made in response to the COVID-19 pandemic. All OPOs began limiting the onsite presence of staff in March 2020. During this time, 11 OPOs reported an increase in remote referral responses and donor management and 8 OPOs withdrew from all onsite interactions unless donor brain death was confirmed. One OPO initiated live video streaming of organ recovery for all out-of-state teams during March 2020 which continued throughout May. Seven OPOs reported either increasing or completely converting to virtual and telephonic approaches for donor family authorization in March 2020 and initial family contact was made by telephone for 18% of potential donors. By May 2020, 8 additional OPOs employed virtual and telephonic approaches for donor family authorization and initial family contact by telephone increased to 40% of donors. Two OPOs introduced narrower donor criteria in March 2020, with 1 OPO specifically excluding DCD cases over 50 years or “marginal” DBDs. By May 2020, 2 additional OPOs decreased the upper age limit for DCDs from 70 to 65 years.
4. DISCUSSION
In the modern era, most practice guidelines are heavily supported by concrete scientific and clinical research. In current times, however, the rapidly changing landscape of a global pandemic has resulted in immediate health reform as all disciplines attempt to prepare for a proportionate response to the COVID-19 virus. In the context of surgery, elective procedures saw an immediate halt and a “surgery-only-if needed” philosophy was adopted by most units for cases where timely interventions can significantly alter outcomes.17 These are truly laudable efforts during an unprecedented time and, consequently, the collateral impact of COVID-19 is perhaps best measured by studying the influence on individual services rather than considering a monolithic medical or surgical community. Organ transplantation is a highly specialized field offering the only therapeutic option for terminal organ failure. Given the rising number of cases and lack of an approved, licensed treatment for COVID-19 at present, the transplant community has seen key policy changes and expert recommendations in a short period of time.11 , 18 , 19
The results of this study raise some important issues in relation to donation practices during the current viral pandemic and comprehensively report a stark decline in organ donation and transplantation from an OPO perspective. Several reports have both predicted and established a dramatic change to transplant services during the initial crisis and our study primarily aimed to explore this apparent anomaly by considering the collateral influence on organ donation.20, 21, 22 In this context, and at a time of focus on real-time information and quantitative measures of impact, our findings provide novel data captured by nearly one third of OPOs throughout the United States and Puerto Rico, and highlight some of the challenges faced by the transplant community during this time.
The current study found a 17% decline in organ recovery rates between 2 similar 90-day time frames in 2020 and 2019 and, consequently, an 18% decrease in the number of transplanted organs. As with all observational data, direct causality testing is challenging and the reasons for this disparity are likely multifactorial with several elements underpinning these phenomena. The conventional explanation for our findings would be that some transplant centers are prioritizing and transplanting only extremely sick patients, particularly at the height of the pandemic in April 2020, because of health resource limitation during an unpredictable time. An alternative explanation could be that social distancing restrictions and changes in the cause of death landscape, specifically in the number of motor vehicle accidents and violent crimes as seen in our results, which often yield the most suitable donors, have reduced the overall donor pool and limited organ availability. This could be consistent with our findings in which we also demonstrate an overall decline in DBDs, DCDs, and ECDs. However, and notwithstanding the dramatic decline in overall organ donation and transplantation activity, the frequency of organ donors following substance abuse during the 2020 study period is substantial, an increase of 35% (2020 vs 2019; n = 220 vs n = 163, P = .0001). Whether this is directly attributed to the COVID-19 pandemic is unclear and the current crisis may only be a lens through which we are now viewing preexisting social and economic constraints on population health and the delivery of care, which both warrant further examination.
One unique aspect to our study is our analysis of donor authorization rates and OPO interactions with donor families. In our study, organ authorization decreased by 11% between the 2 study periods. Furthermore, several OPOs cite limited onsite interactions and increased telephonic approaches with donor families for both initial contact and follow-up correspondences. It may be a plausible thesis that the shift from a visible onsite presence by OPOs and meaningful face-to-face consultations has affected the family consent process. In addition, several units have issued policies limiting family visits to hospitals and the added quarantine rules may have resulted in missed opportunities to discuss the organ donation process with trained personnel. Recent evidence also suggests that public misinformation and speculation about the COVID-19 virus have led to a great deal of fear, anxiety, and significant psychosocial implications.23, 24, 25 In such instances, the overwhelming negative perceptions and fear of contracting the infection through hospital contact may also explain the reduced engagement of families with OPO and hospital staff. From a patient perspective, part of the challenge could be to rebuild public confidence in engaging with OPO staff and guaranteeing the safety of families in not contracting the virus through health-worker interaction. One OPO reported live video streams of donor procurement by out-of-state teams, an innovative modification in current times. Some theorists argue that, based on historical trends, global pandemics may accelerate changes already underway rather than completely shift the direction of preexisting practices.26 , 27 This is currently evident as health systems now adopt to virtual consultations and sophisticated screening and surveillance technology. However, the approach of “contactless” patient interactions, specifically as it applies to organ donation and the fundamental characteristics of face-to-face family authorization may expose existing fault lines in this method and complicate the organ donation process, an observation that can be interpreted from our analysis.
Global health services are operating in a rapidly changing circumstance. The basis of the shutdown, physical distancing, and ever-evolving health policies was and remains justifiable. Understanding the extent of the work that has been deferred and affected by the pandemic over the past 3 months merits further consideration and, from a transplant perspective, the effects on wait-list times and subsequent morbidity are unclear. Moreover, if the downward trend in donation practices is sustained, the unmet needs of patients awaiting transplantation are a cause for concern and warrant careful health policy and capacity planning to prepare for the potential consequences.
This study has some limitations. Recent changes in donor organ allocation strategies and recalibrating geographic boundaries historically considered by DSAs may explain some of the discrepancies between the 2 studied periods. In addition, our results reflect the experiences of 17 OPOs and may generate a potential selection bias, especially since we provide no information from the northeast. Despite these limitations, we include responses from several regions and a wide spectrum of the population to minimize these influences. Our findings suggest that the examination of additional OPO experiences should be considered to, not only determine the changes in organ donation activity but also map the nationwide imbalance of COVID-19 cases and its proportionate impact on individual systems.
5. CONCLUSION
This study has a broad scope, including a brief analysis on organ donation practices at a national level to reflect the changes incurred by COVID-19 by comparing 2 similar time periods. Data integrity is high and maintained by OPOs in real time through regular auditing to create a national patient registry of potential organ donors. As such, the study primarily aimed to explore the collateral impact of the virus on an important aspect of the transplantation process, not only through institutional counts but also by exploring the changing demographics of patient deaths. The causes of the stark decline in organ donation are complex and a potential change in patient and family authorization dynamics coupled with OPO adjustments during this time are key elements underlying these observations. Larger studies are required across the national and international consortia to further quantify the current and prospective impact of the COVID-19 pandemic on organ transplantation, waitlist structures, and associated patient morbidity. In addition, detailed population-projection models with practical applications are needed and the authors welcome work towards this objective through collaboration with public health specialists to anticipate and strategically plan for the full restoration of services and how healthcare delivery should adjust in the post-pandemic era.
ACKNOWLEDGMENTS
We wish to thank all survey respondents for their contribution and timely responses to the study.
DISCLOSURE
The authors of this manuscript have no conflicts of interest to disclose as described by the American Journal of Transplantation.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
SUPPORTING INFORMATION
Additional supporting information may be found online in the Supporting Information section.
File S1
File S2
File S3
REFERENCES
- 1.Wang C, Horby PW, Hayden FG, et al. A novel coronavirus outbreak of global health concern. The Lancet. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lai C-C, Shih T-P, Ko W-C, et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. 2020;55(3):105924. doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rowan NJ, Laffey JG. Challenges and solutions for addressing critical shortage of supply chain for personal and protective equipment (PPE) arising from Coronavirus disease (COVID19) pandemic - Case study from the Republic of Ireland. Sci Total Environ. 2020;725:138532. doi: 10.1016/j.scitotenv.2020.138532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clarke AL, et al. Coping with COVID-19: ventilator splitting with differential driving pressures using standard hospital equipment. Anaesthesia. 2020;75(7):872–880. doi: 10.1111/anae.15078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bai Y, Yao L, Wei T, et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020;323(14):1406. doi: 10.1001/jama.2020.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Massey PA, McClary K, Zhang AS, et al. Orthopaedic surgical selection and inpatient paradigms during the coronavirus COVID-19 pandemic. J Am Acad Orthop Surg. 2020;28(11):436–450. doi: 10.5435/JAAOS-D-20-00360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Coimbra R, Edwards S, Kurihara H, et al. European Society of Trauma and Emergency Surgery (ESTES) recommendations for trauma and emergency surgery preparation during times of COVID-19 infection. Eur J Trauma Emerg Surg. 2020;46(3):505–510. doi: 10.1007/s00068-020-01364-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zarrintan S. Surgical operations during the COVID-19 outbreak: Should elective surgeries be suspended? Int J Surg. 2020;78:5–6. doi: 10.1016/j.ijsu.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yeo D, et al. COVID-19 & the general surgical department - measures to reduce spread of SARS-COV-2 among surgeons. Ann Surg. 2020;272(1):e3–e4. doi: 10.1097/SLA.0000000000003957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Halazun KJ, Rosenblatt R. Lest we forget. Am J Transplant. 2020;20(7):1785–1786. doi: 10.1111/ajt.15888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wall AE, Pruett T, Stock P, et al. Coronavirus disease 2019: Utilizing an ethical framework for rationing absolutely scarce healthcare resources in transplant allocation decisions [published online ahead of print 2020]. Am J Transplant. 2020; 10.1111/ajt.15914 [DOI] [PMC free article] [PubMed]
- 12.Iacobucci G. Covid-19: all non-urgent elective surgery is suspended for at least three months in England. BMJ. 2020;368:m1106. doi: 10.1136/bmj.m1106. [DOI] [PubMed] [Google Scholar]
- 13.Diaz A, Sarac BA, Schoenbrunner AR, et al. Elective surgery in the time of COVID-19. Am J Surgery. 2020;219(6):900–902. doi: 10.1016/j.amjsurg.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Vries APJ, et al. Immediate impact of COVID-19 on transplant activity in the Netherlands. Transpl Immunol. 2020;61:101304. doi: 10.1016/j.trim.2020.101304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Steinbrook R. Organ donation after cardiac death. N Engl J Med. 2007;357(3):209. doi: 10.1056/NEJMp078066. [DOI] [PubMed] [Google Scholar]
- 16.Sharing U.N.f.O. Organ Procurement organizations. 2020 [cited 2020 05/08/2020]; Available from: https://unos.org/transplant/opos-increasing-organ-donation/
- 17.Brindle M, Gawande A. Managing COVID-19 in surgical systems. Annals of Surgery, 9000. 2020;272(1):e1–e2. doi: 10.1097/SLA.0000000000003923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boyarsky BJ, Po-Yu Chiang T, Werbel WA, et al. Early Impact of COVID-19 on transplant center practices and policies in the United States. Am J Transplant. 2020;20(7):1809–1818. doi: 10.1111/ajt.15915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.OPTN. Covid-19 emergency policy package 2020, Organ Procurement and Transplantation Network. Richmond Virginia.
- 20.Agopian V, Verna E, Goldberg D. Changes in liver transplant center practice in response to COVID-19: Unmasking dramatic center-level variability. Liver Transpl. 2020;26(8):1052–1055. doi: 10.1002/lt.25789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shah MB, et al. Utilization of deceased donors during a pandemic: an argument against using SARS-CoV-2 positive donors. Am J Transplant. 2020;20(7):1795–1799. doi: 10.1111/ajt.15969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Woolley AE, Mehra MR. Dilemma of organ donation in transplantation and the COVID-19 pandemic. J Heart and Lung Transplant. 2020;39(5):410–411. doi: 10.1016/j.healun.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lin C-Y. Social reaction toward the 2019 novel coronavirus (COVID-19) Social Health and Behavior. 2020;3(1):1–2. [Google Scholar]
- 24.Pakpour A, Griffiths M. The fear of COVID-19 and its role in preventive behaviors. J Concurrent Disorders. 2020;2:58–63. [Google Scholar]
- 25.Sohrabi C, Alsafi Z, O’Neill N, et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int J Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.He H, Harris L. The impact of Covid-19 pandemic on corporate social responsibility and marketing philosophy. J Business Res. 2020;116:176–182. doi: 10.1016/j.jbusres.2020.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Allen J, et al. How the world will look after the coronavirus pandemic. Foreign Policy. 2020. https://foreignpolicy.com/2020/03/20/world-order-after-coroanvirus-pandemic/. Accessed June 21, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
File S1
File S2
File S3
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.