Abstract
Objective. To assess and characterize Doctor of Pharmacy (PharmD) students’ well-being across the first professional year (P1) and determine the relationship between the number of examinations taken, student grade point average, and well-being scores.
Methods. All P1 students (N=76) enrolled at one college of pharmacy self-reported their career, community, financial, physical, social, and overall well-being on a weekly basis during the fall and spring semesters. Parametric statistical tests were used to examine the extent to which students’ well-being scores varied throughout the academic year, the extent to which their domain-specific well-being scores predicted overall well-being scores, and the association between their well-being scores and the number of examinations they had taken in a week and their grade point average.
Results. Overall and domain-specific well-being scores significantly decreased from the beginning to the end of fall semester. Students’ overall well-being across the academic year was most frequently predicted by their career well-being, physical well-being, and social well-being scores. Career, community, physical, and overall well-being scores were significantly negatively associated with the number of examinations the students completed during the week. Students’ self-reported overall well-being during the fall semester was positively associated with their fall semester GPA.
Conclusion. Significant variation was found in students’ domain-specific and overall well-being across the P1 year. These findings can guide both the development and timing of school interventions to promote student well-being.
Keywords: well-being, longitudinal, pharmacy student, thriving, suffering
INTRODUCTION
The constructs of well-being and wellness in health professionals, trainees, and students are receiving increased attention in the peer-reviewed literature and lay press. While consensus definitions are arguably lacking for both, and in some cases the terms are considered synonyms, wellness is often defined in terms of health, whereas well-being is usually defined in a more holistic sense. The Centers for Disease Control and Prevention (CDC) has defined well-being as “the presence of positive emotions and moods (eg, contentment, happiness), the absence of negative emotions (eg, depression, anxiety), satisfaction with life, fulfillment and positive functioning.”1 Gallup, a global leader in assessing population and individual-level well-being, operationalizes well-being as five interconnected elements: purpose or career well-being (liking what one does each day), social well-being (having supportive relationships and love in one’s life), financial well-being (the security of one’s finances), physical well-being (having good health and enough energy to get things done daily), and community well-being (liking where one lives and taking pride in the community).2 Using the 0-10 Cantril self-anchoring striving scale as a foundation, Gallup measures levels of well-being in terms of thriving (well-being that is strong, consistent, and progressing; score of 7-10), struggling (well-being that is moderate or inconsistent; score of 4-6) and suffering (well-being that is rated as poor and considered high-risk; score of <4).3,4 Other entities define well-being in more granular domains. For example, Ohio State University, an institution with a vision of becoming the healthiest university and community in the world, categorizes well-being across nine domains.5,6
Among the general population, high levels of well-being (ie, thriving) are desirable and associated with several positive outcomes, including increased engagement, productivity, and satisfaction, as well as lower risk of developing chronic diseases.2,7,8 Specific to health care providers, poor well-being is associated with decreases in satisfaction with their professional career, increases in suicide and suicidal ideation, increases in medical errors, increases in patient morbidity and mortality, and decreases in health care quality outcomes.9-14 Modeling research estimates the annual cost of physician burnout alone to be in the billions of dollars.15 In 2017, the National Academy of Medicine (NAM) established the Action Collaborative on Clinician Well-Being and Resilience to combat increases in provider burnout and to advance the science of resilience and well-being.16 Since 2017, the American Association of Colleges of Pharmacy (AACP), a network organization of the Action Collaborative, has emphasized the importance of clinician well-being and resilience through focused attention in Standing Committee Charges, well-being-specific programming, and approval of policy statements supporting well-being promotion in colleges and schools.17,18 Likewise, the most recent Accreditation Council for Pharmacy Education Standards require schools and colleges of pharmacy to provide services that promote student well-being.19
While research specific to well-being in health professions students is limited, both anecdotal and empirical evidence suggests that students, like clinicians, experience distress and burnout, both of which are negatively associated with thriving.20-23 Stoffel and Cain’s 2018 review of the “grit and resilience” literature in health professions education provides a summary of the protective role of resilience on well-being.24 There is a dearth of information specific to pharmacy education.15,24 Some studies have cross-sectionally examined constructs that align with one or more well-being domains, such as social isolation,21 personal finance perceptions,25 sleep duration,26 and quality of life.27 To date, no studies have examined pharmacy student well-being in a longitudinal manner. In alignment with a 2017 commentary published in the Journal regarding the impact of transitioning to pharmacy school on student well-being,20 the overarching goal of our study was to better understand first professional year (P1) pharmacy students’ perceptions of well-being across an entire academic year. Specifically, the objectives of the study were to: longitudinally characterize P1 students’ weekly self-reported, domain-specific, and overall well-being across the first professional year; determine the extent to which domain-specific well-being predicted overall well-being evaluations across the first professional year; and examine associations of the number of examinations in a week and student grade point average (GPA) with students’ well-being scores.
METHODS
This study was approved by the East Tennessee State University (ETSU) Institutional Review Board. The study population was the 2017-2018 first professional year cohort at the ETSU Gatton College of Pharmacy (N=76). Students were recruited to participate in the study during the first class session of a required course series that spanned from August to December (fall semester) and January to May (spring semester). Consented students completed six TurningPoint (Turning Technologies, Youngstown, OH) audience response questions during each two-hour weekly class session. The questions elicited students’ perceptions of their current well-being across the Gallup-defined well-being domains: career well-being, community well-being, financial well-being, physical well-being, and social well-being. Questions were phrased as, “On a scale from 1 (extremely poor) to 7 (extremely good), I’d describe my current physical well-being as…”. One additional item (“On a scale from 1 (extremely poor) to 7 (extremely good), I’d describe my current overall well-being as…“) elicited students’ perceptions of their current overall well-being. Responses to all items were based on a seven-point scale (1=extremely poor, 2=poor, 3=somewhat poor, 4=neutral, 5=somewhat good, 6=good, 7=extremely good). Students from the previous P1 cohort were recruited to determine the face validity of survey items.
The P1 students were introduced to well-being, including all Gallup domains, the Cantril Self-Anchoring Scale, and the seven-point item response scale during a two-hour didactic and active-learning class session at the beginning of the fall semester. During this class session, students completed a self-reflection exercise in which they identified action items to improve each well-being domain. Reflections were reviewed by the investigator to assess the extent to which student-reported action items reflected an understanding of each well-being domain. Students assessed their well-being for a total of 14 weeks during the fall semester and 11 weeks during the spring semester. Data were not able to be collected during one week of the fall semester and three weeks of the spring semester because of inoperability of the audience response system. Thus, data were collected for 25 out of 29 class sessions across the P1 academic year. Additional times during which data were not collected were the Thanksgiving holiday break (November), one day (February) when classes were cancelled because of inclement weather, and spring break (March).
Data were collected and maintained by the principal investigator, who also taught in the course. Gender was the only demographic variable collected from respondents. Data were linked to individual students until the conclusion of the spring semester, at which time the data set was de-identified. Data were analyzed using SPSS Statistics, version 25 (IBM Corp, Armonk, NY). Descriptive statistics were calculated for all items. To evaluate the cohort using Gallup’s thriving, struggling, and suffering categories, additional variables were constructed using the weekly overall well-being ratings. On the original 0-10 Gallup scale, the cutoff score for thriving was 7; for struggling, 4-6.9, and for suffering, less than 4. Using these parameters as a guide, student ratings of 1-2 were considered suffering; 3-4, struggling; and 5-7, thriving. The number of examinations per week and semester GPA data were obtained from the Office of Academic Affairs.
The Wilcoxon signed rank test was used to evaluate differences in domain-specific and overall well-being scores across the beginning, midpoint, and end of each semester. Linear regression techniques were employed to explore the extent to which domain-specific well-being scores predicted overall well-being scores at the beginning, midpoint, and end of each semester. Multiple imputation techniques were employed to handle missing data. Relationships between the number of examinations in a week and well-being scores were evaluated using Pearson’s correlation coefficient, as were relatonships between students’ averaged overall well-being scores across the semester and GPA for the fall and spring semesters. A p<.05 was considered significant for all statistical analyses.
RESULTS
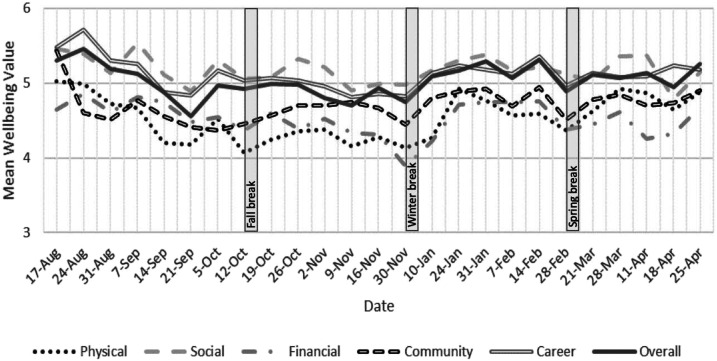
Seventy-six first professional year students participated in the study (100% response rate). Weekly participation rates ranged from 66% to 100% during the fall semester and 62.8%-100% during the spring semester. Average participation across the study period was 81.5%. Twenty-five percent (N=19) of the cohort reported being male. Figure 1 presents the average domain-specific and overall well-being scores reported by students longitudinally across the P1 year. During the fall semester, overall and domain-specific well-being scores decreased from the beginning to the end of the semester (career, mean=5.5 vs 4.8, p<.001; community, mean=5.4 vs 4.5, p<.001; financial, mean=4.7 vs 3.9, p=.001; physical, mean=5.0 vs 4.1, p<.001; social, mean=5.5 vs 5.0, p=.016; overall, mean=5.3 vs 4.8, p=.003). As compared to the end of the fall semester, only community well-being significantly changed (increased) upon returning from winter break (mean=4.5 vs 4.8, p=.018). From spring semester beginning to end, significant increases were noted for physical well-being (mean=4.3 vs 4.9, p=.001) and financial well-being (mean=4.2 vs 4.7, p=.042). Only community well-being significantly varied (decreased) from academic year beginning to end (mean=5.4 vs 4.9, p=.005). Over the course of the academic year, overall well-being significantly differed across gender on one occasion (08/31), with female students reporting higher overall well-being than male students (mean=5.3 vs. 4.8, p=.018).
Figure 1.
Doctor of Pharmacy Students’ Well-being Scores for Career, Community, Financial, Physical, Social, and Overall Across the 2017-2018 First Professional Year
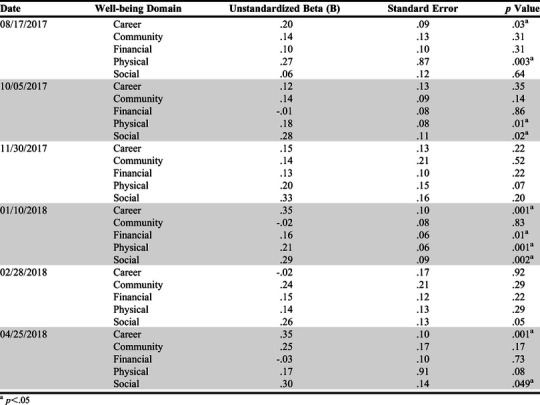
The results of regression analyses used to explore the extent to which domain specific well-being scores predicted overall well-being scores at the beginning, midpoint, and end of each semester are presented in Table 1. Career well-being, physical well-being, and social well-being predicted students’ overall well-being at three points across the academic year, whereas financial well-being predicted overall well-being one time and community well-being zero times. Physical well-being was the most frequent predictor of overall well-being in the fall semester, and career and social the most frequent predictors in the spring semester.
Table 1.
Predicting Doctor of Pharmacy Students’ Overall Well-being Scores Across the First Professional Year
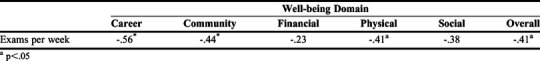
The relationship between students’ domain-specific and overall well-being scores and the number of examinations during the same week are presented in Table 2. Weekly career, community, physical, and overall well-being scores were significantly negatively associated with the number of examinations in the same week, with career well-being having the strongest association (r=-.56, p<.05). Students’ average overall well-being for the fall semester was positively associated with their fall semester GPA (r=.25, p=.039). No relationship was noted between aggregated spring overall well-being scores and spring GPA (r=.16, p=.185).
Table 2.
Correlation Between Pharmacy Students’ Well-being Scores and Number of Examinations Taken During the Same Week
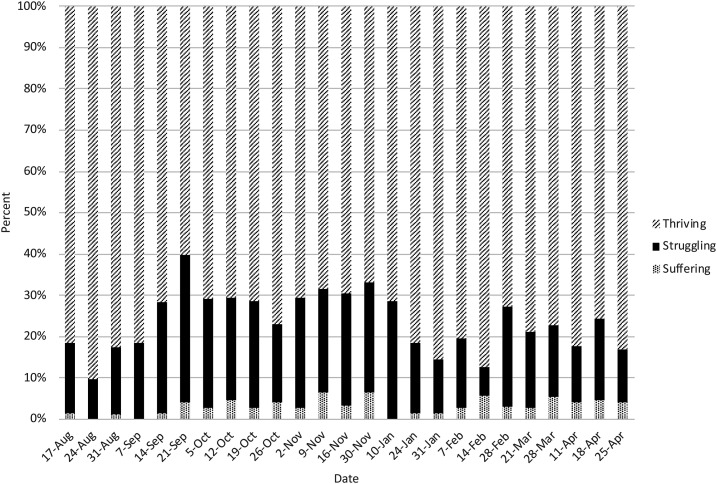
Based on self-reported overall well-being, a longitudinal analysis of the percent of students who provided responses categorized as thriving, struggling, and suffering across the P1 academic year is presented in Figure 2. The percent of students categorized as suffering in a given week ranged from 0% in weeks 2 and 4 of the fall semester and week 1 of the spring semester to 6.4% in week 12 and the final week of the fall semester. Across the academic year, 17 students (22.4%) reported overall well-being scores that would place them in the suffering category at least one time, and 55 students (72.4%) reported overall well-being categorized as struggling at least once. Twenty-one students (27.6%) reported that they were thriving across all 25 weeks analyzed.
Figure 2.
Percent of Doctor of Pharmacy Students Thriving, Struggling, and Suffering Across the First Professional Year (P1) of the Curriculum (N=76)
DISCUSSION
Well-being is a complex, multidimensional construct that is understudied in health professions students, including pharmacy students. To our knowledge, this is the first study to assess pharmacy student well-being in a longitudinal manner. Noteworthy findings from this study include the extent to which well-being varies across the first professional year, the extent to which students reported struggling and suffering, the identification of domains predictive of overall well-being, and the relationships between examination intensity and GPA and well-being. Each of these findings have the potential to inform the efforts of schools and colleges to understand and proactively promote student well-being.
A large majority of the well-being literature captures well-being data (as well as data on burnout, resiliency, grit, and other aspects of well-being) cross sectionally, either at one point in time or using a pre-/post-intervention. In the same manner that only weighing a patient during an annual physical examination may miss significant fluctuations in weight that occur throughout the year, assessing well-being infrequently could lead to overestimating or underestimating the climate of well-being among students. This study revealed significant fluctuations in student well-being, particularly across the first semester of the professional program. This finding aligns with Kulig and Persky’s concern for students’ well-being during times of transition.20 If schools and colleges elect to assess the well-being of their students, the number and timing of assessments should be considered to ensure that evidence-informed peaks and troughs are captured. Of note, informing students about the significant relationship between overall well-being during the fall semester and semester GPA may motivate students to engage in well-being promoting activities during the transition into pharmacy school.
Career, physical, and social well-being were the most frequent predictors of overall well-being in pharmacy students throughout the first professional year. While our results are specific to one cohort of students at one institution, in an environment of limited resources, targeting interventions at these well-being domains may provide the greatest return on investment for schools and colleges. Importantly, interventions should not only be considered from the student perspective, but also from the school’s perspective. In other words, having conversations with students to encourage them to be physically active or to get adequate sleep (both of which could be considered interventions) may produce limited results if the realities of a professional program (eg, heavy course load, examination schedule) keep them from doing so. As Shanafelt and Noseworthy note, interventions targeted at the individual are typically resisted unless a culture exists in which well-being and organization-level efforts have been made to address factors that contribute to decreased well-being.31
Not surprisingly, the number of examinations in a week was significantly negatively associated with students’ career, community, physical, and overall well-being scores. While examinations are inherent components of professional programs, their timing and frequency throughout the academic year may warrant increased attention by pharmacy schools. Students had examination-free weeks for seven out of the 25 weeks studied, which typically occurred at the beginning of each of the two semesters. The concept of job stress recovery is well studied in the occupational health literature, including the relationship between recovery and well-being, and pharmacy educators may be able to apply some of those findings to students in professional programs.32 From a student perspective, recovery periods range from relatively long such as in between semesters (ie, macro recovery), to very short, such as in between classes (ie, micro recovery). Students’ well-being scores in this study were higher when they were assessed after having taken brief breaks (eg, fall break, spring break). Considering again the relationship between examination frequency and well-being in our study, research is warranted to examine the timing of examinations on students’ engagement in evidence-based recovery activities. For example, Monday morning examinations may discourage recovery during the previous weekend. Importantly, students may need to be introduced to the concept and importance of recovery as well as the stress-recovery cycle.33
Nearly 25% of students’ responses indicated they were suffering at one or more times during the semester, while the responses of another 25% indicated that they had not struggled or suffered during the semester. The prevalence of pharmacy student suffering aligned with Gallup’s weekly US data which report that between 1% and 7% of the US population suffered during 2017.28 In the same manner that a failing or low grade on an assessment can alert an administrator, mentor, or advisor to reach out to a student, the feasibility of using weekly well-being assessments to target interventions with students who identify as suffering (or struggling) warrants investigation. Similar monitoring studies have been conducted with other constructs, including mood and sleep.29,30 With student permission and navigation of legal restrictions, technology-based applications could be used to support such tracking. While data specific to pharmacy schools are lacking in the literature, anecdotal reporting of increases in student suicides by member institutions represented at the 2018 AACP Fall Institute warrant mention. Tracking suffering or struggling students could serve as an intervention point that prevents loss of life.
Given the intense nature of pharmacy education and health professions education in general, fostering resilience and minimizing burnout in students are notable goals. In this study, well-being trended downward in most domains or was maintained at best across the P1 year. The idea that students’ well-being could be increased during pharmacy school is counterintuitive to the typical perception that the difficulty of school necessitates that well-being be “back-burnered” for three, four, or more years. Given the evidence-based link between burnout, distress, and other factors downstream including well-being and patient outcomes, equipping students to thrive is not only in their best interest, but also in the best interest of the patients they will serve.
This study has several limitations. First, the study was limited to one relatively small cohort at one institution. Given the number of assessments conducted, expanding the study to include other cohorts (eg, P2 and P3 students) or other institutions was not possible. Therefore, the generalizability of the findings to pharmacy students in other years of the program or pharmacy students at other institutions is unknown. Second, despite familiarizing students with the well-being constructs in a comprehensive manner at the beginning of the semester, students may have misinterpreted the well-being constructs when completing weekly well-being assessments. Similarly, representing each well-being domain and overall well-being with individual items is a limitation. Costs associated with full administration of Gallup’s Wellbeing Finder assessment, as well as the time burden necessary to do so, prohibited the investigators from using a validated assessment in a longitudinal manner.
CONCLUSION
Pharmacy students reported significant variation in domain specific and overall well-being across the first professional year. Career, physical, and social well-being most frequently predicted overall well-being scores. Examination frequency was negatively associated with domain-specific and overall well-being scores. Nearly 25% of students reported suffering at least once. Future research is warranted to advance the Academy’s understanding of pharmacy student well-being.
REFERENCES
- 1.Centers for Disease Control and Prevention. Health-Related Quality of Life (HRQOL). https://www.cdc.gov/hrqol/wellbeing.htm. Published 2018. Accessed June 22, 2020.
- 2.Rath T, Harter J. Wellbeing: The Five Essential Elements. New York, NY: Gallup Press; 2010. [Google Scholar]
- 3.Cantril H. The Pattern of Human Concerns. New Brunswick, NJ: Rutgers University Press; 1965. [Google Scholar]
- 4.Gallup Inc. Understanding how gallup uses the cantril scale: development of the thriving, striuggling, suffering categories. https://news.gallup.com/poll/122453/understanding-gallup-uses-cantril-scale.aspx. Published 2019. Accessed June 22, 2020.
- 5.The Ohio State University. Nine Dimensions of Wellness. https://swc.osu.edu/about-us/nine-dimensions-of-wellness/. Published 2019. Accessed June 22, 2020.
- 6.The Ohio State University. 2019-2024. Wellness Strategic Plan. Columbus, OH2019. [Google Scholar]
- 7.Chida Y, Steptoe A. Positive psychological well-being and mortality: a quantitative review of prospective observational studies. Psychosom Med. 2008;70(7):741-756. [DOI] [PubMed] [Google Scholar]
- 8.Davidson KW, Mostofsky E, Whang W. Don't worry, be happy: positive affect and reduced 10-year incident coronary heart disease: the Canadian Nova Scotia Health Survey. Eur Heart J. 2010;31(9):1065-1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salvagioni DAJ, Melanda FN, Mesas AE, Gonzalez AD, Gabani FL, Andrade SM. Physical, psychological and occupational consequences of job burnout: a systematic review of prospective studies. PLoS One. 2017;12(10):e0185781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shanafelt T, Goh J, Sinsky C. The business case for investing in physician well-being. JAMA Intern Med. 2017;177(12):1826-1832. [DOI] [PubMed] [Google Scholar]
- 11.Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251(6):995-1000. [DOI] [PubMed] [Google Scholar]
- 12.Williams ES, Manwell LB, Konrad TR, Linzer M. The relationship of organizational culture, stress, satisfaction, and burnout with physician-reported error and suboptimal patient care: results from the MEMO study. Health Care Manage Rev. 2007;32(3):203-212. [DOI] [PubMed] [Google Scholar]
- 13.West CP, Tan AD, Habermann TM, Sloan JA, Shanafelt TD. Association of resident fatigue and distress with perceived medical errors. JAMA. 2009;302(12):1294-1300. [DOI] [PubMed] [Google Scholar]
- 14.Shanafelt TD, Balch CM, Dyrbye L, et al. Special report: suicidal ideation among American surgeons. Arch Surg. 2011;146(1):54-62. [DOI] [PubMed] [Google Scholar]
- 15.Han S, Shanafelt TD, Sinsky CA, et al. Estimating the attributable cost of physician burnout in the United States. Ann Intern Med. 2019. [DOI] [PubMed] [Google Scholar]
- 16.National Academy of Medicine. National Academy of Medicine Action Collaborative on Clinician Well-Being and Resilience. National Academy of Medicine; https://nam.edu/initiatives/clinician-resilience-and-well-being/. Published 2019. Accessed June 22, 2020. [Google Scholar]
- 17.Miller ML, Boyer C, Emerson MR, et al. Report of the 2017-2018 Student Affairs Standing Committee. Am J Pharm Educ. 2018;82(7):7159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.American Association of Colleges of Pharmacy. AACP Statement on Commitment to Clinician Well-being and Resilience. https://www.aacp.org/article/commitment-clinician-well-being-and-resilience. Published 2018. Accessed June 22, 2020.
- 19.Accreditation Council for Pharmacy Education. Accreditation Standards and Key Elements for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. In. Chicago, IL: Accreditation Council for Pharmacy Education; 2015. [Google Scholar]
- 20.Kulig CE, Persky AM. Transition and student well-being - why we need to start the conversation. Am J Pharm Educ. 2017;81(6):100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ray ME, Coon JM, Al-Jumaili AA, Fullerton M. Quantitative and qualitative factors associated with social isolation among students from graduate and professional health science program. Am J Pharm Educ. 2019;83(7):6983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bullock G, Kraft L, Amsden K, et al. The prevalence and effect of burnout on graduate health care students. Can Med Educ J. 2017;8(3):e90-e108. [PMC free article] [PubMed] [Google Scholar]
- 23.Dyrbye LN, West CP, Satele D, et al. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014;89(3):443-451. [DOI] [PubMed] [Google Scholar]
- 24.Stoffel JM, Cain J. Review of grit and resilience literature within health professions education. Am J Pharm Educ. 2018;82(2):6150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chisholm-Burns MA, Spivey CA, Jaeger MC, Williams J. Associations between pharmacy students' attitudes toward debt, stress, and student loans. Am J Pharm Educ. 2017;81(7):5918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zeek ML, Savoie MJ, Song M, et al. Sleep duration and academic performance amongsStudent Pharmacists. Am J Pharm Educ. 2015;79(5):63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hirsch JD, Do AH, Hollenbach KA, Manoguerra AS, Adler DS. Students' health-related quality of life across the preclinical pharmacy curriculum. Am J Pharm Educ. 2009;73(8):147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gallup Inc. U.S. Life Evaluation (Weekly). Gallup, Inc; https://news.gallup.com/poll/151157/life-evaluation-weekly.aspx. Published 2019. Accessed June 22, 2020. [Google Scholar]
- 29.Malhi GS, Hamilton A, Morris G, Mannie Z, Das P, Outhred T. The promise of digital mood tracking technologies: are we heading on the right track? Evid Based Ment Health. 2017;20(4):102-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.DeMasi O, Feygin S, Dembo A, Aguilera A, Recht B. Well-being tracking via smartphone-measured activity and sleep: cohort study. JMIR Mhealth Uhealth. 2017;5(10):e137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shanafelt TD, Noseworthy JH. Executive leadership and physician well-being: nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92(1):129-146. [DOI] [PubMed] [Google Scholar]
- 32.Sonnentag S, Venz L, Casper A. Advances in recovery research: what have we learned? what should be done next? J Occup Health Psychol. 2017;22(3):365-380. [DOI] [PubMed] [Google Scholar]
- 33.Johnson & Johnson Human Performance Institute. The Power of Resilience: How Reframing Stress Can Fuel Performance. 2018. [Google Scholar]