To the Editor,
Recent articles have pointed the impact of co‐epidemics/co‐infections of coronavirus disease 2019 (COVID‐19) and other infectious diseases on an already overburdened healthcare infrastructure. 1 , 2 With the present toll of COVID‐19 cases reaching beyond 10 922 324 infected cases and claiming 523 011 lives. 3 In Pakistan, the numbers of COVID‐19 are continually on the rise and the condition is worsening, with around 225 283 infected individuals. The death rate in Pakistan is comparatively low as compared with the western countries and has claimed 4619 lives so far as shown in Figure 1. 4 Pakistan is entirely occupied with the COVID‐19 catastrophe; simultaneously around 20 000 typhoid cases within 10 days of June 2020 have also been reported along with COVID‐19. 5 Such conditions would result in the havoc and would take a heavy toll on the public health sector thus losing lives as a result of an inability to cater all patients at the same time with a limited financing and healthcare resources. 6
Figure 1.
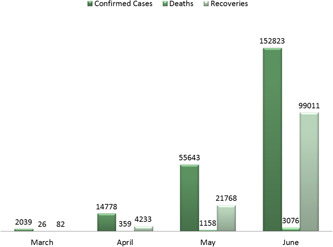
Number of coronavirus disease 2019 (COVID‐19) confirmed cases in Pakistan. *Data retrieved from National Institute of Health (NIH) (From 1st March 2020 to 4th July 2020)
Typhoid fever is a public health concern mainly in middle and lower‐income countries due to their poor sanitation and unhygienic environment. Typhoid is a bacterial infection caused by gram‐negative rod‐shaped serovars of Salmonella enterica subsp. enterica (S. typhi). The most common clinical manifestations observed in typhoid inflicted patients are; fever, headache, rash, fatigue, and abdominal pain. The transmission of typhoid can be through the intake of contaminated water and food with infected person feces (fecal‐oral route). 7 According to the World Health Organization (WHO), globally 11 to 21 million people get infected from typhoid and claiming the lives of 128 000 to 161 000 people every year. The children and communities lacking adequate sanitation and safe drinking water are most vulnerable to get infected from typhoid. 8
Federal Disease Surveillance and Response Unit, Field Epidemiology & Disease Surveillance Division, National Institute of Health (NIH) reported a total of 22 571 typhoid cases from 1 November 2016, to 16 February 2020, from Sindh province of Pakistan. Among these almost 16 thousand cases were characterized as extensively drug‐resistant typhoid cases (XDR). The estimated attack rate of typhoid was calculated to be 15.5/10 000 population. This strain of typhoid is resistant to all antibiotic treatments available for its treatment, which makes it extremely costly and challenging to treat. The outbreak of typhoid in Pakistan is currently characterized as XDR, which has infected more than 19 thousand people, most of them are from Sindh province of Pakistan. 9 In November 2019, Pakistan became the first‐ever country to introduce WHO recommended typhoid conjugate vaccine. 10
A total of 220 patients were tested for Salmonella Typhi in Lahore from 15th March to 15th June 2020. Lahore is a metropolitan city and showed the highest burden of COVID‐19 in Punjab Province. Study group includes 122 (55.4%) male and 98 (44.5%) females. Out of total patients tested 48% patients were found to be typhoid positive. Typhoid was most prevalent in the age group of 21 to 40 years (44%), followed by 25% in 41 to 60, 24% in 0 to 20, and lowest of 7% in 61 to 80 years. The overall incidence of typhoid was observed to be higher in males as shown in Figure 2. Since 2016, the highest incidence of XDR typhoid was reported in the year 2019 to be 9994 infected individuals. 11 The year wise distribution of typhoid cases is shown in Figure 3. 12 There is no data available from the whole country therefore available data from Sindh Province is shown in the figure. The surveillance and reporting of typhoid in Pakistan is quite inadequate and haphazard. To conclude the actual prevalence of typhoid in Pakistan is difficult due to low sample size and unavailability of proper clinical diagnosis.
Figure 2.
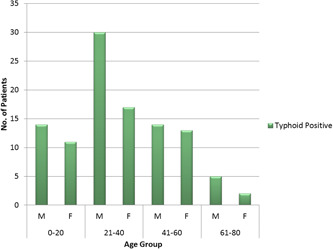
Prevalence of Salmonella Typhi in Lahore, Pakistan
Figure 3.
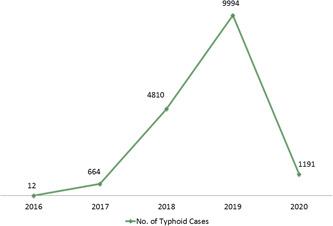
Year wise number of typhoid confirmed cases in Sindh Province, Pakistan. *Data retrieved from NIH (From 1st January 2016 to 6th June 2020)
According to a study conducted by Umer Rashid and co‐workers, typhoid was most prevalent in age ranging from 21 to 30 (42.32%) followed by age group based incidence in 11 to 20 (30.42%) and 1 to 10 (8.46%). Results show significant variation in the incidence pattern of typhoid during different months of the year. Incidence of typhoid infected cases was highest in the summer season (July‐September) 82.46% and in winters (December‐February) 14.92%. Based on the seasonal occurrence of typhoid it can be speculated, that the number of infections in the coming days will increase. The risk of acquiring typhoid can be reduced by ensuring the vaccination, provision of filtered water, and good sanitation. 13 According to several reports the export of XDR typhoid has been observed in many countries; United States, United Kingdom, Australia, Denmark, Taiwan, and Canada from Pakistani travelers. 14
The morbidity and mortality reported from Asia constitute 90% of all cases worldwide. In Asia, the estimated disease burden is based on the compilation of clinically diagnosed patients of typhoid by the government with uncertain denominators. The specified typhoid clinical diagnosis requires access to a competent laboratory that is scarce in such developing countries. Typhoid can range from acute to severe symptoms that occur after 0 to 36 days after the onset of the disease. In poor resource countries medications are usually prescribed without the proper diagnosis in such cases. Besides, to the presentation of nonspecific symptoms of typhoid, they are similar to other diseases like malaria, dengue, and COVID‐19. Due to the common symptoms of these diseases, it is difficult to identify the actual underlying cause without the proper diagnosis tests. 15 In the COVID‐19 pandemic, healthcare workers are overburdened with the high influx of patients with COVID‐19 in hospitals, in such situations rise in the number of typhoid cases has also been observed. Doctors are facing complications in the diagnosis and differentiating both diseases due to almost common symptoms like fever, fatigue, body pain, and diarrhea in some cases. Out of a total of 20 000 typhoid patients, 8000 cases have been identified in five major hospitals of Lahore, Punjab, Pakistan. 5
The government of Pakistan has taken various measures for the containment of the virus, but they are proving to be insufficient as the numbers of COVID‐19 infected cases are continually on the rise. The overburdened and poor health infrastructure of Pakistan's health system due to COVID‐19 is at the brink of collapsing. In such cases, another epidemic in the country can prove to be quite devastating. To deal with the situation efficiently the government should impose strict lockdowns and should focus on providing good sanitation and filtered water, in addition to vaccinating the children with the typhoid vaccine. The government of Pakistan should focus on educating the masses about the preventive strategies of both the disease as well as their deteriorating effect on society if they went out of control. In addition, a need of proper clinical diagnosis plays important role before the prescription of medicines otherwise the broad use of antibiotics would favor in the already out of hand antimicrobial resistance.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
The author conceived the study, discussed the results, drafted the first manuscript, critically read and revised the manuscript, and gave final approval for publication.
ETHICS STATEMENT
Ethical approval or individual consent was not applicable.
DISCLAIMER
The funding agencies had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
REFERENCES
- 1. Haqqi A, Awan UA, Ali M, Saqib MAN, Ahmed H, Afzal MS. COVID‐19 and dengue virus co‐epidemics in Pakistan: a dangerous combination for overburdened healthcare system. J Med Virol. 2020:jmv.26144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ozaraszaras R, Cirpin R, Duran A, et al. Influenza and COVID‐19 co‐infection: report of 6 cases and review of the literature. J Med Virol. 2020. 10.1002/jmv.26125 [DOI] [PubMed] [Google Scholar]
- 3. Organization WH. Coronavirus disease (COVID‐19) . Situation report—166. Accessed 04 July 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200704-covid-19-sitrep-166.pdf?sfvrsn=6247972_2
- 4. Health NIo. Pakistan Cases Details (COVID‐19 Dashboard) . Accessed 04 July 2020. http://covid.gov.pk/stats/pakistan
- 5. NEWS A . Doctors report increasing typhoid cases in Punjab than COVID‐19. Accessed 19 June 2020. https://arynews.tv/en/doctors-report-increasing-typhoid-cases-punjab/
- 6. Shaikh BT, Ali N. COVID‐19 and fiscal space for health system in Pakistan: It is time for a policy decision. Int J Health Plann Manage. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Crump JA. Progress in typhoid fever epidemiology. Clin Infect Dis. 2019;68(suppl_1):S4‐S9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Organization WH . Typhoid. Accessed 19 February 2020. https://www.who.int/immunization/diseases/typhoid/en/
- 9. Today P. Over 19 000 typhoid cases reported in Sindh in three years. Updated 21 Novemeber 2019. Accessed 19 February 2020. https://www.pakistantoday.com.pk/2019/11/21/over-19000-typhoid-cases-reported-in-sindh-in-three-years/
- 10. Organization WH. Pakistan first country to introduce new typhoid vaccine into routine immunization programme. Accessed 19 June 2020. http://www.emro.who.int/pak/pakistan-news/pakistan-first-country-to-introduce-new-typhoid-vaccine-into-routine-immunization-programme.html
- 11. Health NIo . Weekly field epidemiology report. Accessed 19 June 2020. https://www.nih.org.pk/wp-content/uploads/2020/03/07-FELTP-Pakistan-Weekly-Epidemiological-Report-Feb-03-Feb-09-2020.pdf
- 12. Health NIo . Weekly field epidemiology report. Accessed 28 June 2020. https://www.nih.org.pk/wp-content/uploads/2020/06/24-FELTP-Pakistan-Weekly-Epidemiological-Report-June-07-13-2020.pdf
- 13. Rasul F, Sughra K, Mushtaq A, Zeeshan N, Mehmood S, Rashid U Surveillance report on typhoid fever epidemiology and risk factor assessment in district Gujrat, Punjab, Pakistan. 2017.
- 14. Control ECfDPa . Increase of XDR Typhoid fever in travellers returning from Pakistan. Updated 09 October 2020. Accessed 19 June 2020. https://www.ecdc.europa.eu/en/news-events/increase-xdr-typhoid-fever-travellers-returning-pakistan
- 15. Ochiai RL, Acosta CJ, Danovaro‐Holliday MC, et al. A study of typhoid fever in five Asian countries: disease burden and implications for controls. Bull World Health Organ. 2008;86:260‐268. [DOI] [PMC free article] [PubMed] [Google Scholar]


