Introduction
Since January 2020, the coronavirus disease 2019 (COVID‐19) has swept across the United States affecting all facets of the population. As of the end of May 2020, there have been over 100 000 deaths in the United States attributed to the infection. 1 COVID‐19 has put an unprecedented strain on the U.S. healthcare system. In Physical Medicine and Rehabilitation (PM&R), the scope of challenges varies greatly depending on location, practice setting, and subspecialty. 2 In some states where the outbreak was especially severe, such as New York, many physiatrists found themselves working on the front line. 3 For doctors with outpatient practices, telemedicine visits became the new normal. 4 This pandemic not only shifted the medical practice of PM&R but also had a great impact on medical education. 5 Fellows and residents faced alterations in their schedules and routines as many were redeployed to other services to work with COVID‐19 positive patients in the emergency department, intensive care unit, or other medical unit. 3 In an effort to not slow education, didactics and other learning opportunities moved to the virtual realm. 3 pm&R societies and subspecialty organizations hosted daily didactics for interested learners and webinars on navigating care during COVID‐19. Medical students also felt the impact of the global crisis as in‐person classes were moved online, clinical rotations were canceled, and board exams were postponed. 6 , 7 Changes in work environment and policy standard as a result of COVID‐19 posed great challenges for the entire field of physiatry. At every level, these challenges gave way to opportunity for innovation using available technologies. To understand the immediate impact of the COVID‐19 pandemic on PM&R medical education and practice, and gain insights into how technology was leveraged for health care and education, the experiences and insights from persons within, or committed to, PM&R were pooled. This information was utilized to create an anonymous survey that was distributed online to the PM&R community. We also share portions of the personal accounts used to inform the surveys as they offer unique perspectives on the impact of COVID‐19 on PM&R.
Methods
This study was classified as exempt by the institutional review board at the University of Texas Health Science Center at San Antonio. In an attempt to capture the mood and environment of the time, and inform the survey, the investigators compiled experiences and feelings of COVID‐19's effects on the landscape of the field of physiatry from persons committed to the field: a medical student, an intern, a resident, a residency program director, and a department chair. Using these compiled experiences and opinions, the survey was designed with the goal of determining the adoption of the use of virtual patient care and education modalities in PM&R during the COVID‐19 pandemic. The survey was designed to provide a series of questions customized to the responder's level of education (medical student, intern, resident/fellow, or attending physician). Once each responder selected their level of education, they received a tailored set of questions to gauge their challenges and experiences with education and patient care. Regardless of survey track, the electronic survey consisted of a series of approximately 15 questions. Responders to the survey answered multiple choice, short answer, and Likert scale questions. The survey is available online here: https://bit.ly/2TBBqrT. Participants from the field of PM&R and medical students interested in the field were invited to participate in the anonymous electronic survey that was distributed online via Google Forms, through social media platforms, and via email by way of program coordinators and program directors at the 93 Accreditation Council for Graduate Medical Education (ACGME) accredited PM&R residency programs in the United States. No identifying information was collected, and all responses were kept anonymous. The survey's online dissemination and anonymity prevented the ability to calculate a response rate. Responses were collected from 21 April 2020 to 30 April 2020. Responders were medical students and interns committed to PM&R, PM&R residents, PM&R fellows, and attending physiatrists.
Descriptive statistics were evaluated for each level of education separately to summarize the descriptions of single variables for each group (ie, percentage responses). Chi‐square and Kruskal‐Wallis H tests were performed on the Likert scale data by converting each answer (strongly disagree‐strongly agree) to an ordinal value (1‐5). Our analysis focused on each individual level of education independently and did not look at the differences between these groups. All statistical analysis was conducted using SPSS Statistics (SPSS for Mac OSX, Version 26.0.0.0, IBM Corp., Armonk, NY).
Results
The survey was completed by 501 people including 178 (35.5%) attending physicians, 183 (36.5%) residents and fellows, 29 (5.8%) interns, and 111 (22.2%) medical students. One resident began but did not complete the survey. Thirty‐nine states were represented, as well as the District of Columbia and Puerto Rico. The states most represented were Texas (20.1%), New York (10.9%), Pennsylvania (9.9%), Illinois (6.4%), and Ohio (6.2%). Responses from other states represented <5% of the sample each. Demographics of those responding to the survey are reported in Table 1.
Table 1.
Demographics of members of the PM&R community who answered the survey
| Category | n (%) (n = 501) |
|---|---|
| Level of education | |
| Attending physician | 178 (35.5) |
| Fellow and resident (PGY2‐PGY4) | 183 (36.5) |
| Intern (PGY1) | 29 (5.8) |
| First‐ and second‐year medical student | 27 (5.4) |
| Third‐ and fourth‐year medical student | 84 (16.8) |
| Attending physician work setting ‐ prior to COVID‐19 | |
| Completely inpatient | 16 (9.0) |
| Mostly inpatient | 22 (12.4) |
| Mix inpatient/outpatient | 58 (32.6) |
| Mostly outpatient | 35 (19.4) |
| Completely outpatient | 47 (26.4) |
| Attending physician work setting ‐ following COVID‐19 | |
| Telehealth | 118 (66.3) |
| Inpatient rehabilitation | 88 (49.4) |
| Outpatient rehabilitation | 66 (38.2) |
| Inpatient medicine | 13 (7.3) |
| Fellow and resident physician work setting ‐ prior to COVID‐19 | |
| Completely inpatient | 51 (28.0) |
| Mostly inpatient | 23 (12.6) |
| Mix inpatient/outpatient | 33 (18.2) |
| Mostly outpatient | 24 (13.2) |
| Completely outpatient | 51 (28.0) |
| Fellow and resident physician work setting ‐ following COVID‐19 | |
| Inpatient rehabilitation | 99 (53.5) |
| Telehealth | 62 (33.5) |
| Outpatient rehabilitation | 45 (24.3) |
| Inpatient medicine | 22 (11.9) |
| Emergency department | 3 (1.6) |
| Intern physician work setting ‐ prior to COVID‐19 | |
| Completely inpatient | 20 (69.0) |
| Mostly inpatient | 4 (13.8) |
| Mix inpatient/outpatient | 4 (13.8) |
| Mostly outpatient | 0 (0) |
| Completely outpatient | 1 (3.4) |
| Intern physician work setting ‐ following COVID‐19 | |
| Inpatient medicine | 24 (80.0) |
| Emergency department | 5 (16.7) |
| Inpatient rehabilitation | 5 (16.7) |
COVID‐19 = coronavirus disease 2019; PGY = postgraduate year; PM&R = physical medicine & rehabilitation.
Of the 178 attending physicians responding to the survey, 84.3% spent a majority of their time in patient care prior to the viral outbreak. This decreased to 60% following the outbreak. Physicians spending most of their time doing administrative work increased from 10.7% to 26.3% after the outbreak. Prior to the outbreak, physicians responding to the survey were evenly distributed across inpatient and outpatient work settings. After the outbreak, a majority of physicians reported telehealth as being their main workplace. Many others responded that they were now working in a completely inpatient setting with 7.3% of responders noting a redeployment to inpatient medicine teams (Table 1). A small minority of physiatrists reported using telehealth for patient care before the pandemic. This number increased to over 86% after the viral outbreak (Table 2). Following the start of the pandemic, the majority of attending physicians responded agree or strongly agree to the question, “I feel comfortable with telehealth.” A summary of attending physician opinions on telehealth can be seen in Figure 1. At the time that the survey was collected, most physicians reported that they felt that telehealth visits were inappropriate for an initial patient encounter. However, 82.5% of the same sample felt that the service was sufficient for follow‐up visits (Figure 1). Almost all physicians responding to the survey also felt that telehealth is going to play a larger role in patient care after the COVID‐19 pandemic (Figure 1). The number of physicians utilizing telehealth after the viral outbreak increased in all practice settings, with the largest increase being an 84.5% increase in physicians practicing in a mixed inpatient/outpatient setting. The changes in telehealth use from before to during the pandemic can be visualized in Figure 2. Physicians who were practicing in mixed outpatient or completely outpatient settings were significantly more comfortable with telehealth use than those who worked mostly or completely in inpatient rehabilitation (χ2(4) = 19.180, P = .001). Practice setting prior to the viral outbreak had no impact on views of the future of telehealth within the field (χ2(4) = 5.127, P = .275). These results can be seen in Figure 3.
Table 2.
Objective measures on transition to telemedicine and virtual education from survey responders. Series of questions are divided by education level; attending physician, resident/fellow, and intern answers are represented separately
| Response | ||
|---|---|---|
| Question | Yes n (%) | No n (%) |
| Attending physicians (N = 178) | ||
| Completed telehealth visits prior to COVID‐19 | 26 (16.6) | 152 (85.4) |
| Completed telehealth visit post COVID‐19 | 154 (86.5) | 24 (13.5) |
| Residents/fellows (N = 182) | ||
| Attended virtual didactics prior to COVID‐19 | 37(20.3) | 145(79.7) |
| Attended virtual didactics post COVID‐19 | 169(92.9) | 13(7.1) |
| Institutional collaboration for virtual didactics with other institutions | 93(51.1) | 89(48.9) |
| Attended virtual didactics from other organizations | 143(78.6) | 39(21.4) |
| Interns (N = 29) | ||
| Attended virtual didactics prior to COVID‐19 | 7(24.1) | 22(75.9) |
| Attended virtual didactics post COVID‐19 | 27(93.1) | 2(6.9) |
| Institutional collaboration for virtual didactics with other institutions | 13(44.8) | 16(55.2) |
| Attended virtual didactics from other organizations | 17(58.6) | 12(41.4) |
COVID‐19 = coronavirus disease 2019.
Figure 1.
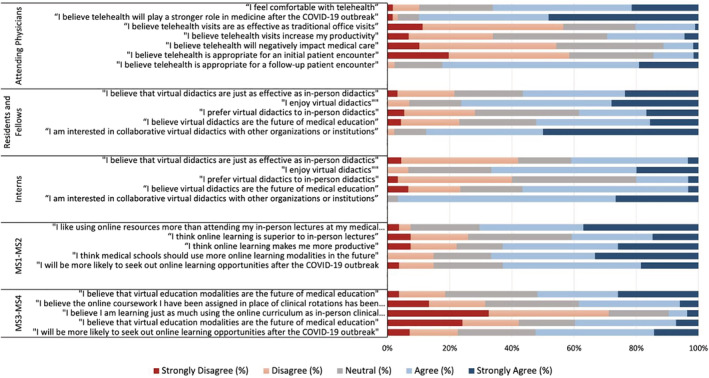
The figure shows each group of participants in the survey (attending physicians, resident and fellows, interns, and medical students) and their survey responses to multiple survey questions. Each set of questions was tailored to their level of training. For example, attending physicians answered questions focused on telehealth whereas residents, interns, and students answered questions focused on virtual education. Answer choices were recorded on a Likert scale ranging from strongly disagree to strongly agree. Each answer choice is represented by a separate color as represented in the figure. COVID‐19 = coronavirus disease 2019.
Figure 2.
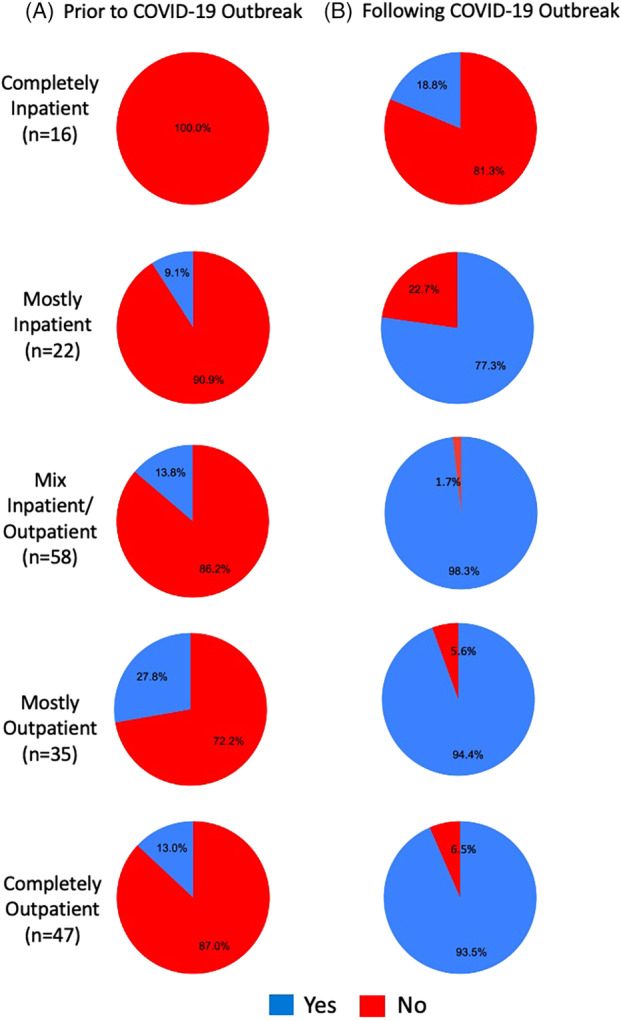
Attending physician use of telehealth before and after the coronavirus disease 2019 (COVID‐19) pandemic by practice setting. Left column (A) represents the physician responses for their telehealth use before the COVID‐19 pandemic. Right column (B) represents the responses of attending physicians following the outbreak. Each row represents a practice setting, labeled to the left of the figure. The response of “Yes” indicating the use of telehealth is represented in color blue. The response of “No” representing no use of telehealth is represented in the color red. Percentages represent the percentage of responses for each practice setting for before and after the pandemic.
Figure 3.
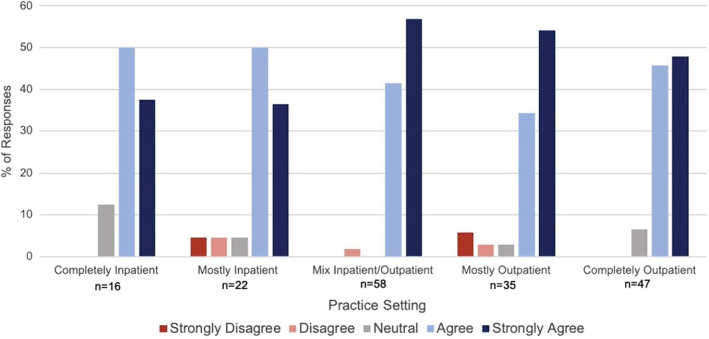
Attending physician responses to survey question “I believe telehealth will play a stronger role in medicine after the COVID‐19 pandemic.” Responses are separated by attending physician practice settings. Responses per practice setting are shown as percentages of each answer to the question ranging from strongly disagree to strongly agree. COVID‐19 = coronavirus disease 2019.
Before COVID‐19, PM&R trainees, as would be expected, worked in a variety of settings, evenly distributed through inpatient and outpatient services. Following the outbreak, most residents shifted to inpatient rehabilitation services with 13.5% of residents being redeployed to non‐PM&R services (Table 1). Only 20.3% of residents reported attending virtual lectures prior to the virus. This number grew to more than four times the amount after the COVID‐19 pandemic (Table 2). Half of trainees responding to the survey reported that their institution collaborated with other institutions for virtual didactics. A total of 78.6% of residents reported having either attended didactics from other institutions or hosted by a national organization during the pandemic. Of the residents surveyed, 76.4% enjoyed virtual didactics and the majority of residents felt that they were as effective as in‐person didactics; 52.2% felt that this new platform was the future of resident education. Residents who attended virtual didactics provided by other residencies or national organizations were more likely to report that they enjoyed virtual didactics in general (χ2(4) = 9.881, P = .020), thought they were as effective as in‐person didactics (χ2(4) = 11.509, P = .021), and preferred them to in‐person didactics (χ2(4) = 10.477, P = .033). Residents' opinions of virtual education can be viewed in Figure 1.
Before COVID‐19, interns worked in a variety of settings across inpatient and outpatient medicine, with 65.6% working in the inpatient setting. After the outbreak, 98.7% found themselves working on inpatient medicine team, or in the emergency department (Table 1). Approximately one third of interns surveyed had their United States Medical Licensing Examination (USMLE) Step 3 or Comprehensive Osteopathic Medical Licensing Examination (COMLEX) Level 3 exam canceled because of the outbreak. Virtual didactics were available to less than a quarter of interns that responded to the survey prior to COVID‐19 and almost universally to all of them after the pandemic (Table 2). Interns' opinions of virtual education can be viewed in Figure 1.
Of medical students who responded to the survey, 87.5% had scheduling of their USMLE Step 1 or COMLEX Level 1 affected and 55% had scheduling of their USMLE Step 2 or COMLEX Level 2 affected. In addition, 94% of students that responded to the survey had scheduling of fourth year elective rotations affected and 60.4% of fourth‐year medical students who responded to the survey had their graduation date affected. Virtual lectures were more common at all times among medical students who responded to the survey with 51.8% of first‐ and second‐year medical students reporting having attended online lectures prior to the outbreak and 100% of students reported attending lectures online after the pandemic. A majority (62.9%) of students felt that online learning makes them more productive and 62.5% of students will seek out further virtual learning opportunities after the pandemic. Additional students' opinions on virtual education can be seen in Figure 1.
Discussion
PM&R has felt the impact of the global crisis, and day‐to‐day activities of both patient care and education have been greatly affected, as demonstrated by our survey results of attending physicians, trainees, and students in the field of PM&R. Many physicians saw a shift in their work environment and residents had to adjust to new services and modes of education. The severity of the pandemic led to some physiatrists and residents in epicenters to work on the frontlines. Practice settings may continue to be affected for some time as COVID‐19 patients survive the acute illness and transition into a post‐acute phase of rehabilitation. In order to capture the environment at the time that this survey was completed, we have chosen to include extended portions, both in table and narrative form, of the personal perspectives obtained when formulating the survey (see the Limitations section and Table 3).
Table 3.
Reflections and perspectives from the authors from each level of education: department chair, residency program director, resident, intern, and medical student. Each column highlights the challenges, solutions and future implications that the pandemic brings from their respective point of view
| Challenges | Solutions | Future Implications | |
|---|---|---|---|
| Department Chair |
|
|
|
| Program Director |
|
|
|
| Resident |
|
|
|
| Intern |
|
|
|
| Student |
|
|
|
ACGME = Accreditation Council for Graduate Medical Education; COVID‐19 = coronavirus disease 2019; PM&R = physical medicine & rehabilitation; PPE = personal protective equipment.
Physicians quickly made the adaptation to using telehealth as the viral outbreak evolved with the percentage of physiatrists using telehealth increasing from 14.6% to 86.5% of physicians. The use of telehealth was seen to ubiquitously increase across all practice settings, regardless of the percentage of time spent in the outpatient setting. Although many physicians did not think that the service was amenable to initial patient visits, they did believe that telehealth had value for patient follow‐up. Most physiatrists responding to the survey felt that telemedicine will be utilized to a greater extent as the medical community moves forward from the threat of COVID‐19. This sentiment was not affected by the work setting of the responder of the survey, further indicating that the use of this platform may continue by all members of the field. Physicians who practiced more in the outpatient setting prior to COVID‐19 felt more comfortable with the use of telehealth than those who spent a majority of their time in the inpatient setting. Despite this, all attending physicians showed a rapid adaptation of telehealth. This finding mirrors some findings of a recent survey study focused on one outpatient sports medicine department that found that most patients found value in their telehealth visits, nearly all of the physicians in the study rated their experience with telehealth positively and all of the physicians in the study planned on using telehealth if reimbursement for the service continued. 8 This use of telehealth has rapidly expanded because of a waiver from the Center for Medicare and Medicaid Services (CMS), and organizations like the American Medical Association (AMA) plan on fighting to maintain these new policies post pandemic. 9 , 10 There are barriers to the use of telehealth including difficulty in communicating with patients with sensory disability, the inability to perform a majority of the physical exam, and technological faults. 8 The use of telehealth within physiatry will most certainly be an area for deeper evaluation and reflection. Not only were clinical patterns changed by COVID‐19, but so was education. Medical education of trainees and medical students could not continue in the same way given the new safety considerations brought on by COVID‐19. Still, educational opportunities had to continue in order to prepare residents for board exams and maintain national accreditation standards (ACGME) as much as possible. 11 Many residents had virtual lecture and education experiences in medical school; however, this was not the norm in residency with only 19.9% of residents reporting virtual didactics pre‐COVID‐19. With over 90% of residents reporting attending virtual didactics after the viral outbreak, it is clear that this was an adjustment made by residency programs to continue providing the training their residents required. Residents that attended virtual didactics from other residency programs and national institutions had a significantly more positive outlook on virtual didactics, with 60.9% who attended collaborative didactics finding virtual didactics to be as effective as in‐person didactics, compared to 38.4% of the cohort who did not attend collaborative virtual didactics sharing this sentiment. Similarly, 81.2% of the residents who attended collaborative didactics found virtual didactics to be enjoyable compared to only 59.0% of those that did not attend collaborative didactics. This model of communal and virtual education affords the ability to consistently provide high quality lectures from leaders in the field to all trainees and could aid in standardizing didactic education across programs. There are clear limitations to the virtual education model as many didactic sessions have a hands‐on focus such as ultrasound skills and injection technique, which can be lost by using a virtual platform. Despite limitations, virtual education has the potential to enhance traditional medical education following the resolution of the pandemic.
Postponement and cancellation of examinations and elective rotations will have ramifications on the 2021 residency match cycle and beyond and may affect interns as they transition into their first year of PM&R training. Almost a third of current interns had their board exams rescheduled and may be forced to take exams during their PM&R residency. Preparing for their final USMLE or COMLEX exam as they start their physiatry residency may have an impact on their transition to the field. Additionally, the medical school class of 2021 faces new challenges during the residency application cycle as the AAMC along with other national organizations have advised against away rotations and have recommended that all residency interviews be held virtually. 12 These changes and challenges may have lasting impacts on the incoming PM&R residents for the upcoming residency application cycles.
Although this study focused on the technological impact of the COVID‐19 pandemic, the burden the crisis imposed was widespread and variable. Future areas of study should focus on the economic impact on the field of physiatry, and operational changes outside of the virtual realm that facilities were forced to take due to the surge of post‐critical care patients.
Limitations
Our study has limitations, including interpreting the results of this survey. Because of the nature of the survey being disseminated anonymously online, it is not possible to calculate a true response rate. Although the survey was shared with all residency program directors and program coordinators in the country, due to the anonymity of the survey we could not determine which institutions responded to or shared the form. Although a response rate could not be calculated, it has been found that for a web‐based survey with no added monetary incentive, response rate is approximately 17.1%. 13 Also, by distributing on a virtual platform there may be self‐selection bias toward responders with a predilection to the use of virtual technology.
To supplement the findings of the survey, we present and share excerpts from the personal accounts and opinions that were used to create the survey. We felt these perspectives, although not always technologically based, give important insight to the tenor and sense of the environment surrounding the field of physiatry at the time the survey was collected.
A Medical Student Perspective
Medical students face uncertainty and angst because of broad changes to milestone events of medical education. Waves of board exam cancellations, with minimal notification from testing centers, caused confusion and panic among those who spent months preparing. 14 After hours of preparing their resumes and themselves for the residency application circuit, medical students are left with the uncertainty around the fate of elective rotations and interview season. In addition to accepting cancellations of match day celebrations and graduations, fourth‐year students had to bear the weight of entering the beginning of intern year during a pandemic. Others graduated early and supported those on the front lines. 15 Although the crisis caused loss, and provided challenges to students, some found opportunities for growth and innovation to improve their medical career and also help their peers. The challenges, solutions, and future implications for medical students can be found in Table 3.
An Intern Perspective
Overall, internship training during COVID‐19 pandemic completely changed. Medical licensing examinations were canceled, along with didactics, grand‐rounds, and hands‐on procedural training, and virtual education became the new normal. Interns had to quickly adapt the effects of this infectious crisis, including the uncertainty of their medical education in the future. Being an intern during COVID‐19 was unique and provided a mix of fear, excitement, and uncertainty. However, there was the opportunity for residency programs and trainees to reevaluate and improve resident medical education systems. Being an intern during COVID‐19 pandemic was challenging on many levels. These challenges allowed interns to grow and build autonomy faster than they otherwise would have and created a strong and confident foundation for their practice of medicine. Further discussion on challenges, solutions, and future implications for interns can be found in Table 3.
A Resident Perspective
Though tension surrounding COVID‐19 in early March 2020 was rising, most in the U.S. medical system were not yet aware of the forthcoming threat that COVID‐19 would present. Because of the dramatic and swift effects of COVID‐19, PM&R residents began discussing the virus and its potential implications on their experience as residents. Downtime was spent tracking the growing number of cases and learning more about the disease from international experiences. Although some PM&R residents, including many in New York City, would ultimately participate in acute medical care of persons with COVID‐19 due to high disease burden on their institutions, 3 the majority of the country shifted their focus to inpatient rehabilitation and remote clinical management, as evidenced by our survey results. Training efforts were buttressed by robust virtual conferencing efforts at the level of national professional societies and academic institutions.
The use of remote clinical support systems is of particular importance to residents. One model that was employed by some PM&R departments included the use of remote teams to support inpatient resident teams. The benefit was offloading inpatient burden while simultaneously protecting residents from unnecessary exposures, thus ensuring residents were available to provide care if some were exposed. This strategy also prevents fatigue and burnout in a unique way and perhaps improves program cohesion as residents work more closely to support one another intra‐ and interprofessionally. Further discussion on challenges, solutions, and future implications for residents can be found in Table 3.
A Program Director Perspective
PM&R residency programs spend years cultivating teaching faculty, refining didactic schedules, optimizing resident exposure and more in order to perfect training of their residents to meet all standards. COVID‐19 has strained and continues to strain these systems in a host of new and unanticipated ways. One of the most unexpected ways this is occurring is through inequality. There is no bias involved, but it is true that PM&R residency education during the time of COVID‐19 is uneven. For example, many programs in New York have been granted Stage 3: Pandemic Emergency Guidance Status with residents redeployed to general medicine floors or intensive care units. 16 These residents are working long hours and are emotionally and physically drained from working on these services. They do not have time, nor are they expected to study PM&R specific topics or attend PM&R didactics. Still many programs in other states throughout the country are not functioning under emergency status but are facing limitations in education due to social distancing. The PM&R community has banded together, and several programs are sharing online and virtual education with one another.
Wellness is difficult to measure during this time in residents or attendings. PM&R is made up of many different personalities; however, most trainees did not enter PM&R believing they would deal with daily life and death situations. The recurring toll of such interactions could certainly lead to burnout or depression. Also, many residents, their families, or loved ones are affected directly by COVID‐19. How can a resident be expected to acquire knowledge if, for example, one of their parents is sick in the hospital? Still other residents seem to thrive in this environment.
Regardless of resident personality, physical isolation can take its toll over time and perhaps the most important job of a residency program is providing a sense of community and nonjudgmental support. In the end, all residents are human, and all humans should be treated with respect and feel cared about. From this place of security, the new normal of PM&R education in the time of COVID‐19 will emerge. The challenges, solutions, and future implications for program directors can be found in Table 3.
A Department Chair Perspective
Many adaptations at the faculty level during COVID‐19 have been required. Faculty have many duties: teaching, mentoring, research, patient care, administration, and more. In PM&R, we have an ampersand that holds together the physical medicine and rehabilitation. Although some faculty in the inpatient rehabilitation setting may have seen little change to their daily tasks, the role of the outpatient PM&R physician changed. Outpatient clinics and elective procedures were overwhelmingly canceled and there is now more utilization of telemedicine. 4 , 17
As we learn from collective experiences around the COVID‐19 pandemic, we have to remain adaptable in the way we deliver care. Often, this means changes in how a patient is being evaluated. For example, an attending physician may be the only one entering a patient room or may have to do all visits via telemedicine. Ultimately, patient care and education will adapt.
Overall, there needs to be frequent and transparent communication with faculty, staff, and trainees. Again, adaptability and a holding presence is key in this situation. There must be understanding that levels of stress and grief will be high in this situation. Wellness and mental health services should be readily available. Faculty and trainees may have significant personal stressors, for example issues with childcare. Moreover, faculty may also be feeling financial losses given closing of clinics and procedures being canceled. Finally, a department should create a team to help create a new normal as we continue in this pandemic. The challenges, solutions and future implications for the department's chair can be found in Table 3.
Conclusion
The COVID‐19 pandemic has strained every facet of the medical system in the United States. The field of PM&R has had to quickly respond to the rapidly changing burden of the global crisis. Although these changes have created many stressors around patient care and education, they have also provided the opportunity for adaptation and growth by shifting to virtual modalities for patient care and education. The survey provided insight that PM&R physicians made the transition to telemedicine to provide safe care to patients. Responders to the survey also highlighted the collaboration of residency programs and national organizations across the country to provide lectures through virtual platforms to offload burdened faculty while maintaining high‐quality educational content. The pandemic provided teachable moments that allowed PM&R to revisit traditional routines in medical education and adapt to new practices to enhance educational and patient experiences. As the field moves forward and the pandemic resolves, the lessons learned will continue to augment the treatment of patients and education of trainees. We foresee continued successful use of these new virtual platforms to enhance patient care and trainee education.
Disclosure: Dr. Escalon, Dr. Tieppo Francio, Mr. Raum, and Dr. Eubanks have no disclosures related to this work. Dr. Verduzco‐Gutierrez has no disclosures related to this work. She serves as Social Media editor of the American Journal of Physical Medicine and Rehabilitation. She has also been a consultant or done prior research with Allergan, Merz, Ipsen, Medtronic, and ReNeuron.
References
- 1. WHO (COVID‐19) homepage . World Health Organization website. https://covid19.who.int/region/amro/country/us. Published May 3, 2020. Accessed May 3, 2020.
- 2. McNeary L, Maltser S, Verduzco‐Gutierrez M. Navigating coronavirus disease 2019 (Covid‐19) in physiatry: a CAN report for inpatient rehabilitation facilities. PM R. 2020;12:512‐515. 10.1002/pmrj.12369. [DOI] [PubMed] [Google Scholar]
- 3. Escalon M, Herrera J. Adapting to the COVID‐19 pandemic in New York City. Am J Phys Med Rehabil. 2020;99(6):453–458. 10.1097/PHM.0000000000001451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Verduzco‐Gutierrez M, Bean AC, Tenforde AS, Tapia RN, Silver JK. How to conduct an outpatient telemedicine rehabilitation or prehabilitation visit. PM R. 2020;12:714‐720. 10.1002/pmrj.12380. [DOI] [PubMed] [Google Scholar]
- 5. Gallagher TH, Schleyer AM. "We signed up for this!" ‐ student and trainee responses to the Covid‐19 pandemic. N Engl J Med. 2020;382:e96. 10.1056/NEJMp2005234. [DOI] [PubMed] [Google Scholar]
- 6.Whelan A, Prescott J, Young G, et al. Guidance on medical students' participation in direct patient contact activities. Association of American Medical Colleges. https://www.aamc.org/system/files/2020‐04/meded‐April‐14‐Guidance‐on‐Medical‐Students‐Participation‐in‐Direct‐Patient‐Contact‐Activities.pdf. Accessed April 1, 2020.
- 7. National Board of Medical Examiners website . Coronavirus (COVID‐19): Assessment Information and Updates. https://www.nbme.org/news/coronavirus-covid-19-assessment-information-and-updates. Updated April 3, 2020. Accessed April 17, 2020.
- 8. Tenforde AS, Iaccarino MA, Borgstrom H, et al. Feasibility and high quality measured in the rapid expansion of telemedicine during COVID‐19 for sports and musculoskeletal medicine practice. PM R. 2020. https://onlinelibrary.wiley.com/doi/10.1002/pmrj.12422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Center for Medicare & Medicaid Services website . Medicare Telemedicine Health Care Provider Fact Sheet. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet. Updated March 17, 2020. Accessed May 2, 2020.
- 10. Albert Henry T. COVID‐19 Makes Telemedicine Mainstream. Will it Stay that Way? American Medical Association website. https://www.ama-assn.org/practice-management/digital/covid-19-makes-telemedicine-mainstream-will-it-stay-way. Updated April 29, 2020. Accessed May 1, 2020.
- 11. Holmboe E, Edgar L, Hamstra S. The Milestones Guidebook. Accreditation Council for Graduate Medical Education (ACGME); 2016. [Google Scholar]
- 12. Association of American Medical Colleges Web site . Medical Student Away Rotations and in‐Person Interviews for 2020‐21 Residency Cycle. https://www.aamc.org/what-we-do/mission-areas/medical-education/away-rotations-interviews-20201. Accessed April 1, 2020.
- 13. Guo Y, Kopec JA, Cibere J, Li LC, Goldsmith CH. Population survey features and response rates: a randomized experiment. Am J Public Health. 2016;106(8):1422‐1426. https://www.ncbi.nlm.nih.gov/pubmed/27196650. 10.2105/AJPH.2016.303198. Accessed April 9, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. United States Medical Licensing Examination website . USMLE announcements. https://www.usmle.org/announcements/?ContentId=169. Updated May 1, 2020. Accessed May 1, 2020.
- 15. Korn M, Harley‐McKeown L. Medical students in Europe and U.S. graduate early to join coronavirus front‐lines. Wall Street Journal. April, 18. 2020. https://www.wsj.com/articles/medical-students-in-europe-and-u-s-graduate-early-to-join-coronavirus-front-lines-11587233541. Accessed April 20, 2020. [Google Scholar]
- 16. Accreditation Council for Graduate Medical Education (ACGME) website . Three Stages of GME during the COVID‐19 Pandemic. https://acgme.org/COVID-19/Three-Stages-of-GME-During-the-COVID-19-Pandemic. Accessed April 17, 2020.
- 17. Karri J, Seymour M, Verduzco‐Gutierrez M, Jayaram P. Point of care procedures in physiatry: practice considerations during the covid‐19 pandemic. Am J Phys Med Rehabil. 2020;99(7):567–570. https://www.ncbi.nlm.nih.gov/pubmed/32398402. 10.1097/PHM.0000000000001463. Accessed July 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]


