Abstract
Objective. To determine how pharmacy students’ perceptions of electronic nicotine delivery systems (ENDS) differ from those of other health care students.
Methods. A 33-item questionnaire was sent to health professional students at a Midwestern university to assess their tobacco use, insights regarding ENDS, cessation education, and perceptions. Health professions included were pharmacy, nursing, public health, optometry, dental hygiene, and others.
Results. The overall response rate to the questionnaire was 41% (1152/2799). The study population reported high ENDS use. Almost half (47%) of the respondents had ever used ENDS and 14% were current users (6% pharmacy students vs 19% other health care students). A lower percentage of pharmacy students than other health care students agreed that using ENDS is healthier than using tobacco (18% vs 26%). Overall, pharmacy students more strongly agreed that they had received enough education to counsel patients regarding tobacco cessation (rated 4.7 by pharmacy students vs 3.6 by other health care students on a seven-point Likert scale) and ENDS cessation (rated 3.3 by pharmacy students vs 2.9 by other health care students). Finally, pharmacy students were less likely than other health care students to recommend the use of ENDS to aid patients in quitting traditional cigarette use (2.9 vs 3.2, respectively).
Conclusion. The rapid rise in use of ENDS and the continued use of cigarettes in the United States makes it imperative for health care professionals to be knowledgeable about these products and prepared to counsel patients regarding them. We found that pharmacy students tended to have more negative perceptions about ENDS and a lower percentage of pharmacy students than other health care students agreed that ENDS should be used as a cessation tool for quitting traditional cigarettes.
Keywords: electronic cigarettes, cessation, health care students, pharmacy students, electronic nicotine-delivery systems
INTRODUCTION
Electronic cigarettes, also known as electronic nicotine delivery systems (ENDS), encompass a wide array of non-combustible inhaled aerosols that may or may not contain nicotine. “Vaping” and “juuling” are terms that have become synonymous with the use of ENDS, and popularity among youth and young adults has surged in the last decade.1 Based on safety concerns, the Food and Drug Administration (FDA) extended its authority to regulate tobacco products to include ENDS starting in 2016.2
A rapid rise in the use of ENDS and little evidence regarding the long-term effects of their use has left health care providers largely unprepared to address the topic of ENDS with their patients. A study from the Centers for Disease Control and Prevention (CDC) found that among cigarette smokers attempting to quit, a greater number used ENDS rather than an FDA-approved medication during their most recent attempt.3 In contrast, a 2017 study of family physicians found that 82% did not recommend ENDS as a cessation tool for their patients, citing a lack of efficacy and safety data.4
According to a 2016 study regarding the prevalence of ENDS use in the United States, young adults between 18 and 24 years of age were the highest user group, with 9.2% of this population using ENDS compared to 4.5% overall.5 As this demographic aligns with college-age students, perceptions within this group about ENDS may be especially telling of future interactions with patients. Franks and colleagues found that 44% of health professions students agreed that using ENDS is less harmful than smoking traditional cigarettes; however, 25% agreed that ENDS were a reasonable choice of a cessation tool for patients.6 Although this study provided insight into perceptions of health professions students overall, little is known about Doctor of Pharmacy (PharmD) students specifically. As pharmacists are becoming increasingly involved in primary care, public health, and nicotine cessation efforts, how pharmacy students perceive the safety and efficacy of ENDS is an important area to explore. The primary objective of this study was to determine how pharmacy students’ perceptions of ENDS differ from that of other health care students.
METHODS
A cross-sectional questionnaire regarding ENDS was created by faculty members at the College of Pharmacy at Ferris State University based on a review of current ENDS publications, tobacco publications, the CDC’s National Youth Tobacco Survey, and related news releases.1,4,6,8-10 Additional insight was gathered by visiting local vape shops and presenting a draft survey at a research roundtable for feedback.
To further improve validity, the authors asked four current fourth-year PharmD students to pilot the questionnaire and review it for readability. Students also provided input on missing or redundant answer choices and suggested how the wording of questions could be clarified.
To assess reliability, 17 students piloted the online questionnaire twice, about one week apart. Responses were evaluated using Spearman rank correlation coefficients and Cronbach alpha. A statistician reviewed the validity results and then the authors made final revisions to the questionnaire. The study was approved by the Ferris State University institutional review board.
Health professions students enrolled in programs in pharmacy, optometry, nursing, social work, dental hygiene, respiratory care, public health, allied health sciences, nuclear medicine technology, medical laboratory science, health information management, molecular diagnostics, diagnostic medical sonography, medical laboratory technology, radiography, health information technology, and certificate programs for cancer information management, vascular ultrasound, and long-term care were included in the survey population. Excluded individuals were minors (<18 years of age), non-English speakers, prisoners or anyone that did not know what ENDS were. Inclusion and exclusion criteria was listed in the recruitment email, and individuals not meeting study criteria were exited from the questionnaire and responses were thrown out. In September 2018, the finalized 33-item questionnaire was sent from an online platform (www.questionpro.com, QuestionPro, Austin, TX) to all health care students who had a university email account.7 The email contained a link to the questionnaire and stated its purpose to determine students’ perceptions regarding electronic cigarettes and tobacco products.8,9 All responses were collected anonymously through QuestionPro. Participants had the option at the end of the questionnaire to enter a drawing for one of eight $25 gift cards. The questionnaire was open for four weeks, during which time students received a reminder email at one and two weeks.
The first section of the questionnaire asked basic demographic questions. The questionnaire was constructed using conditional logic to learn about students’ personal use of various tobacco forms. Definitions similar to those used in a national tobacco survey were included in the questionnaire.10 Current use of all tobacco forms and ENDS was categorized by asking if they now use each product every day or only on some days.
Students’ perceptions of ENDS were assessed using a seven-point Likert scale. Additional questions asked students about the perceived risks and benefits of ENDS. The final set of questions focused on participants’ education, likelihood of counseling on cessation of traditional cigarette use and use of ENDS, and past counseling on cessation of traditional cigarette use and use of ENDS.
Frequencies and descriptive statistics were used to describe demographic data, tobacco use, and perceptions. Questionnaire responses were compared between pharmacy students and students of other health profession majors. Chi-square tests were used for categorical variables (eg, demographics) and Mann-Whitney and Kruskal-Wallis tests were used for ordinal variables (eg, Likert scale questions). A p value of <.05 was considered statistically significant. All statistical analyses were performed using Stata, version 13 (StataCorp LLC, College Station, TX).
RESULTS
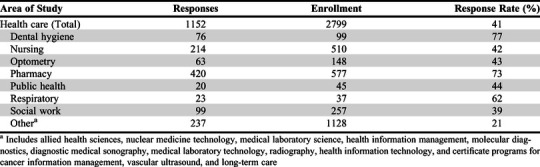
A total of 1152 health care students participated in the study, of which 420 were pharmacy students. The overall response rate to the questionnaire was 41% (Table 1). The mean age of both pharmacy students and other health care students was 24 years and thus not statistically different. The proportion of nonwhite students was not significantly different between the two groups (12% of pharmacy vs 13% of other health care). A significantly lower proportion of pharmacy students were female compared to other health care students (59% vs 88% respectively, p<.001). Pharmacy students were less likely to have a history of smoking traditional cigarettes compared to other health care students (10% vs 16%, respectively, p<.05) as well as a history of ENDS use (6% of pharmacy vs 19% of other health care, p<.001). Of the students with a history of ENDS use, pharmacy students were less likely to be current ENDS users compared to other health care students (14% vs 37%, respectively, p<.001).
Table 1.
Questionnaire Response Rates of Health Professions Students Who Participated in a Study to Assess Their Knowledge and Perceptions of Electronic Nicotine Delivery Systems
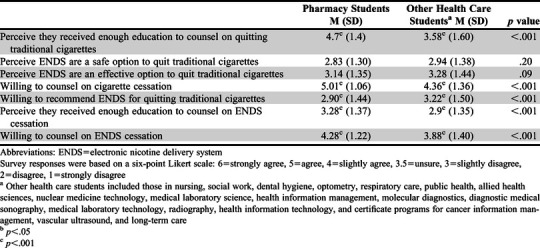
Significant differences were found in pharmacy students’ perceptions of the harms and benefits of ENDS compared to other health care students’ perceptions (Table 2). Table 3 compares pharmacy students’ and other health care students’ perceptions related to education of traditional cigarettes and ENDS. Pharmacy students were significantly more likely than other health care students to agree that they had received enough education to counsel someone about quitting traditional cigarettes. Pharmacy students were also more likely to agree they received enough education to counsel patients on quitting ENDS. While there were not significant differences in the level of agreement regarding ENDS as a safe or effective option to quit traditional cigarettes, other health care students were significantly more willing to recommend ENDS for quitting traditional cigarettes than pharmacy students. Finally, a significantly higher proportion of pharmacy students than other health care students indicated having experience in counseling patients about tobacco cessation (47% vs 38%, respectively; p=.005). However, only a relatively small proportion of students in each group indicated having experience with counseling patients regarding cessation of ENDS use (10% vs 13%, respectively; p=.137)
Table 2.
Health Professions Students’ Perceptions of the Harm and Benefits from the Use of Electronic Nicotine Delivery Systems
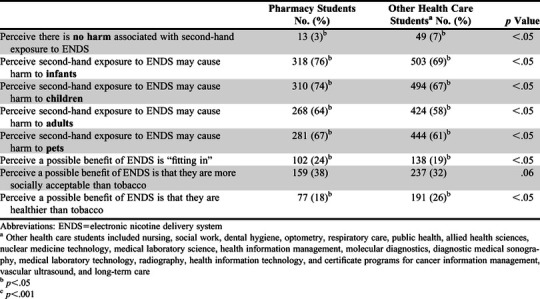
Table 3.
Health Professions Students’ Perceptions of Their Level of Agreement Regarding Cessation Education and ENDS Utility
DISCUSSION
In this study, we found that a history of ENDS use was high among health care students. As compared to a similar study, mean ENDS use in our study occurred at twice the previously reported rate in health care professional students (24% vs 48%, respectively).6 While this trend is not surprising considering the national prevalence of ENDS use in the United States has steadily increased over the last decade, it is very concerning as it may indicate greater acceptance of ENDS among health professionals.11
With regard to the safety of ENDS, pharmacy students had a more negative perception of these devices compared to other health care students. This finding may be related to a lower rate of overall ENDS use among pharmacy students. Pharmacy students were also more likely to correctly identify known risks of ENDS use. Pharmacy students were significantly less likely than other health care students to agree that ENDS are healthier than other forms of tobacco delivery (18% vs 26%, respectively), and these percentages are much lower than previously reported.6 The release of the 2016 Surgeon General’s report: E-cigarette use among youth and young adults which more clearly described the harms caused by ENDS, may have been a contributing factor to health professions students’ more negative perceptions.12
The students surveyed in this study were not confident they had received adequate education to counsel patients regarding methods to quit use of ENDS, but they were confident on counseling patients about the use of traditional cigarettes. This is a gap that has been discussed in previous health professions literature.6,13-15 The responses from this questionnaire support findings in medical education that health care students are lacking in knowledge about ENDS and comfort with counseling patients about ENDS use and that a curricular change is needed to bring additional focus to this emerging topic.13-15 Within this school’s pharmacy curriculum, ENDS are covered briefly during nicotine dependence lectures in the self-care course and integrated pharmacotherapy module; however, there are minimal studies published on helping patients who desire to quit using ENDS.16-19 Despite limited education and evidence, pharmacy students were more willing than other health professions students to counsel patients about stopping the use of ENDS. As we continue to see rises in ENDS use, pharmacists have the opportunity to be a source of truth and guidance to both patients and other health care providers. However, that is only possible if pharmacy curricula provide students with the knowledge, education, and skills to discuss literature on ENDS and to promote ENDS cessation.
Perhaps the most telling finding from this survey was the responses to the question about agreement with recommending ENDS as an option for quitting traditional cigarette smoking, as this is a question frequently encountered in clinical practice. Although pharmacy students were significantly less likely to agree that ENDS should be used as a cessation tool, the mean rating was still within the “slightly disagree” to “disagree” category for both groups, indicating that neither group felt comfortable with recommending ENDS as a cessation tool. Whether ENDS are appropriate to use as a cessation tool has been a topic of debate over the last several years primarily because of the lack of high quality literature on the topic and limited long-term safety data.20,21 The possible role of ENDS as a cessation tool remains largely unclear at this time, so it was not surprising that all health professions students were unsure or disagreed with this statement.
The limitations of this study primarily relate to including only a single university. The university does not have a degree program for physicians, physician assistants, or clinical nurse practitioners. As the majority of students who were surveyed were white the applicability of our findings to more diverse populations is difficult. Although response rates were relatively high, especially among pharmacy students, the distribution was not equal across all professions. Finally, an imbalance of current ENDS use between pharmacy students and other health care students may have impacted knowledge and perceptions as well.
CONCLUSION
The results of this study provide insight into health professional students’ perceptions about use of tobacco and ENDS. There were clear differences between pharmacy students’ and other health care students’ perceptions of ENDS, with pharmacy students having more negative views about these products. However, there continues to be a major gap in ENDS knowledge and education in health care curricula of US universities, which needs to be addressed given the ever-changing landscape of ENDS. An interprofessional approach to health care education that covers the safety and utility of ENDS may offer the most practical solution to address such a nuanced topic. Additional assessment is needed regarding how to deliver ENDS education, and its impact on health care students’ knowledge and perception of ENDS.
REFERENCES
- 1.Wang TW, Gentzke A, Sharapova S, et al. Tobacco product use among middle and high school students-United States, 2011-2017. MMWR Morb Mortal Wkly Rep. 2018;67:629-633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Food and Drug Administration, HHS. Deeming tobacco products to be subject to the Federal Food, Drug, and Cosmetic Act, as amended by the Family Smoking Prevention and Tobacco Control Act; restrictions on the sale and distribution of tobacco products and required warning statements for tobacco products. Final rule. Fed Reg. 2016;81:28973-29106. [PubMed] [Google Scholar]
- 3.Caraballo RS, Shafer PR, Patel D, Davis KC, McAfee TA. Quit methods used by US adult cigarette smokers, 2014-2016. Prev Chronic Dis. 2017;14:160600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ofei-Dodoo S, Kellerman R, Nilsen K, et al. Family physicians’ perceptions of electronic cigarettes in tobacco use counseling. J Am Board Fam Med. 2017;30:448-459. [DOI] [PubMed] [Google Scholar]
- 5.Mirbolouk M, Charkhchi P, Kianoush S, et al. Prevalence and distribution of e-cigarette use among U.S. adults: Behavioral Risk Factor Surveillance System, 2016. Ann Intern Med.2018;169:429-438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Franks AM, Hawes WA, McCain KR, Payakachat N. Electronic cigarette use, knowledge, and perceptions among health students. Curr Pharm Teach Learn. 2017;9:1003-1009. [DOI] [PubMed] [Google Scholar]
- 7. Free online survey software & tools. QuestionPro. https://www.questionpro.com.
- 8.Weaver SR, Kim H, Glasser AM, et al. Establishing consensus on survey measures for electronic nicotine and non-nicotine delivery system use: current challenges and considerations for researchers. Addict Behav. 2018;79:203-212. doi: 10.1016/j.addbeh.2017.11.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gibson LA, Creamer MR, Breland AB, et al. Measuring perceptions related to e-cigarettes: Important principles and next steps to enhance study validity. Addict Behav. 2018;79:219-225. doi: 10.1016/j.addbeh.2017.11.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Health CO on S and Smoking and Tobacco Use; Data and Statistics; Surveys; National Youth Tobacco Survey (NYTS). Smoking and Tobacco Use. http://www.cdc.gov/tobacco/data_statistics/surveys/nyts/. Published December 23, 2019.
- 11.Cullen KA, Ambrose BK, Gentzke AS, Apelberg BJ, Jamal A, King BA. Notes from the field: use of electronic cigarettes and any tobacco product among middle and high school students-United States, 2011-2018. MMWR Morb Mortal Wkly Rep. 2018;67:1276-1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. 2016. Surgeon General’s report: e-cigarette use among youth and young adults. https://www.cdc.gov/tobacco/data_statistics/sgr/e-cigarettes/index.htm Accessed June 30, 2020.
- 13.Hinderaker K, Power DV, Allen S, Parker E, Okuyemi K. What do medical students know about e-cigarettes? a cross-sectional survey from one U.S. medical school. BMC Medical Education. 2018;18(1):32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhou S, Van Devanter N, Fenstermaker M, Cawkwell P, Sherman S, Weitzman M. A study of the use, knowledge, and beliefs about cigarettes and alternative tobacco products among students at one U.S. medical school. Acad Med. 2015;90(12):1713-1719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Erku DA, Gartner CE, Morphett K, Steadman KJ. Beliefs and self-reported practices of health care professionals regarding electronic nicotine delivery systems (ENDS): a mixed-methods systematic review and synthesis. Nicotine Tob Res. 2019; Apr 2. pii: ntz046. doi: 10.1093/ntr/ntz046 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 16.Silver B, Ripley-Moffitt C, Greyber J, Goldstein AO. Successful use of nicotine replacement therapy to quit e-cigarettes: lack of treatment protocol highlights need for guidelines. Clin Case Rep. 2016;4(4):409-411. doi: 10.1002/ccr3.477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sahr M, Kelsh SE, Blower N. Pharmacist assisted vape taper and behavioral support for cessation of electronic nicotine delivery system use. Clin Case Rep. 2019;8(1):100-103. doi: 10.1002/ccr3.2599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barkat SS, Tellier SM, Eloma AS. Varenicline for cessation from nicotine-containing electronic cigarettes. American Journal of Health-System Pharmacy. 2019;76(23):1894-1895. doi: 10.1093/ajhp/zxz218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Graham AL, Jacobs MA, Amato MS. Engagement and 3-month outcomes from a digital e-cigarette cessation program in a cohort of 27000 teens and young adults. Nicotine & Tobacco Research. 2020;22(5):859-860. doi: 10.1093/ntr/ntz097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McRobbie H, Bullen C, Hartmann-Boyce J, Hajek P. Electronic cigarettes for smoking cessation and reduction. Cochrane Database Syst Rev. 2014;(12):CD010216. [DOI] [PubMed] [Google Scholar]
- 21.Hajek P, Phillips-Waller A, Przulj D, et al. A randomized trial of e-cigarettes versus nicotine replacement therapy. N Engl J Med. 2019;380:629-637. [DOI] [PubMed] [Google Scholar]


