Abstract
Background
Inconsistencies regarding the use of appropriate personal protective equipment (PPE) have raised concerns for the safety of surgical staff during the coronavirus disease 2019 (COVID‐19) pandemic. This rapid review synthesizes the literature and includes input from clinical experts to provide evidence‐based guidance for surgical services.
Methods
The rapid review comprised of targeted searches in PubMed and grey literature. Pertinent findings were discussed by a working group of clinical experts, and consensus recommendations, consistent with Australian and New Zealand Government guidelines, were formulated.
Results
There was a paucity of high‐quality primary studies specifically investigating appropriate surgical PPE for healthcare workers treating patients possibly infected with COVID‐19. SARS‐CoV‐2 is capable of aerosol, droplet and fomite transmission, making it essential to augment standard infection control measures with appropriate PPE, especially during surgical emergencies and aerosol‐generating procedures. All biological material should be treated a potential source of SARS‐COV‐2. Staff must have formal training in the use of PPE and should be supervised by a colleague during donning and doffing. Patients with suspected or confirmed COVID‐19 should wear a surgical mask during transfer to and from theatre. Potential solutions exist in the literature to extend the use of surgical P2/N95 respirators in situations of limited supply.
Conclusion
PPE is advised for all high‐risk procedures and when a patient's COVID‐19 status is unknown. Surgical departments should facilitate staggered rostering, remote meeting attendance, and self‐isolation of symptomatic staff. Vulnerable surgical staff should be identified and excluded from operations with a high risk of COVID‐19 infection.
Keywords: COVID‐19, healthcare worker, personal protective equipment, SARS‐CoV‐2, surgery
Inconsistencies regarding the use of appropriate personal protective equipment have raised concerns for the safety of surgical staff during the coronavirus disease 2019 pandemic. This rapid review synthesises the literature that includes input from clinical experts to provide evidence‐based guidance for surgical services.
Introduction
Coronavirus disease 2019 (COVID‐19) was first identified in December 2019 in the city of Wuhan, China, 1 and rapidly developed into a global pandemic. 2 The novel human coronavirus responsible has since been named severe acute respiratory syndrome coronavirus‐2 (SARS‐CoV‐2). 3
SARS‐CoV‐2 particles are spherical, with a diameter of 60–140 nm. 4 The virus is capable of aerosol, droplet and fomite transmission, and, depending on the inoculum shed, can remain viable in aerosols for up to 3 h and on surfaces for up to 3 days. 5 Asymptomatic carriers of COVID‐19 6 can create substantial undocumented infection, facilitating rapid human‐to‐human transmission and geographical spread. 7 Given its size, multiple modes of transmission and ease of transmission, standard infection control measures against SARS‐CoV‐2, while still necessary, are inadequate for preventing its spread, especially within healthcare settings.
Healthcare workers (HCWs) are at significant risk of COVID‐19 infection, 8 , 9 , 10 however, the correct use of personal protective equipment (PPE) will mitigate this risk. 11 Appropriate PPE is especially important in surgical care, where the potential exposure to biohazardous material places staff at a significant risk of contracting infectious diseases from patients. 12 , 13 , 14
PPE comprises a variety of garments or other safety equipment worn for the protection of HCWs, including disposable gowns, aprons, gloves, face shields, goggles, outer foot coverings, head coverings, surgical masks, filtering facepiece respirators (FFRs) and powered air‐purifying respirators. 15 However, PPE is only effective if used correctly and appropriately. This was demonstrated in the 2003 severe acute respiratory syndrome virus (SARS) outbreak, where improper or inconsistent use of PPE was significantly associated with HCW SARS infection. 16 , 17 , 18 , 19
This rapid review aims to provide evidence‐based guidance on the appropriate use of PPE for the safety of surgical staff.
Methods
The working group responsible for this evidence‐based guidance consisted of expert general surgeons, with additional advice from representatives from three specialty colleges and one surgical association within Australia and New Zealand.
Royal Australasian College of Surgeons researchers affiliated with the Australian Safety and Efficacy Register of New Interventional Procedures – Surgical, and Research, Audit and Academic Surgery conducted a rapid review of the literature, 20 , 21 , 22 consisting of targeted searches of the PubMed database and grey literature. Collation of evidence, literature review and in‐depth discussions with the working group members produced consensus recommendations on PPE 23 in harmony with the Australian and New Zealand Government Departments of Health's PPE guidelines.
Results and discussion
At the time of this publication, the epidemiology of COVID‐19 is still unclear. 24 , 25 The use of PPE is situational and influenced by jurisdiction and access to medical resources. As such, the recommendations developed here (Table 1) consider the variability within different clinical situations, the supply of and access to PPE, and the COVID‐19 status of the surgical patient being treated. Individual surgical teams may adapt this guidance to suit their clinical and resource environments.
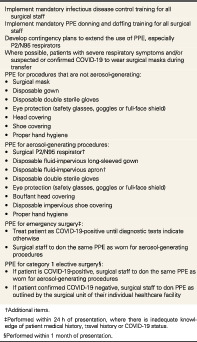
Table 1.
Recommendations from the working group on personal protective equipment (PPE) for surgical staff during COVID‐19 (5 May 2020) 26
| Implement mandatory infectious disease control training for all surgical staff |
| Implement mandatory PPE donning and doffing training for all surgical staff |
| Develop contingency plans to extend the use of PPE, especially P2/N95 respirators |
| Where possible, patients with severe respiratory symptoms and/or suspected or confirmed COVID‐19 to wear surgical masks during transfer |
PPE for procedures that are not aerosol‐generating:
|
| PPE for aerosol‐generating procedures: |
PPE for emergency surgery‡:
|
PPE for category 1 elective surgery§:
|
Additional items.
Performed within 24 h of presentation, where there is inadequate knowledge of patient medical history, travel history or COVID‐19 status.
Performed within 1 month of presentation.
For individual healthcare centres within Australia, it is recommended that the advice on PPE provided in this publication is supplemented with that issued by the Australian Government Department of Health. 27 Similarly, healthcare centres within New Zealand should also refer to the Ministry of Health, New Zealand, for guidance. 28
Biodistribution of COVID‐19
Several small observational studies have demonstrated the presence of SARS‐CoV‐2 viral particles in various organ systems. A study of 205 COVID‐19 patients by Wang et al., 29 investigated the biodistribution of SARS‐CoV‐2 RNA using real‐time reverse transcription‐polymerase chain reaction (RT‐PCR). They reported that bronchoalveolar lavage fluid showed the highest positive rates, followed by sputum, nasal swabs, fibrobronchoscope brush biopsy, pharyngeal swabs, faeces and blood, but it was not detected in urine specimens. Stool samples from four patients with high viral RNA loads were cultured and subjected to scanning electron microscopy and live SARS‐CoV‐2 particles were found in two of the four samples. It was noted that these two viral‐positive patients did not have diarrhoea. Similarly, Xiao et al., 30 found infectious virus isolated from faeces and gastrointestinal epithelial cells that stained positive for the nucleocapsid protein of SARS‐CoV‐2. The virus continued to be detected from faeces of 20% of patients testing negative for viral RNA in the respiratory tract post‐infection. The current evidence indicates that all biological material should be treated as a potential source of SARS‐CoV‐2, and surgical staff should take precautionary measures when donning (putting on) and doffing (removing) PPE.
COVID‐19 testing and PPE
The literature reporting different testing methods for COVID‐19 is still embryonic, as many modalities are still being refined. 31 The most common diagnostic test to date has been by RT‐PCR, which detects SARS‐CoV‐2 RNA in clinical samples. 32 , 33 It is a rapid diagnostic test that can be implemented on a large scale; however, a recent review by Lippi et al. found that, mainly due to patients being tested while in the early stages of disease progression (and therefore expressing low viral loads), the RT‐PCR test may report false negatives at a rate as high as 30%. 34 Due to this element of uncertainty, it is inadvisable to rely solely on RT‐PCR confirmation of COVID‐19 when directing the use of PPE.
Safe practices for protecting surgical departments during COVID‐19
There is a dearth of primary evidence investigating the education of surgical staff on safe practices to prevent the spread of COVID‐19. The importance of timely staff education and training was seen in the 2003 Hong Kong outbreak of SARS, the human coronavirus most closely related to that responsible for COVID‐19. 5 , 35 , 36 , 37 According to recent guidance from the World Health Organization, the most effective preventive measures that surgical staff can take during the COVID‐19 pandemic include maintaining at least 1 m of physical distance from others, performing frequent hand hygiene with an alcohol‐based hand rub, avoiding touching their eyes, nose and mouth, practising respiratory hygiene, wearing a surgical mask if symptomatic and routinely disinfecting frequently touched surfaces. 15
In surgical care, a confirmed case of a staff member with COVID‐19 could severely compromise, if not paralyse, a department's services for 2 weeks or more. Hence, the number of surgical staff present within a healthcare facility should be minimized wherever possible. Allocating surgical staff to alternating ‘teams’ for staggered attendance within each department could prevent care from being adversely impacted in such a situation. 38 If any surgical staff member were to display any symptoms suspicious of COVID‐19, the staff member and all exposed contacts must self‐isolate according to both local and national guidelines. 39
Where possible, teleconferencing and virtual meetings are practical means to replace in‐person meetings.
Identification of vulnerable surgical staff
Multiple large‐scale COVID‐19 population‐based data analyses have highlighted the need to identify vulnerable surgical staff and ensure their safety during the pandemic. Reports from China 8 and Italy 9 have demonstrated that the case‐fatality rate amongst COVID‐19 patients is significantly greater in those over 70 years of age. Individuals with chronic conditions or those immunocompromised are especially vulnerable. 8 For their own safety, surgical staff within any of these high‐risk groups should not be involved in high‐risk operations on patients who could potentially transmit the disease, especially those involving aerosol‐generating procedures (Table 2).
Table 2.
Aerosol‐generating procedures (Sources: Australian and New Zealand College of Anaesthetists 40 and Australian Government 41 )
| Aerosol‐generating procedures |
|
| High‐risk procedural aerosol‐generating procedures |
|
| High‐risk surgical aerosol‐generating procedures |
|
Education for correct ‘donning’ and ‘doffing’ of PPE
In order to minimize the spread of COVID‐19, formal education and training on proper procedures for donning and doffing PPE must be provided to all surgical staff, regardless of prior experience. Correct donning and doffing of PPE is crucial to ensuring the safety of surgical staff and patients. Deviations from accepted protocols and the practise of improper sequences frequently results in self‐contamination 42 , 43 , 44 and can significantly increase the risk of nosocomial SARS‐CoV‐2 infection. The Australian Commission for Safety and Quality in Healthcare and the Centers for Disease Control and Prevention in the USA are just two of many organizations that have adopted the responsibility of outlining sequences of correctly donning and doffing PPE for non‐sterile patient encounters. 45 , 46 , 47
Donning and doffing of PPE before and after operating on potential COVID‐19‐positive patients
High‐risk situations where full PPE is required for surgery due to potential COVID‐19 exposure, are outlined in Table 2. Donning and doffing of PPE must be carried out in a controlled and methodical fashion, especially during surgical emergencies where the risks of contamination and infection of surgical staff are greater. 48 There are currently no peer‐reviewed publications that outline a validated sequence of donning and doffing PPE specifically for surgery on patients who are potentially COVID‐19 positive.
Table 3 outlines a sequence of donning and doffing PPE for performing sterile surgical procedures on patients with potential COVID‐19 infection, which has been adapted from multiple sources. 45 , 46 , 47 , 49 This may be modified to suit the protocols of individual healthcare facilities. Ideally, another trained staff member should supervise the entire donning and doffing procedure to ensure that each step is carried out correctly. 42 , 51
Table 3.
Sequence of donning and doffing personal protective equipment (PPE) for operating on patients with potential COVID‐19 infection (Adapted from multiple sources 45 , 46 , 47 , 49 )
| Sequence of donning PPE before surgery | Sequence of doffing PPE after surgery |
|---|---|
|
|
Aerosol‐generating procedures
The possible exposure to SARS‐CoV‐2 viral particles during aerosol‐generating procedures is a potential risk to surgical staff. During the current pandemic, surgical and perioperative medical colleges, societies and associations have provided guidance on potential aerosol‐generating procedures (including those within surgical operations), for example, the recent statement from the Australian and New Zealand College of Anaesthetists (Table 2). 40
Surgical masks
Standard surgical masks are loose‐fitting, single‐use items that cover the nose and mouth. They are used as part of standard droplet‐infection precautions to protect against splashes and sprays, including the respiratory secretions of patients.
There are three levels of barrier protection provided by surgical masks, which can be utilized depending on the situational risk of exposure to droplets and biological material. 52 However, standard surgical masks do not provide a seal around the face and thus are inferior to FFRs in protecting against airborne respiratory infections. This has been demonstrated in multiple randomized controlled trials of large sample size. 53 , 54 , 55 Given that SARS‐CoV‐2 is viable in aerosols, 5 standard surgical masks do not provide adequate protection for COVID‐19. However, surgical masks offer a degree of infection control barrier when worn by coughing patients, they can limit the potential dissemination of infectious respiratory secretions. 46 , 56 Such use can be advocated when transporting surgical patients to and from the operating theatre as a method of infection control. 57
Surgical P2 and N95 FFRs
Evidence validating the use of surgical P2/N95 respirators is dominated by small, laboratory‐based studies. However, because standard surgical masks fail to provide adequate protection for the aerosol transmission of SARS‐CoV‐2, surgical P2/N95 respirators protecting against viral particles should be used. 15 A good facial fit that minimizes aerosol contact with the mucous membranes of the nose and mouth is the key to their design and use. These respirators consist of four to five layers of material, providing filtration through both mechanical impaction and electrostatic capture. 46 They can be used as part of airborne precautions during COVID‐19.
While the terms ‘P2 respirator’ and ‘N95 respirator’ are often used interchangeably in the healthcare setting, they are required to meet different national standards. In Australia and New Zealand, the requirements for P2 respirators (Australian/New Zealand Standards 1716: 2012 58 and 1715: 2009 59 ) include a filter efficiency of at least 94% in standardized testing with a sodium chloride aerosol at a flow rate of 95 L/min. 46 The National Institute for Occupational Safety and Health in the USA sets the standards for N95 respirators, 60 which require a filter efficiency of at least 95% in standardized testing with a sodium chloride aerosol at a flow rate of 85 L/min. 46 , 61
As most particle penetration of P2/N95 respirators occurs through face‐seal leakage, 62 optimizing facial fit through comprehensive fit‐testing and fit‐checking is essential to ensure adequate protection against airborne transmission 63 , 64 of SARS‐CoV‐2. Fit checks must be performed at every instance of donning to ensure the respirator is properly applied. 46 It is also recommended that all members of surgical staff are clean‐shaven, if possible, to ensure optimal facial seal and fit. 65
Extending the use of P2 and N95 respirators
At the time of publication, there is a worldwide shortage in the supply of PPE relative to the demand created by the COVID‐19 global pandemic. 15 , 66 , 67 This is especially true for FFRs. Options for safely extending their use must be considered, however, scientific studies investigating these methods have been small and laboratory‐based.
Using a full‐face shield over a surgical P2/N95 respirator protects it from droplets and aerosols, which may allow its extended use. 68 Similarly, covering respirators with standard surgical masks or similar disposable covers can potentially extend the life of the respirator without significant adverse effects on the cardiorespiratory physiology of the wearer. 69 Laboratory‐based studies on the disinfection of surgical P2/N95 respirators by ultraviolet germicidal irradiation are promising and may be a potential option to allow safe re‐use. 70 This is particularly encouraging for the COVID‐19 pandemic, since the ultraviolet dose required to inactivate single‐stranded RNA viruses such as SARS‐CoV‐2 is relatively low. 71
Conclusions
In the fight against COVID‐19, it is essential to supplement standard infection control measures with the appropriate use of PPE, especially where there are risks of potential exposure to any biohazardous material. Surgical departments must ensure that their staff receive formal training in the correct use of PPE. Donning and doffing must always be methodical and supervised by another staff member, especially during surgical emergencies and aerosol‐generating procedures. Standard surgical masks fail to protect against the airborne transmission of SARS‐CoV‐2, so properly fit‐tested and fit‐checked surgical P2/N95 respirators are a necessary PPE item for surgical staff. Where possible, patients with severe respiratory symptoms and those with suspected or confirmed COVID‐19 should wear surgical masks during transfer to and from the operating theatre. Potential solutions have been published in the peer‐reviewed literature to enable the extended use of surgical P2/N95 respirators in situations of limited supply.
Conflicts of interest
None declared.
Acknowledgements
The authors acknowledge Dr Vanessa Beavis, representing the Australian and New Zealand College of Anaesthetists; Dr Vicky H. Lu, representing the Royal Australian and New Zealand College of Ophthalmologists; Dr James Churchill, representing the Royal Australasian College of Surgeons Trainees' Association; Dr Chloe Ayres, representing the Royal Australian and New Zealand College of Obstetricians and Gynaecologists.
L. Tan BSc (Hons), PhD; J. G. Kovoor; P. Williamson BHlth Sci (Hons), PhD; D. R. Tivey BSc (Hons), PhD; W. J. Babidge BApp Sci (Hons), PhD; T. G. Collinson MS, FRACS; P. J. Hewett MBBS, FRACS; T. J. Hugh MD, FRACS; R. T. A. Padbury PhD, FRACS; S. J. Langley MBChB, FRACS; G. J. Maddern PhD, FRACS.
References
- 1. World Health Organization . Pneumonia of unknown cause–China. Emergencies preparedness, response, Disease outbreak news. World Health Organization. 2020.
- 2. World Health Organization . WHO Director‐General's Opening Remarks at the Media Briefing on COVID‐19, 11 March 2020. 2020.
- 3. Coronaviridae Study Group of the International Committee on Taxonomy of Viruses . The species severe acute respiratory syndrome‐related coronavirus: classifying 2019‐nCoV and naming it SARS‐CoV‐2. Nat. Microbiol. 2020; 5: 536–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zhu N, Zhang D, Wang W et al. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020; 382: 727–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. van Doremalen N, Bushmaker T, Morris DH et al. Aerosol and surface stability of SARS‐CoV‐2 as compared with SARS‐CoV‐1. N. Engl. J. Med. 2020; 382: 1564–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bai Y, Yao L, Wei T et al. Presumed asymptomatic carrier transmission of COVID‐19. JAMA 2020; 323: 1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Li R, Pei S, Chen B et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS‐CoV2). Science 2020; 368: 489–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID‐19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020; 323: 1239. [DOI] [PubMed] [Google Scholar]
- 9. Livingston E, Bucher K. Coronavirus disease 2019 (COVID‐19) in Italy. JAMA 2020; 323: 1335. [DOI] [PubMed] [Google Scholar]
- 10. Novel Coronavirus Pneumonia Emergency Response Epidemiology Team . The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID‐19) in China. Zhonghua Liu Xing Bing Xue Za Zhi 2020; 41: 145–51.32064853 [Google Scholar]
- 11. Chang XH, Rebaza A, Sharma L, Dela Cruz CS. Protecting health‐care workers from subclinical coronavirus infection. Lancet Respir. Med. 2020; 8: e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gerberding JL, Littell C, Tarkington A, Brown A, Schecter WP. Risk of exposure of surgical personnel to patients' blood during surgery at San Francisco General Hospital. N. Engl. J. Med. 1990; 322: 1788–93. [DOI] [PubMed] [Google Scholar]
- 13. Panlilio AL, Foy DR, Edwards JR et al. Blood contacts during surgical procedures. JAMA 1991; 265: 1533–7. [PubMed] [Google Scholar]
- 14. Nagao M, Iinuma Y, Igawa J et al. Accidental exposures to blood and body fluid in the operation room and the issue of underreporting. Am. J. Infect. Control 2009; 37: 541–4. [DOI] [PubMed] [Google Scholar]
- 15. World Health Organization . Rational Use of Personal Protective Equipment for Coronavirus Disease ( COVID‐19) and Considerations During Severe Shortages: Interim Guidance, 6 April 2020. 2020.
- 16. Beam EL, Gibbs SG, Boulter KC, Beckerdite ME, Smith PW. A method for evaluating health care workers' personal protective equipment technique. Am. J. Infect. Control 2011; 39: 415–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chen Y‐C, Chen P‐J, Chang S‐C et al. Infection control and SARS transmission among healthcare workers, Taiwan. Emerg. Infect. Dis. 2004; 10: 895–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ofner‐Agostini M, Gravel D, McDonald LC et al. Cluster of cases of severe acute respiratory syndrome among Toronto healthcare workers after implementation of infection control precautions: a case series. Infect. Control Hosp. Epidemiol. 2006; 27: 473–8. [DOI] [PubMed] [Google Scholar]
- 19. Shigayeva A, Green K, Raboud J et al. Factors associated with critical‐care healthcare workers' adherence to recommended barrier precautions during the Toronto severe acute respiratory syndrome outbreak. Infect. Control Hosp. Epidemiol. 2007; 28: 1275–83. [DOI] [PubMed] [Google Scholar]
- 20. Watt A, Cameron A, Sturm L et al. Rapid versus full systematic reviews: validity in clinical practice? ANZ J. Surg. 2008; 78: 1037–40. [DOI] [PubMed] [Google Scholar]
- 21. Watt A, Cameron A, Sturm L et al. Rapid reviews versus full systematic reviews: an inventory of current methods and practice in health technology assessment. Int. J. Technol. Assess. Health Care 2008; 24: 133–9. [DOI] [PubMed] [Google Scholar]
- 22. Khangura S, Konnyu K, Cushman R, Grimshaw J, Moher D. Evidence summaries: the evolution of a rapid review approach. Syst. Rev. 2012; 1: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Royal Australasian College of Surgeons . Guidelines for Personal Protective Equipment, 1st edn. [Cited 9 Jun 2020.] Available from URL: https://umbraco.surgeons.org/media/5302/2020‐05‐05‐covid19‐ppe‐guidelines.pdf
- 24. Swerdlow DL, Finelli L, Lipsitch M. Epidemiology of Covid‐19. N Engl J Med. 2020; 382: 1869–70. [DOI] [PubMed] [Google Scholar]
- 25. Lipsitch M, Swerdlow DL, Finelli L. Defining the epidemiology of Covid‐19 – studies needed. N. Engl. J. Med. 2020; 382: 1194–6. [DOI] [PubMed] [Google Scholar]
- 26. Royal Australasian College of Surgeons . Guidelines for Personal Protective Equipment: A Rapid Review Commissioned by RACS. [Cited 9 May 2020.] Available from URL: https://umbraco.surgeons.org/media/5302/2020-05-05-covid19-ppe-guidelines.pdf
- 27. Australian Government Department of Health . Interim advice on non‐inpatient care of persons with suspected or confirmed Coronavirus disease (COVID‐19), including use of personal protective equipment (PPE). [Cited 10 Apr 2020.] Available from URL: https://www.health.gov.au/sites/default/files/documents/2020/03/interim‐advice‐on‐non‐inpatient‐care‐of‐persons‐with‐suspected‐or‐confirmed‐coronavirus‐disease‐2019‐covid‐19‐including‐use‐of‐personal‐protective‐equipment‐ppe.pdf
- 28. Ministry of Health New Zealand . Case definition of COVID‐19 infection. [Cited 16 May 2020.] Available from: https://www.health.govt.nz/our‐work/diseases‐and‐conditions/covid‐19‐novel‐coronavirus/covid‐19‐resources‐health‐professionals/case‐definition‐covid‐19‐infection
- 29. Wang W, Xu Y, Gao R et al. Detection of SARS‐CoV‐2 in different types of clinical specimens. JAMA 2020; 323: 1843–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H. Evidence for gastrointestinal infection of SARS‐CoV‐2. Gastroenterology 2020; 158: 1831–1833.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Patel R, Babady E, Theel ES et al. Report from the American Society for Microbiology COVID‐19 International Summit, 23 March 2020: Value of Diagnostic Testing for SARS–CoV‐2/COVID‐19. mBio 2020; 11: e00722‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sharfstein JM, Becker SJ, Mello MM. Diagnostic testing for the novel coronavirus. JAMA 2020; 323: 1437. [DOI] [PubMed] [Google Scholar]
- 33. World Health Organization . Laboratory Testing for Coronavirus Disease 2019 (COVID‐19) in Suspected Human Cases: Interim Guidance, 2 March 2020. 2020.
- 34. Lippi G, Simundic AM, Plebani M. Potential preanalytical and analytical vulnerabilities in the laboratory diagnosis of coronavirus disease 2019 (COVID‐19). Clin. Chem. Lab. Med. 2020; 58: 1070–6. [DOI] [PubMed] [Google Scholar]
- 35. Lau JT, Fung KS, Wong TW et al. SARS transmission among hospital workers in Hong Kong. Emerg. Infect. Dis. 2004; 10: 280–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Wu A, Peng Y, Huang B et al. Genome composition and divergence of the novel coronavirus (2019‐nCoV) originating in China. Cell Host Microbe 2020; 27: 325–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Lu R, Zhao X, Li J et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 2020; 395: 565–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Zaman S, MacIsaac AI, Jennings GL et al. Cardiovascular disease and COVID‐19: Australian/New Zealand consensus statement. Med. J. Aust. 2020. [DOI] [PubMed] [Google Scholar]
- 39. Johnson RM. PDA responds to the novel coronavirus situation. PDA J. Pharm. Sci. Technol. 2020; 74: 170. [DOI] [PubMed] [Google Scholar]
- 40. Australian and New Zealand College of Anaesthetists . ANZCA Statement on Personal Protection Equipment During the SARS‐CoV‐2 Pandemic (9 April 2020). [Cited 9 Apr 2020.] Available from URL: http://www.anzca.edu.au/documents/anzca‐covid‐ppe‐statement‐v24‐09042020‐(1).pdf
- 41. Australian Government . Guidance on the Use of Personal Protective Equipment (PPE) in Hospitals During the COVID‐19 Outbreak. In: Department of Health (ed.), 2020; 1–9.
- 42. Kwon JH, Burnham CD, Reske KA et al. Assessment of healthcare worker protocol deviations and self‐contamination during personal protective equipment donning and doffing. Infect. Control Hosp. Epidemiol. 2017; 38: 1077–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Verbeek JH, Rajamaki B, Ijaz S et al. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database Syst. Rev. 2020; 4: CD011621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Tomas ME, Kundrapu S, Thota P et al. Contamination of health care personnel during removal of personal protective equipment. JAMA Intern. Med. 2015; 175: 1904–10. [DOI] [PubMed] [Google Scholar]
- 45. Siegel JD, Rhinehart E, Jackson M, Chiarello L. Health care infection control practices advisory committee. 2007 guideline for isolation precautions: preventing transmission of infectious agents in health care settings. Am. J. Infect. Control 2007; 35: S65–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Australian Commission on Safety and Quality in Health Care . Australian Guidelines for the Prevention and Control of Infection in Healthcare. Canberra: National Health and Medical Research Council; 2019; 2019. [Google Scholar]
- 47. Centers for Disease Control and Prevention . Use Personal Protective Equipment (PPE) When Caring for Patients with Confirmed or Suspected COVID‐19. [Cited 19 Apr 2020.] Available from URL: https://www.cdc.gov/coronavirus/2019-ncov/downloads/A_FS_HCP_COVID19_PPE.pdf
- 48. Brindle M, Gawande A. Managing COVID‐19 in surgical systems. Ann. Surg. 2020; 272: e1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Evans HL, Thomas CS, Bell LH et al. Development of a sterile personal protective equipment donning and doffing procedure to protect surgical teams from SARS‐CoV‐2 exposure during the COVID‐19 pandemic. Surg. Infect. 2020. 10.1089/sur.2020.140. [DOI] [PubMed] [Google Scholar]
- 50. Ti LK, Ang LS, Foong TW, Ng BSW. What we do when a COVID‐19 patient needs an operation: operating room preparation and guidance. Can. J. Anesth. 2020; 67: 756–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Chughtai AA, Chen X, Macintyre CR. Risk of self‐contamination during doffing of personal protective equipment. Am. J. Infect. Control 2018; 46: 1329–34. [DOI] [PubMed] [Google Scholar]
- 52. Standards Australia . Australian Standard: Single‐Use Face Mask for Use in Health Care. Standards Australia, 2015.
- 53. MacIntyre CR, Wang Q, Seale H et al. A randomized clinical trial of three options for N95 respirators and medical masks in health workers. Am. J. Respir. Crit. Care Med. 2013; 187: 960–6. [DOI] [PubMed] [Google Scholar]
- 54. MacIntyre CR, Wang Q, Rahman B et al. Efficacy of face masks and respirators in preventing upper respiratory tract bacterial colonization and co‐infection in hospital healthcare workers. Prev. Med. 2014; 62: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. MacIntyre CR, Wang Q, Cauchemez S et al. A cluster randomized clinical trial comparing fit‐tested and non‐fit‐tested N95 respirators to medical masks to prevent respiratory virus infection in health care workers. Influenza Other Respi. Viruses 2011; 5: 170–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Bałazy A, Toivola M, Adhikari A, Sivasubramani SK, Reponen T, Grinshpun SA. Do N95 respirators provide 95% protection level against airborne viruses, and how adequate are surgical masks? Am. J. Infect. Control 2006; 34: 51–7. [DOI] [PubMed] [Google Scholar]
- 57. Wong J, Goh QY, Tan Z et al. Preparing for a COVID‐19 pandemic: a review of operating room outbreak response measures in a large tertiary hospital in Singapore. Can. J. Anaesth. 2020; 67: 732–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Standards Australia Limited/Standards New Zealand . AS/NZS 1716: 2012, Respiratory Protective Devices. SAI Global Limited, Standards New Zealand, 2012.
- 59. Standards Australia Limited/Standards New Zealand . AS/NZS 1715: 2009, Selection, Use and Maintenance of Respiratory Protective Equipment. Standards Australia, Standards New Zealands, 2009.
- 60. National Institute for Occupational Safety and Health . Procedure No. TEB‐APR‐STP‐0059: Determination of Particulate Filter Efficiency Level for N95 Series Filters Against Solid Particulates for Non‐powered, Air‐purifying Respirators Standard Testing Procedure (STP). 2019.
- 61. Gralton J, McLaws ML. Protecting healthcare workers from pandemic influenza: N95 or surgical masks? Crit. Care Med. 2010; 38: 657–67. [DOI] [PubMed] [Google Scholar]
- 62. Cho KJ, Reponen T, McKay R et al. Large particle penetration through N95 respirator filters and facepiece leaks with cyclic flow. Ann. Occup. Hyg. 2010; 54: 68–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Centers for Disease Control Prevention . Laboratory performance evaluation of N95 filtering facepiece respirators, 1996. MMWR Morb. Mortal Wkly. Rep. 1998; 47: 1045–9. [PubMed] [Google Scholar]
- 64. Coffey CC, Lawrence RB, Campbell DL, Zhuang Z, Calvert CA, Jensen PA. Fitting characteristics of eighteen N95 filtering‐facepiece respirators. J. Occup. Environ. Hyg. 2004; 1: 262–71. [DOI] [PubMed] [Google Scholar]
- 65. Stobbe TJ, daRoza RA, Watkins MA. Facial hair and respirator fit: a review of the literature. Am. Ind. Hyg. Assoc. J. 1988; 49: 199–204. [DOI] [PubMed] [Google Scholar]
- 66. Newman M. Covid‐19: Doctors' Leaders Warn That Staff Could Quit and May Die Over Lack of Protective Equipment. 2020. [DOI] [PubMed]
- 67. Livingston E, Desai A, Berkwits M. Sourcing personal protective equipment during the COVID‐19 pandemic. JAMA 2020; 323: 1912. [DOI] [PubMed] [Google Scholar]
- 68. Forrester JD, Nassar AK, Maggio PM, Hawn MT. Precautions for operating room team members during the COVID‐19 pandemic. J. Am. Coll. Surg. 2020; 230: 1098–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Sinkule EJ, Powell JB, Goss FL. Evaluation of N95 respirator use with a surgical mask cover: effects on breathing resistance and inhaled carbon dioxide. Ann. Occup. Hyg. 2013; 57: 384–98. [DOI] [PubMed] [Google Scholar]
- 70. Vo E, Rengasamy S, Shaffer R. Development of a test system to evaluate procedures for decontamination of respirators containing viral droplets. Appl. Environ. Microbiol. 2009; 75: 7303–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Tseng C‐C, Li C‐S. Inactivation of viruses on surfaces by ultraviolet germicidal irradiation. J. Occup. Environ. Hyg. 2007; 4: 400–5. [DOI] [PMC free article] [PubMed] [Google Scholar]


