Abstract
Background and Objectives
Coronavirus disease 2019 (COVID‐19) lockdown has presented a unique challenge for sarcoma care. The purpose of this study is to evaluate the early results and feasibility of surgeries for bone sarcomas during the COVID‐19 lockdown.
Methods
Our prospectively collected orthopaedic oncological database was reviewed to include two groups of patients‐ those who underwent surgery in the immediate 4 weeks before lockdown (non‐lockdown group) and those operated in the first 4 weeks of lockdown (lockdown group). All patients were followed‐up clinically and telephonically to collect the outcome data.
Results
Out of the 91 patients who qualified for inclusion, fifty were classified into the non‐lockdown group while 41 patients formed the lockdown group. Both the groups were comparable with respect to baseline demographic parameters. However, during the lockdown period 37 patients (90%) had undergone a major surgical intervention as against 24 patients (48%) in the non‐lockdown group (P < .001). There was no significant difference in type of anaesthesia, median estimated blood loss and procedure duration. None of the patients/health care workers had evidence of severe acute respiratory syndrome‐coronavirus 2 infection at 15 days follow‐up.
Conclusion
Our study results suggest that appendicular bone tumours can be safely operated with adequate precautions during the lockdown period.
Keywords: bone tumour surgery, COVID‐19, lockdown, orthopaedic oncology, safety, sarcoma treatment
1. INTRODUCTION
The coronavirus disease 2019 (COVID‐19) pandemic continues to spread across the globe. Nationwide lockdown has been the most common response by majority of countries across the world to contain the spread. Despite lockdown being the commonest means, there is considerable variability in the response of healthcare systems to the pandemic between different countries. Healthcare systems in advanced countries like Sweden continued to function unabated during the pandemic, while most others have ceased normal functioning due to nation‐wide lockdown. 1 , 2 In India too, a nationwide lockdown was imposed from the midnight of 24 March 2020. This was supposed to be one of the strictest lockdowns in the world. 3
Like in rest of the world, during the nationwide Indian lockdown, it was agreed that elective surgeries had to be deferred and emergency life‐saving procedures should be performed with adequate personal protective equipment (PPE) if COVID‐19 test results are awaited. Yet there was considerable ambiguity on semi‐elective procedures such as bone sarcoma surgery, as it is well known that delay in surgery can significantly increase the mortality risk in these patients. 4 , 5 , 6
As a tertiary bone sarcoma referral centre catering to a large population, we continued to perform oncological procedures during the lockdown period with strict adherence to local protocols. The present study is an evaluation of bone sarcoma patients operated during the lockdown period and their comparison to the cohort operated in the month immediately before the lockdown. We suppose that this study would be useful in providing inputs in formulating guidelines for bone sarcoma surgery in times like the current COVID‐19 pandemic.
2. MATERIALS AND METHODS
The study was conducted at New Delhi where lockdown was in effect from 6 am on 23rd March 2020. We identified two groups of patients, namely the “non‐lockdown group” which was defined as those patients who were operated between 24th February and 22nd March 2020; and the “lockdown group” included those patients operated between 23rd March and 18th April 2020. Data regarding patient demographics, tumour characteristics and intraoperative details were collected from a prospectively maintained, dedicated musculoskeletal oncological database.
As the lockdown was sudden and unprecedented, some changes were made in patient selection for surgical procedures. Ever since lockdown, all patients and their caretakers were thoroughly screened for COVID‐19 symptoms through a safety checklist (Figure 1). Those patients/caretakers, who failed the checklist, were immediately referred to designated COVID‐19 testing area for further evaluation. We did not perform routine COVID‐19 testing on all our preoperative patients as per existing guidelines during that period. All healthcare workers were following the PPE protocols as per hospital guidelines. For those patients who had to undergo a chest computed tomography scan for preoperative staging work up (as per standard sarcoma guidelines), radiologists were asked to specifically look for evidence of COVID‐19 infection to rule out asymptomatic carriers. During surgery, pulse lavage irrigation of the wound was avoided to reduce droplet contamination. 7 However, we continued to use electrocautery albeit minimally so as to reduce intraoperative blood loss. In those procedures where intramedullary reaming was required, power reamers were used as necessary.
Figure 1.
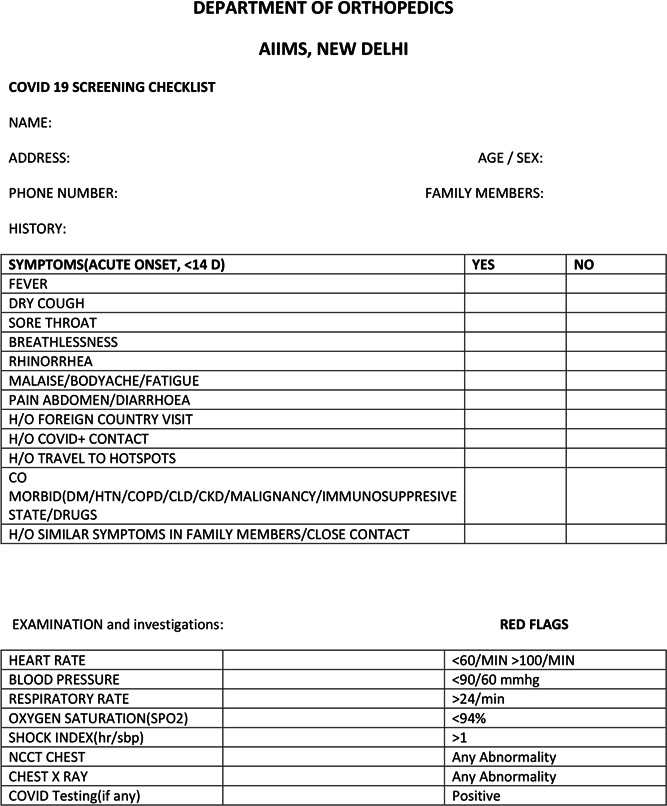
Checklist used for screening patients and their relatives during lockdown
Tele consultation services were provided for sarcoma patients apart from routine hospital visits for wound check. All patients included in the study had a minimum follow‐up of 15 days following the procedure. During follow‐up, apart from routine examination, each patient was specifically asked for symptoms/evidence of COVID‐19.
Statistical analysis was performed using R statistical software version 3.6.1. Categorical data was analysed using the χ 2 test. Fisher's exact test was employed if the expected frequency in any cell was less than 5. Test for normality was employed for continuous data. Those following normal distribution were analysed using the Student t test. Non parametric data were analysed using Wilcoxon test. Statistical significance was attributed when p value is less than or equal to 0.05.
3. RESULTS
A total of 91 patients had been treated during the entire study period. Of these, 50 patients had been classified in the ‘Non‐Lockdown’ group; while the remaining 41 as 'Lockdown' group. Table 1 compares the baseline characteristics between the groups. During the lockdown period, malignant tumours were operated in preference to benign tumours and biopsy procedures (P < .001). The only benign tumour patient that had been operated during lockdown had a displaced pathological fracture of femur secondary to solid ABC for which she had undergone bone grafting and plating. Out of the five giant cell tumor (GCT) patients who had surgery during this period, two had pathological fracture (in proximal femur), two had impending fungation and one nursing mother had distal radial GCT with severe pain restricting her baby care. Hence, these procedures qualified for urgent intervention. The most common location was distal femur followed by proximal tibia in both groups (Figure 2). There was no statistically significant difference in tumour location between the two groups. However, due to logistic reasons, we could not operate upon pelvic and sacral tumours during the Lockdown period.
Table 1.
Comparison of baseline demographic and tumour characteristics between the two groups
| Variable | Lockdown group (n = 41) | Non‐lockdown group (n = 50) | P value |
|---|---|---|---|
| Age (y), mean (SD) | 24.1 (14.9) | 28.6 (17.9) | .188 |
| Sex ratio (male: female) | 21: 20 | 28: 22 | .649 |
| Diagnosis | <.001 | ||
| Osteosarcoma | 12 | 7 | |
| Ewing's sarcoma | 10 | 3 | |
| Chondrosarcoma | 5 | 1 | |
| Other malignant tumours | 4 | 3 | |
| GCT | 5 | 8 | |
| Benign tumours | 1 | 2 | |
| Lesion for biopsy | 4 | 26 | |
| Metastasis | .433 | ||
| Chest | 6 | 2 | |
| Bone | 2 | 0 | |
| Procedure performed | <.001 | ||
| Major | 37 | 24 | |
| Minor (core biopsy) | 4 | 26 | |
| Preoperative chemotherapy | 20 | 9 | .041 |
Note: Bold values mean that the P‐value is significant at <.05.
Abbreviation: GCT, giant cell tumor.
Figure 2.
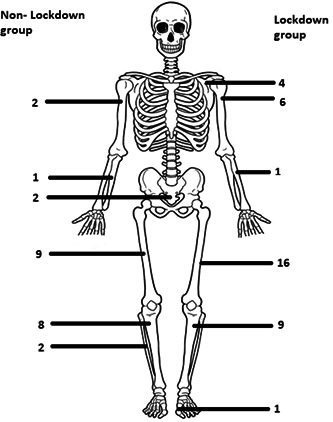
Skeleton diagram comparing the location (bone involved) of tumours between the two groups
There was a significant increase in number of major surgeries performed during lockdown (37 out of 41) as compared with normal period (24 out of 50). This is because of availability of extra theatre time during the lockdown period as other elective orthopaedic procedures like arthroplasty, arthroscopy, etc. were deferred. We had a significantly higher proportion of patients who had pre‐operative chemotherapy in the lockdown group (49% vs 18%). Also, the American Society of Anesthesiologists grades, intraoperative blood loss and duration of procedures were not different compared with nonlockdown group (Table 2). None of the patients had symptoms/evidence of COVID‐19 at a minimum of 15 days follow‐up.
Table 2.
Comparison of perioperative characteristics between the two groups
| Variable | Lockdown group (n = 37) | Non‐lockdown group (n = 24) | P value |
|---|---|---|---|
| Estimated blood loss (in mL) median (IQR) | 500 (400‐800) | 500 (375‐800) | .905 |
| Duration of surgery (in min) median (IQR) | 170 (100‐180) | 165 (110‐215) | .9 |
| ASA grade | .68 | ||
| Grade 1 | 27 | 15 | |
| Grade 2 | 3 | 3 | |
| Grade 3 | 7 | 6 | |
| Grade 4 | 0 | 0 | |
| Anaesthetic method | .103 | ||
| General | 21 | 7 | |
| Regional | 12 | 12 | |
| Combined | 4 | 5 | |
| Procedure type | .55 | ||
| Biological limb salvage | 14 | 7 | |
| Endoprosthetic reconstruction | 9 | 8 | |
| Nail cement spacer | 8 | 7 | |
| Amputation | 6 | 2 | |
| Complications | 2 | 2 |
Abbreviations: ASA, American Society of Anesthesiologists grade; IQR, interquartile range.
Out of the major procedures (n = 37) performed during the lockdown period, 31 (84%) were limb salvage procedures (Table 2). Our choice of reconstruction did not defer during the lockdown period as compared with normal group. However, we had faced certain challenges which will be discussed under a separate heading below. Despite the associated risks, 25 patients (21 GA + 4 combined) had general anaesthesia in the lockdown group. There was no report of health care worker getting infected from an asymptomatic patient carrier either from the anaesthetic or surgical team at a minimum follow‐up of 15 days from the last procedure (until 4 May 2020). However, one of the health care workers was diagnosed to have COVID‐19 about 2 weeks after completion of this study (on 16th May, 2020) which was probably attributed to community transmission on contact tracing. He recovered uneventfully. We had two complications in each group‐two vein injuries which were repaired, one patient had common peroneal nerve coursing through the tumour that had to be sacrificed and one had an iatrogenic cautery burn.
4. DISCUSSION
Surgical procedures during COVID‐19 lockdown are fraught with risk of disease transmission to health care workers as well as to the patient. 8 This acts as a deterrent for appropriate decision‐making in patient care. Guo et al 9 reported an orthopaedic forum survey from Wuhan where they reported the outcomes of 24 orthopaedic surgeons infected by severe acute respiratory syndrome‐novel coronavirus 2 (SARS‐nCoV2) from eight Wuhan hospitals. The common suspected site of infection was either general wards (79.2%) or public places (20.8%) visited by respondents with only 12.5% respondents suspecting infection exposure from operating rooms. An interesting point to note is that all 24 respondents recovered following treatment. On the other hand, deferring surgery for a later date can significantly increase the risk of recurrence of these tumours. Poudel et al 10 had studied the risk factors associated with local recurrence of Osteosarcoma and had reported that each week delay in surgery after completion of neo‐adjuvant chemotherapy increases recurrence risk by 1.14 times. Also, at a mean follow‐up of 2.8 years, just 20% patients with recurrence were surviving as against 60% of survivors in the group without local recurrence. Hence, we continued to serve our patients with due precautions. Even the NHS England report says “cancer services will need to continue ….” and elective surgeries with expectation of cure, prioritised to priority level 2 so as to save life and to prevent progression of disease to beyond operability. 11 , 12
Out of the 41 patients who had been treated during the lockdown, three patients were referred for COVID‐19 screening. In all these three patients, these symptoms were picked up in the waiting area before they entered the ward or operation theatre with the help of the checklist in Figure 1. Out of these three patients, two patients did not require testing as per standard Indian Council of Medical Research guidelines. Hence, they were taken up for surgery. In the third patient, COVID‐19 testing was done and found to be negative. Also, as mentioned earlier, every non‐contrast computerized tomography chest scan was discussed with a radiologist to rule out radiological evidence of COVID‐19. Although there is no fool proof mechanism to identify asymptomatic carriers, a proper checklist and strict adherence to local infectious disease protocol can help in reducing inadvertent disease transmission. This is especially important in a country like India with 1.3 billion population where national lockdown was declared well before the disease entered the community transmission stage. While it is well known that lockdown can plateau the epidemic curve, it should be understood that the disease may not be eradicated in the near future in our setting. Hence, deferring surgery to a later date for sarcomas will only risk patient's life and may put undue pressure on the system when national lockdown is relaxed.
We performed a significantly higher number of major surgeries (90%) during the lockdown. While we had reported increased availability of theatre slots under the “results” section, another important factor is that patients could not reach our tertiary centre due to transport lockdown (Figure 3). We had performed only four biopsy procedures during the 4 week Lockdown period as against 26 biopsy procedures during the preceding 4 weeks. Our hospital caters to patients from at‐least 12 different states in the north and central part of the country and most of our patients belong to the low socioeconomic strata. As lockdowns may become the new normal until we find an efficient vaccine or drug for COVID‐19, the state machinery has to chalk out proper referral pathways for ensuring timely diagnosis and treatment initiation of patients with sarcoma, failing which we may end up losing more lives due to non‐COVID‐19 deadly diseases. This stands true mainly for developing and third world countries where referral mechanisms are not streamlined.
Figure 3.
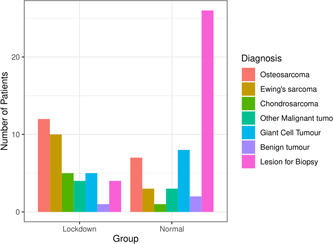
Bar diagram comparing the diagnosis of patients between the two groups [Color figure can be viewed at wileyonlinelibrary.com]
5. CHALLENGES TO SARCOMA SURGERY
As the situation continued to evolve, different challenges were faced by the treating team. To compensate for Intensive Care specialists posted on COVID‐19 intensive care units, we had to cut down on those surgeries that stand a high chance of requiring postop intensive care unit care. Due to cancellation of scheduled blood donation camps, availability of adequate blood products became difficult. Hence, we had to defer pelvic and sacral tumour surgeries for a later date. Few patients with pelvic PNET had to be referred for definitive radiotherapy. Problems were faced in arranging implants, especially endoprosthesis, due to transportation difficulties. Intraoperative frozen section became unavailable as the pathologist deferred the support as per their guidelines due to risk of aerosol generation. 13
6. CONCLUSION
Surgical treatment of bone tumour patients, with strict adherence to personal protective measures and local guidelines, did not increase the risk of contracting SARS‐Cov2 to either Health care workers or patients during the lockdown period. If our effort is to save human lives, irrespective of the disease they suffer from, then Sarcoma surgery shall continue without lowering our guards. National Lockdown and Hospital Lockdown may not go hand‐in‐hand.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
SYNOPSIS
Bone sarcoma surgery during COVID‐19 pandemic lockdown was not associated with increased risk of disease transmission to either the patients or the health care workers. If our effort is to save human lives, irrespective of the disease they suffer from, then Sarcoma surgery shall continue without lowering our guards. National Lockdown and Hospital Lockdown may not go hand‐in‐ hand when it comes to bone sarcoma surgeries.
Kumar VS, Banjara R, Thapa S, et al. Bone sarcoma surgery in times of COVID‐19 pandemic lockdown‐early experience from a tertiary centre in India. J Surg Oncol. 2020;122:825:825–830. 10.1002/jso.26112
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1.COVID‐19 pandemic in Sweden. Wikipedia, 2020. https://en.wikipedia.org/w/index.php?title=COVID-19_pandemic_in_Sweden&oldid=961189922. Accessed 7 June 2020.
- 2.Comparing Six Health‐Care Systems in a Pandemic. Council on foreign relations. https://www.cfr.org/backgrounder/comparing-six-health-care-systems-pandemic. Accessed 7 June 2020.
- 3. Gopichandran V, Subramaniam S, Kalsingh MJ. COVID‐19 pandemic: a litmus test of trust in the health system. Asian Bioethics Rev. 2020;12:1‐221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Penel N, Bonvalot S, Minard V, et al. French sarcoma group proposals for management of sarcoma patients during the COVID‐19 outbreak. Annals Oncol. 2020;31:965‐966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cardoso P, Rodrigues‐Pinto R. Surgical management of bone and soft tissue sarcomas and skeletal metastases during the COVID‐19 pandemic. European J Surg Oncol. 2020;46:1178‐1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bartlett DL, Howe JR, Chang G, et al. Management of cancer surgery cases during the COVID‐19 pandemic: considerations. Ann Surg Oncol. 2020:1‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Simpson AHRW, Dall G, Haas JG. COVID‐19: potential transmission through aerosols in surgical procedures and blood products. Bone Joint Res. 2020;9:200‐201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wong J, Goh QY, Tan Z, et al. Preparing for a COVID‐19 pandemic: a review of operating room outbreak response measures in a large tertiary hospital in Singapore. Can J Anesth. 2020;67:1‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Guo X, Wang J, Hu D, et al. Survey of COVID‐19 disease among orthopaedic surgeons in Wuhan, People's Republic of China. J Bone Joint Surg Am. 2020;102:847‐854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Poudel RR, Tiwari V, Kumar VS, et al. Factors associated with local recurrence in operated osteosarcomas: a retrospective evaluation of 95 cases from a tertiary care center in a resource challenged environment. J Surg Oncol. 2017;115:631‐636. [DOI] [PubMed] [Google Scholar]
- 11. Burki TK. Cancer guidelines during the COVID‐19 pandemic. Lancet Oncol. 2020;21:629‐630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coronavirus » Specialty guides. https://www.england.nhs.uk/coronavirus/secondary-care/other-resources/specialty-guides/#cancer. Accessed 7 June 2020.
- 13.Pathologists TRC of. Document library. https://www.rcpath.org/document-library-search.html?resource_keyword=frozen. Accessed 7 June 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


