1. INTRODUCTION
The rapid global spread of coronavirus disease 2019 (COVID‐19) is now well‐known with the first case in South Africa on 5 March 2020, 1 and since then, the country has been experiencing a persistent increase in the number of positive cases. By 24 May 2020, there were 99 433 confirmed cases in Africa where the tuberculosis (TB) incidence is 231/100 000. 2 , 3 There is uncertainty of the impact of possible dual epidemics of TB and COVID‐19 and whether tuberculous lung disease would be a risk factor for severe COVID‐19. We describe the first recorded case of COVID‐19 coinfection in a young child with airway compression due to Mycobacterium tuberculosis (MTB).
2. CASE PRESENTATION
A 2‐year 5‐month‐old human immunodeficiency virus (HIV)‐negative boy presented to his local hospital with fever, coughing, worsening respiratory distress, and loss of appetite 1 month after being diagnosed with pulmonary tuberculosis (PTB) with a positive GeneXpert MTB/RIF, Rifampicin sensitive, on gastric aspirate. The chest radiograph at diagnosis demonstrated subcarinal lymph nodes and mild narrowing of the left main bronchus. He was started on a 4‐drug, weight‐appropriate, TB regimen at diagnosis. He did not receive prednisone at the time as the airway obstruction was deemed not to be clinically significant. There was no close contact with an adult TB source case at the time of the original or the current diagnosis. The mother was screened but was negative. He had no travel history, and at the time of presentation, we were not aware of contact with a confirmed COVID‐19 case. He did not receive the Bacillus Calmette‐Guérin (BCG) vaccine at birth due to local shortage at the time.
On clinical examination, the saturations were 100% on nasal prong oxygen and respiratory rate was 30 breaths per minute. He had a blocked nose, subcostal recession, and dullness to percussion in the right upper lobe. On auscultation, wheezing was detected, more significant on the right. He was hemodynamically stable. A supine frontal chest radiograph demonstrated confluent air‐space disease in the right upper and middle lobes with a small focus of breakdown corresponding to the dullness on percussion elicited clinically. Airway narrowing of the left main bronchus and the bronchus intermedius are surrogate representations of hilar and mediastinal lymphadenopathy, which in conjunction with the air‐space disease, support a diagnosis of primary PTB. A lateral chest radiograph performed during the same admission confirmed the area of parenchymal breakdown (presumably in the right middle lobe) and also confirmed the presence of lymphadenopathy posteroinferiorly to the bronchus intermedius (for both frontal and lateral views, see Figure 1). He had a white cell count of 8.03 × 109/L, neutrophils 3.56 × 109/L, lymphocytes 3.45 × 109/L, and C‐reactive protein of 11 mg/L.
Figure 1.
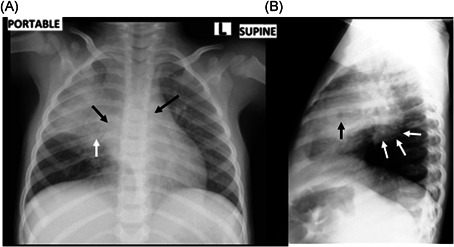
A, A supine frontal chest radiograph was performed as a portable examination. There is confluent air‐space disease in the right upper and middle lobes with a small focus of breakdown (white arrow) and airway narrowing at the left main bronchus and the bronchus intermedius (black arrows), which represent surrogate markers of hilar and mediastinal lymphadenopathy. In conjunction with the air‐space disease, the parenchymal breakdown and airway narrowing support a diagnosis of primary pulmonary tuberculosis, which was confirmed using Gene Xpert on a gastric washing sample. B, Lateral radiograph confirms the area of parenchymal breakdown (black arrow), presumably in the right middle lobe, and also confirms the lymphadenopathy (white arrows) posteroinferiorly to the bronchus intermedius
Due to his symptoms of new‐onset fever and coughing, he was tested by polymerase chain reaction (PCR) for COVID‐19. This was positive, within 24 hours, for both the child and his asymptomatic mother. They classified as cases of local spread of COVID‐19. Nasal prong oxygen and oral co‐amoxiclav were commenced. The 4‐drug antituberculous treatment regimen, including rifampicin, isoniazid, pyrazinamide, and ethambutol, was continued and adjuvant oral prednisone 2 mg/kg was added before the diagnosis of COVID‐19, interrupted at COVID‐19 diagnosis, and restarted again at discharge. Improvement was rapid with discharge on day 5, followed by self‐isolation. He received two doses of oral prednisone before the diagnosis of COVID‐19. The airway obstruction will be re‐evaluated 4 weeks postdischarge. Consent was given by the patient's parents for publication of this case and permission for the report was granted by the Institutional Review Board of the Health Science Faculty of Stellenbosch University.
3. DISCUSSION
Coinfection with other pathogens has been described in up to 40% of children with COVID‐19, including influenza A and B, mycoplasma, respiratory syncytial virus, and cytomegalovirus. 4 This is the first report of coinfection with MTB. Airway obstruction due to MTB is known to be complicated by a viral infection, causing additional inflammation, thereby worsening the obstruction. 5
BCG vaccination confers decreased risk of severe childhood TB disease in high‐burden areas, an effect negated by low vaccine coverage. 6 Besides protection against TB, BCG vaccination also modulates the immune response to subsequent infections caused by other pathogens, including viruses, by the induction of innate immunity and heterologous lymphocyte activation. 7 , 8 In this case, the question raised is whether lack of BCG vaccination increased susceptibility to severe pulmonary TB, COVID‐19, and possibly other viral coinfection. The protective effects of BCG vaccination against severity and poor outcome in COVID‐19 infection is currently a subject of clinical trials. 9
This case highlights the difficulty that diagnosis and management of COVID‐19 presents to clinicians in resource‐constrained countries with high TB and HIV burden. This child, known with PTB, presented with clinical symptoms that could have been presumed to be related due to either TB or COVID‐19. Routine management of children with significant airway obstruction is also compromised due to the risk bronchoscopy may hold. The nonspecific clinical and radiological findings of COVID‐19 in children complicate recognition. Computed tomography (CT) findings are thought to be more specific, 4 but in TB endemic countries, CT scans are not easily available. In patients with complicated PTB, with extensive parenchymal involvement, it would be impossible to differentiate from COVID‐19, based on symptoms and chest radiograph findings alone. Bronchoscopy has been used to confirm and determine the severity of tuberculous airway obstruction in children, guiding the decision either to treat medically with antituberculous drugs and oral prednisone or intervene surgically. 10 As bronchoscopy is a very high‐risk aerosol‐generating medical procedure, in TB endemic areas, this has to be performed with strict indications and with full personal protective equipment (PPE). 11 The indications for bronchoscopy in pediatric TB may need to be revised as full PPE, although optimal, is not always available in a resource‐constrained world and may be limited to only N95 masks.
Currently, it would be very difficult to predict whether PTB in children confers additional risk of developing severe COVID‐19. This case illustrates that children with confirmed PTB may have persistent or worsening symptoms due to other viral infections, including COVID‐19 infection, and may present with new pneumonia and exacerbation of TB‐associated nodal airway obstruction. However, the rapid improvement is reassuring. The child experienced short‐term deterioration of his airway obstruction due to COVID‐19, which subsequently rapidly improved. Oral prednisone at 2 mg/kg for TB airway obstruction was continued for 1 month even after recovery from COVID‐19.
4. CONCLUSION
COVID‐19 may result in deterioration in children with TB. More data on the effect of COVID‐19 on presentation and treatment response in children with TB (including the full spectrum) is needed. The effect of corticosteroid and possible impact of BCG vaccination in these children also requires better description.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
ACKNOWLEDGMENT
The authors wish to acknowledge Dr Janette Verster with her help in reviewing this manuscript.
Goussard P, Solomons R, Andronikou S, Mfingwana L, Verhagen L, Rabie H. COVID‐19 in a child with tuberculous airway compression. Pediatric Pulmonology. 2020;55:2201–2203. 10.1002/ppul.24927
REFERENCES
- 1. National Institute of Communicable Diseases . https://www.nicd.ac.za/first-case-of-covid-19-coronavirus-reported-in-sa. Accessed 5 March 2020.
- 2. World Health Organization Regional Office for Africa . https://www.afro.who.int/health-topics/coronavirus-covid-19. Accessed 24 May 2020.
- 3. World Health Organization. Global Tuberculosis Report . WHO Report 2018, Geneva, Switzerland.
- 4. Xia W, Shao J, Guo Y, Peng X, Li Z, Hu D. Clinical and CT features in pediatric patients with COVID‐19 infection: different points from adults. Pediatr Pulmonol. 2020;55:1169‐1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Goussard P, Gie RP. Airway involvement in pulmonary tuberculosis. Paediatr Respir Rev. 2007;8:118‐123. [DOI] [PubMed] [Google Scholar]
- 6. du Preez K, Seddon JA, Schaaf HS, et al. Global shortages of BCG vaccine and tuberculous meningitis in children. Lancet Glob Health. 2019;7:e28‐e29. [DOI] [PubMed] [Google Scholar]
- 7. Moorlag S, Arts RJW, van Crevel R, Netea MG. Non‐specific effects of BCG vaccine on viral infections. Clin Microbiol Infect. 2019;25:1473‐1478. [DOI] [PubMed] [Google Scholar]
- 8. Schaaf HS, du Preez K, Kruger M, et al. Bacille Calmette‐Guérin (BCG) vaccine and the COVID‐19 pandemic : responsible stewardship is needed. The Union. 2020;1–6. 10.5588/ijtld.20.0267 [DOI] [PubMed] [Google Scholar]
- 9. World Health Organization . Bacille Calmette‐Guérin (BCG) vaccination and COVID‐19: scientific brief, 12 April 2020.
- 10. Goussard P, Gie R. The role of bronchoscopy in the diagnosis and management of pediatric pulmonary tuberculosis. Expert Rev Respir Med. 2014;8:101‐109. [DOI] [PubMed] [Google Scholar]
- 11. Wahidi MM, Lamb C, Murgu S, et al. American Association for Bronchology and Interventional Pulmonology (AABIP) statement on the use of bronchoscopy and respiratory specimen collection in patients with suspected or confirmed COVID‐19 infection [published online ahead of print March 18, 2020]. J Bronchol Interv Pulmonol. 10.1097/LBR.0000000000000681 [DOI] [PMC free article] [PubMed] [Google Scholar]


