Abstract
Background
Multiple professional bodies have temporarily revised recommendations for gestational diabetes mellitus (GDM) testing during the COVID‐19 pandemic to reduce person‐to‐person contact. The current Australian temporary criteria advise that if the fasting glucose is ≤4.6 mmol/L, then no glucose tolerance test (GTT) is required.
Aims
The aim of this study is to examine the extent of underdiagnosis of GDM using a fasting glucose ≤4.6 mmol/L as a cut‐off to determine that a GTT is not necessary.
Materials and Methods
De‐identified data from pregnant women having a GTT test in the Illawarra area during a six‐year period was used to determine the number of women with GDM and the proportion of positive cases that would be missed for different fasting glucose values.
Results
There were 16 522 results identified and GDM was diagnosed in 12.2%. The majority of women were more than 30 years of age (85.2%) and diagnosed at ≥20 weeks gestation (81.1%). Of those diagnosed with GDM, 29% had a fasting glucose of ≤4.6 mmol/L and would have been missed.
Conclusions
Our results show that using a fasting glucose of 4.6 mmol/L or less would miss nearly a third of women who would otherwise be diagnosed with GDM.
Keywords: COVID‐19, gestational diabetes, pregnancy, screening
Introduction
Gestational diabetes mellitus (GDM) is a very common medical problem found in pregnancy. The Australasian Diabetes in Pregnancy Society (ADIPS) 1 recommends that all women in every pregnancy be tested, ideally using a two‐hour glucose tolerance test (GTT). The diagnostic criteria come from recommendations of the World Health Organization (WHO) which were based on the results of the Hyperglycaemia and Pregnancy Outcomes study (HAPO). 2 In Australia, in a nationally representative population, the prevalence of hyperglycaemia in pregnancy (HIP) was found to be 13.1% with 0.4% having diabetes in pregnancy (DIP) and 12.7% having GDM. 3 Testing in centres or regions with a higher number of women with risk factors is likely to show a higher prevalence.
While so far with the COVID‐19 pandemic there appear to be no concerns with the outcome of pregnancies, 4 it would be potentially prudent to reduce the number of women requiring a GTT in order to reduce person‐to‐person contact and limit the time spent in a health service environment. While the WHO has not made any recommendations about simplifying the diagnostic process, 5 multiple professional bodies, including those from Australia, 6 Canada, 7 and the United Kingdom, 8 have temporarily revised their recommendations for testing.
The current ADIPS temporary criteria during the COVID‐19 pandemic are based on the Queensland Clinical Guidelines. 9 These recommend a HbA1c in the first trimester for women with risk factors and, for women not diagnosed with GDM, a fasting glucose at 24–28 weeks gestation. If the fasting glucose is ≥5.1 mmol/L, then a diagnosis of GDM is established. If the fasting glucose is ≤4.6 mmol/L, then no GTT is required. Only if the fasting glucose is 4.7–5.0 mmol/L is a GTT recommended.
It is inevitable that not proceeding to a GTT for women with a fasting glucose ≤4.6 mmol/L will underdiagnose GDM. The purpose of the study herein reported is to examine the extent of this underdiagnosis.
Materials and Methods
This study was conducted in the Illawarra area centred around the city of Wollongong. The area is very suitable for epidemiological research as it has a population of about 300 000 and is geographically defined and confined. For obstetric care there is one public and one private hospital. The overall population is very similar to Australia as a whole with respect to country of birth and indigenous origin (2.9% vs 2.8%). For women, the percentage aged 20–44 years (31.4%) is similar to Australia overall (34.3%). For women aged 20–44 years born outside of Australia, the five major countries of origin are similar to Australia as a whole (China, England, India, New Zealand and The Philippines). 10 , 11
There is one dominant private pathology provider in the area who conducts most of the tests for both women who will be attending the public hospital and those who are receiving care in the private sector. De‐identified data from all pregnant women having a GTT for a six‐year period between December 2013 and December 2019 were provided by the private laboratory with year of birth and gestational week of testing. These data included the results of the fasting, one‐hour and two‐hour glucose levels after a GTT.
The data were analysed to determine the number of women with GDM and the distribution of these positive tests for maternal age and gestational week. The proportion of positive cases missed for different fasting glucose from 3.5 to 5.0 mmol/L was calculated using a 95% confidence interval for proportions.
Ethics approval
This audit conforms to the standards established by the National Health and Medical Research Council for ethical quality. The University of Wollongong and Illawarra Shoalhaven Local Health District Health and Medical Human Research Ethics Committee did not require the audit herein reported to be reviewed. 12
Results
In total 16 552 results for the 75 g oral GTT during pregnancy were identified over this six‐year period. There were 289 records (1.7%) with some missing data and these were not considered further. Of the remaining 16 263 results, HIP was diagnosed in 2031 (12.5%) women of whom 39 (0.2%) had DIP and were not considered further. There were 1992 women with GDM (12.2%) and these were considered in further analyses.
Of the 1992 women with GDM, 1087 (54.6%) had an abnormal fasting level (≥5.1 mmol/L), 395 (19.8%) were diagnosed on the one‐hour glucose (≥10.0 mmol/L) level alone, 324 (16.3%) on the two‐hour glucose (≥8.5 mmol/L) alone and 186 (9.3%) had both elevated one‐ and two‐hour glucose levels.
Of women diagnosed with GDM, 376 (18.9%) were at <20 weeks gestation and 1616 (81.1%) were diagnosed at ≥20 weeks gestation. Most women diagnosed with GDM were aged more than 30 years (85.2%).
Of the 1992 women diagnosed with GDM, 596 (29%; 95% CI 28.0–32.0%) had a fasting glucose of ≤4.6 mmol/L and would have been missed. The percentage of cases of GDM missed for different fasting glucose levels from 3.5 to 5.0 mmol/L with 95% CI are shown in Figure 1. As an example, based on these data, the cut‐off for the fasting glucose required to pick up at least 95% of GDM cases would be ≥4.0 mmol/L.
Figure 1.
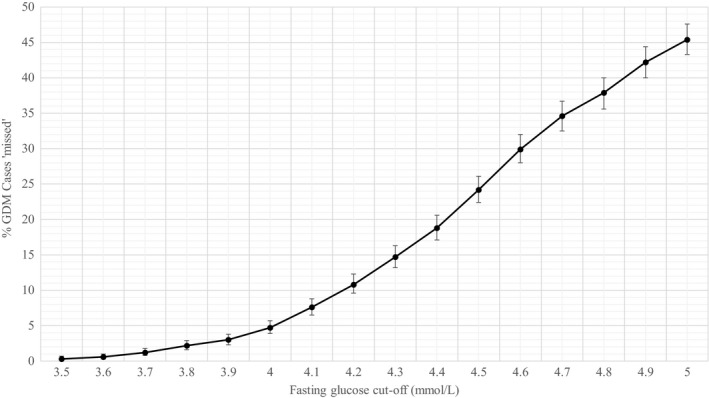
Percentages of gestational diabetes mellitus (GDM) positive cases that would be missed for different fasting glucose cut‐offs if each cut‐off was used to determine no need for a glucose tolerance test (95% confidence intervals).
Discussion
The temporary COVID‐19 pandemic revised guidelines for the diagnostic pathway of pregnant women being tested for GDM will certainly reduce the number of women being potentially exposed but will miss about a third of all cases. Perhaps women with a low fasting level but diagnostic one and/or two‐hour levels may be in a lower risk group for adverse pregnancy outcomes but there is limited data available on this. In 2019 McIntyre et al. 13 presented data from five of the HAPO sites and found that 25% of women with a fasting glucose <4.6 mmol/L had GDM but their outcomes were similar to women who were not diagnosed with GDM. The ethnicity of the women at these HAPO sites was not detailed and may not necessarily be relevant to an Australia population.
The strengths of the study herein reported are that it involved a large number of results and included women who were being treated in both the public and private sectors. This is important as approximately 25% of women elect to use the private system and their details and results are not often recorded or included in analyses. It also used a population that had a very similar demographic to Australia as a whole with respect to ethnicity and age. The results of GDM testing may vary greatly, with a lower or higher prevalence, if populations at different risks of GDM are considered.
As this was a retrospective audit looking at de‐identified data, we are not able to factor in other variables and risk factors for GDM, such as previous GDM, family history and maternal body mass index and so on.
It would be ideal to limit the number of women requiring a GTT during a pandemic to reduce the risk of exposure. However, this must be weighed against potential adverse outcomes secondary to undiagnosed and possibly poorly controlled GDM. Our results show that using a fasting glucose of 4.6 mmol/L or less would miss nearly a third of women who would otherwise be diagnosed with GDM. Ideally, before choosing a diagnostic pathway, a woman’s individual risk should be taken into consideration as well as her personal preference for testing knowing the potential for a missed diagnosis. This would need to be done on an individual basis by the obstetric care provider. On the other hand, it is acknowledged that the guidelines are temporary, advisory and not obligatory and under the current circumstances can be deemed both reasonable and responsible. Data from selected HAPO sites 13 did find that women with GDM but with a fasting glucose of <4.6 mmol/L did have a lower rate of large for gestational age infants and caesarean sections. More data are required in an Australian population to examine whether women with lower fasting levels, or in effect women who are diagnosed on the post‐glucose load results, have lower obstetric and perinatal risks. It is possible that data obtained during the temporary COVID‐19 changes may be relevant to revising the recommended ADIPS criteria for the future.
Conflicts of Interest: The authors report no conflicts of interest.
References
- 1. ADIPS Consensus Guidelines for the Testing and Diagnosis of Hyperglycaemia in Pregnancy in Australia and New Zealand (modified November 2014). [Accessed 17 April 2020.] Available from URL: http://www.adips.org/downloads/2014ADIPSGDMGuidelinesV18.11.2014_000.pdf
- 2. HAPO Collaborative Research Group . Hyperglycemia and adverse pregnancy outcomes. N Engl J Med 2008; 358: 1991–2002. [DOI] [PubMed] [Google Scholar]
- 3. Moses R, Wong V, Lambert K et al. The prevalence of hyperglycaemia in pregnancy in Australia. Aust N Z J Obstet Gynaecol 2016; 56: 341–345. [DOI] [PubMed] [Google Scholar]
- 4. Poon LC, Yang H, Kapur A et al. Global interim guidance on coronavirus disease 2019 (COVID‐19) during pregnancy and puerperium from FIGO and allied partners: information for healthcare professionals. Int J Gynecol Obstet 2020; 149(3): 273–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. McIntyre HD, Moses RG. The diagnosis and management of gestational diabetes mellitus in the context of the COVID‐9 pandemic. Diabetes Care 2020; 43: 1433–1434 [DOI] [PubMed] [Google Scholar]
- 6. Diagnostic testing for gestational diabetes mellitus (GDM) during the COVID 19 pandemic: Antenatal and postnatal testing advice. Joint statement from the Australasian Diabetes in Pregnancy Society, the Australian Diabetes Society, the Australian Diabetes Educators Association and Diabetes Australia. [Accessed 16 April 2020.] Available from URL: https://www.adips.org/documents/COVID‐19GDMDiagnosis030420ADIPSADSADEADAforWebsite.pdf
- 7. Urgent update – temporary alternative screening strategy for gestational diabetes screening during the COVID‐19 pandemic. A joint consensus statement from the Diabetes Canada Clinical Practice Guidelines Steering Committee and the Society of Obstetricians and Gynaecologists of Canada. [Accessed 17 April 2020.] Available from URL: https://els‐jbs‐prod‐cdn.jbs.elsevierhealth.com/pb/assets/raw/Health%20Advance/journals/jcjd/JCJD_COVID_guidelines_020420‐1585856697530.pdf
- 8. Guidance for maternal medicine services in the evolving coronavirus (COVID‐19) pandemic. Royal College of Obstetricians and Gynaecologists Version 1.1. [Accessed 17 April 2020.] Available from URL: https://www.rcog.org.uk/globalassets/documents/guidelines/2020‐04‐03‐guidance‐for‐maternal‐medicine.pdf
- 9. Queensland Clinical Guidelines . Gestational Diabetes Mellitus. Notice of Update During COVID‐19 Pandemic. [Accessed 18 April 2020.] Available from URL: https://www.health.qld.gov.au/__data/assets/pdf_file/0022/950503/g‐gdm.pdf
- 10. 2016 Census Community Profiles – Illawarra Code 107 (SA4). [Accessed 18 April 2020.] Available from URL: https://quickstats.censusdata.abs.gov.au/census_services/getproduct/census/2016/communityprofile/107?opendocument
- 11. 2016 Census Community Profiles – Australia Code 0 (AUST). [Accessed 18 April 2020.] Available from URL: https://quickstats.censusdata.abs.gov.au/census_services/getproduct/census/2016/communityprofile/036?opendocument
- 12. Ethical Considerations in Quality Assurance and Evaluation Activities, NHMRC March 2014. [Accessed 25 April 2020.] Available from URL: https://www.nhmrc.gov.au/sites/default/files/documents/attachments/ethical‐considerations‐in‐quality‐assurance‐and‐evaluation‐activites.pdf
- 13. McIntyre H, Gibbons KS, Sacks DA et al. Using fasting plasma glucose to identify women with gestational diabetes at low risk of complications. Diabetologia 2019; 62(Suppl 1): S79. [Google Scholar]


