Abstract
The coronavirus disease‐2019 (COVID‐19) pandemic has heightened the awareness of aerosol generation by human expiratory events and their potential role in viral respiratory disease transmission. Concerns over high severe acute respiratory syndrome‒coronavirus‐2 (SARS‐CoV‐2) viral burden of mucosal surfaces has raised questions about the aerosol‐generating potential and dangers of many otorhinolaryngologic procedures. However, the risks of aerosol generation and associated viral transmission by droplet or airborne routes for many otorhinolaryngology procedures are largely unknown. Indoor aerosol and droplet viral respiratory transmission risk is influenced by 4 factors: (1) aerosol or droplet properties; (2) indoor airflow; (3) virus‐specific factors; and (4) host‐specific factors. Herein we elaborate on known aerosol vs droplet properties, indoor airflow, and aerosol‐generating events to provide context for risks of aerosol infectious transmission. We also provide simple but typically effective measures for mitigating the spread and inhalation of viral aerosols in indoor settings. Understanding principles of infectious transmission, aerosol and droplet generation, as well as concepts of indoor airflow, will assist in the integration of new data on SARS‐CoV‐2 transmission and activities that can generate aerosol to best inform on the need for escalation or de‐escalation from current societal and institutional guidelines for protection during aerosol‐generating procedures.
Keywords: aerosol, aerosol‐generating procedure, airborne, droplet, COVID‐19, SARS‐CoV‐2
Coronavirus disease‐2019 (COVID‐19), caused by the novel severe acute respiratory−syndrome coronavirus‐2 (SARS‐CoV‐2), is a respiratory disease with an evolving and expanding list of systemic manifestations 1 , 2 , 3 and a mortality rate that has yet to be fully clarified but is estimated at 1.4% to 3.2%. 1 , 4 The COVID‐19 pandemic has fundamentally shaken the perceptions and approaches to otorhinolaryngology medical practices and procedures. Many otorhinolaryngology procedures involve instrumentation of respiratory mucosal surfaces and proximity to a patient's airway for a period ranging from minutes to hours, and there has been concern that many of these procedures may be aerosol‐generating procedures (AGPs) that increase the risk of contracting COVID‐19 due to inhalation of airborne droplets or aerosols. 5 , 6 , 7 , 8 , 9 The lack of studies within the otorhinolaryngology field assessing the aerosol‐generating potential of procedures involving mucosal surfaces pre‒COVID‐19 made it challenging to understand in an evidence‐based fashion the potential risks of SARS‐CoV‐2 transmission associated with instrumentation of the upper airway; that is, whether these procedures may be infectious AGPs. At the early stages of the pandemic, based on the risks of exposure to high viral load mucosal surfaces, 10 , 11 as well as on the lack of any immunity to SARS‐CoV‐2 and of any vaccines or effective treatments, an array of practice changes to protect health‐care workers and patients were recommended and instituted for otorhinolaryngology procedures involving upper airway mucosal surfaces. 9 , 12 , 13 , 14 , 15 , 16 , 17
Respiratory disease transmission can occur through contact (touching a contaminated surface followed by self‐inoculation of the eyes, nose, or mouth), droplet (inhalation in nasal/upper airway or direct inoculation of eyes, nose, or mouth), or aerosol transmission (inhalation into upper or lower airway) (Fig. 1). 8 , 18 In addition, airborne respiratory pathogen transmission is ill‐defined with proposed definitions of short‐range droplet (<2 or 3 meters) vs long‐range aerosol transmission. 19 When considering modes of transmission for SARS‐CoV‐2, it is important to recognize that airborne transmission remains controversial as a significant or common mode of transmission for viral respiratory diseases, such as influenza, severe acute respiratory syndrome (SARS), and Middle East respiratory syndrome (MERS). 19 , 20 , 21 , 22 , 23 SARS‐CoV‐1 and SARS‐CoV‐2 both target the surface receptor angiotensin‐converting enzyme‐2 (ACE‐2) in humans as a means of entry, 24 , 25 and ACE‐2 is expressed on type II pneumocytes in the lung 26 , 27 and ciliated cells of nasal mucosa, 27 , 28 suggesting that there is a biologically plausible mechanism for an airborne route of transmission. Observational studies and models are emerging suggesting airborne transmission of SARS‐CoV‐2 can occur. 29 , 30 , 31
FIGURE 1.
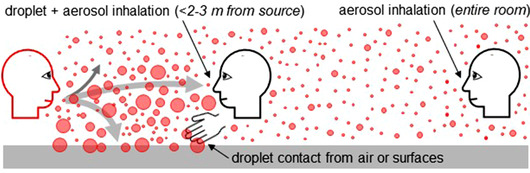
Three possible mechanisms of respiratory pathogen transmission. Transmission can occur through self‐inoculation after contact with droplets that settle on surfaces, direct deposition/inspiration of infectious droplets in the mouth or nose and deposition on the eyes, as well as through airborne transmission with inhalation of aerosols. Short range (<2 to 3 meters) aerosol transmission can be difficult to separate from droplet transmission and long‐range transmission for viral respiratory pathogens, including influenza and coronaviruses, remains controversial.
Indoor airborne viral respiratory transmission risk is influenced by 4 factors: (1) aerosol and droplet properties; (2) indoor airflow; (3) virus‐specific factors; and (4) host‐specific factors. Herein we elaborate on known aerosol vs droplet properties, aerosol‐generating events, and concepts of indoor airflow. Combining principles of these elements with those of infectious transmission can inform simple yet typically effective measures for mitigating the concentration, distribution, and inhalation of viral aerosols in indoor settings.
Characteristics of indoor aerosol and droplet behavior
An aerosol is “a suspension of fine solid particles or liquid droplets in air or another gas,” 32 and an aerosol can be usefully envisioned as a particle that follows the streamlines of the flowing gas (indoor air in our case) in which it resides. Yet, this definition does not fully encompass the wide range of airborne particle behaviors, which depend on particle size. The dominant method of classifying particle behavior is by size based on diameter, typically in micrometers (µm).
Generally, indoor aerosols exist as particles of diameter size of subnanometer to several hundred micrometers, and they may be most broadly defined as ultrafine (<0.1 µm), fine (0.1‐2.5 µm), or coarse (>2.5 µm). 33 Although droplets are often discussed in some communities as distinct from aerosols, both are airborne particulate matter cast on a continuum of size. The definition of droplet is nebulous, and droplets have been variously defined as having diameters of >5, >10, or >100 µm. However, this distinction has utility, as droplets should be thought of as particles that fall out of the air rapidly while aerosols do not and remain airborne indoors. Thus, characterization of the size of the particle is crucial for calculating particle deposition on surfaces, where particles above ∼10 µm in size are more likely to fall out of airflow streams and settle or impact onto surfaces (Fig. 2). Because a droplet is often a large particle consisting mostly of water, with an associated aerosol‐size nucleus (ie, a droplet nucleus), evaporation kinetics driven by conditions such as relative humidity, air temperature, and velocity determine a droplet critical size below which the droplet rapidly evaporates to form an aerosol with an appreciable indoor air lifetime and above which evaporation kinetics are slow enough that the droplet quickly settles out of the air. 34
FIGURE 2.
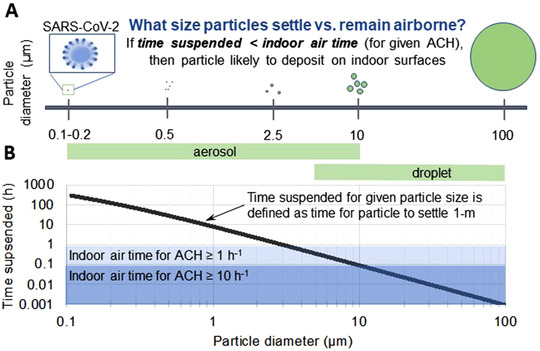
Suspension time of aerosols and droplets in indoor environments. (A) The relative sizes of aerosol and droplet particles are shown compared with a single coronavirus. (B) As particle size decreases, airborne suspension time increases—particles >5 to 10 µm have suspension times on the order of seconds and are considered droplets, whereas particles with smaller diameter remain airborne much longer and are considered aerosol. For context, the time for a particle to fall 1 meter due to gravity can be calculated using its terminal settling velocity, 77 and particles of 100, 10, 1, and 0.1 µm will settle a distance of 1 meter in 3.3 seconds, 5.6 minutes, 9.3 hours, and 39 days, respectively. Particle settling is important when the suspension time is less than the indoor air residence time, which is how long air resides indoors before being exhausted and replaced by fresh ventilation air. The suspension time is defined as amount of time for a particle of a given size to settle 1 meter with no air flow, as depicted by the black line. The influence of the number of ACHs is depicted; that is, particles with a suspension time of >0.1 hour will be less likely to deposit on surfaces and will be cleared from a room with ≥10 ACHs, and those with suspension times >1 hour will behave similarly when there is ≥1 ACH. Although ultrafine and smaller fine aerosols never appreciably settle due to gravity on surfaces indoors, they do deposit effectually on indoor surfaces by the Brownian diffusion mechanism. 78 Note that the graph represents suspension times and indoor air times for well‐mixed environments, and does not include impact of local airflow, source proximity, or evaporation. ACH = air changes per hour.
Aerosol and droplet descriptions and divisions are based on characteristic behaviors of particles from modeling and experimental data, but they do not account for the infectious composition of the particles. Often, descriptions of aerosol regarding infectious disease transmission have followed similar paradigms—with divisions based on particle size that can be inhaled into different respiratory regions (Fig. 3). 8 , 18 , 35 To date, SARS‐CoV‐2 viral RNA has been detected predominantly in the >1‐µm‐diameter range, with the majority of viral RNA detected in aerosols >4 µm in hospitals with large outbreaks of COVID‐19. 36 This study, in conjunction with particle lung deposition models (Fig. 3), 32 suggests that a preponderance of viral‐laden infectious particles may deposit in the nasal airway.
FIGURE 3.
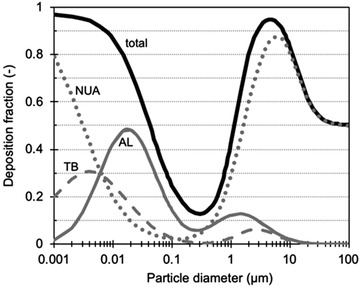
ICRP lung deposition model, predicted with fitted equations from Hinds. 32 Total (solid black line) and regional deposition in NUA (gray dotted line), TB (hashed gray line), and AL (solid gray line) regions for light exercise with nasal breathing. A greater percentage of particles less than ∼1 to 2.5 µm deposit in the tracheobronchial and alveoli regions, 79 , 80 whereas larger particles deposit in the upper airway. Respirable aerosols are defined as particles <10 µm in diameter and inhalable aerosols as <2.5 µm. 8 AL, alveolar; ICRP = International Commission on Radiological Protection; NUA, nasal upper airway; TB = tracheobronchial.
Aerosol emissions from breathing, talking, coughing, singing, and sneezing
With regard to aerosol‐ or droplet‐generating expiratory actions, it is important to consider both the quantity and size range of emitted particles, as well as the velocity of the generating or initial carrying event that impact the transport of particles (especially droplets). 37 Breathing, talking, coughing, and sneezing generate aerosols and/or droplets, and aerosol generation with these actions is not uniform, with a high degree of variability from individual to individual. 38 , 39 , 40 , 41 , 42 In addition, aerosol generation in those with viral respiratory infections may be increased when compared with healthy individuals. 38 With the exception of sneezing, which emits large droplets with central tendencies of particles at tens or hundreds of micrometers, 43 studies have reported that these events generate more submicrometer than supermicrometer particles, that there is high variability among test subjects, and that the order of least‐producing actions is breathing followed by talking and then coughing. 44 Moreover, newer work has demonstrated that speech generates hundreds or thousands of sub‐ and supermicrometer particles per second, 45 and that emission rates correlate with the loudness of the speech. 46 Singing and sustained vocalization also have increased emission rates, 47 , 48 and singing in close proximity in an enclosed space was recently linked with a large documented cluster of COVID‐19 cases associated with a choir practice highlighting the concern for airborne transmission. 29
Aerosol‐generating procedures
The US Centers for Disease Control and Prevention (CDC) defines “aerosol‐generating procedures” (AGPs) as procedures with the potential to generate infectious respiratory particles at higher concentrations than breathing, coughing, sneezing, or talking (Table 1), or procedures that create uncontrolled respiratory secretions. 49 , 50 As also noted by the CDC, the list of AGPs is both limited in accuracy and completeness. The limited data on airborne transmission risks with most commonly performed medical procedures involving mucosal surfaces has made it challenging to arrive at a unified consensus defining otolaryngology procedures that are AGPs. The current CDC list of infectious AGPs includes some otolaryngology‐associated procedures, among them open suctioning of airways, intubation, and bronchoscopy. 49 Recent work examining endonasal procedures and mastoidectomy has demonstrated droplet dispersion with high‐speed endonasal drilling 51 and drilling of the mastoid, 52 respectively. Aerosols in the 1‐ to 10‐µm‐diameter range were observed after nasal endoscopy, endonasal electrocautery, or high‐speed endonasal drilling. 53 Most procedures listed as AGPs have limited or no data characterizing particle size‒resolved emission rates, resulting characteristics of indoor particle transport, or quantification of infectious agents recoverable from emitted aerosol.
TABLE 1.
CDC's list of aerosol‐generating procedures *
| Bronchoscopy |
| Cardiopulmonary resuscitation |
| Extubation |
| High‐flow oxygen |
| Intubation |
| Manual ventilation |
| Nebulizer delivery |
| Noninvasive ventilation |
| Open suctioning of airways |
| Sputum induction |
*List of AGPs based on a meta‐analysis by Tran et al of health‐care worker infection from the 2003 SARS outbreak, assessing data from retrospective case series involving procedures generally thought to be aerosol generating. Intubation was noted as the highest risk procedure. 48
CDC = US Centers for Disease Control and Prevention; SARS
= severe acute respiratory syndrome.
Indoor aerosol movement and transport
Aerosol transport in buildings has been well researched and the physics of particle movement in indoor environments is understood. 54 , 55 , 56 , 57 , 58 In a room setting, particle emission from the mouth or nose is influenced by its initial velocity. A sneeze, for example, can generate an extremely high velocity initially (∼50 m/s), but it will quickly dissipate over a short distance (∼5 m/s after 0.6 meter), 59 whereas talking generates a lower velocity at ∼3 m/s, 60 with the initial airflow field likely dissipating completely within 1 meter from the mouth. 61 Because the majority of generated particles are <10 µm for all but sneezing, larger diameter droplets will fall to a surface quickly, but, for an aerosol without appreciable settling, the bulk indoor airflow governs its movement as the initial velocity dissipates.
In the indoor environment, bulk airflow is impacted largely by 2 forces: the first is the movement from thermal buoyancy of equipment and occupants; and the other is the forced‐air movement of the heating, ventilation, and air‐conditioning (HVAC) system. For aerosols, these mechanisms greatly increase the distance exhaled particles can spread indoors. 62 , 63 An HVAC system conditions and distributes air around a building using various amounts of recirculated and ventilation (fresh outdoor) air, and an aerosol emission can be transported from its point of origin to the entire HVAC zone or building due to the recirculation, although the concentration will diminish due to dilution and filtration. 64 In one documented example from Guangzhou, China, Li et al 30 observed that, in a poorly ventilated space, the transmission of SARS‐CoV‐2 could be traced to localized airflow, highlighting the importance of indoor local airflow patterns for COVID‐19 transmission.
Aerosol exposure risk and mitigation strategies
Transmission of a respiratory viral pathogen requires exposure to and successful inoculation with an infectious titer of virus. Opportunistic aerosol transmission due to local airflow between an aerosol source and susceptible host is an area of concern and controversy due to challenges in clearly delineating this mode of transmission from droplet transmission. Nevertheless, proximity to an aerosol or droplet source increases the risk of exposure and successful viral transmission, particularly as the distance between particle source (eg, airway during an expiratory event) and susceptible host decreases to <1 meter, 65 a typical situation during both physical examination and any otolaryngology procedure.
Guidelines for use of eye protection do not currently delineate between protective goggles or face shields; however, we advocate for use of face shields as they provide additional protection beyond shielding the eyes. Face shields are effective at preventing early exposure to cough‐ or sneeze‐generated aerosols by intercepting droplets and high‐velocity airborne particles before impacting on a face mask or respirator. 66 Face‐shield efficacy is reduced as time increases after the expiratory event as aerosol particles are able to “slip” around the face shield 66 when particle transport associated with bulk airflow takes over. At this point, the role of an effective face mask or respirator becomes critical. Of note, current clinical data is not clear cut on the efficacy of N95 masks over surgical masks in preventing disease transmission 67 , 68 , 69 ; however, a recent analysis has suggested that N95 masks are likely more effective than surgical masks at reducing coronavirus‐associated disease transmission. 65
Although long‐range viral respiratory pathogen aerosol transmission is controversial and has not been definitively established as a common mechanism of SARS‐CoV‐2 transmission to date, principles associated with bulk airflow can be used to help minimize risks of aerosol transmission. Reducing infectious aerosols can be achieved by increasing the building ventilation (dilution) rate and using higher efficiency filtration. Hospital‐based clinic rooms require a minimum of 6 air changes per hour (ACHs) and operating rooms (ORs) a minimum of 15 ACH, of which 3 at a minimum (in the OR only) are air changes with outdoor air, 70 whereas, according to the American Society for Heating, Refrigeration, and Air‐Conditioning Engineers (ASHRAE), outpatient care facilities should have about 2 ACHs. The risk of aerosol transmission is likely highest in clinic settings, particularly office‐building‒based practices and older or repurposed buildings with poor ventilation or older HVAC systems with no or lower efficiency filtration.
Indoor air dilution to reduce aerosol exposure is the key strategy that ASHRAE recommends for building protection during the pandemic reopening phase, 71 advocating for increasing ventilation air intake in buildings to 3 ACHs, roughly 3 to 5 times higher than the minimum ventilation standard in offices or similar building types. 72 At 3 ACHs, the outdoor air dilution is able to remove about 95% of the contaminants indoors within 1 hour, assuming the space is well mixed. HVAC systems should be operated to increase ventilation (outdoor) air as much as the system constraints allow for optimization of these dilutional effects. Whenever possible, opening windows can increase crossflow and is also a simple and effective option for enhancing dilution and decreasing concentrations of indoor‐emitted aerosol.
HVAC systems in buildings usually employ intentional particle filtration, which will further diminish aerosol concentrations. Properly installed, the most efficient filter typically used (MERV 16) can remove >95% of the 0.3‐ to 10‐µm‐size range of particles. 73 Knowledge of the HVAC zones (what nonclinic rooms are connected to airflow from clinic rooms) may help inform how best to approach and optimize enhanced filtration that can remove aerosols and reduce risks of circulating infectious aerosols within an HVAC zone. Strongly increasing ventilation air and filtration may not be possible with all systems due to increased system strain or the configuration or age of the HVAC system. Especially in these, but in our opinion possibly all situations, there is a role for portable air cleaners with high clean air delivery rates (CADRs) to reduce aerosol concentrations in a room, such as a stand‐alone HEPA filter with a high flow rate. 74 , 75 , 76 The CADR is the effective flow rate of particle‐free air supplied by the device. The impact a portable air cleaner will have in a room can be determined by dividing the CADR by the room volume. For example, a unit with a CADR of 200 ft3/min will effectively add 12 ACHs in terms of particle removal for a room that is ∼1000 ft3 (eg, for a room of 12 ft × 10 ft × 8.3 ft; CADR = 200 ft3/min × 60 min/h = 12,000 ft3/h; impact = CADR/volume = 12,000 ft3/h/1000 ft3 = 12 h−1 is equivalent to 12 ACHs).
The risk of long‐range aerosol transmission in an OR setting meeting current federal guidelines for ACH is likely minimized due to aerosol exhaust, dilution, and filtration. In this type of setting, the key transport mechanism for potential aerosol transmission relies on duration of exposure to local airflow within an OR between the emitter and a given target. Because aerosols move with bulk air, specific airflow design strategies can be used to control or mitigate exposure to pathogens indoors. Awareness of the location of the air‐handling vents and the general direction of airflow may be helpful in orienting patient positioning to maximize airborne particle movement away from the health‐care provider. However, given the complexity of assessing and modeling airflows, impacts of such changes to risks of infectious airborne transmission will likely need to be assessed on a case‐by‐case basis.
Conclusion
The risk of long‐range airborne transmission of SARS‐CoV‐2 remains controversial; however, the nature of an otolaryngology practice makes it plausible that the proximity to a patient's airway during elements of the physical examination and some otorhinolaryngologic procedures carries a risk of opportunistic aerosol transmission due to short‐term viral exposure at a high concentration or cumulative viral exposure over time. Awareness of local airflow patterns within a clinical space can help orient patient positioning to enhance aerosol movement away from the provider. The grim reality is that the true measure of protection will be tracking COVID‐19 among health‐care workers at high risk for droplet and aerosol exposure, which will be challenging to separate from ongoing community spread. By combining enhanced HVAC or portable air‐cleaner filtration with increased ventilation, clinic spaces can be prepared to better protect occupants from possible aerosol transmission. These actions will narrow the key transport mechanism for potential aerosol transmission to rely on local air movement between the emitter and a given target, which is a mechanism that can be mitigated with the use of face shields and respirators. This approach can improve overall clinical safety and allow clinics to remain operational as regional surges in cases occur. As we learn more about COVID‐19 transmission, understanding the principles of infectious transmission, airborne particle and droplet generation, and concepts of indoor airflow will help us to make informed and rational decisions on escalation or de‐escalation of our current societal and institutional guidelines for AGPs.
Acknowledgement
M.A.K., L.J.L., and M.S.W. contributed to the background research, writing, and figure preparation for this study.
How to Cite this Article:Kohanski MA, Lo LJ, Waring MS. Review of indoor aerosol generation, transport, and control in the context of COVID‐19. Int Forum Allergy Rhinol. 2020;10:1173–1179.
Funding sources for the study: ARS Friends in Research (to M.A.K.).
Potential conflicts of interest: M.A.K., L.J.L., and M.S.W. are inventors on a pending patent for aerosol and droplet protective devices.
References
- 1. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708‐1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Helms J, Kremer S, Merdji H, et al. Neurologic features in severe SARS‐CoV‐2 infection. N Engl J Med. 2020;382(23):2268‐2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Oxley TJ, Mocco J, Majidi S, et al. Large‐vessel stroke as a presenting feature of Covid‐19 in the young. N Engl J Med. 2020;382:e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. US Centers for Disease Control and Prevention . Geographic differences in COVID‐19 cases, deaths, and incidence—United States, February 12‒April 7, 2020. 2020. https://www.cdc.gov/mmwr/volumes/69/wr/mm6915e4.htm?s_cid=mm6915e4_w. Accessed May 20, 2020.
- 5. Chowell G, Abdirizak F, Lee S, et al. Transmission characteristics of MERS and SARS in the healthcare setting: a comparative study. BMC Med. 2015;13:210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Christian MD, Loutfy M, McDonald LC, et al. Possible SARS coronavirus transmission during cardiopulmonary resuscitation. Emerg Infect Dis. 2004;10:287‐293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fowler RA, Guest CB, Lapinsky SE, et al. Transmission of severe acute respiratory syndrome during intubation and mechanical ventilation. Am J Respir Crit Care Med. 2004;169:1198‐1202. [DOI] [PubMed] [Google Scholar]
- 8. Tellier R, Li Y, Cowling BJ, Tang JW. Recognition of aerosol transmission of infectious agents: a commentary. BMC Infect Dis. 2019;19:101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Vukkadala N, Qian ZJ, Holsinger FC, Patel ZM, Rosenthal E. COVID‐19 and the otolaryngologist: preliminary evidence‐based review. [published online ahead of print, 2020 March 26]. Laryngoscope. 2020. [DOI] [PubMed] [Google Scholar]
- 10. Zou L, Ruan F, Huang M, et al. SARS‐CoV‐2 Viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177‐1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wolfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients with COVID‐2019. Nature. 2020;581(7809):465‐469. [DOI] [PubMed] [Google Scholar]
- 12. Panuganti BA, Pang J, Califano J, Chan JYK. Procedural precautions and personal protective equipment during head and neck instrumentation in the COVID‐19 era. Head Neck. 2020;42(7):1645‐1651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kowalski LP, Sanabria A, Ridge JA, et al. COVID‐19 pandemic: effects and evidence‐based recommendations for otolaryngology and head and neck surgery practice. Head Neck. 2020;42(6):1259‐1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Givi B, Schiff BA, Chinn SB, et al. Safety recommendations for evaluation and surgery of the head and neck during the COVID‐19 pandemic. JAMA Otolaryngol Head Neck Surg. 2020. [DOI] [PubMed] [Google Scholar]
- 15. Castelnuovo P, Turri‐Zanoni M, Karligkiotis A, et al. Skull base surgery during the Covid‐19 pandemic: the Italian skull base society recommendations. Int Forum Allergy Rhinol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Howard BE. High‐risk aerosol‐generating procedures in COVID‐19: Respiratory protective equipment considerations. Otolaryngol Head Neck Surg. 2020;163(1):98‐103. [DOI] [PubMed] [Google Scholar]
- 17. McGrath BA, Brenner MJ, Warrillow SJ, Pandian V, Arora A, Cameron TS, et al. Tracheostomy in the COVID‐19 era: global and multidisciplinary guidance. Lancet Respir Med. 2020;8(7):717‐725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cole EC, Cook CE. Characterization of infectious aerosols in health care facilities: an aid to effective engineering controls and preventive strategies. Am J Infect Control. 1998;26:453‐464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tellier R. Aerosol transmission of influenza A virus: a review of new studies. J R Soc Interface. 2009;6(Suppl 6):S783‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Brankston G, Gitterman L, Hirji Z, Lemieux C, Gardam M. Transmission of influenza A in human beings. Lancet Infect Dis. 2007;7:257‐265. [DOI] [PubMed] [Google Scholar]
- 21. Cowling BJ, Ip DK, Fang VJ, et al. Aerosol transmission is an important mode of influenza A virus spread. Nat Commun. 2013;4:1935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Killingley B, Nguyen‐Van‐Tam J. Routes of influenza transmission. Influenza Other Respir Viruses. 2013;7(Suppl 2):42‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Seto WH. Airborne transmission and precautions: facts and myths. J Hosp Infect. 2015;89:225‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hoffmann M, Kleine‐Weber H, Schroeder S, et al. SARS‐CoV‐2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271‐280.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Li W, Moore MJ, Vasilieva N, Sui J, Wong SK, Berne MA, et al. Angiotensin‐converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003;426:450‐454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203:631‐637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hou YJ, Okuda K, Edwards CE, et al. SARS‐CoV‐2 Reverse genetics reveals a variable infection gradient in the respiratory tract. Cell. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sungnak W, Huang N, Becavin C, et al. SARS‐CoV‐2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat Med. 2020;26:681‐687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hamner L, Dubbel P, Capron I, et al. High SARS‐CoV‐2 attack rate following exposure at a choir practice—Skagit County, Washington, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69:606‐610. [DOI] [PubMed] [Google Scholar]
- 30. Li Y, Qian H, Hang J, et al. Evidence for probable aerosol transmission of SARS‐CoV‐2 in a poorly ventilated restaurant. medRxiv. 2020;2020.04.16.20067728. [Google Scholar]
- 31. Zhang R, Li Y, Zhang AL, Wang Y, Molina MJ. Identifying airborne transmission as the dominant route for the spread of COVID‐19. Proc Natl Acad Sci USA. 2020;117(26):14857‐14863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hinds WC. Aerosol Technology: Properties, Behavior, and Measurement of Airborne Particles. Hoboken, NJ: Wiley; 1999. [Google Scholar]
- 33. Nazaroff WW. Indoor particle dynamics. Indoor Air. 2004;14(Suppl 7):175‐183. [DOI] [PubMed] [Google Scholar]
- 34. Xie X, Li Y, Chwang AT, Ho PL, Seto WH. How far droplets can move in indoor environments—revisiting the Wells evaporation‐falling curve. Indoor Air. 2007;17:211‐225. [DOI] [PubMed] [Google Scholar]
- 35. Jones RM, Brosseau LM. Aerosol transmission of infectious disease. J Occup Environ Med. 2015;57:501‐508. [DOI] [PubMed] [Google Scholar]
- 36. Chia PY, Coleman KK, Tan YK, et al. Detection of air and surface contamination by SARS‐CoV‐2 in hospital rooms of infected patients. Nat Commun. 2020;11:2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kleinstreuer C, Zhang, Z . Airflow and particle transport in the human respiratory system. Annu Rev Fluid Mech. 2010;42:301‐334. [Google Scholar]
- 38. Fabian P, Brain J, Houseman EA, Gern J, Milton DK. Origin of exhaled breath particles from healthy and human rhinovirus‐infected subjects. J Aerosol Med Pulm Drug Deliv. 2011;24:137‐147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Edwards DA, Man JC, Brand P, et al. Inhaling to mitigate exhaled bioaerosols. Proc Natl Acad Sci USA. 2004;101:17383‐17388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Yang S, Lee GW, Chen CM, Wu CC, Yu KP. The size and concentration of droplets generated by coughing in human subjects. J Aerosol Med. 2007;20:484‐494. [DOI] [PubMed] [Google Scholar]
- 41. Holmgren H, Ljungström E, Almstrand AC, Bake B, Olin AC. Size distribution of exhaled particles in the range from 0.01 to 2.0 µm. J Aerosol Sci. 2010;41:439‐446. [Google Scholar]
- 42. Wurie F, Le Polain de Waroux O, Brande M, et al. Characteristics of exhaled particle production in healthy volunteers: possible implications for infectious disease transmission. F1000Res. 2013;2:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Han ZY, Weng WG, Huang QY. Characterizations of particle size distribution of the droplets exhaled by sneeze. J R Soc Interface. 2013;10:20130560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Papineni RS, Rosenthal FS. The size distribution of droplets in the exhaled breath of healthy human subjects. J Aerosol Med. 1997;10:105‐116. [DOI] [PubMed] [Google Scholar]
- 45. Stadnytskyi V, Bax CE, Bax A, Anfinrud P. The airborne lifetime of small speech droplets and their potential importance in SARS‐CoV‐2 transmission. Proc Natl Acad Sci USA. 2020;117(22):11875‐11877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Asadi S, Wexler AS, Cappa CD, Barreda S, Bouvier NM, Ristenpart WD. Aerosol emission and superemission during human speech increase with voice loudness. Sci Rep. 2019;9:2348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Johnson GR, Morawska L, Ristovski ZD, et al. Modality of human expired aerosol size distributions. J Aerosol Sci. 2011;42:839‐851. [Google Scholar]
- 48. Loudon RG, Roberts RM. Singing and the dissemination of tuberculosis. Am Rev Respir Dis. 1968;98:297‐300. [DOI] [PubMed] [Google Scholar]
- 49. US Centers for Disease Control and Prevention . Which procedures are considered aerosol generating procedures in healthcare settings? 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-faq.html. Accessed May 18, 2020.
- 50. Tran K, Cimon K, Severn M, Pessoa‐Silva CL, Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012;7:e35797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Workman AD, Welling DB, Carter BS, et al. Endonasal instrumentation and aerosolization risk in the era of COVID‐19: simulation, literature review, and proposed mitigation strategies. Int Forum Allergy Rhinol. 2020;10(7):798‐805. [DOI] [PubMed] [Google Scholar]
- 52. Chen JX, Workman AD, Chari DA, et al. Demonstration and mitigation of aerosol and particle dispersion during mastoidectomy relevant to the COVID‐19 era. Otol Neurotol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Workman AD, Jafari A, Welling DB, et al. Airborne aerosol generation during endonasal procedures in the era of COVID‐19: risks and recommendations. Otolaryngol Head Neck Surg. 2020:194599820931805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Wallace L. Indoor particles: a review. J Air Waste Manag Assoc. 1996;46:98‐126. [DOI] [PubMed] [Google Scholar]
- 55. Loomans M. The measurement and simulation of indoor air flow. Technische Universiteit Eindhoven; 1998. 10.6100/IR518750. [DOI]
- 56. Tham KW. Indoor air quality and its effects on humans—a review of challenges and developments in the last 30 years. Energy Build. 2016;130:637‐650. [Google Scholar]
- 57. Nazaroff WW. Indoor particle dynamics. Indoor Air. 2004;14(Suppl 7):175‐183. [DOI] [PubMed] [Google Scholar]
- 58. Fu S., Biwole PH, Mathis C. Particle tracking velocimetry for indoor airflow field: a review. Build Environ. 2015;87:34‐44. [Google Scholar]
- 59. Tang JW, Nicolle AD, Klettner CA, et al. Airflow dynamics of human jets: sneezing and breathing—potential sources of infectious aerosols. PLoS One. 2013;8:e59970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Chao CYH, Wan MP, Morawska L, et al. Characterization of expiration air jets and droplet size distributions immediately at the mouth opening. J Aerosol Sci. 2009;40:122‐133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Gupta JK, Lin CH, Chen Q. Characterizing exhaled airflow from breathing and talking. Indoor Air. 2010;20:31‐39. [DOI] [PubMed] [Google Scholar]
- 62. Lu W, Howarth AT, Adams NM, Riffat SB. CFD modeling and measurement of aerosol particle distributions in ventilated multizone rooms. ASHRAE Trans. 1999;105:116. [Google Scholar]
- 63. Mui KW, Wong LT, Wu CL, Lai AC. Numerical modeling of exhaled droplet nuclei dispersion and mixing in indoor environments. J Hazard Mater. 2009;167:736‐744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Zhang Z, Chen Q. Experimental measurements and numerical simulations of particle transport and distribution in ventilated rooms. Atmos Environ. 2006;40:3396‐3408. [Google Scholar]
- 65. Chu DK, Akl EA, Duda S, et al. Physical distancing, face masks, and eye protection to prevent person‐to‐person transmission of SARS‐CoV‐2 and COVID‐19: a systematic review and meta‐analysis. Lancet. 2020;395(10242):1973‐1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Lindsley WG, Noti JD, Blachere FM, Szalajda JV, Beezhold DH. Efficacy of face shields against cough aerosol droplets from a cough simulator. J Occup Environ Hyg. 2014;11:509‐518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Radonovich LJ Jr, Simberkoff MS, Bessesen MT, et al. N95 respirators vs medical masks for preventing influenza among health care personnel: a randomized clinical trial. JAMA. 2019;322:824‐833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Smith JD, MacDougall CC, Johnstone J, Copes RA, Schwartz B, Garber GE. Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: a systematic review and meta‐analysis. CMAJ. 2016;188:567‐574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Loeb M, Dafoe N, Mahony J, et al. Surgical mask vs N95 respirator for preventing influenza among health care workers: a randomized trial. JAMA. 2009;302:1865‐1871. [DOI] [PubMed] [Google Scholar]
- 70. Centers for Disease Control and Prevention. Division of Healthcare Quality Promotion . Environmental Infection Control Guidelines: Appendix B. 2019. https://www.cdc.gov/infectioncontrol/guidelines/environmental/appendix/air.html. Accessed May 24, 2020.
- 71. American Society for Heating, Refrigeration, and Air‐Conditioning Engineers . ASHRAE position document on infectious aerosols 2020. https://www.ashrae.org/technical-resources/resources. Accessed XX
- 72. American Society for Heating, Refrigeration, and Air‐Conditioning Engineers . Ventilation for acceptable indoor air quality. Standard 621‐2019. Atlanta, GA: American National Standards Institute; 2019. [Google Scholar]
- 73. Sublett JL, Seltzer J, Burkhead R, Williams PB, Wedner HJ, Phipatanakul W, et al. Air filters and air cleaners: rostrum by the American Academy of Allergy, Asthma & Immunology Indoor Allergen Committee. J Allergy Clin Immunol. 2010;125:32‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Zhao B, An N, Chen C. Using air purifier as a supplementary protective measure in dental clinics during the COVID‐19 pandemic. Infect Control Hosp Epidemiol. 2020:1‐4. 10.1017/ice.2020.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Shaughnessy RJ, Sextro RG. What is an effective portable air cleaning device? A review. J Occup Environ Hyg. 2006;3:169‐181; quiz D45. [DOI] [PubMed] [Google Scholar]
- 76. Waring MS, Siegel JA, Corsi RL. Ultrafine particle removal and generatin by portable air cleaners. Atmos Environ. 2008;42:5003‐5014. [Google Scholar]
- 77. Tsuda A, Henry FS, Butler JP. Particle transport and deposition: basic physics of particle kinetics. Compr Physiol. 2013;3:1437‐1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Lai AC, Nazaroff W. Modeling indoor particle deposition from turbulent flow onto smooth surfaces. J Aerosol Sci. 2000;31:463‐476. [Google Scholar]
- 79. Darquenne C. Aerosol deposition in health and disease. J Aerosol Med Pulm Drug Deliv. 2012;25:140‐147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Roy CJ, Milton DK. Airborne transmission of communicable infection—the elusive pathway. N Engl J Med. 2004;350:1710‐1712. [DOI] [PubMed] [Google Scholar]


