Abstract
The nuance of operative decision making for those in need of emergent operation during coronavirus disease 2019 (COVID‐19) pandemic is increasingly complex in the absence of robust data or guidelines. We present two cases of thoracic aortic emergencies with COVID‐19 disease who survived high‐risk operations to highlight the potential for successful outcomes even in situations compounding patient disease, morbid operation, and the added risk associated with virulent disease in the pandemic time.
Keywords: aortic dissection, aortic surgery, COVID‐19, intramural hematoma
1. INTRODUCTION
Even with the abrupt decline in the number of patients presenting with acute conditions during the coronavirus disease 2019 (COVID‐19) pandemic, 1 the sickest and the most acute patients continue to require appropriate care, including high‐risk operations. Given the morbidity of the operation now compounded with the risk of contracting or suffering from the highly virulent severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) in the postoperative vulnerable period, the operative decision making has become all the more complex, 2 with one existing report of a patient with acute type A dissection and COVID‐19 disease resulting in operative mortality. 3 We encountered two cases of surgical thoracic aortic emergencies, one undergoing an operation with known COVID‐19 positive status and another undergoing an operation and contracted COVID‐19 in the postoperative period. Both patients survived and recovered well to demonstrate the potential value in pursuing aggressive surgical treatment even in the nuanced context of increased postoperative risk of succumbing to this lethal COVID‐19 disease.
2. CASES
The first patient is a 54‐year‐old man who was otherwise without comorbidity who presented with a sudden onset chest pain and found to have intramural hematoma involving the aortic root and ascending aorta on computed tomography (CT) (Figure 1). The patient had a family history of thoracic aortic aneurysm and dissection. Patient reported symptoms suggestive of COVID‐19 disease although never tested before this visit. He also had social contact with an individual who tested positive for COVID‐19. Patient denied any respiratory symptoms on presentation but the SARS‐CoV‐2 polymerase chain reaction test returned positive. CT findings of bilateral ground‐glass opacities in the lung were also suggestive of a history of COVID‐19 disease (Figure 1). Given the intramural hematoma in the aortic root and ascending aorta, patient was taken emergently to the operating room designated for COVID‐19 positive patients.
Figure 1.
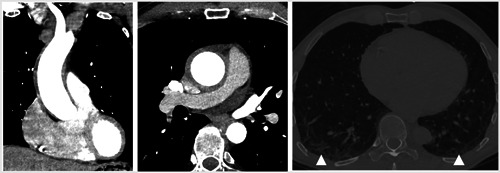
Preoperative computed‐tomography scans of patient 1. The figure shows intramural hematoma involving the aortic root and ascending aorta (left), axial view (middle), and ground‐glass opacities (white arrow, right image) in the bilateral lower lobes of the lung suggestive of a sequela of respiratory disease
Through median sternotomy, the patient was cannulated centrally and cooled to 18°C for deep hypothermic circulatory arrest (DHCA) and retrograde cerebral perfusion. Following an aortotomy, the primary tear site above the right coronary artery ostium was observed without coronary dissections (Figure 2). The patient had a dilated root (52 mm) with extensive intramural hematoma involvement. The aortic valve was trileaflet without significant structural pathology and appropriate geometric heights. Because of the dilated root, a valve‐sparing root reimplantation was performed using a 30‐mm Dacron Valsalva graft (Terumo Aortic, Somerset, NJ) with direct reimplantation of the coronary buttons. A hemiarch replacement using a 26‐mm Dacron straight graft (Terumo Aortic) was used to replace the ascending aorta and lesser curvature of the aortic arch, effectively resecting all aortic pathologic segments. The patient had difficulty coming off cardiopulmonary bypass with isolated left ventricular dysfunction, at which time a saphenous vein was harvested and used to bypass to the left anterior descending artery. Following the bypass grafting, he had normal biventricular function and came off cardiopulmonary bypass easily. The recovery course was uneventful, the aortic valve was competent without any leak with mean gradient of 6mm Hg on postoperative echocardiography. The patient was discharged to home on postoperative day 6. Postoperative CT angiogram showed intact surgical repair without any residual dissection.
Figure 2.
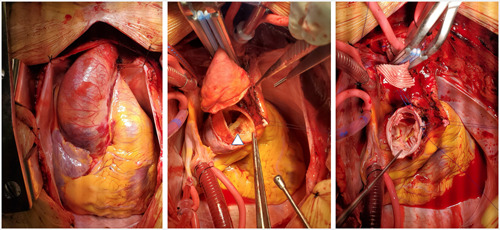
Operative images. Figures show enlarged aorta with intramural hematoma (left), aortic root with the entry tear (middle) with white triangle indicating the tear, and reconstructed aortic root and reimplanted aortic valve (right)
The second patient is an 82‐year‐old woman with history of paroxysmal atrial fibrillation, diastolic heart failure, chronic obstructive pulmonary disease on steroids, and pacemaker for sick sinus syndrome, who presented with sudden onset chest pain and facial weakness, anuria and acute kidney injury, and found to have acute type A aortic dissection (Figure 3). She presented at the time when COVID test was not routinely available and she was without symptoms suggestive of COVID‐19. Patient was taken to the operating room where the transesophageal echocardiogram revealed a dissection flap in the ascending aorta with severe aortic insufficiency. Through median sternotomy, she was placed on cardiopulmonary bypass, and was cooled to 18°C for DHCA with retrograde cerebral perfusion. There was a primary tear in the proximal ascending aorta. The dissection flap extended into the right, noncoronary, and left coronary sinuses. The aortic valve was grossly intact. The aortic valve was resuspended at the level of the commissures with horizontal mattress pledgeted sutures. The coronary sinuses were reconstructed using the felt and bioglue neomedia technique. The ascending aorta and hemiarch were replaced with a Dacron Gelweave graft (Terumo Aortic).
Figure 3.
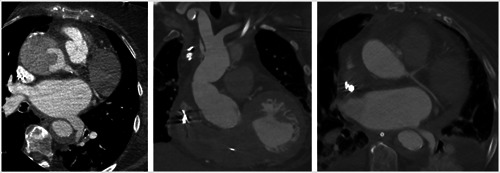
Pre‐ and postoperative computed‐tomography scans of patient 2. Figures show axial view of the dissected aortic root and descending aorta (left), postoperative coronal scan of the ascending aorta (middle), and an axial view of postoperative aortic root and descending aorta (right)
Postoperatively, she had complete neurologic recovery. Her course was complicated by renal failure requiring dialysis. She was discharged on postoperative day 30 but was readmitted from rehabilitation facility on postoperative day 66 for respiratory illness at which time she tested positive for COVID‐19 disease. She required supplemental oxygen but subsequently weaned off without the need for mechanical ventilation, and was discharged 2 weeks later. She was recovering well at skilled nursing facility on postdischarge follow‐up.
Individual consents were obtained and Yale Institutional Review Board (2000020932) approved this study.
3. COMMENTS
We reported two cases involving COVID‐19 positive patients, with one undergoing the high‐risk operation with the disease, while the other undergoing the operation without the disease but contracting one in the postoperative period. In the setting of the only reported case of aortic dissection with COVID‐19 not surviving, 3 our patients highlight the possibility of favorable recovery from the combination of the highly morbid pathology undergoing high‐risk operations in the setting of highly virulent respiratory illness. These cases may support the notion that emergent operations can be considered even in the nuanced situation of COVID‐19 pandemic and patients with COVID‐19 positive status or those in high‐risk demographics and with comorbidity. 2 This is important to consider especially with a report of 24% perioperative mortality among cases that took place during the pandemic. 4
COVID‐19 pandemic resulted in an abrupt decline in hospital presentations for acute conditions, such as myocardial infarction, 1 likely resulting in delayed presentation of late complications such as ventricular septal rupture. In the setting where acute care facilities have capacity to accept patients, it may be important to create a community awareness that acute conditions continue to warrant early treatment despite the perceived risk of contracting COVID‐19 disease in the hospital, because late complications may be dire. Operative decision making is nuanced in the pandemic era, as the current decision models for elective operations 5 and known risk factors for mortality 6 may not readily apply to cardiac surgical patients undergoing emergent operations. Logistically, it may be important for hospitals to dedicate a cardiac surgery operating room equipped with negative pressure for patients with COVID‐19 to facilitate timely operations while the SARS‐CoV‐2 diagnostic test is processed.
4. CONCLUSION
Although COVID‐19 is highly morbid, extremely high‐risk operations such as extensive aortic repair for thoracic aortic emergencies may have successful outcomes, even in an elderly contracting COVID‐19 in the morbid postoperative recovery period. In the absence of strong evidence or guidelines in these nuanced situations, our report may provide important examples that these challenging operations could yield successful results.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
Mori M, Geirsson A, Vallabhajosyula P, Assi R. Surgical management of thoracic aortic emergency with pre‐ and postoperative COVID‐19 disease. J Card Surg. 2020;35:2832–2834. 10.1111/jocs.14865
REFERENCES
- 1. De Filippo O, D'Ascenzo F, Angelini F, et al. Reduced rate of hospital admissions for ACS during Covid‐19 outbreak in Northern Italy. N Engl J Med. 2020;383:88‐89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rosenbaum L. The untold toll—the pandemic's effects on patients without Covid‐19. N Engl J Med. 2020;382:2368‐2371. [DOI] [PubMed] [Google Scholar]
- 3. Fukuhara S, Rosati CM, El‐Dalati S Acute type A aortic dissection during COVID‐19 outbreak [published online ahead of print April 22, 2020]. Ann Thorac Surg. 10.1016/j.athoracsur.2020.04.008 [DOI] [PMC free article] [PubMed]
- 4. COVIDSurg Collaborative . Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS‐CoV‐2 infection: an international cohort study. Lancet. 2020;396:27‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tam DY, Naimark D, Natarajan MK, et al. The use of decision modelling to inform timely policy decisions on cardiac resource capacity during the COVID‐19 pandemic [published online ahead of print May 21, 2020]. Can J Cardiol. 10.1016/j.cjca.2020.05.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID‐19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054‐1062. [DOI] [PMC free article] [PubMed] [Google Scholar]


