Abstract
COVID‐19 has posed major challenges for health care. Hospitals around the world have needed to rapidly prepare for the emerging pandemic. Translational simulation – simulation that is integrated and focused on emerging clinical priorities – offers numerous opportunities to aid in pandemic preparation. We describe our approach to preparing our institution’s maternity services for the COVID‐19 pandemic using translational simulation. We suggest lessons for providers of maternity services, and for those who support them through simulation activities.
Keywords: coronavirus, COVID‐19, maternity, simulation, translational simulation
Introduction
COVID‐19 has posed major challenges for health care. Hospitals around the world have needed to rapidly prepare for the emerging pandemic. Translational simulation – simulation that is integrated and focused on emerging clinical priorities – offers numerous opportunities to aid in pandemic preparation for individuals, teams and healthcare systems. 1
We describe our approach to preparing our institution’s maternity services for the COVID‐19 pandemic using translational simulation. We suggest lessons for providers of maternity services, and for those who support them through simulation activities.
What do We Need to Change for COVID‐19?
Healthcare teams caring for maternity patients with COVID‐19 face many challenges. Wearing personal protective equipment (PPE) during usual patient care is difficult. Communication while wearing PPE and working in and out of isolation rooms is challenging. Traditional team structures and coordination for clinical emergencies need to change. Healthcare equipment such as emergency boxes and trolleys can no longer be brought into contaminated rooms. Our clinical and educational leaders anticipated a number of key challenges in preparing for the COVID‐19 pandemic.
How do we manage obstetric emergencies when it takes several minutes to put PPE on effectively?
How do we communicate in and out of isolation rooms when we can’t just pick up our phones?
How do we manage time critical birth suite emergencies such as post partum haemorrhage (PPH) that usually require a large coordinated team and equipment such as PPH boxes to be brought into rooms?
How do we safely transfer patients to theatre with COVID‐19?
How do we effectively coordinate a multidisciplinary team for emergencies such as an urgent caesarean section?
How Might Translational Simulation Help in Theory
Many maternity units use simulation for teaching and education, including maternity drills and obstetric emergency courses. ‘Translational’ simulation describes a healthcare simulation strategy focused directly on improving patient care and systems – through diagnosing safety and performance issues, and delivering simulation‐based interventions. 1 Applications include testing new clinical facilities before opening to identify latent systems issues, and trialling new operating theatre procedures or protocols. Targeting team and system level performance, translational simulation may employ a range of simulation techniques – in situ simulations in clinical environments, task trainer skills training, logistical tabletop exercises and instructional videos.
Given the urgency and high stakes nature of the changes required, we employed a translational simulation strategy to iteratively diagnose issues, then test and embed revisions into systems and protocols. This rapid simulation prototyping of solutions allowed clinicians to develop inventive solutions and enact change immediately without prolonged delays.
What We Did in Practice
Gold Coast University Hospital (GCUH) has an active multidisciplinary simulation service. On 8 March 2020 we introduced a simulation strategy for COVID‐19 preparation. 2 The GCUH simulation service delivered more than 250 translational simulations involving more than 1500 healthcare staff from many departments. 2
Maternity simulations involved over 250 staff participants. Simulations included multiple large‐scale ‘in situ’ simulations in the clinical environments involving multidisciplinary teams from midwifery, obstetrics, anaesthetics, neonatal, logistical support staff and perioperative staff. Maternity services have a limited ability to reduce clinical activity for our pregnant patients, and this added further challenges for preparation while maintaining service delivery.
Initially a multidisciplinary team developed maternity COVID‐19 simulation scenario packages. These packages are now freely available on the Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) website – COVID‐19 Maternity Simulation Scenarios. 3
Our maternity team started with a diagnostic in situ simulation of a fetal bradycardia requiring an emergency caesarean section in a pregnant woman with COVID‐19. This simulation was utilised as it required coordination of a large multidisciplinary team and transfer of a pregnant woman with COVID‐19 through to the operating theatre. This initial diagnostic simulation identified multiple difficulties in the care of women with COVID‐19. Challenges included the logistics of donning and doffing PPE, communication difficulties in and out of isolation rooms, division of inside and outside teams, equipment difficulties in the isolation room, logistics of transfer to the operating theatre, patient flow through the operating theatre and coordination of the multidisciplinary team.
Following this initial diagnostic simulation, multiple logistical walk through simulations with key stake holders were performed to further identify issues and trouble‐shoot solutions. Smaller educational simulations occurred for practice of PPE and normal birth. Further large‐scale simulations included a respiratory deterioration of a pregnant woman with COVID‐19 on the maternity ward requiring intubation and an emergency caesarean section. We also performed multiple simulations involving a postnatal woman with COVID‐19, diagnosed with a large PPH who required transfer and management in the operating theatre.
What We Developed for Our Maternity Unit
Following the initial diagnostic simulations, we aimed to rapidly develop solutions for the difficulties we identified. This included multidisciplinary education on donning (DON) and doffing (DOFF) PPE, allocation of appropriate spaces in both birth suite and theatre for this to occur, and upskilling of PPE ‘buddies’ to observe the donning and doffing processes. We trialled solutions for the communication difficulties in and out of isolation rooms and between clean and contaminated areas of the operating theatre – which involved speaker phones, baby monitors, walkie talkies, intercoms and Facetime. Single‐use grab bags for emergency equipment were developed including grab bags for PPH, instrumental birth, neonatal resuscitation and anaesthetic induction equipment (Fig. 1).
Figure 1.
Prepacked neonatal COVID‐19 birth suite bags.
High‐impact single‐page infographics were developed to disseminate information to the wider maternity team not directly involved in the simulations. This included infographics on normal birth, midwifery and obstetric team structures for COVID‐19 maternity emergencies and management differences for PPH for COVID‐19 patients both in and out of theatre (Fig. 2). The team is now disseminating these work flows through educational videos. Overall our maternity unit followed three distinct phases using translational simulation, including a diagnostic phase, a testing phase and an embedding phase (Fig. 3).
Figure 2.
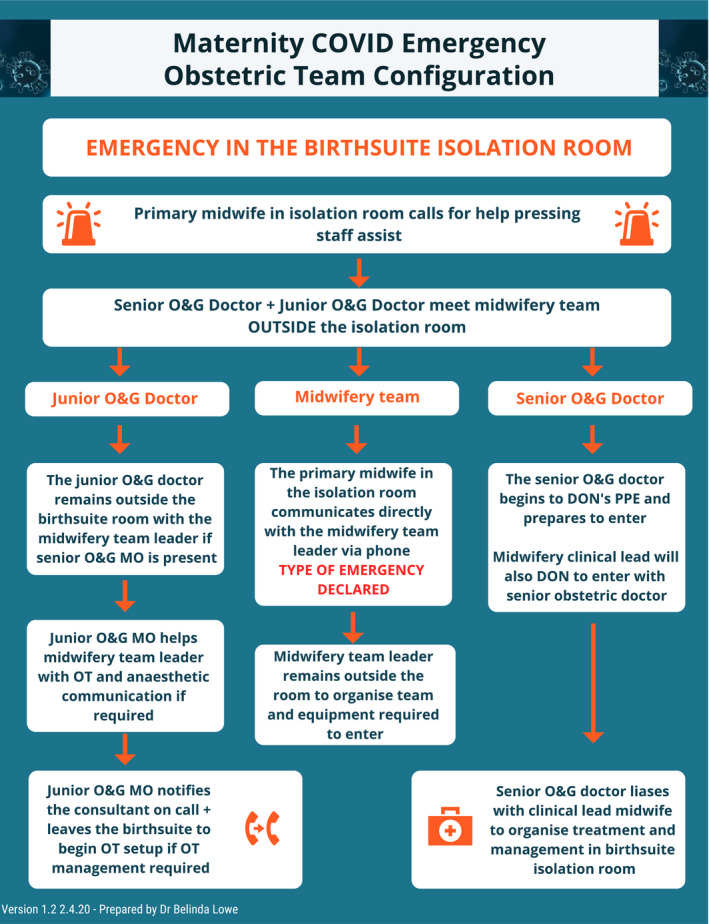
Maternity COVID emergency obstetric team configuration.
Figure 3.
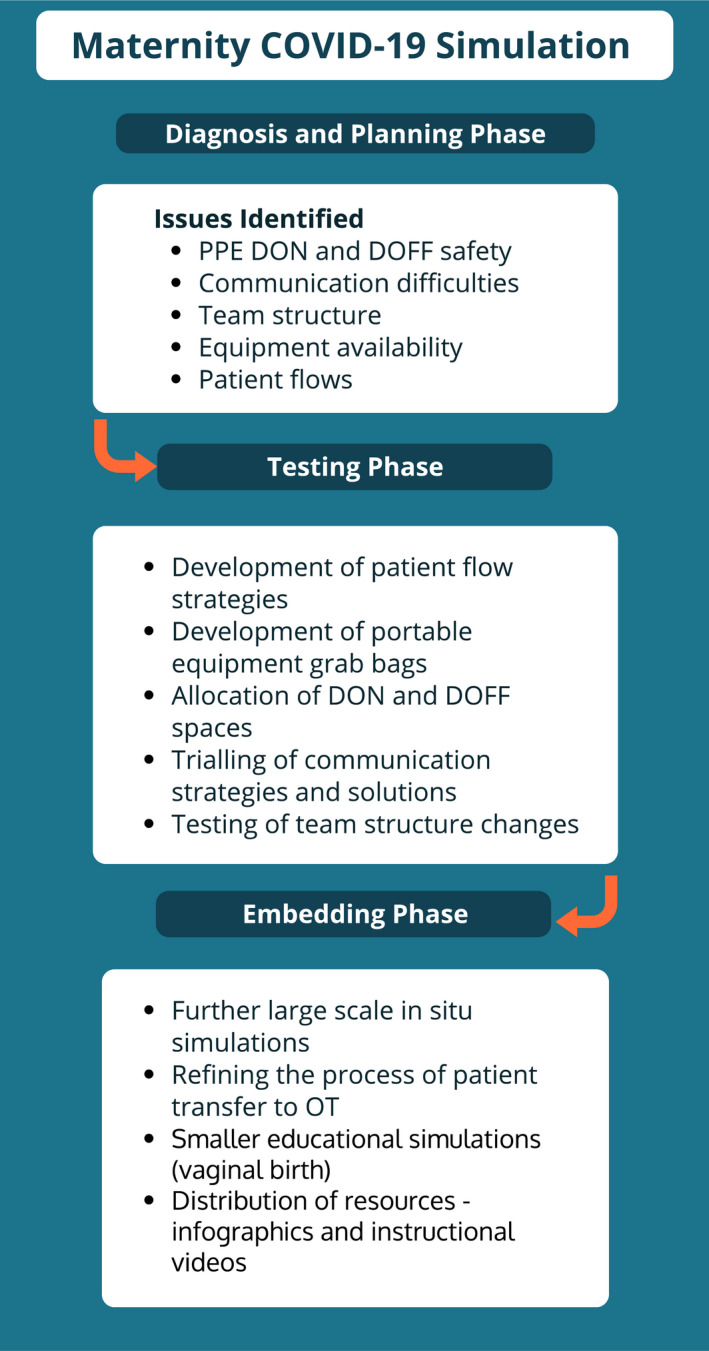
Maternity COVID‐19 simulation phases.
What We Learned About Simulation and Change Management
There are many common themes learnt in the maternity COVID‐19 simulations performed and several of the lessons learnt were consistent with those from COVID‐19 simulations performed by the GCUH simulation team across the hospital. Challenges of PPE, communication, team structure, equipment and patient flows for COVID‐19 patients occurred across specialities.
Maternity COVID Simulation Lessons Learned
Safe PPE DON and DOFF requires education and PPE ‘buddies’ should be used wherever possible
PPE DON and DOFF is time‐consuming and will impact the management of obstetric emergencies
Communication in isolation rooms is difficult – solutions have included speaker phones, baby monitors and walkie talkies
Teams should consider who will be needed both in and out of the isolation room for patients with COVID who have an obstetric emergency
Minimise teams needed to treat emergencies in isolation rooms wherever possible
Managing obstetric emergencies without usual equipment in rooms is challenging – consider pre‐packaged single‐use grab bags for vital equipment, eg PPH
Patient flow through theatre is completely different – consider the location of DON and DOFF spaces and theatre flow logistics
Clarify neonatal plans and consider the use of pre‐prepared single‐use bags for neonatal resuscitation
Somewhat unexpectedly, simulation was also an instrumental tool in helping team anxiety and feelings of preparedness. When faced with confirmed and suspected COVID patients, the maternity team reiterated the importance simulation had played in team preparation.
Tonight we had a caesarean section for a suspected COVID case. I just wanted to say thanks… the SIMs [simulations] made the situation so much easier to navigate. It is helping us all prepare
Translational simulation was a highly effective tool to rapidly identify the systems and processes that needed to change for maternity patients with COVID‐19. This strategy helped our team diagnose potential systems issues, and select appropriate simulation techniques to test potential solutions and embed changes required to safely care for maternity patients with COVID‐19.
The COVID‐19 pandemic has highlighted the importance of maternity units having translational simulation capability. The preparations performed would not have been possible without strong existing skills in simulation and established relationships between the simulation team and maternity clinicians.
Ethics Approval
The project was reviewed by the Human Research Ethics Committee at the Gold Coast Health Service and ethical waiver granted (LNR/2020/QGC/62707)
Conflicts of Interest: The authors report no conflicts of interest.
References
- 1. Brazil V. Translational simulation: not ‘where?’ but ‘why?’ A functional view of in situ simulation. Adv Simulat 2017; 2(1): 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Brazil V, Lowe B, Ryan L et al. Translational simulation for rapid transformation of health services, using the example of the COVID‐19 pandemic preparation. Adv Simulat 2020, Early online. doi: 10.1186/s41077-020-00127-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. The Royal Australian and New Zealand College of Obstetricians and Gynaecologists [homepage on the internet]. Australia: COVID‐19 Maternity Simulation Scenarios. [Cited 18 April 2020.] Available from URL: https://ranzcog.edu.au/news/covid‐19‐maternity‐simulation‐scenarios?fbclid=IwAR1naYv0GAJHkDjsCezZBm0O9aMY9w9KAKsyIsviIWlPrjnzS1H1_YBLvm4 [Google Scholar]


