Summary
The scoping review was undertaken to outline the vulnerabilities of Pakistan's public health and healthcare system, which put the population at increased risk of coronavirus disease 2019 (COVID‐19) associated morbidity and mortality. The major electronic databases were searched using both “text words” and “thesaurus terms,” focusing on viral infections, COVID‐19 and healthcare systems in Pakistan. The content of the selected articles was analyzed by using thematic approach. Out of the total 171 potentially relevant citations, 24 articles were included in the data synthesis. We found that the recent COVID‐19 outbreak is a major threat to Pakistan's public health and healthcare system, and the country is not in a position to control spread of disease and provide required standards of care deemed necessary by the World Health Organization. A number of intertwined reasons that expose the Pakistani population at increased risk of COVID‐19 associated morbidity and mortality, include public related demurrals, healthcare workforce related demurrals, organizational and regulatory voids, and travel patterns. To cope with the upsurge of COVID‐19 in Pakistan, the regulators need to re‐examine and recognize deficiencies in the healthcare system, and thereafter reinforce core capacities in workforce and monetary resources, surveillance, laboratory services, and hospital preparedness for isolation and ventilation of patients.
Keywords: coronaviruses, COVID‐19, healthcare system, Pakistan, SARSCoV‐2
ABBREVIATIONS
- AIDS
acquired immunodeficiency syndrome
- CDC
Center for Disease Control and Prevention
- CoVs
coronaviruses
- FE&DSD
Field Epidemiology and Disease Surveillance Division
- IHR
International Health Regulations
- MERS
Middle East Respiratory Syndrome
- SARS
Severe Acute Respiratory Syndrome
- SARSCoV‐2
Severe Acute Respiratory Syndrome Coronavirus 2
- SOP
standard operating procedure
- WHO
World Health Organization
1. BACKGROUND
The emergence and reemergence of human coronaviruses (CoVs) has always triggered a new global threat. 1 In the 1960s, Tyrell and Bynoe identified the first CoV (named B814) in human tracheal organ cultures. 1 Broadly distributed CoVs are enveloped single‐stranded RNA viruses with a characteristic “halo appearance” (i.e., a corona on electron microscopy). Since their first identification, CoVs have been graded into four subgroups: alpha, beta, delta and gamma. 2 Among these, alpha and beta CoVs are known to infect humans. The alpha coronavirus subgroup comprises of 229E and NL63, and the beta coronavirus subgroup includes OC43, HKU1, Severe Acute Respiratory Syndrome (SARS)‐CoV and Middle East Respiratory Syndrome (MERS)‐CoV. Four human CoVs (i.e., HCoV‐229E, HCoV‐OC43, HCoV‐NL63 and HCoV‐HKU1) are endemic in humans and are primarily related to moderate, self‐limiting respiratory diseases. In comparison, SARS‐CoV and MERS‐CoV are zoonotic in origin and cause severe respiratory syndromes and pose a considerable threat to humans with their high mortality rates. 3
In relation to CoVs, an outbreak of atypical pneumonia was first emerged in China in 2002 before spreading to 29 countries/regions in 2003. The disease was named SARS, 4 and the causative agent was identified as a completely novel CoV, termed SARS‐CoV. 5 A total of 8098 patients were affected worldwide with a case fatality rate of 9.6% (774 deaths). 6 Nearly, a decade after the SARS outbreak, another deadly MERS‐CoV appeared in the Arabian Peninsula that caused severe viral pneumonia (i.e., MERS), and about 35% patients succumbed to MERS‐CoV. 7 Once again in December 2019, an outbreak emerged as a mysterious cluster of respiratory illnesses in Wuhan City, Hubei Province of China. 8 The Chinese Center for Disease Control and Prevention (CDC) confirmed within a week that the latest outbreak is attributable to a new CoV and temporarily named it as “2019‐nCoV.” 9 On 11 February 2020, the International Committee on Taxonomy of Viruses named the virus as severe acute respiratory syndrome coronavirus 2 (SARSCoV‐2), and the World Health Organization (WHO) named the disease caused by this virus as COVID‐19. 10 On 11 March 2020, considering the worldwide spread and death associated with COVID‐19, the WHO categorized the disease as a pandemic. As of 25 May 2020, worldwide, a total of 5 307 298 confirmed cases of COVID‐19 (mortality in 342 070 cases) have been documented by the WHO. 11
To date, there is a lot of ambiguity about various aspects of COVID‐19, including epidemiology, transmission, clinical manifestation, pathophysiology and prevention and management. According to the reports, the clinical presentations in the confirmed cases of COVID‐19 were very close to SARS‐CoV and MERS‐CoV infections. 8 , 12 , 13 The median time from the onset of symptom to first hospital admission was 7 days, and to the intensive care unit admission was 10.5 days. 8 The common symptoms at the onset of illness were fever, cough and myalgia or fatigue followed by less common symptoms, that is, sputum production, headache, haemoptysis and diarrhea. 8 , 12 , 13 Shortness of breath and breathing difficulties occurred in 55% of the patients. 8 The consequences of infection were not limited to common respiratory symptoms but severe outcomes included pneumonia, acute respiratory distress syndrome, acute cardiac injury, secondary infections, kidney failure and death. 8 , 13 According to the United States (US) CDC and the WHO, the best way to prevent the infection is to avoid being exposed to this virus and minimizing person‐to‐person spread. 14 , 15 The management of COVID‐19 patients relies on early detection, prompt isolation and initiation of effective infection prevention and control measures; delivery of symptomatic care for those with mild illness and optimized supportive care for those with severe disease. 16 In this regard, the healthcare system and financial stability of nations plays a crucial role in achieving the required standards of prevention and management strategies. Recently, the WHO has alarmed that the increase of COVID‐19 cases from the Eastern Mediterranean Region is of great concern due to a number of deficits in their healthcare systems and financial instability. 17
Pakistan is a low‐ and middle‐income country that has been recently ranked 152th out of 189 countries with a Human Development Index value of 0.560. 16 The country encountered a variety of healthcare challenges in last several decades and endured a great deal from many epidemics that had devastating effect on people in terms of morbidity, mortality and economic burden. 18 , 19 In 2017, lower respiratory tract infections and tuberculosis were among the top causes of mortality in Pakistan. 20 Whereas, the majority of the pediatrics died from acute respiratory infections, diarrhea and sepsis in 2013. 21 Due to failure to attain good healthcare standards, Pakistan has become a reservoir for infectious diseases, and thousands of people have succumbed to viral epidemics such as polio, acquired immunodeficiency syndrome (AIDS), measles, dengue, hepatitis and so forth (Figure 1). 12 , 22 , 23 , 24 , 25 , 26 , 27 The dilemma could be gauged by the reemergence of polio virus in Pakistan, which has been exterminated, elsewhere. 22
FIGURE 1.
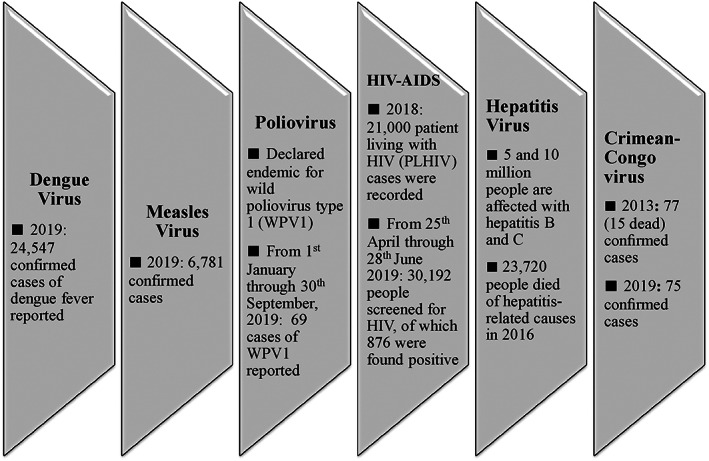
Most recent trend of emerging and reemerging viral infections in Pakistan
Similarly, the unprecedented COVID‐19 outbreak poses significant threat to Pakistan owing to a number of reasons. In Pakistan, the first case of COVID‐19 was confirmed on 25 February 2020. 28 As of 25 May 2020, the number of confirmed cases surpassed 56 349, with 1167 fatalities. 29 Considering the upsurge of the confirmed cases and deficits in the healthcare system, the disease is expected to spread like wildfire across the country. On 23 April 2020, the WHO warned the Pakistani government that the country is at an increased risk of COVID‐19 associated mortality and morbidity, if no appropriate counteractions are taken to curb the infection. 30 We undertook this review to outline the shortcomings of Pakistan's public health and healthcare systems, which place the population at increased risk of COVID‐19 related morbidity and mortality. The policy makers may take benefit of our findings to avert the anticipated agony associated with COVID‐19 as well as future infectious outbreaks.
2. METHODS
2.1. Design
We carried out a scoping review of literature informed by the methodological framework of Arksey and O'Malley. 31 The five step framework involves (a) identifying the research question; (b) searching for relevant studies; (c) selecting studies; (d) charting the data and (e) collating, summarizing and reporting the results. Even though, the scoping review has a lot of things in common with a systematic review, quality assessment is not necessary and the findings are generally published in a narrative format. 32 This approach enabled us to gain an overview of the breadth of literature in a developing field, especially where an area such as COVID‐19 is new and has not been comprehensively synthesized earlier. 31
2.2. Search strategy
The major electronic databases, that is, Embase, EconLit, Google Scholar, Medline, PubMed, ProQuest, Scopus, Springer Link and Science Direct databases, were searched using both “text words” and “thesaurus terms,” focusing on viral infections, COVID‐19 and healthcare system in Pakistan. The references of selected papers were also examined to identify relevant literature. We also screened the databases of leading organizations, such as CDC, the WHO and so forth. The commentaries, editorials, perspective articles and book chapters were also included because of the limited data published in scientific journals. As provided in the flow diagram (Figure 2), the initial literature search resulted in 171 potentially relevant citations. Of these, 33 duplicates were detected in Endnote and were omitted. Out of the 138 remaining articles, 73 were excluded based on abstracts being irrelevant. Subsequently, 65 studies were carefully examined, and 44 articles were excluded at this stage for failing to present pertinent information. In the final grouping, 24 articles were selected for this review.
FIGURE 2.
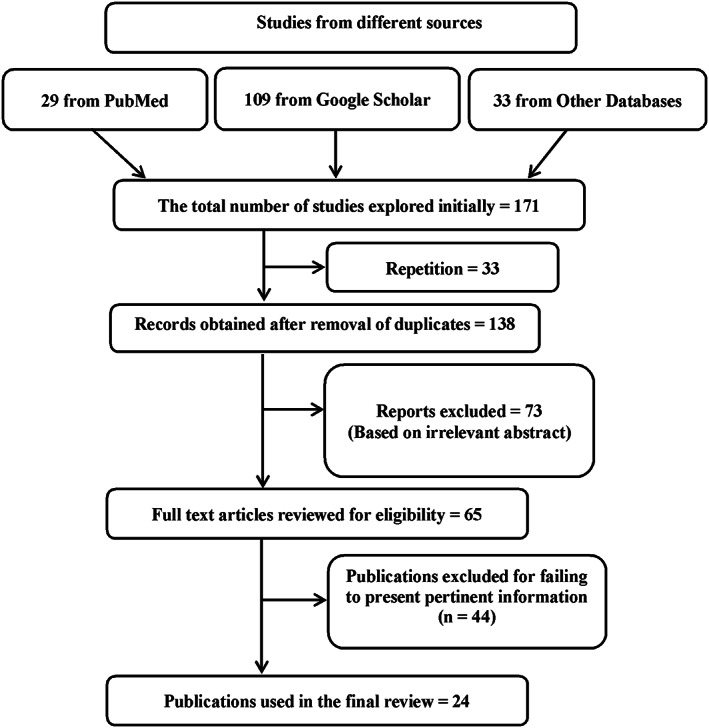
Flow diagram
2.3. Data extraction and analysis
The information emerging from the literature was classified using a purpose‐designed data extraction tool. Each record outlined the existing information about the vulnerabilities of Pakistan's public health and healthcare systems. The entered data were summarized, rechecked and charted using a data sheet. The content of the articles was analyzed by using thematic approach 33 and presented as a set of themes representing our key focus. The author name, year of publication, article type and vulnerabilities retrieved from articles are provided in Supporting Information File 1.
3. FINDINGS AND DISCUSSION
Following the thematic approach, a total of four themes emerged. All themes summarized information about the vulnerabilities of Pakistan's public health and healthcare systems. Our assessment showed that the country is not in a position to provide required standards of care due to many intertwined reasons. These include, community and healthcare workforce related demurrals, organizational and regulatory voids and travel patterns. Fishbone diagram (Figure 3) was also created with the goal of grouping the causes 34 that create or contribute to a high risk of COVID‐19 and other emerging infectious diseases in Pakistan and like nations. The themes are discussed below.
FIGURE 3.
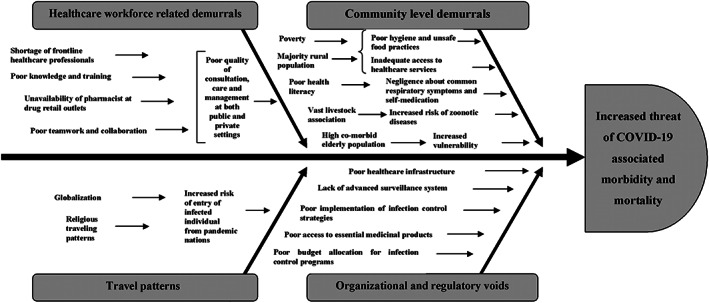
A fishbone diagram to show causes contributing to high risk of COVID‐19 associated morbidity and mortality
3.1. Community level demurrals
Infectious diseases and poverty are closely associated. Existing literature indicates that the incidence rates of infectious diseases are highest in places where poverty is at its peak. 35 Unfortunately, about 25% of the people in Pakistan are living below the poverty line and poor hygiene practices are very common. 19 , 33 They reside in very congested areas and most of them do not have access to hospitals and medications. 36 In view of this scenario, it is quite challenging for them to comply with the WHO's standard precautionary measures against COVID‐19, including hand and respiratory hygiene, environmental cleaning, self‐isolation, social distancing, use of personal protective equipment and so forth.
In addition, Pakistan's population consists of around one third of the urban residents (37%) and two thirds of the rural residents (63%). 33 , 37 There are a plethora of factors that place rural communities at high risk of COVID‐19 acquisition. The facilities at rural health centers are currently inadequate to cater to the needs of rural communities at times of disaster, as indicated by Shah et al. 36 In specific, the facilities lack space, beds and equipment required for disaster relief, and the healthcare staff at rural health centers lacks proper training and expertise. Considering the fact that most rural citizens are associated with the livestock industry and have little access to healthcare facilities, 33 they are undoubtedly at increased risk of COVID‐19, especially if the virus spreads to animals in the future.
Furthermore, lack of knowledge and awareness driven by low literacy among Pakistani citizens leads to healthcare negligence. 38 For a variety of reasons, ranging from time shortages to financial constraints, the majority of the population does not seek advice from healthcare professionals 38 on common respiratory tract infections, and attempt to self‐medicate with home‐remedies or over the counter medicines. 39 Such practices could lead to delayed diagnosis of COVID‐19 followed by increased risk of morbidity and mortality. The ignorance and noncooperative attitude exhibited by the general public can fuel the rapid spread of COVID‐19 throughout Pakistan. 40 Recently, COVID‐19 focused Pakistani studies revealed that social distancing was significantly influenced by situational awareness, 41 and poor knowledge regarding transmission of COVID‐19 was perceived as a major obstacle in infection control practices. 42
Pakistan is an agricultural country, and the people and its economy depends heavily on agriculture and natural resources. A total of about 40% of the total population in Pakistan is engaged in animal husbandry, livestock handling, fishing industry and forestry. 19 Considering the fact that zoonotic diseases are gaining momentum in Pakistan, a One Health Hub was created under Field Epidemiology & Disease Surveillance Division (FE&DSD) with the goal of preventing and managing the zoonotic diseases of national and international concern through well‐coordinated response by human, animal and environmental departments. 43 Regarding COVID‐19, although the preliminary cases were linked to livestock (seafood market), 44 animal‐to‐human and human‐to‐animal transmission has not been greatly observed till date. However, at this point, the patterns of COVID‐19 transmission cannot be firmly predicted due to persistent ambiguity about various aspects. Accordingly, Pakistani people with such high exposure to livestock should be deemed at greater risk of acquiring COVID‐19 and other zoonotic diseases.
In Pakistan, the incidence of noncommunicable chronic diseases (i.e., hypertension, diabetes, cardiovascular disease and malignancy) is high, 45 and about 80% of elderly are suffering from such chronic illnesses. 46 This makes elderly population more susceptible to COVID‐19 and associated mortality, as the WHO declared that the seriousness of the disease strongly corresponds to underlying host conditions, including age (elderly) and overall health (comorbid and immunity level). 13 , 47
3.2. Organizational and regulatory voids
Pakistan has limited health system capacity for appropriate management of crisis. 48 The existing legislations and policies regarding infection control and prevention are far below the international standards. 27 , 49 Although Pakistan developed its first national infection guidelines in 2006, implementation and compliance are not satisfactory. 50 The public healthcare settings do not have formal standard operating procedures (SOPs) that meet the national guidelines on hospital infection control and prevention. 51 One study, for instance, confirmed that even simple hand washing facilities were not available at about one quarter (25%) of Pakistan's public sector hospitals. 52 Another study revealed that disasters‐related capacities and preparedness level of healthcare institutions in Pakistan was unsatisfactory. 53 According to a study, there were nonexistent SOPs for triage in Pakistani hospitals, thereby leading to mismanagement of patients during disasters. 54
Pakistan lacks a strong healthcare infrastructure. 21 , 55 , 56 , 57 There are 5527 basic health units, 686 rural health centers and 5671 dispensaries in the country to serve the healthcare needs of a population of more than 207 million citizens. 19 In 2018, only one bed was available for 1608 patients. 19 In addition, the Pakistani health system is constantly being attacked by terrorists. 27 Approximately, 29% of healthcare facilities in Khyber Pakhtunkhwa were destroyed. 58 , 59 As a result, regardless of the current governmental level efforts in response to the COVID‐19, the number of hospitals and quarantine facilities in the country are less, 60 which may highly contribute to the delay in the diagnosis and treatment of infected patients, and ultimately results in morbidity and mortality. Another problem is the limited capacity of laboratories and it seems challenging to scale‐up the laboratory facilities, 60 , 61 , 62 for screening of such a large population.
Along with the harrowing surge in COVID‐19 cases, the whole world is witnessing the emerging vulnerabilities of pharmaceutical supply chain. 63 Previous Pakistani evidences indicated major gaps in access to essential medicines in Pakistan driven by deficits in the pharmaceutical supply chain and ambiguous pharmaceutical regulations. 38 , 55 , 56 , 64 , 65 Unsurprisingly, due to sudden demand fluctuation, raw material availability issues and nontraditional distribution tactics several essential (such as antipyretic, analgesics and other flu and cough medicines) and life‐saving medicines, facemasks, sanitizers and other protective equipment are currently short or scarcely available at high prices. 40 Taking into account this scenario, it will be a great challenge for the Pakistani government to fulfill the medicinal product related needs of the population, especially after the discovery of COVID‐19 treatment and vaccination. Additionally, lack of access to basic medicinal products may also have severe consequences for patients with other communicable and noncommunicable diseases.
Pakistan also lacks well‐defined system to eliminate the possibility of abrupt outbreaks and a robust infectious agent alarm system to address the threat of emerging germs. 27 According to the Global Health Security Index 2019, Pakistan attained 0.0 index scores in various aspects of healthcare system, including emergency preparedness and response planning, communication with healthcare workers, infection control practices and availability of equipment, cross‐border agreements on public health emergency response and risk communication systems. 66 Although, a Disease Early Warning System was developed in 2005 through the collaboration of the WHO and the Federal Ministry of Health, it was not enforced properly. 25 Later in 2013, considering the upsurge of communicable diseases, and deficits in emergency response and preparedness, the Ministry of National Health Services, Regulations and Coordination established a division named FE&DSD. The aim of FE&DSD was to respond to outbreaks and epidemics, national and international events of public health significance and provide the necessary input to the concerned stakeholders. However despite meaningful governmental level efforts, recent outbreaks of AIDS, polio, dengue, hepatitis, measles and now COVID‐19 (Figure 1) raise concerns and call for improvements in the functioning of FE&DSD. 12 , 22 , 23 , 24 , 25 , 26
The budgetary constraints further exacerbate all the aforementioned disparities in Pakistan, 56 as the spending on health has been less than 3% of gross domestic product. 67 Although, commendably, specific budget is earmarked by the government with the help of international funding for activities concerning COVID‐19 control and prevention, but the prevailing mismanagement at lower hierarchy level 55 and biased distribution practices may endanger these efforts. 68
3.3. Healthcare workforce related demurrals
Human resources for healthcare are identified as one of the core building blocks of a health system and workforce crisis are one of the major obstacles to the quality healthcare. 68 According to the WHO, the overall Pakistani health sector is confronted with an imbalance in the number, expertise and distribution of healthcare professionals and insufficient allotment of resources across various levels of healthcare. 69 Currently, one physician is available to serve every 963 persons in Pakistan. 19 With regard to availability of healthcare professionals, a total of 220 829 registered doctors, 22 595 registered dentists and 108 474 registered nurses are actively working in Pakistan. 19 The availability of pharmacists in Pakistan (1.6 pharmacists per 10 000 person population) is also meager compared to the target (five pharmacists per 10 000 person population) set by the WHO. 70 In addition, a number of studies have indicated that existing healthcare workforce were overburdened, 21 , 71 and the mean consultation time (1.2‐2.2 minutes) and the dispensing time (8.7‐38 seconds) in the public sector facilities were suboptimal. 72 , 73 Moreover, unavailability of qualified and trained community pharmacists at drug retail outlets add fuel to the fire, 74 as patients are not provided with required consultation and infection prevention measures for common infections. 38 , 75 , 76 , 77 However, there are growing debates that pharmacists—being the first to be reached by patients in resource deprived settings—have all the abilities and expertise to forestall and resolve minor health issues, including infectious diseases, through proper counseling. 76 , 78 Well‐trained community pharmacists can refer the critically ill patients (eg, presumptive COVID‐19 patients) to specialized healthcare facilities. This has been borne out by a recent study, according to which “pharmacist job” was one of the substantial determinants of good COVID‐19 infection control practices. 42
Apart from limited healthcare workforce, negligence, unaccountability, lack of follow up of existing infection control guidelines, and inadequate experience, knowledge and formal training of healthcare professionals about emerging diseases continue to severely derail the existing healthcare resources. 49 , 50 , 79 The Joint External Evaluation task study (2016) of the International Health Regulations (IHR) raised concerns that staff members in Pakistan lack the requisite experience and background knowledge on control and prevention of health issues. 80 , 81 Similarly, a previous study reported that healthcare professionals had suboptimal knowledge of preventive methods (72%) and diagnostic techniques (59%) and other aspects of MERS infection since advanced training and continued medical education were not mandatory in Pakistan. 68 Likewise, Khan et al has recently reported that front‐line healthcare workers were not well aware of the COVID‐19 related strategies for the prevention and control of infection, and were not prepared for the alarming situation in the country. 82 Beside this, poor collaboration among all the healthcare professionals, such as physicians, clinical microbiologist, pharmacists and nurses 83 is other well‐known factor that undermines infection control efforts. 84 , 85 Taking into account all the aforementioned healthcare workforce related deficits, COVID‐19 might put undue pressure on the healthcare professionals.
3.4. Travel patterns
Pakistan is at high risk of transmission and spread of COVID‐19 due to its travel patterns. 86 , 87 Being a Muslim country, the majority of the Pakistani people visit religious places in Saudi Arabia and Iran for the Hajj/Umrah pilgrimage and other important religious events. This exposes Pakistani population to increased risk of COVID‐19 transmission, as evidenced by the fact that the majority of the confirmed cases of COVID‐19 had travel history to Iran. 40
Globalization is a multifaceted phenomenon and a driving force behind vibrant world economies. 88 Recognizing this, Pakistan has also established different sort of alliances with other nations around the globe, in particular with four border‐sharing countries, namely China, Iran, India and Afghanistan. As a result, a number of workers, scholars and commodities travel in and out of the country. 88 , 89 Therefore, in the current situation, when there is COVID‐19 pandemic, the threat of harm posed to our vulnerable nation by COVID‐19 tainted travelers is significant. For instance, the trade agreement with China has contributed to an influx of COVID‐19 infected individuals from this regional epicenter. 40 Although, in response to alerts from Chinese authorities, Pakistani government has taken preventive steps in line with the IHR‐2005 to prevent the entry of infection at the country's entry points, but has failed to prevent the contamination because of delays in enforcing immigration policies. 40 , 90
3.5. The current situation
The Federal Government of Pakistan, in collaboration with the Ministry of National Health Services Regulations and Coordination, has prepared “The National Action Plan for The Corona Virus Disease (COVID‐19) Pakistan” to better tackle the COVID‐19 epidemic. 40 Although, Pakistani government is demonstrating its dedication toward the threat of COVID‐19 and has taken a range of initiatives, the country is unable to take measures against COVID‐19 like those seen in China. There are currently only a few quarantine centers in Pakistan and these centers are overflowing with patients and consequently, the “one person one room” policy has been badly violated. 40 Significant concerns exist over availability of medicinal products, including protective equipment, essential medicines and ventilators. 91 , 92 The limited healthcare workforce combined with poor expertise further impedes the delivery of services needed for the standard management of patients. 40 In addition to existing workforce related issues, the morbidity and mortality of doctors and other healthcare workers has emerged as a new major concern. 93 As of 29 April 2020, the total number of infected medical workers in the country has risen to 444 (i.e., 216 doctors, 67 nurses and 161 healthcare staff). 94 Due to fear of being infected, some healthcare professionals have shown reluctance to handle presumptive COVID‐19 patients. In view of the increasing number of infected cases and lack of occupational safety measures and crucial protective suits for healthcare personnel, 40 , 93 a further shortage of emergency response teams is anticipated in the near future. Moreover, currently only few Pakistani hospitals have the facility to test COVID‐19 suspects. 40 Lapses in the screening system and resulting proliferation of COVID‐19 warrant the implementation of a more efficient system. 40 , 93 The ignorant and noncooperative attitude of patients and general public toward COVID‐19 response is further drastically endangering all governmental level efforts.
Apart from concerns about morbidity, mortality and economic loss associated with COVID‐19, there are significant concerns regarding the management of other communicable and non‐communicable diseases due to ongoing lockdown in the country. A number of factors indicate collapsed healthcare system, particularly shortage of healthcare workforce, poor infrastructure, limited availability of pharmacist at community settings and poor availability of essential medicines at drug retail outlets.94 21 , 38 , 55 , 70
4. CONCLUSION
The COVID‐19 is swiftly spreading in Pakistan. Although, low death rate due to COVID‐19 has been reported so far, but what is likely to happen in the near future is uncertain at this moment. Nevertheless, considering the vulnerable public health and healthcare system, and sudden upsurge of the infected cases, the country is definitely at high risk of morbidity and mortality associated with COVID‐19. A number of intertwined reasons that expose the Pakistani population at increased risk can be degraded into public related demurrals (i.e., poverty, poor literacy level, negligence, rural lifestyle, huge association with livestock industry and high prevalence of comorbidities), healthcare workforce related demurrals (i.e., poor caregiver to patient ratio, poor knowledge and training of healthcare professionals, poor teamwork and collaboration), organizational and regulatory voids (i.e., poor healthcare infrastructure, poor implementation of infection control strategies, limited access to essential medical products, poor surveillance system and budgetary constraints), and travel patterns (i.e., increased religious traveling patterns and globalization).
4.1. Recommendations
The current COVID‐19 situation and a number of vulnerabilities identified in this review warrants political leaders, religious figures, healthcare workforce (doctors, nurses, pharmacists and paramedics), scientists and the general public to unite together to take steps to counter this harrowing pandemic.
It is suggested that the regulators may consider examining and recognizing all the healthcare workforce related challenges and organizational and regulatory voids, and thereafter reinforce core capacities in workforce and monetary resources, surveillance, laboratory services and, especially, hospital preparedness for isolation and ventilation of patients. In this regard, the Pakistani National Institute of Health needs to play a more vigilant role not only in implementing protocols regarding COVID‐19 prevention, transmission and detection, but also in training of healthcare professionals.
To minimize the impact of community related demurrals, Pakistani government may need to improve the communication patterns through ensuring the easy interpretation of operational scientific research, changes in behavior, mental resilience, and fact checking and fighting fake news. 95 Until the danger has been overcome, inhibiting people's movement and social activities through strict lockdown should be seen as the most promising approach. Otherwise, Pakistan cannot afford to suffer altogether from increased morbidity and mortality and economic loss. Nevertheless, heading for full lockdown and then maintaining it would be a great challenge for Pakistani government due to socioeconomic impact.
Regarding travel patterns, it is vital that high‐risk countries like ours be adequately equipped with ample quantity of screening kits, and should not only revise the immigration policies, but also ensure their proper implementation to limit the further entry of COVID‐19 travelers in Pakistan.
Although, Pakistani government is utilizing all the available resources and demonstrating its dedication toward the threat of COVID‐19, we are of the opinion that Pakistan does not have the capacity to meet the required standards of care and address these issues on its own, so the international community is called upon to support Pakistan and like nations to mitigate the potential danger of COVID‐19 by providing all types of resources needed to respond to this outbreak.
CONFLICT OF INTEREST
The authors have no competing interests.
AUTHOR CONTRIBUTIONS
Both authors participated in all phases of the study, including study conceptualization, design, data analysis, visualization and draft writing.
Supporting information
Supporting information.
Biographies
Muhammad Atif is currently serving as Associate Professor (Pharmacy Practice) at the Department of Pharmacy, the Islamia University of Bahawalpur, Pakistan. He has supervised more than 30 MPhil (Pharmacy Practice) students. His core research interests include health services research, drug utilization studies, patient reported outcomes, antimicrobial resistance, pharmaceutical policy and practice and the study of pharmaco‐epidemiology related to infectious disease management, mainly tuberculosis. Muhammad Atif has authored more than 80 full length publications in reputable international journals with a current impact factor of more than 90. Out of the published articles, more than 40 articles are published as FIRST author. He has authored five book chapters in international books. Muhammad Atif's research contributions have expanded beyond the boundaries of Pakistan and he is working internationally with the researchers affiliated with many reputable universities from New Zealand, the United Kingdom, Malaysia and the United Arab Emirates. Besides this, he has presented research findings at various international peer‐reviewed conferences and national forums, and has also been granted a number of awards and travel grants. Aside from aforementioned responsibilities and accomplishments, Muhammad Atif also serves as an Associate Editor in the Journal of Pharmaceutical Policy and Practice, which is one of the leading journals in pharmaceutical policy.
Iram Malik, an emerging researcher from the Islamia University of Bahawalpur, Punjab, Pakistan, has completed her MPhil (2019) in the field of Pharmacy Practice. Currently, she is active with several research ventures. Her major research interests include access to medicines, pharmaceutical policy and practice, health services research, drug utilization studies, patient reported outcomes and the study of pharmaco‐epidemiology related to infectious disease management. Above all, her in‐depth research on medicines shortages filled the major research gap regarding inadequate access to essential and life saving medicines in Pakistan, and catapulted her into the limelight. Iram Malik has authored more than 10 full length publications in reputable international journals. These include, BMJ Open, Research in Social and Administrative Pharmacy, Infection and Drug Resistance, Therapeutic Innovation & Regulatory Science, Medicina, Journal of the Chinese Medical Association and BMC research notes. She has also contributed chapters in international books entitled “Encyclopedia of Pharmacy Practice and Clinical Pharmacy”, “Drug Safety in Developing Countries” and “Global Pharmaceutical Policy.” She has presented research findings at many national forums. She serves as an Editorial Team Member in the Journal of Pharmaceutical Policy and Practice, which is one owned by BMC.
Atif M, Malik I. Why is Pakistan vulnerable to COVID‐19 associated morbidity and mortality? A scoping review. Int J Health Plann Mgmt. 2020;35:1041–1054. 10.1002/hpm.3016
Contributor Information
Muhammad Atif, Email: phd1pharmacist_atif@yahoo.com, Email: muhammad.atif@iub.edu.pk.
Iram Malik, Email: iramalik686@gmail.com.
DATA ACCESSIBILITY
All data generated or analyzed during this study are included in this article.
REFERENCES
- 1. Kenneth M. Coronaviruses in the Limelight. J Infect Dis. 2005;191(4):489‐491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. de Wilde AH, Snijder EJ, Kikkert M, van Hemert MJ. Host factors in coronavirus replication. Curr Top Microbiol Immunol. 2017;419:1‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Coleman CM, Frieman MB. Coronaviruses: important emerging human pathogens. J Virol. 2014;88(10):5209‐5212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Poutanen SM, Low DE, Henry B, et al. Identification of severe acute respiratory syndrome in Canada. N Engl J Med. 2003;348(20):1995‐2005. [DOI] [PubMed] [Google Scholar]
- 5. Peiris J, Lai S, Poon L, et al. Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet. 2003;361(9366):1319‐1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hui DS, Zumla A. Severe acute respiratory syndrome: historical, epidemiologic, and clinical features. Infect Disease Clin. 2019;33(4):869‐889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gastanaduy PA. Update: severe respiratory illness associated with Middle East respiratory syndrome coronavirus (MERS‐CoV)—worldwide, 2012–2013. MMWR Morb Mortal Wkly Rep. 2013;62(23):480. [PMC free article] [PubMed] [Google Scholar]
- 8. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Clinical Features of Patients Infected with 2019 Novel Coronavirus in Wuhan. The Lancet: China; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hui DS, I Azhar E, Madani TA, et al. The continuing 2019‐nCoV epidemic threat of novel coronaviruses to global health — the latest 2019 novel coronavirus outbreak in Wuhan, China Int J Infect Diseases 2020;91:264‐266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. World Health Organization . Rolling updates on coronavirus disease (COVID‐19). Coronavirus disease 2019. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen. Accessed 05 April, 2020.
- 11. World Health Organization . Coronavirus disease (COVID‐19) Pandemic. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessed 05 April, 2020.
- 12. World Health Organization . Crimean‐Congo haemorrhagic fever in Pakistan: update. 2013. http://www.emro.who.int/pandemic-epidemic-diseases/news/crimean-congo-haemorrhagic-fever-in-pakistan-update.html. Accessed 05 April, 2020.
- 13. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus‐infected pneumonia in Wuhan, China. Jama. 2020;323(11):1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. World Health Organization . Novel Coronavirus (2019‐nCoV) advice for the public. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public. Accessed 05 April, 2020.
- 15. Centre for Disease Control and Prevention . Prevention & Treatment. Novel Coronavirus 2019. 2020. https://www.cdc.gov/coronavirus/2019-ncov/about/prevention-treatment.html. Accessed 05 April, 2020.
- 16. The United Nations Development Programme . Human Development Report 2019. Beyond income, beyond averages, beyond today: Inequalities in human development in the 21st century New York, USA. New York, USA: The United Nations Development Programme; 2019. [Google Scholar]
- 17. World Health Organization . Coronavirus disease 2019 (COVID‐19) Situation Report – 43. 2020; https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200303-sitrep-43-covid-19.pdf?sfvrsn=2c21c09c_2. Accessed 01 April, 2020.
- 18. Morens DM, Folkers GK, Fauci AS. The challenge of emerging and re‐emerging infectious diseases. Nature. 2004;430(6996):242‐249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ministry of Finance . Economic Survey 2018–19. Pakistan: Finance Division, Government of Pakistan; 2019. [Google Scholar]
- 20. Atif M, Malik I, Asif M, Qamar‐Uz‐Zaman M, Ahmad N, Scahill S. Drug safety in Pakistan. In: Al‐Worafi Y, ed. Drug Safety in Developing Countries: Achievements and Challenges. India: Elsevier; 2020:686. [Google Scholar]
- 21. Atif M, Ahmad M, Saleem Q, Curley L, Qamar‐uz‐Zaman M. Pharmaceutical policy in Pakistan. Pharmaceutical Policy in Countries with Developing Healthcare Systems. Switzerland: Springer; 2017:25‐44. [Google Scholar]
- 22. World Health Organization . Circulating vaccine‐derived poliovirus type 2 – Pakistan. 2019. https://www.who.int/csr/don/28-november-2019-polio-pakistan/en/.
- 23. World Health Organization . HIV cases–Pakistan. 2019. https://www.who.int/csr/don/03-july-2019-hiv-cases-pakistan/en/.
- 24. World Health Organization . 15 million people affected with hepatitis B and C in Pakistan: Government announces ambitious plan to eliminate hepatitis. 2019. https://www.who.int/hepatitis/news-events/pakistan-hepatitis-elimination-plan/en/.
- 25. Khan H, Ahmad I. Internally displaced persons and health challenges. Gomal J Med Sci. 2014;12(2):1‐764. [Google Scholar]
- 26.Federal Disease Surveillance and Response Unit. Weekly field epidemiology report Pakistan: National Institute of Health, 2020. [Google Scholar]
- 27. Khalil AT, Ali M, Tanveer F, et al. Emerging viral infections in Pakistan: issues, concerns, and future prospects. Health Secur. 2017;15(3):268‐281. [DOI] [PubMed] [Google Scholar]
- 28. World Health Organization . Coronavirus disease 2019 (COVID‐19) Situation Report – 38. 2020; https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200227-sitrep-38-covid-19.pdf?sfvrsn=9f98940c_2. Accessed 3 April, 2020. [Google Scholar]
- 29. Ministry of National Health Services Regulations & Coordination . KNOW ABOUT COVID‐19: See the Realtime Pakistan and Worldwide COVID‐19 situation! 2020. http://covid.gov.pk/. Accessed 25 April, 2020.
- 30. The News . WHO warns Pakistan's COVID‐19 cases can surge to 200,000 by mid July. The News. 2020. https://www.thenews.com.pk/latest/648722-who-warns-pakistans-covid-19-cases-can-surge-to-200000-by-mid-july
- 31. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Social Res Methodol. 2005;8(1):19‐32. [Google Scholar]
- 32. Rumrill PD, Fitzgerald SM, Merchant WR. Using scoping literature reviews as a means of understanding and interpreting existing literature. Work (Reading, Mass). 2010;35(3):399‐404. [DOI] [PubMed] [Google Scholar]
- 33. Atif M, Saqib A, Ikram R, Sarwar MR, Scahill S. The reasons why Pakistan might be at high risk of Crimean Congo haemorrhagic fever epidemic; a scoping review of the literature. Virol J. 2017;14(1):63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ilie G, Ciocoiu CN. Application of fishbone diagram to determine the risk of an event with multiple causes. Manage Res Practice. 2010;2(1):1‐20. [Google Scholar]
- 35. Bhutta ZA, Salam RA, Das JK, Lassi ZS. Tackling the existing burden of infectious diseases in the developing world: existing gaps and the way forward. Infect Dis Poverty. 2014;3:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Shah AA, Abid M, Ye J. An Assessment of Primary Health Care Facilities and their Preparedness Level in Khyber Pakhtunkhwa Province of Pakistan: Strengths, Weaknesses, Opportunities, and Threats (SWOT). Public Health and Disasters. Switzerland: Springer; 2020:245‐264. [Google Scholar]
- 37. The World Bank . Rural population (% of total population) ‐ Pakistan. 2019. https://data.worldbank.org/indicator/SP.RUR.TOTL.ZS?locations=PK.
- 38. Atif M, Rasheed W, Mushtaq I, Malik I, Kanwal S, Qamar‐Uz‐Zaman M. Medication related knowledge and practices among patients attending pharmacies in Bahawalpur, Pakistan: a cross‐sectional study. Lat Am J Pharm. 2019;38(7):1404‐1415. [Google Scholar]
- 39. Aziz MM, Masood I, Yousaf M, Saleem H, Ye D, Fang Y. Pattern of medication selling and self‐medication practices: a study from Punjab, Pakistan. PLoS One. 2018;13(3):e0194240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Javed B, Sarwer A, Soto EB, Mashwani Z‐U‐R. Is Pakistan on track to have COVID‐19 transmission and mortality rates similar to those of Italy, Iran or the USA? Drugs Ther Perspect. 2020;1‐5. 10.1007/s40267-020-00726-w. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Qazi A, Qazi J, Naseer K, et al. Analyzing situational awareness through public opinion to predict adoption of social distancing amid pandemic COVID‐19. J Med Virol. 2020;92(7):849‐855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Saqlain M, Munir MM, Rehman SU, et al. Knowledge, attitude, practice and perceived barriers among healthcare professionals regarding COVID‐19: a cross‐sectional survey from Pakistan. J Hosp Infect. 2020;105(3):419‐423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. National Institute Of Health . Field Epidemiology & Disease Surveillance Division (FE&DSD). 2020. https://www.nih.org.pk/field-epidemiology-disease-surveillance-division-fedsd/.
- 44. Robertson D, Jiang X. Relationship to bat coronaviruses and recombination signals no snakes. 2020. http://virological.org/t/ncovs-relationship-to-bat-coronaviruses-recombination-signals-no-snakes/331. Accessed 5 April, 2020.
- 45. Rafique I, Saqib MA, Munir MA, et al. Prevalence of risk factors for noncommunicable diseases in adults: key findings from the Pakistan STEPS survey. East Mediterr Health J. 2018;24(1):33‐41. [PubMed] [Google Scholar]
- 46. Sarwar MR, Atif M, Scahill S, Saqib A, Qamar‐uz‐Zaman M, Babar Z. Drug utilization patterns among elderly hospitalized patients on poly‐pharmacy in Punjab, Pakistan. J Pharmaceut Policy Practice. 2017;10(1):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Gralinski LE, Menachery VD. Return of the coronavirus: 2019‐nCoV. Viruses. 2020;12(2):135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Ul‐Haq Z, Shah BH, Ardakani M, et al. Health system preparedness in Pakistan for crisis management: a cross‐sectional evaluation study. East Mediterr Health J. 2019;25(8):553‐561. [DOI] [PubMed] [Google Scholar]
- 49. Rehman IU, Bukhsh A, Khan TM. Measles in Pakistan: time to make steps towards eradication. Travel Med Infect Dis. 2017;18:67‐69. [DOI] [PubMed] [Google Scholar]
- 50. Punjwani R, Khatoon A, Fatima D, Ahmed A. Practices and policies of infection control and prevention, Pakistan‐a review for patient safety. Med Safety Global Health. 2016;5:1‐5. [Google Scholar]
- 51. Sarwar MR, Saqib A, Iftikhar S, Sadiq T. Antimicrobial use by WHO methodology at primary health care centers: a cross sectional study in Punjab, Pakistan. BMC Infect Dis. September 29, 2018 2018;18(1):492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Rao MH, Arain GM, Khan MI, et al. Assessment of knowledge, attitude and practices pattern of hand washing in some major public sector hospitals of Pakistan (a multi‐center study). Pakistan J Med Res. 2012;51(3):76‐83. [Google Scholar]
- 53. Shah AA, Shaw R, Ye J, et al. Current capacities, preparedness and needs of local institutions in dealing with disaster risk reduction in Khyber Pakhtunkhwa, Pakistan. Int J Disaster Risk Reduction. 2019;34:165‐172. [Google Scholar]
- 54. Ullah S, Latif N, Nasre Alam A, Zaman T. Challenges of hospital preparedness in disasters in Balochistan. Pakistan J Public Health. 2017;7(1):30‐37. [Google Scholar]
- 55. Zaidi S, Bigdeli M, Aleem N, Rashidian A. Access to essential medicines in Pakistan: policy and health systems research concerns. PLoS One. 2013;8(5):e63515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Sabih F, Bile K, Buehler W, Hafeez A, Nishtar S, Siddiqi S. Implementing the district health system in the framework of primary health care in Pakistan: Can the evolving reforms enhance the pace towards the millennium development goals? East Mediterr Health J 2010;16(supplement):S132‐S144. [PubMed] [Google Scholar]
- 57. Akram M, Khan FJ. Health care services and government spending in Pakistan. Islamabad, Pakistan: Pakistan Institute of Development Economics; 2007:1‐31. [Google Scholar]
- 58. Elahi N, Nyborg ILP, Nawab B. Participatory development practices: A critical analysis of gender empowerment and development in pre‐ and post‐crises swat, Pakistan. Forum Dev Stud. 2015;42(2):333‐356. [Google Scholar]
- 59. Shaikh BT. Health systems research in Pakistan: issues, challenges and way forward. J Ayub Med Coll Abbottabad. 2015;27(2):257‐258. [PubMed] [Google Scholar]
- 60. Waris A, Khan AU, Ali M, Ali A, Baset A. COVID‐19 outbreak: current scenario of Pakistan. New Microbes New Infect. 2020;35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Saeed DK, Hasan R, Naim M, et al. Readiness for antimicrobial resistance (AMR) surveillance in Pakistan; a model for laboratory strengthening. Antimicrob Resist Infect Control. 2017;6(1):101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Guerin PJ, Singh‐Phulgenda S, Strub‐Wourgaft N. The consequence of COVID‐19 on the global supply of medical products: why Indian generics matter for the world? F1000Research. 2020;9(225):225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Global Health Security Index . 2019. GHS index country profile Pakistan. 2019. https://www.ghsindex.org/country/pakistan/.
- 64. The World Bank . Current health expenditure (% of GDP) ‐ Pakistan. 2017. https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS?locations=PK.
- 65. Khalid F, Abbasi AN. Challenges faced by Pakistani healthcare system: Clinician's perspective. J College Phys Surg Pakistan. 2018;28(12):899‐901. [DOI] [PubMed] [Google Scholar]
- 66. World Health Organization . WHO country cooperation strategy at a glance: Pakistan. Geneva: World Health Organization; 2018. [Google Scholar]
- 67. Ministry of National Health Services, Regulations & Coordination . Pakistan: Human Resources for Health Vision 2018–30. Pakistan: Ministry of National Health Services, Regulations & Coordination; 2018. Available from http://phkh.nhsrc.pk/sites/default/files/2019-06/Pakistan%20Human%20Resources%20for%20Health%20Vision%202018.pdf. [Google Scholar]
- 68. Saqib A, Atif M, Ikram R, Riaz F, Abubakar M, Scahill S. Factors affecting patients' knowledge about dispensed medicines: A Qualitative study of healthcare professionals and patients in Pakistan. PloS one. 2018;13(6):e0197482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Atif M, Sarwar MR, Azeem M, Naz M, Amir S, Nazir K. Assessment of core drug use indicators using WHO/INRUD methodology at primary healthcare centers in Bahawalpur, Pakistan. BMC Health Serv Res. 2016;16(1):684‐684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Atif M, Sarwar MR, Azeem M, et al. Assessment of WHO/INRUD core drug use indicators in two tertiary care hospitals of Bahawalpur, Punjab, Pakistan. J Pharm Policy Pract. 2016;9(1):27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Malik I, Atif M. Global menace of superbugs: time to consider a "pharmacist led one health approach" to counteract the crisis. Res Social Admin Pharmacy. Jun 2020;16(6):848‐849. [DOI] [PubMed] [Google Scholar]
- 72. Atif M, Asghar S, Mushtaq I, Malik I. Community pharmacists as antibiotic stewards: a qualitative study exploring the current status of antibiotic stewardship program in Bahawalpur, Pakistan. J Infect Public Health. 2019;13(1):118‐124. [DOI] [PubMed] [Google Scholar]
- 73. Atif M, Razzaq W, Mushtaq I, et al. Pharmacy services beyond the basics: a qualitative study to explore perspectives of pharmacists towards basic and enhanced pharmacy Services in Pakistan. Int J Environ Res Public Health. 2020;17(7):2379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. World Health Organization . Joint External Evaluation of IHR Core Capacities of the Islamic Republic of Pakistan. Geneva: World Health Organization; 2017:73. [Google Scholar]
- 75. Parvez MK, Parveen S. Evolution and emergence of pathogenic viruses: past, present, and future. Intervirology. 2017;60(1–2):1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Khan S, Khan M, Maqsood K, Hussain T, Noor‐ul‐Huda, Zeeshan M. Is Pakistan prepared for the COVID‐19 epidemic? A questionnaire‐based survey. J Med Virol. 2020;92(7):824‐832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Malik I, Ikram H, Rafiq S. 71st anniversary of pharmacy profession in Pakistan: why pharmacists' are still flying under the radar? Res Social Admin Pharmacy. 2019;15(12):1495‐1496. [DOI] [PubMed] [Google Scholar]
- 78. San Martín‐Rodríguez L, Beaulieu M‐D, D'Amour D, Ferrada‐Videla M. The determinants of successful collaboration: a review of theoretical and empirical studies. J Interprof Care. 2005;19:132‐147. [DOI] [PubMed] [Google Scholar]
- 79. Reller LB, Weinstein MP, Peterson LR, et al. Role of clinical microbiology laboratories in the management and control of infectious diseases and the delivery of health care. Clin Infect Dis. 2001;32(4):605‐610. [DOI] [PubMed] [Google Scholar]
- 80. Gardner LM, Chughtai AA, MacIntyre CR. Risk of global spread of Middle East respiratory syndrome coronavirus (MERS‐CoV) via the air transport network. J Travel Med. 2016;23(6):taw063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Ahmad T, Khan M, Malik S. Re‐emergence of Congo virus in Pakistan: call for preparedness. Biomed Res Therapy. 2016;3(08):742‐744. [Google Scholar]
- 82. Hassan ST, Xia E, Huang J, Khan NH, Iqbal K. Natural resources, globalization, and economic growth: evidence from Pakistan. Environ Sci Pollut Res. 2019;26(15):15527‐15534. [DOI] [PubMed] [Google Scholar]
- 83. World Health Organization . Measles – Global situation. 2019. https://www.who.int/csr/don/26-november-2019-measles-global_situation/en/. Accessed 5 April, 2020.
- 84. Mukhtar F, Mukhtar N. Coronavirus (COVID‐19): LET'S prevent not panic. J Ayub Med Coll Abbottabad. 2020;32(1):141‐144. [PubMed] [Google Scholar]
- 85. Waris A, Atta UK, Ali M, Asmat A, Baset A. COVID‐19 outbreak: current scenario of Pakistan. New Microbes New Infect. 2020;35:100681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Saqlain M, Munir MM, Ahmed A, Tahir AH, Kamran S. Is Pakistan prepared to tackle the coronavirus epidemic? Drugs Therapy Perspect. 2020;36(5):213‐214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Nafees M, Khan F. Pakistan's response to COVID‐19 pandemic and efficacy of quarantine and partial lockdown: a review. Electron J Gen Med. 2020;17(2):emXXX. [Google Scholar]
- 88. Tahir N. 26‐Year‐Old Doctor Dies Due to Coronavirus in Rawalpindi. 2020. https://www.dawn.com/news/1554002/26-year-old-doctor-dies-due-to-coronavirus-in-rawalpindi.
- 89. Correia T. SARS‐CoV‐2 pandemics: the lack of critical reflection addressing short‐ and long‐term challenges. Int J Health Plann Manage. 2020;35(3):669‐672. [DOI] [PubMed] [Google Scholar]
- 90. Atif M, Malik I. COVID‐19 and community pharmacy services in Pakistan: challenges, barriers and solution for progress. J Pharm Policy Pract. 2020;13(1):33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Malik I, Atif M, Scahill S, Babar ZUD. Pharmacy Practice and Policy Research in Pakistan: A Review of Literature Between 2014 and 2019. Babar Z.U.D, Global Pharmaceutical Policy. United Kingdom: Palgrave Macmillan; 2020:139‐175. [Google Scholar]
- 92. Ikram R, Saqib A, Mushtaq I, Atif M. Scope of improvement in the functioning of national regulatory authority—A step toward international accreditation: A qualitative study from Pakistan. Ther Innov Regul Sci. 2019;53(6):787‐794. [DOI] [PubMed] [Google Scholar]
- 93. Malik I, Atif M, Riaz F, Asghar S, Ahmad N. Pediatric antibiotic pack size compliance with the dosage regimen: A descriptive study. Ther Innov Regul Sci. 2020;54(3):492‐506. 10.1007/s43441-019-00081-7. [DOI] [PubMed] [Google Scholar]
- 94. Atif M, Malik I, Mushtaq I, Asghar S. Medicines shortages in Pakistan: a qualitative study to explore current situation, reasons and possible solutions to overcome the barriers. BMJ Open. 2019;9(9):e027028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Atif M, Azeem M, Rehan Sarwar M, et al . Evaluation of prescription errors and prescribing indicators in the private practices in Bahawalpur, Pakistan. J Chin Med Assoc. 2018;81(5):444‐449. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Data Availability Statement
All data generated or analyzed during this study are included in this article.


