Abstract
Objective
To determine if changes to community‐based services have effected paediatric ED attendances for mental health issues and neonates during the COVID‐19 pandemic.
Methods
Analysis of total presentations, presentations with a mental health diagnoses and presentation of neonates during the early stages of the pandemic compared with the previous year for four Victorian hospitals.
Results
There was a 47.2% decrease in total presentations compared with 2019, with a 35% increase in mental health diagnoses and a 2% increase in neonatal presentations.
Conclusion
Vulnerable paediatric patients are seeking care elsewhere during the pandemic because of the closure of community services.
Keywords: delivery of healthcare, paediatric emergency medicine, pandemics
International data suggest a decrease in paediatric ED usage during the COVID‐19 pandemic. 1 , 2 However, with the closure of some community services, it is possible that some vulnerable groups have no alternative but to seek care in the ED. In Victoria, community child/adolescent mental health services and maternal and child health services have reduced their face‐to‐face sessions to promote social distancing, 3 , 4 yet care for some of the most vulnerable children in our community.
To determine if changes to community‐based services have affected ED attendances, we analysed presentations of patients <18 years during the early stages of the pandemic to two tertiary hospitals (Royal Children's Hospital [RCH] and Monash Medical Centre) and two urban district hospitals (Dandenong and Casey). The research was assessed as not requiring full ethical approval by the Human Research Ethics Committees of both the RCH and Monash Health.
The Australian government announced the closure of borders to non‐residents on 20 March 2020. When comparing the 2‐month period after this to the same period in 2019, there is a 47.2% decrease in total presentations (26 871 vs 14 170), with a significant difference in daily means (440.5 vs 232.3, difference −208.2, 95% confidence interval [CI] −221.7 to −194.7, P < 0.001). Conversely, there was a 35% (485 vs 656) increase in mental health patients (daily means 8.0 vs 10.8, difference 2.8, 95% CI 1.7–3.9, P < 0.001), while neonatal presentations did not change significantly (2% increase, 498 vs 507; daily means 8.2 vs 8.3, difference 0.1, 95% CI −0.8 to 1.1, P = 0.754).
Figure 1 demonstrates a dramatic reduction in overall paediatric presentations to the four EDs in 2020 during the COVID‐19 pandemic. Presentations for children with mental health diagnoses (ICD‐10 F codes) and neonates (<28 days old) did not decrease.
Figure 1.
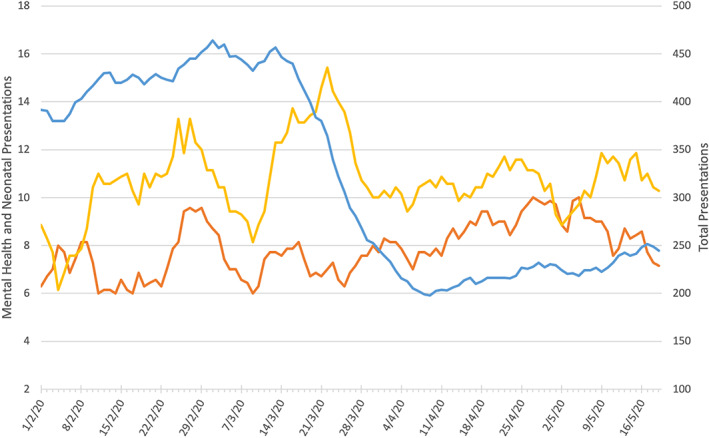
Seven‐day rolling average, number of presentations (age <18 years). ( ) Neonatal (<28 days); (
) Neonatal (<28 days); ( ) mental health; (
) mental health; ( ) total.
) total.
For RCH alone there was a 25% increase in neonatal presentations (270 vs 240; daily mean 4.4 vs 5.6, difference 1.1, 95% CI 0.5–1.8, P < 0.001). Local municipalities surrounding RCH have more strictly curtailed face‐to‐face visits compared with those around the other sites (L. Gawler, Maternal and Child Health Nurse, RCH, pers. comm. 10 June 2020).
The numbers of mental health and neonatal presentations are small, but they have not decreased in line with other presentations. A proportion of these vulnerable patients are seeking care elsewhere, which raises the possibility that some of them are not having their needs met. Currently in Victoria there is no plan to compel access to face to face community consultations for these groups of patients.
We suggest that community care for vulnerable patient groups is an essential health service, and face‐to‐face access during the COVID‐19 pandemic or any future pandemics should continue (with appropriate patient screening and use of personal protective equipment). If not, families may be forced to seek acute care in the ED, which is neither ideal for families nor without cost implications, and in the event of increased community transmission may represent a greater risk.
Author contributions
JAC and HH conceived the study. JAC and SSC obtained and analysed the data. JAC, SSC, AW, SL and HH provided significant contribution to the final manuscript. JAC takes responsibility for the article as a whole.
Competing interests
SSC is a section editor for Emergency Medicine Australasia.
John A Cheek, MBBS, FACEM, Deputy Director Emergency Medicine, Honorary Senior Fellow; Simon S Craig, MBBS, MHPE, MPH, FACEM, Emergency Physician, Adjunct Clinical Professor; Adam West, MBBS, MHSM, DRANZCOG, FACEM, Director Paediatric Emergency; Stuart Lewena, MBBS, BMedSci, FRACP, Director Emergency Medicine; Harriet Hiscock, MBBS, FRACP, Principle Fellow, Paediatrician.
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- 1. Isba R, Edge R, Jenner R, Broughton E, Francis N, Butler J. Where have all the children gone? Decreases in paediatric emergency department attendances at the start of the COVID‐19 pandemic of 2020. Arch. Dis. Child. 2020; 105: 704. [DOI] [PubMed] [Google Scholar]
- 2. Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID‐19. Lancet Child Adolesc. Health 2020; 4: e10–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Orygen Youth Health. Responding to the COVID‐19 Outbreak. [Cited 10 Jun 2020.] Available from URL: https://www.orygen.org.au/About/Responding-to-the-COVID-19-outbreak
- 4. Department of Health and Human Services . COVID‐19 Update Maternal and Child Health Services. [Cited 10 Jun 2020.] Available from URL: https://fac.dhhs.vic.gov.au/sites/default/files/2020-03/COVID%20-19%20update%20for%20Maternal%20and%20Child%20Health%20Services.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


