Abstract
Background
The COVID‐19 pandemic outbreak might induce acute stress disorder (ASD) to people living in the epidemic regions. The current study aims to investigate the association of COVID‐19‐related stressful experiences with ASD and possible psychological mechanisms of the association among college students.
Methods
Data were collected from 7,800 college students via an online survey during the initial stage of the COVID‐19 outbreak in China (from 31 January to 11 February 2020). Existing scales were adapted to measure stressful experiences, resilience, coping, social support, and ASD symptoms. Path analysis was employed to examine the research hypotheses.
Results
Among the 7,800 college students, 61.53% were women and their mean age was 20.54 years. Both direct and indirect effects from COVID‐19‐related stressful experiences to ASD symptoms were significant. The relationship between COVID‐19‐related stressful experiences and ASD could be mediated by resilience (β = 0.01, p < .001), adaptive coping strategies (β = 0.02, p < .001), and social support (β = 0.01, p < .001); while not being significantly mediated by maladaptive coping strategies.
Conclusion
The findings presented the ASD symptoms related to the COVID‐19 outbreak and the mediating role of interpersonal and intrapersonal factors in the association. Identifying the risk and protective factors is important to reduce acute psychological responses.
Keywords: acute stress disorder, coping strategies, COVID‐19, resilience, social support
INTRODUCTION
In December 2019, a novel coronavirus, which caused the outbreak of coronavirus disease (COVID‐19), was identified as the pathogen of a series of unknown pneumonia cases emerged in Wuhan, China (Chen et al., 2020; Zhu et al., 2020). The COVID‐19 outbreak is creating a confusing and rapidly evolving situation. As a public health emergency, the COVID‐19 outbreak was featured by its rapid transmission (comparable or higher than SARS) (Y. Liu et al., 2020; Rocklöv et al., 2020), uncertainty about how it spreads, and considerable mortality rate (1.4%) (Guan et al., 2020). Consequently, a total of 80,813 COVID‐19 cases were identified as of 13th March in China (NHCC, 2020). Although the number of new cases has lately been decreasing smoothly (NHCC, 2020), a rapidly rising number of exported cases were reported in 114 oversea countries and territories across the globe (more than 118,000 cases), which resulting in almost 4,300 deaths worldwide up to 11th March 2020 (World Health Organization (WHO), 2020a). Responding to such a global public health crisis, WHO characterized COVID‐19 as a pandemic because the coronavirus caused unusual and extensive outbreaks in many countries and very high levels of pandemic in several months and many people had no pre‐existing immunity (WHO, 2020a). At the early stage of the outbreak, the Chinese government also implemented a series of strict self‐ and forced‐quarantine measures, including the historical lockdown of a big city (Wuhan) with a population of over 10 million people (Central People Government‐Hubei Provincial Governmental Portal, 2020). During this outbreak, people living in the epidemic region not only had to face physiological threat, but also unbearable psychological stress (Rubin & Wessely, 2020; Xiang et al., 2020).
Previous outbreaks of infectious disease (e.g. SARS, Ebola, MERS) have shown the detrimental influences of disease‐related stress on emerging psychological distress (Lau et al., 2016; Lee et al., 2018; Zheng et al., 2005). Similarly, the pandemic itself and responses (e.g. city lockdown) to COVID‐19 can also induce various psychological problems in people living in the epidemic regions (Shigemura et al., 2020). In terms of the outbreak, the public face a severe shortage of personal protective equipment (e.g. masks), health personnel, diagnostic facilities, and isolation wards, which is worsened by the unavailability of specific treatments or vaccines (WHO, 2020b). In addition, the unpredictable future of this epidemic has been exacerbated by myths and misinformation, often driven by erroneous news reports and the public's misunderstanding of health messages, thus causing worry in the population (Bao et al., 2020). Regarding the government responses, the quarantine of a big city and the subsequent isolation from social networks, as well as the stigma associated with the epidemic and the inconvenience caused to their daily life results in people living in China becoming more stressed. Further travel bans and some executive orders to quarantine travelers during the spring festival holiday (which sought to contain the outbreak) might also have generated public anxiety. The stressful experiences from either the outbreak itself or the subsequent government responses to the outbreak (e.g. lockdown, travel restrictions) occurred in a very short time period at the early stage of the pandemic, which in all likelihood would induce acute stress disorder (ASD) symptoms. ASD refers to the specific constellations of symptoms occuring within 2–28 days following the traumatic experiences, such as actual or threatened death or serious injury (Bryant et al., 1998). ASD was found to be one of the key precursors for posttraumatic stress disorder (PTSD) (Bryant, 2011) and the diagnosis of ASD was introduced into the DSM‐IV (American Psychiatric Association, 1994) to identify acutely traumatised people who would develop chronic PTSD (Bryant, 2005). For example, meta‐analysis showed that over 50 per cent of the individuals who were diagnosed as ASD would develop chronic PTSD within 6 months of the trauma (Zhou et al., 2015). Therefore, investigating the factors associated with ASD would be beneficial for the prevention of subsequent occurrence of PTSD. To the best of our knowledge, no research has studied COVID‐19‐related ASD. The few studies that investigated ASD symptoms among other emergent public crisis (e.g. earthquakes) were either conducted among the affected individuals or front‐line health care workers (Sattler et al., 2006; Wang et al., 2010). Little is known about the COVID‐19‐related ASD particularly for a large non‐infected community.
A better understanding of the pathways through which COVID‐19‐related stressful experiences link to ASD may allow for future tailored psychological behavioral interventions (Park & Park, 2020). Developmental Systems Theoretical models suggested some environmental and individual assets that may play crucial mediating roles in the development of plasticity in mental and behavior functioning after exposure to stressful experiences for youth (Benson, 2003). The presence of ecological assets (e.g. social support) and individual strengths (e.g. effective coping strategies and resilience) may explain the underlying mechanism of the association between traumatic experiences and mental health (Scales et al., 2016). Resilience, a critical concept in positive psychology, is defined as a personal resource to cope with or overcome a variety of adversities and perceived stress (Connor & Davidson, 2003; Luthar & Zigler, 1991). It has been an area of increasing research to understand that resilience may alter mechanisms underlying the negative effects of stressful experiences on psychological adverse outcomes (Chi et al., 2016; Jamshidi et al., 2017; Wilks & Croom, 2008). Individuals with higher levels of perceived stress may develop lower levels of resilience (Wilks & Croom, 2008). In turn, lower levels of resilience were associated with higher levels of traumatic stress responses and psychological morbidity (Kun et al., 2009; Tugade & Fredrickson, 2004). Additionally, previous research showed that resilience essentially mediated the relationship between traumatic experiences and posttraumatic adjustment (e.g. ASD symptoms) (Daniels et al., 2012; Karatzias et al., 2017). Consequently, it is possible that COVID‐19‐related stressful experiences may affect ASD symptoms through the pathway of resilience among college students.
Other psychosocial factors may also play crucial roles in the development of ASD symptoms after exposure to stressful experiences, particularly coping strategies and social support (Rahat & İlhan, 2016; Wolfe & Ray, 2015). Coping is defined as an individual's use of behavioral and cognitive strategies to modify adverse aspects of their environment, as well as to minimise or escape internal threats induced by stress or trauma (Gil, 2005). Generally, coping can be categorised into adaptive and maladaptive strategies. When the coping strategy aligns with the stressors (e.g. aims at reducing the emotional distress and developing positive self‐instructions), people experience fewer psychological symptoms (e.g. less ASD) after stressful events (Park et al., 2001). Adaptive coping strategies (e.g. trying to look on the bright side) may help individuals to rebuild the meaning of life and integrate the stressful experience with existing cognitive schemas about the self and the world, which were linked with better psychological adjustment (Luszczynska et al., 2005; Prati & Pietrantoni, 2009; Strasshofer et al., 2018). On the contrary, maladaptive coping strategies (e.g. using drinking as an avoidance behavior) were closely associated with more dissatisfaction with life and more severe symptoms of psychological responses after the stressful experiences (Dörfel et al., 2008; Tsay et al., 2001). Thus, coping strategies would serve as another mediator between stressful life events and ASD symptoms, and the mediating effects of distinct coping strategies may vary in accordance with their specific type.
The mediating effect of social support on the association of perceived stress and mental health has long been recognised. Social support refers to support accessible to an individual through social ties to other individuals, groups, and the larger community (Cooke et al., 1988). People commonly access family and social networks to elicit support following trauma; however, the severity of traumatic experiences may detrimentally affect people's perceived social support directly by reducing the social support seeking behaviors (Borja et al., 2009; Mak et al., 2009). In turn, social support is a key resource for traumatised people to move beyond coping with the distress towards accommodating the traumatic experiences in positive ways (Helgeson & Lopez, 2010). Lower levels of social support are strongly related to higher risk of posttraumatic stress symptoms (Brewin et al., 2000; Ozer et al., 2003). Therefore, stressful events may aggravate the severity of ASD symptoms via jeopardising the social support systems for college students. Taken together, a large body of existing research has revealed the mediating effects of resilience, coping strategies, and social support on the association between traumatic experience and psychological morbidity, but whether these factors would serve as mediators between COVID‐19‐related stressful life events and ASD among Chinese college students during the pandemic remains unclear.
Given the limited data and public health significance, the current study aimed to examine the relationship between COVID‐19‐related stressful experiences and ASD as well as the roles of resilience, coping strategies, and social support in mediating the association among college students. Informed by previous studies (Tam et al., 2020), we developed a mediation model (Figure 1). This model hypothesised that (i) COVID‐19‐related stressful experiences would be directly associated with ASD; (ii) resilience, coping strategies, and social support would have a direct association with ASD; and (iii) resilience, coping, and social support would mediate the association between COVID‐19‐related stressful experiences and ASD symptoms.
FIGURE 1.
Hypothetical mediation model.
METHODS
Sample and Study Design
A total of 7,942 college students were recruited online in China. The inclusion criteria were college students: (1) who were currently enrolled in universities; and (2) who were staying in the epidemic areas of Mainland China during the outbreak of COVID‐19. The exclusion criteria were students who showed regularity in responses (i.e. cases whose responses were all constant in the scales). After excluding cases who did not meet the inclusion criteria (n = 142), our final sample consisted of 7,800 individuals, of whom 61.53% were women. The mean age of the sample was 20.54 (SD = 2.11) years, ranging from 18 to 50 years.
With the approval of the Institutional Review Board of the Faculty of Psychology, Beijing Normal University (BNU), data were collected using an online survey from 31 January to 11 February 2020, which could be considered to be the fastigial period of the COVID‐19 epidemic (NHCC, 2020). The anonymous questionnaire was developed and distributed using SO JUMP, a well‐known Chinese online survey platform providing functions equivalent to Amazon Mechanical Turk (Wang et al., 2015). The online survey can be completed using multiple electronic devices, such as laptops and smartphones. Students all provided online informed consent and confirmed their voluntary participation prior to the survey. The invited participants were allowed to share the survey link with other college students. All constructs in the survey were assessed with self‐reports by recalling their experience in the past 1 or 2 weeks.
Measures
Demographics
The demographic characteristics included gender, age, school years (e.g. freshmen), major (e.g. medicine), and current residence (whether in Hubei or other regions of Mainland China).
Acute Stress Disorder (ASD)
An adapted 13‐item Acute Stress Disorder Scale was used to assess ASD (Bryant et al., 2000). Participants were asked to report the extent of symptoms they had experienced during the last week (e.g. “Avoid thinking about the outbreak” and “Intrusive memories about information and reports related to the outbreak”). The response of the scale was rated from 1 (not at all) to 5 (very much). The internal consistency was excellent in this sample (Cronbach's α = 0.94). The sum score ranging from 13 to 65 was used as the indicator of ASD, with higher scores indicating greater levels of ASD symptoms.
COVID‐19‐related Stressful Experiences
COVID‐19‐related stressful experienceswere assessed using a nine‐item scale adapted from the checklist of SARS‐related stressors (Main et al., 2011). Participants answered 1 (yes) or 0 (no) to stressful events, such as whether they heard or talked about the severity and epidemic‐related news from authoritative sources, whether they felt out of control during the outbreak of COVID‐19 and there was disruption to work or study plans, and whether friends or relatives had similar symptoms to the infection. The sum score of the responses to all items were calculated to reflect the levels of stress participants perceived. The range of scores was from 0 to 9, with higher scores indicating higher levels of COVID‐19‐related stressful experiences. The Cronbach's α coefficient was 0.60 for the scale.
Resilience
The 10‐item Connor‐Davidson Resilience Scale (10‐item CD‐RISC) (Campbell‐Sills & Stein, 2007) was used to measure participants' resilience (e.g. “I am able to adapt to change”, “I can deal with whatever comes”). This unidimensional scale was revised from the original 25‐item CD‐RISC (Connor & Davidson, 2003) by Campbell‐Sills and Stein (2007) and demonstrated acceptable internal consistency among Chinese college students (Lyu et al., 2017) (Cronbach's α = 0.86). The responses of each item ranged from 1 (not true at all) to 5 (true nearly all the time) and were summed as a reliable indicator for resilience. Higher sum scores indicate greater levels of resilience. The internal consistency for the scale was 0.96.
Social Support
Social support was assessed using an eight‐item scale adapted from the Multidimensional Scale of Perceived Social Support (MSPSS) (Zimet et al., 1988). In the current study, participants reported their perceived social support from significant others (“There is a special person who is around when I am in trouble or in need”), family (“My family really tries to help me”), friends (“I can count on my friends when things go wrong”), teachers (“My teachers really try to help me”) and organisations (“I know some organisations or hotline services that can provide support and help”) on a 5‐point scale ranging from 1 (not true at all) to 5 (true nearly all the time). A composite score ranging from 8 to 40 was used to indicate the level of social support, with a higher score indicating a higher level of social support. The scale showed excellent internal consistency (Cronbach's α = 0.94).
Coping Strategy
Participants’ coping strategy was measured with an eight‐item scale adapted from the revised version of the Ways of Coping (Folkman & Lazarus, 1985; Folkman et al., 1986). The response options ranged from 1 (never used) to 4 (used a great deal). The results of exploratory and confirmatory factor analyses suggested a two‐factor structure labeled as adaptive coping strategies (e.g. “Tried to look on the bright side”) and maladaptive coping strategies (e.g. “Tried to make myself feel better by eating, drinking, smoking, using drugs or medication, and so forth”), respectively (see Appendix A and Appendix B). Both subscales showed acceptable internal consistency, with Cronbach's α = 0.89 for adaptive coping strategies and Cronbach's α = 0.70 for maladaptive coping strategies. The internal consistency for the total scale was 0.78. Sum scores of the items for two subscales were utilised, respectively, as the final scores with higher scores indicate greater levels of two constructs of coping strategies.
Statistical Analysis
First, descriptive statistics were reported on demographic characteristics, COVID‐19‐related stressful experiences, ASD symptoms, resilience, coping, and social support. Second, correlation analyses were performed to examine the bivariate associations among the variables of interest. Third, a mediation model analysis was conducted to examine whether resilience, social support, and two constructs of coping strategies could mediate the association between stressful experiences and ASD, controlling for potential confounders (e.g. gender, age, students’ grade and major (i.e. whether major in medicine)). Bootstrapping was used to examine the significance of the mediation effect. Bootstrapping is an advanced method that does not impose the assumption of normality of the sampling distribution (Preacher & Hayes, 2008). In our analysis, the indirect effects and their 95% confidence intervals (CI) were estimated using 5,000 bootstrap samples.
To assess the model fit, we used normed χ2 (χ2/df < 3.0), Comparative Fit Index (CFI; 0.95 or above indicating excellent fit, 0.90–0.95 reflecting an acceptable fit), and Tucker‐Lewis Index (TLI; 0.95 or above indicating excellent fit, 0.90–0.95 reflecting an acceptable fit) as the indicators of model fitness. We also used the Root Mean Square Error of Approximation (RMSEA; 0.05 or below indicating excellent fit, 0.05–0.08 reflecting an acceptable fit), Standardised Root Mean Square Residual (SRMR; 0.05 or below indicating excellent fit, 0.05–0.08 reflecting an acceptable fit) to evaluate the model fit (Muthén & Muthén, 2012). Statistical analyses were performed using SPSS 22.0 and Mplus 7.1 (Muthén & Muthén, 2012).
RESULTS
Preliminary Analysis
Table 1 shows the demographic characteristics of the study participants. Among the final sample, 7,261 were undergraduates (38.60% men, mean age = 20.22 years, SD = 1.68) and 539 were graduates (36.73% men, mean age = 24.79 years, SD = 2.62). Nearly a quarter (23.72%, 1,850/7,800) of participants majored in medical‐related professions (e.g. medicine). In particular, 2.90% (226/7,800) were in Hubei Province, the province which was considered to be the epicenter of the COVID‐19 outbreak compared with other regions in China. Most of the participants were from less severely affected provinces, such as Zhejiang, Guangdong, Henan, Hunan, Jiangxi, Anhui and Beijing.
TABLE 1.
Sociodemographic Characteristics among College Students (n = 7,800)
| Mean (SD) or n (%) | |
|---|---|
| Age, mean (SD) | 20.54 (2.11) |
| Gender, n (%) | |
| Women | 4,799 (61.53%) |
| Men | 3,001 (38.47%) |
| Major, n (%) | |
| Medicine | 1,850 (23.72%) |
| Engineering | 2,286 (29.31%) |
| Science | 1,067 (13.68%) |
| Literature | 748 (9.59%) |
| Management | 659 (8.45%) |
| Economics | 577 (7.40%) |
| Law | 185 (2.37%) |
| Art | 168 (2.15%) |
| Pedagogy | 116 (1.49%) |
| History | 107 (1.37%) |
| Agronomy | 25 (0.32%) |
| Philosophy | 12 (0.15%) |
| School year,n (%) | |
| Freshman | 2,599 (68.21%) |
| Sophomore | 1,624 (20.82%) |
| Junior | 1,780 (22.82%) |
| Senior | 1,258 (16.13%) |
| Current residence, n (%) | |
| Hubei Province | 226 (2.90%) |
| Other regions in Mainland China | 7,574 (97.10%) |
Table 2 shows the mean scores and standard deviations of the variables, as well as the correlation matrix among all the variables included in the model. The results showed that stressful experiences were positively and significantly correlated with ASD, whereas it was negatively associated with protective indicators, including resilience, social support, and adaptive coping strategies. Resilience, social support, and adaptive coping strategies were positively and significantly associated with each other and negatively related to ASD. Maladaptive coping strategies were moderately associated with resilience, social support, adaptive coping strategies, and ASD. In addition, ASD was positively associated with stressful experiences and maladaptive coping strategies, and negatively related to resilience, social support, and adaptive coping strategies.
TABLE 2.
Correlation Matrix of Measured Variables
| M ± SD | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|
| 1 Stressful experiences | 4.54 ± 1.81 | 1 | |||||
| 2 Resilience | 37.46 ± 8.48 | −0.25*** | 1 | ||||
| 3 Social support | 31.52 ± 7.02 | −0.20*** | 0.52*** | 1 | |||
| 4 Adaptive coping strategies | 15.99 ± 2.81 | −0.18*** | 0.54*** | 0.51*** | 1 | ||
| 5 Maladaptive coping strategies | 6.66 ± 2.22 | 0.01 | 0.09*** | 0.04*** | 0.21*** | 1 | |
| 6 ASD | 27.00 ± 11.00 | 0.22*** | −0.21*** | −0.20*** | −0.20*** | 0.25*** | 1 |
ASD, Acute stress disorder; SD, Standard deviation.
p < .001.
Path Analysis of the Hypothetical Mediation Model
The direct path coefficient from the predictor (stressful experiences) to the criterion (ASD) in the absence of the mediators was significant (β = 0.22, p < .001), indicating that stressful experiences were positively associated with ASD. A multiple mediation model with four mediators and a direct path from stressful experiences to ASD was established and is shown in Figure 2. After controlling for covariates (i.e. gender, age, school year, and students' major), the final model showed a good model fit: χ2/df = 7.21; CFI = 0.99; TLI = 0.97; RMSEA = 0.03; SRMR = 0.02. Specifically, stressful experiences were negatively associated with resilience (β = −0.24, p < .001), social support (β = −0.20, p < .001), and adaptive coping strategies (β = −0.18, p < .001), whilst being positively associated with maladaptive coping strategies (β = 0.02, p < .05) and ASD (β = 0.16, p < .001). The results indicated that participants with higher levels of stressful experiences were more likely to report lower levels of resilience, adaptive coping strategies, and perceived social support. On the contrary, they might have higher levels of maladaptive coping strategies and ASD symptoms. In addition, higher levels of resilience (β = −0.07, p < .001), social support (β = −0.07, p < .001), and adaptive coping strategies (β = −0.16, p < .001) were associated with lower levels of ASD. Finally, maladaptive coping strategies (β = 0.30, p < .001) were positively associated with ASD symptoms.
FIGURE 2.
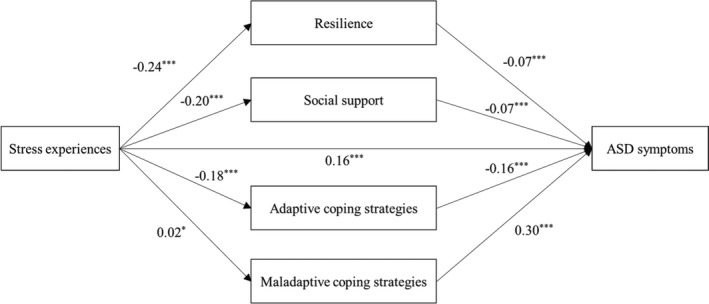
The multiple mediation model of stressful experiences on ASD. Note: * p < .05, ** p < .01, *** p < .001. ASD: Acute stress disorder. All of the parameter coefficients are standardised results.
Indirect Effects
The results from bootstrapping showed that stressful experiences were indirectly related to ASD via resilience, social support, and adaptive coping strategies, with standardised indirect effects of 0.02 (95% CI = [0.01, 0.02]), 0.01 (95% CI = [0.01, 0.02]), and 0.03 (95% CI = [0.02, 0.03]), respectively. However, the mediating effect of maladaptive coping strategies was not significant (see Table 3). The indirect effects explained 29.86% of variance in ASD. Hence, these results revealed that resilience, social support, and adaptive coping strategies partially mediated the link from stressful experiences to ASD symptoms among the participants.
TABLE 3.
Standardised Direct, Indirect, and Total Effects for the Mediation Model
| Model pathways | Standardised estimated effects | 95% CI | p | |
|---|---|---|---|---|
| Lower 2.5% | Upper 2.5% | |||
| Indirect effects | 0.06 | 0.06 | 0.08 | <.001 |
| Stress experiences → Resilience →ASD | 0.01 | 0.01 | 0.02 | <.001 |
| Stress experiences → Social support → ASD | 0.01 | 0.01 | 0.02 | <.001 |
| Stress experiences → Adaptive coping strategies → ASD | 0.02 | 0.02 | 0.03 | <.001 |
| Stress experiences → Maladaptive coping strategies → ASD | 0.00 | −0.00 | 0.01 | .074 |
| Direct effect | 0.16 | 0.13 | 0.18 | <.001 |
| Total effects | 0.22 | 0.19 | 0.25 | <.001 |
ASD, Acute stress disorder; CI, Confidence intervals. Total effect = indirect effect + direct effect.
DISCUSSION
This study was conducted in a critical time period (i.e. the early stage of the COVID‐19 outbreak) and was timely in capturing how COVID‐19‐related stressful experiences affect ASD in a large, non‐infected sample of community college students in China, which is of important public health significance. To the best of our knowledge, this is one of the first studies trying to understand the association between COVID‐19‐related stressful experiences and ASD symptoms as well as the mediating roles of resilience, coping, and social support in the association during the early stage of the COVID‐19 outbreak. Our findings supported that COVID‐19‐related stressful events were directly associated with higher levels of ASD symptoms, but such a link could be indirectly mitigated by intrapersonal (resilience, adaptive coping strategy) and interpersonal factors (social support), although maladaptive coping strategies did not show similar results. Identifying the risk and protective factors at the initial stage of the outbreak is of critical value to envision the psychological impact of both the outbreak and the response (e.g. quarantining a city) to the COVID‐19 health crisis, reduce ASD, and prevent the subsequent occurrence of PTSD.
The findings in the present study emphasised that COVID‐19‐related stressful experiences could be one of the key risk indicators to induce ASD symptoms, which is in line with the results of previous studies conducted during the SARS outbreak (Kwek et al., 2006; Wu et al., 2005). The findings might indirectly reveal the severity of the public panic during the COVID‐19 outbreak. Notwithstanding that the Chinese government implemented rapid and comprehensive physiological and psychological interventions, such as the activation of so‐called first‐level public health emergency responses (e.g. the highest level of emergency public health alerts and responses within the national public health management system) (China Daily, 2020) and released guidelines to promote psychological crisis interventions (e.g. preparing a mental health handbook for the public) (Peking University Sixth Hospital, 2020), the public still suffer high levels of stress from this outbreak. The daily escalating epidemic of COVID‐19 might not give the public enough time to respond properly and thus easily elicit ASD. The specific measures from the government to deal with the public crisis, such as the daily update about the surveillance and active cases on websites and social media, as well as the lockdown of a big city, may not necessarily alleviate the psychological stress but in turn signal the severity of the outbreak. At the same time, the psychological crisis interventions might not have kept up with the physiological measures and thus lost the critical time point to intervene. What is worse, the false rumors about the epidemic and treatment of COVID‐19 on the Internet and social media have increased the spread of public panic to a greater degree. Hence, our findings indicate that a lot of efforts are needed in the future to deal with the ASD symptoms of the outbreak of infectious disease at both the society level and the individual level. For instance, at the society level, effective first aid psychological crisis interventions (e.g. hotline mental health services) need to be implemented in a timely manner and integrated into the prevention measures to contain the outbreak, particularly when taking unprecedented measures (e.g. lockdown). At the same time, the policymakers of the government or the social media should assess the accuracy and guarantee the authenticity of the information before disclosing it in order to decrease uncertainty concerning the disease. At the individual level, avoiding going to public areas and in‐person contact, maintaining moderate physical activities while still following the safety precautions (e.g. staying at home) may also be beneficial for mental health during this critical period (Chen et al., 2020).
In addition, our results showed the mediating effects of multiple factors on the association of COVID‐19‐related stressful experiences and ASD symptoms. Such findings expanded other similar previous research by including resilience, social support, and adaptive coping strategies as the effective intrapersonal and interpersonal protective factors to mitigate the likelihood of ASD symptoms following the outbreak of COVID‐19 (Charuvastra & Cloitre, 2008; Tsay et al., 2001). These mediating effects could possibly be explained because resilient individuals are more capable of dealing with fears from coronavirus stresses, experiencing positive emotions and thoughts, and seeking the necessary social support from family, friends, and teachers, all of which allows them to actively cope with stress and further reduce the ASD symptoms (Feder et al., 2009). Accordingly, the mediation mechanisms of resilience, social support, and adaptive coping strategies on ASD have the following implications for college students. For example, during this kind of emerging health crisis, psychologists and psychiatrists may consider using the internet and social media to target college students in a timely manner when sharing self‐help strategies, such as cultivating resilience and positive emotions and problem‐focused coping strategies, to deal with ASD. Meanwhile, non‐governmental organisations (NGOs), communities, schools, and parents need to be aware of the potential psychological risks of students’ situations (e.g. home confinement, fears of infection, frustration and boredom, and lack of in‐person contact with classmates) (Brooks et al., 2020), being prepared to quickly detect possible mental health problems at a very early stage of the outbreak and provide prompt social support to effectively address these issues (Wang et al., 2020).
It is interesting that maladaptive coping strategies did not significantly mediate the association between COVID‐19‐related stress and ASD symptoms. The possible explanation of this finding was that most of the college students were not from the epicenter of this outbreak (i.e. Wuhan, China) and they might not perceive it as such a severe threat as other pandemic regions. Therefore, they might be less likely to exhibit maladaptive behaviors, especially when most of them stay at home and have their parents monitoring their daily activities. Future studies may benefit from using additional data collected from Wuhan to examine such a relationship. In addition, the adapted subscale for maladaptive coping strategies only included three items which might harm the psychometric quality of the scale and affect the results.
Several limitations are worth noting for the current study. First, the participants in the current study were recruited using a convenience sampling approach. Thus, the study sample may not be representative for all the college students in China. However, we recruited the sample from many universities, which are located in different regions of China, and the results still had strong generalisability. Second, mediation analysis with cross‐sectional data could not establish causality. According to the spirit of mediation modeling and model assumption, future longitudinal studies might be needed to confirm the associations that we found in this study (Maxwell & Cole, 2007). Third, web‐based surveys can facilitate data collection, but selection bias might exist as only those who are familiar with web‐based surveys would respond. Fourth, self‐report data may be subject to social desirability bias. In addition, some scales/items used in this study were adapted from existing scales as no well‐validated measures were available. For example, the low Cronbach’s alpha of stress may threaten the internal validity of the findings in this study. Findings could be strengthened if future studies were to evaluate key variables through additional methods besides self‐report, including family members’ evaluations or direct observations of stress and psychiatry diagnoses of ASD.
Despite these limitations, this study still presents the acute psychological responses related to the COVID‐19 outbreak and the rarely reported mediating role of intrapersonal and interpersonal factors (i.e. resilience, coping, social support) of ASD during this emerging health crisis. Identifying the risk and protective factors at an early stage of the outbreak is important to reduce ASD and prevent future psychological morbidity. The present study has several valuable implications. First of all, given the low utilisation of mental health services, mental health practitioners or psychologists should work to identify individuals experiencing ASD and provide efficient and effective emergency psychological crisis interventions during the outbreak of COVID‐19, and in particular, establish psychological assistance hotlines or online mental health education systems (S. Liu et al., 2020). In addition, communities, schools, and families need to pay more attention to the physical and psychological health of individuals. For instance, communities need to pay close attention to residents’ mental health status. Schools have a critical role in offering an opportunity for students to interact with teachers and obtain immediate psychological counselling when necessary. Family members, as the closest and best resource to seek help from during home quarantine, should support each other with close and open timely communication.
APPENDIX A. . EFA Results of Factoring Loadings for Coping Strategies
| Factor loadings | ||
|---|---|---|
| 1 adaptive coping strategies | 2 Maladaptive coping strategies | |
| (1) Tried to look on the bright side. | 0.88 | 0.07 |
| (2) Rediscovered what is important in life. | 0.88 | 0.09 |
| (3) Made light of the situation; refused to get too serious about it. | 0.79 | 0.18 |
| (4) Tried to control my disappointment, regret, anger, and sadness. | 0.86 | 0.14 |
| (5) Tried to feel better by having a rest, working, or learning. | 0.75 | 0.22 |
| (6) Tried to make myself feel better by eating, drinking, smoking, using drugs or medication, and so forth. | 0.05 | 0.88 |
| (7) Tried to forget the whole thing. | 0.13 | 0.88 |
| (8) Accept the reality because there is no other way. | 0.33 | 0.56 |
Note: Exploratory Factor Analysis (EFA) with half of the participants (n = 3900) was conducted and the results suggested a two‐factor structure (labeled as adaptive coping strategies and maladaptive coping strategies, see Appendix A). This two‐factorial pattern of coping strategies accounted for 67.87% of cumulative variance.
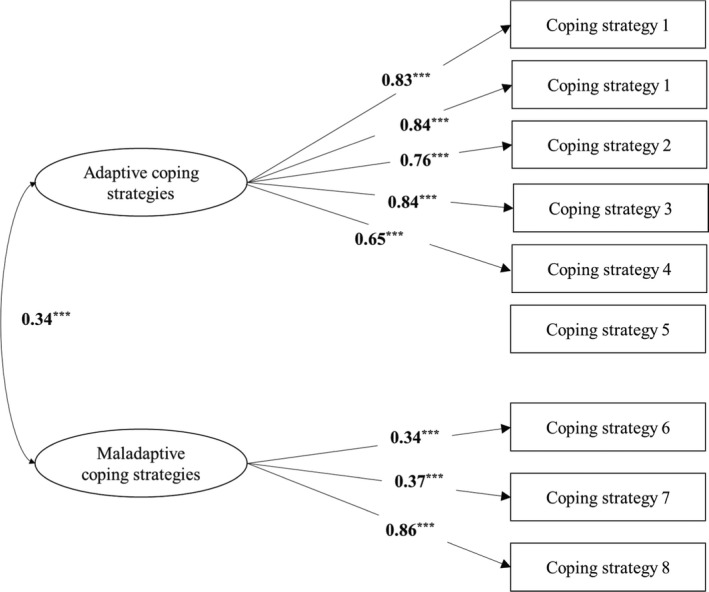
APPENDIX B. . Confirmatory Factor Analysis (CFA) Results of Two‐Factorial Structure of Coping Strategy, n = 3,900
According to items in the domain, the CFA indicates an overall good fit with a RMSEA of 0.07, a CFI of 0.98, a TLI of 0.97, and an SRMR of 0.03, indicating that the latent construct of coping strategy was sufficiently operationalised by the manifest indicator items. *** p < .001.
REFERENCES
[Corrections made on 31 March 2021, after issue publication: Details for Chen et al. (2020) has been updated in this version]
- American Psychiatric Association (1994). Diagnostic and statistical manual of mental disorders (4th edn, Washington, DC: American Psychiatric Association. [Google Scholar]
- Bao, Y. , Sun, Y. , Meng, S. , Shi, J. , & Lu, L. (2020). 2019‐nCoV epidemic: Address mental health care to empower society. The Lancet, 395(10224), e37–e38. 10.1016/S0140-6736(20)30309-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benson, P.L. (2003). Developmental assets and asset‐building community: Conceptual and empirical foundations. In Lerner R.M., & Benson P. (Eds.), Developmental assets and asset‐building communities: Implications for research, policy, and programs (pp. 19–46). New York: Kluwer Academic. [Google Scholar]
- Borja, S.E. , Callahan, J.L. , & Rambo, P.L. (2009). Understanding negative outcomes following traumatic exposure: The roles of neuroticism and social support. Psychological Trauma‐Theory Research Practice and Policy, 1(2), 118–129. [Google Scholar]
- Brewin, C.R. , Andrews, B. , & Valentine, J.D. (2000). Meta‐analysis of risk factors for posttraumatic stress disorder in trauma‐exposed adults. Journal of Consulting and Clinical Psychology, 68(5), 748–766. [DOI] [PubMed] [Google Scholar]
- Brooks, S.K. , Webster, R.K. , Smith, L.E. , Woodland, L. , Wessely, S. , Greenberg, N. , & Rubin, G.J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 395(10227), 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant, R.A. (2005). Predicting posttraumatic stress disorder from acute reactions. Journal of Trauma & Dissociation, 6(2), 5–15. [DOI] [PubMed] [Google Scholar]
- Bryant, R.A. (2011). Acute stress disorder as a predictor of posttraumatic stress disorder: A systematic review. Journal of Clinical Psychiatry, 72, 233–239. [DOI] [PubMed] [Google Scholar]
- Bryant, R.A. , Harvey, A.G. , Dang, S.T. , Sackville, T. , & Basten, C. (1998). Treatment of acute stress disorder: A comparison of cognitive‐behavioral therapy and supportive counseling. Journal of Consulting and Clinical Psychology, 66(5), 862–866. [DOI] [PubMed] [Google Scholar]
- Bryant, R.A. , Moulds, M.L. , & Guthrie, R.M. (2000). Acute Stress Disorder Scale: A self‐report measure of acute stress disorder. Psychological Assessment, 12(1), 61–68. [PubMed] [Google Scholar]
- Campbell‐Sills, L. , & Stein, M.B. (2007). Psychometric analysis and refinement of the Connor–Davidson resilience scale (CD‐RISC): Validation of a 10‐item measure of resilience. Journal of Traumatic Stress: Official Publication of the International Society for Traumatic Stress Studies, 20(6), 1019–1028. [DOI] [PubMed] [Google Scholar]
- Central People Government‐Hubei Provincial Governmental Portal (2020). Municipal headquarters for the prevention and control of pneumonia caused by novel coronavirus (circular No. 1). http://www.wuhan.gov.cn/hbgovinfo/zwgk_8265/tzgg/202001/t20200123304065.html
- Charuvastra, A. , & Cloitre, M. (2008). Social bonds and posttraumatic stress disorder. Annual Review of Psychology, 59, 301–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, P. , Mao, L. , Nassis, G.P. , Harmer, P. , Ainsworth, B.E. , & Li, F. (2020). Coronavirus disease (COVID‐19): The need to maintain regular physical activity while taking precautions. Journal of Sport and Health Science, 9(2), 103–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi, P. , Li, X. , Du, H. , Tam, C.C. , Zhao, J. , & Zhao, G. (2016). Does stigmatization wear down resilience? A longitudinal study among children affected by parental HIV. Personality and Individual Differences, 96, 159–163. [Google Scholar]
- China Daily (2020). Tibet activates highest‐level public health alert. 29 January. https://www.chinadaily.com.cn/a/202001/29/WS5e318a36a3101282172739c1.html
- Connor, K.M. , & Davidson, J.R. (2003). Development of a new resilience scale: The Connor‐Davidson resilience scale (CD‐RISC). Depression and Anxiety, 18(2), 76–82. [DOI] [PubMed] [Google Scholar]
- Cooke, B.D. , Rossmann, M.M. , McCubbin, H.I. , & Patterson, J.M. (1988). Examining the definition and assessment of social support: A resource for individuals and families. Family Relations, 37(2), 211–216. 10.2307/584322 [DOI] [Google Scholar]
- Daniels, J.K. , Hegadoren, K.M. , Coupland, N.J. , Rowe, B.H. , Densmore, M. , Neufeld, R.W.J. , & Lanius, R.A. (2012). Neural correlates and predictive power of trait resilience in an acutely traumatized sample. Journal of Clinical Psychiatry, 73(03), 327–332. [DOI] [PubMed] [Google Scholar]
- Dörfel, D. , Rabe, S. , & Karl, A. (2008). Coping strategies in daily life as protective and risk factors for post traumatic stress in motor vehicle accident survivors. Journal of Loss and Trauma, 13(5), 422–440. [Google Scholar]
- Feder, A. , Nestler, E.J. , & Charney, D.S. (2009). Psychobiology and molecular genetics of resilience. Nature Reviews Neuroscience, 10(6), 446–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folkman, S. , & Lazarus, R.S. (1985). If it changes it must be a process: Study of emotion and coping during three stages of a college examination. Journal of Personality and Social Psychology, 48(1), 150–170. [DOI] [PubMed] [Google Scholar]
- Folkman, S. , Lazarus, R.S. , Dunkel‐Schetter, C. , DeLongis, A. , & Gruen, R.J. (1986). Dynamics of a stressful encounter: Cognitive appraisal, coping, and encounter outcomes. Journal of Personality and Social Psychology, 50(5), 992–1003. [DOI] [PubMed] [Google Scholar]
- Gil, S. (2005). Coping style in predicting posttraumatic stress disorder among Israeli students. Anxiety, Stress & Coping, 18(4), 351–359. [Google Scholar]
- Guan, W.‐J. , Ni, Z.‐Y. , Hu, Y. , Liang, W.‐H. , Ou, C.‐Q. , He, J.‐X. , … Zou, H. (2020). Clinical characteristics of coronavirus disease 2019 in China. New England Journal of Medicine. 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helgeson, V.S. , & Lopez, L. (2010). Social support and growth following adversity. In John W.R., Alex, J.Z. & Hall J.S. (Eds.), Handbook of adult resilience (pp. 309–330). New York: The Guilford Press. [Google Scholar]
- Jamshidi, M.A. , Moghadam, M.F. , Ghorbani, S. , & Farhoush, M. (2017). Self‐efficacy and resilience as mediators in the relationship between test anxiety and spiritual intelligence among high school students in Qom. Journal of Research on Religion & Health, 4(1), 7–21. [Google Scholar]
- Karatzias, T. , Jowett, S. , Yan, E. , Raeside, R. , Howard, R . (2017). Depression and resilience mediate the relationship between traumatic life events and ill physical health: Results from a population study. Psychology, Health & Medicine, 22(9), 1021–1031. [DOI] [PubMed] [Google Scholar]
- Kun, P. , Han, S. , Chen, X. , & Yao, L. (2009). Prevalence and risk factors for posttraumatic stress disorder: A cross‐sectional study among survivors of the Wenchuan 2008 earthquake in China. Depression and Anxiety, 26(12), 1134–1140. [DOI] [PubMed] [Google Scholar]
- Kwek, S.‐K. , Chew, W.‐M. , Ong, K.‐C. , Ng, A.W.‐K. , Lee, L.S.‐U. , Kaw, G. , & Leow, M.K.‐S. (2006). Quality of life and psychological status in survivors of severe acute respiratory syndrome at 3 months postdischarge. Journal of Psychosomatic research, 60(5), 513–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau, J.T. , Wang, Z. , Kim, Y. , Gu, J. , Wu, A.M. , Zhou, Q. , … Hao, Y. (2016). Anticipated negative responses by students to possible Ebola virus outbreak, Guangzhou China. Emerging Infectious Diseases, 22(1), 154–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, S.M. , Kang, W.S. , Cho, A.‐R. , Kim, T. , & Park, J.K. (2018). Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Comprehensive Psychiatry, 87, 123–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, S. , Yang, L. , Zhang, C. , Xiang, Y.‐T. , Liu, Z. , Hu, S. , & Zhang, B. (2020). Online mental health services in China during the COVID‐19 outbreak. Lancet Psychiatry, 7(4), e17–e18. 10.1016/S2215-0366(20)30077-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, Y. , Gayle, A.A. , Wilder‐Smith, A. , & Rocklöv, J. (2020). The reproductive number of COVID‐19 is higher compared to SARS coronavirus. Journal of Travel Medicine, 27(2), 10.1093/jtm/taaa021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luszczynska, A. , Mohamed, N.E. , & Schwarzer, R. (2005). Self‐efficacy and social support predict benefit finding 12 months after cancer surgery: The mediating role of coping strategies. Psychology, Health & Medicine, 10(4), 365–375. [Google Scholar]
- Luthar, S.S. , & Zigler, E. (1991). Vulnerability and competence: A review of research on resilience in childhood. American Journal of Orthopsychiatry, 61(1), 6–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyu, M. , Xi, J. , & Luo, Y. (2017). Daily emotional characteristics in individuals with different resilience levels: Supplementary evidence from experience‐sampling method (ESM). Acta Psychologica Sinica, 49(7), 928–940. [Google Scholar]
- Main, A. , Zhou, Q. , Ma, Y. , Luecken, L.J. , & Liu, X. (2011). Relations of SARS‐related stressors and coping to Chinese college students' psychological adjustment during the 2003 Beijing SARS epidemic. Journal of Counseling Psychology, 58(3), 410–423. [DOI] [PubMed] [Google Scholar]
- Mak, W.W. , Law, R.W. , Woo, J. , Cheung, F.M. , & Lee, D. (2009). Social support and psychological adjustment to SARS: The mediating role of self‐care self‐efficacy. Psychology and Health, 24(2), 161–174. [DOI] [PubMed] [Google Scholar]
- Maxwell, S.E. , & Cole, D.A. (2007). Bias in cross‐sectional analyses of longitudinal mediation. Psychological Methods, 12(1), 23–44. [DOI] [PubMed] [Google Scholar]
- Muthén, L.K. , & Muthén, B.O. (2012). Mplus Version 7 user's guide. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- NHCC (2020). Update on novel coronavirus epidemic situation at 24 :00 on March 13. http://www.nhc.gov.cn/xcs/yqfkdt/202003/816e6f71236b4dca96378df5f6f4ae53.shtml
- Ozer, E.J. , Best, S.R. , Lipsey, T.L. , & Weiss, D.S. (2003). Predictors of posttraumatic stress disorder and symptoms in adults: A meta‐analysis. Psychological Bulletin, 129(1), 5273. [DOI] [PubMed] [Google Scholar]
- Park, C.L. , Folkman, S. , & Bostrom, A. (2001). Appraisals of controllability and coping in caregivers and HIV+ men: Testing the goodness‐of‐fit hypothesis. Journal of Consulting and Clinical Psychology, 69(3), 481–488. [DOI] [PubMed] [Google Scholar]
- Park, S. , & Park, Y.C. (2020). Mental health care measures in response to the 2019 novel coronavirus outbreak in Korea. Psychiatry Investigation, 17(2), 85–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peking University Sixth Hospital (2020). Mental health handbook. Facing novel coronavirus pneumoni, Beijing: Peking University Medical Press. [Google Scholar]
- Prati, G. , & Pietrantoni, L. (2009). Optimism, social support, and coping strategies as factors contributing to posttraumatic growth: A meta‐analysis. Journal of Loss and Trauma, 14(5), 364–388. [Google Scholar]
- Preacher, K.J. , & Hayes, A.F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40(3), 879–891. [DOI] [PubMed] [Google Scholar]
- Rahat, E. , & İlhan, T. (2016). Coping styles, social support, relational self‐construal, and resilience in predicting students' adjustment to university life. Educational Sciences: Theory and Practice, 16(1), 187–208. [Google Scholar]
- Rocklöv, J. , Sjödin, H. , & Wilder‐Smith, A. (2020). COVID‐19 outbreak on the Diamond Princess cruise ship: Estimating the epidemic potential and effectiveness of public health countermeasures. Journal of Travel Medicine, 27(3), 10.1093/jtm/taaa030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin, G.J. , & Wessely, S. (2020). The psychological effects of quarantining a city. BMJ, 2020, 368. [DOI] [PubMed] [Google Scholar]
- Sattler, D.N. , De Alvarado, A.M.G. , De Castro, N.B. , Male, R.V. , Zetino, A. , & Vega, R. (2006). El Salvador earthquakes: Relationships among acute stress disorder symptoms, depression, traumatic event exposure, and resource loss. Journal of Traumatic Stress: Official Publication of the International Society for Traumatic Stress Studies, 19(6), 879–893. [DOI] [PubMed] [Google Scholar]
- Scales, P.C. , Benson, P.L. , Oesterle, S. , Hill, K.G. , Hawkins, J.D. , & Pashak, T.J. (2016). The dimensions of successful young adult development: A conceptual and measurement framework. Applied Developmental Science, 20(3), 150–174. 10.1080/10888691.2015.1082429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shigemura, J. , Ursano, R.J. , Morganstein, J.C. , Kurosawa, M. , & Benedek, D.M. (2020). Public responses to the novel 2019 coronavirus (2019‐nCoV) in Japan: Mental health consequences and target populations. Psychiatry and Clinical Neurosciences, 74(4), 281–282. 10.1111/pcn.12988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strasshofer, D.R. , Peterson, Z.D. , Beagley, M.C. , & Galovski, T.E. (2018). Investigating the relationship between posttraumatic stress symptoms and posttraumatic growth following community violence: The role of anger. Psychological Trauma: Theory, Research, Practice, and Policy, 10(5), 515–522. [DOI] [PubMed] [Google Scholar]
- Tam, C.C. , Benotsch, E.G. , & Weinstein, T.L. (2020). Resilience and psychiatric symptoms as mediators between perceived stress and non‐medical use of prescription drugs among college students. American Journal of Drug and Alcohol Abuse, 46(1), 120–130. [DOI] [PubMed] [Google Scholar]
- Tsay, S.L. , Halstead, M.T. , & McCrone, S. (2001). Predictors of coping efficacy, negative moods and post‐traumatic stress syndrome following major trauma. International Journal of Nursing Practice, 7(2), 74–83. [DOI] [PubMed] [Google Scholar]
- Tugade, M.M. , & Fredrickson, B.L. (2004). Resilient individuals use positive emotions to bounce back from negative emotional experiences. Journal of Personality and Social Psychology, 86(2), 320–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, G. , Zhang, Y. , Zhao, J. , Zhang, J. , & Jiang, F. (2020). Mitigate the effects of home confinement on children during the COVID‐19 outbreak. The Lancet, 395(10228), 945–947. 10.1016/S0140-6736(20)30547-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, J. , Iannotti, R.J. , Luk, J.W. , & Nansel, T.R. (2010). Co‐occurrence of victimization from five subtypes of bullying: Physical, verbal, social exclusion, spreading rumors, and cyber. Journal of Pediatric Psychology, 35(10), 1103–1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, Y. , Yu, Z. , Luo, Y. , Chen, J. , & Cai, H. (2015). Conducting psychological research via the internet: In the west and China. Advances in Psychological Science, 23(3), 510–519. [Google Scholar]
- WHO (2020a). Director‐General's opening remarks at the Mission briefing on COVID‐19—11 March 2020. https://www.who.int/dg/speeches/detail/who‐director‐general‐s‐opening‐remarks‐at‐the‐media‐briefing‐on‐covid‐19–‐11‐march‐2020
- WHO (2020b). Shortage of personal protective equipment endangering health workers worldwide. https://www.who.int/news‐room/detail/03‐03‐2020‐shortage‐of‐personal‐protective‐equipment‐endangering‐health‐workers‐worldwide
- Wilks, S.E. , & Croom, B. (2008). Perceived stress and resilience in Alzheimer's disease caregivers: Testing moderation and mediation models of social support. Aging and Mental Health, 12(3), 357–365. [DOI] [PubMed] [Google Scholar]
- Wolfe, T. , & Ray, S. (2015). The role of event centrality, coping and social support in resilience and posttraumatic growth among women and men. International Journal of Mental Health Promotion, 17(2), 78–96. [Google Scholar]
- Wu, K.K. , Chan, S.K. , & Ma, T.M. (2005). Posttraumatic stress after SARS. Emerging Infectious Diseases, 11(8), 1297–1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang, Y.‐T. , Yang, Y. , Li, W. , Zhang, L. , Zhang, Q. , Cheung, T. , & Ng, C.H. (2020). Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry, 395, 357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng, G. , Jimba, M. , & Wakai, S. (2005). Exploratory study on psychosocial impact of the severe acute respiratory syndrome (SARS) outbreak on Chinese students living in Japan. Asia Pacific Journal of Public Health, 17(2), 124–129. [DOI] [PubMed] [Google Scholar]
- Zhou, Z. , Zhong, X. , Zheng, Y. , & Liu, W. (2015). A systematic review of the relationship between ASD and PTSD. Journal of International Psychiatry, 42(1), 18–22. [Google Scholar]
- Zhu, N. , Zhang, D. , Wang, W. , Li, X. , Yang, B. , Song, J. , … Lu, R. (2020). A novel coronavirus from patients with pneumonia in China, 2019. New England Journal of Medicine, 382(8), 727–733. 10.1056/NEJMoa2001017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimet, G.D. , Dahlem, N.W. , Zimet, S.G. , & Farley, G.K. (1988). The multidimensional scale of perceived social support. Journal of Personality Assessment, 52(1), 30–41. [DOI] [PubMed] [Google Scholar]


