Abstract
Many countries have been affected by the worldwide outbreak of COVID‐19. Among Western countries, Italy has been particularly hit at the beginning of the pandemic, immediately after China. In Italy and elsewhere, women seem to be less affected than men by severe/fatal COVID‐19 infection, regardless of their age. Although women and men are affected differently by this infection, very few studies consider different therapeutic approaches for the two sexes. Understanding the mechanisms underlying these differences may help to find appropriate and sex specific therapies. Here, we consider that other mechanisms are involved to explain this difference, in addition to the protection attributable to oestrogens. Several X‐linked genes (such as ACE2) and Y‐linked genes (SRY and SOX9) may explain sex differences. Cardiovascular comorbidities are among the major enhancers of virus lethality. In addition, the number of sex‐independent, non‐genetic factors that can change susceptibility and mortality is enormous, and many other factors should be considered, including gender and cultural habits in different countries.
Keywords: cardiovascular comorbidities, coronavirus, ACE, ACE2, androgens, oestrogens
Abbreviations
- Ang II
angiotensin II
- CAR‐T
chimeric antigen receptor T‐cells
- COVID‐19
coronavirus disease 2019
- CRS
cytokine release syndrome
- CVD
cardiovascular disease
- DEGs
differentially expressed genes
- HF
heart failure
- ICUs
intensive care units
- IKK
IκB kinase
- MEK
MAPK kinase
- mTOR
mammalian target of rapamycin
- RAS
renin angiotensin system
- TMPRSS2
transmembrane protease, serine 2
1. INTRODUCTION
The outbreak of novel coronavirus disease 2019 (COVID‐19) is likely to have started in China (Zhou, Yang, et al., 2020) and rapidly turned into a global pandemic with Europe, the United States, and South America being particularly affected (https://coronavirus.jhu.edu/map.html, accessed on June 28, 2020). Sex differences are emerging in terms of case fatality (deaths/reported cases), and sex disaggregated data are now starting to be available for many countries. Looking at male/female ratio for death in confirmed cases, it appears that the ratio is always above 1.1 in 34 out of the 35 countries that provide sex disaggregated data (only for Pakistan, the ratio is 0.9). Many European countries (Spain, Italy, England, Belgium, Greece, Denmark, and The Netherlands) have a male/female ratio for death in confirmed cases equal or above 1.7 (https://globalhealth5050.org/covid19/, accessed on May 13, 2020). In particular, on May 11, 28,903 COVID‐19 positive patients had died in Italy (Table 1). Their mean age was 80 years (median, 81; range, 0–100; IQR, 74–87; https://www.iss.it/coronavirus, accessed on May 13, 2020). Deaths in women were 10,934 (lethality 9.6%), whereas for men there were 17,018 deatha (lethality 17.1%). For 951 Italian deaths, sex was not reported. At the moment of the revision of this article, this trend is confirmed in the majority of countries which provide disaggregated data (https://globalhealth5050.org/covid19/sex-disaggregated-data-tracker/, accessed on June 28, 2020). In 47 countries, the male/female ratio for death results above 1, and in four countries (Albania, Costa Rica, Thailand, and The Netherlands), this ratio is even above 2. Only in five countries (Finland, Maldives, Pakistan, Slovenia, and Yemen), the male/female ratio for death is below 1, ranging from 0.94 to 0.55 (https://globalhealth5050.org/covid19/sex-disaggregated-data-tracker/, accessed on June 28, 2020). In the vast majority of countries, the mortality rate among confirmed cases is lower in women than in men. The difference in lethality between sexes may suggest that women are either less prone to develop severe complications or that they are less likely to succumb to the severe complications that ultimately lead to death. The reasons for this sex‐based tolerance are still unknown. Among Italian patients in the age range 10–49 years, only 84 out of 32,345 women died (0.26% lethality), while in the range age of 50–90 years, they were 7975/67,263 (11.9% lethality). Of note, 0.89% of men died (225 deaths over 25,276 cases) in the range 10–49 years, and 21.8% (15,236/69844) in the range 50–90 years. Therefore, lethality seems to increase with age in both sexes, but it is 3.42‐fold higher in young men than in young women (10–49 years) and 1.84‐fold in older men than in older women (50–90 years; https://www.iss.it/coronavirus, accessed on May 13, 2020). This trend in Italian patients is confirmed in data disaggregated by age and sex (https://globalhealth5050.org/covid19/age‐and‐sex‐data/#1589893973981‐6ca5e520‐eb20, accessed on June 28, 2020).
TABLE 1.
Cases and fatality of severe Covid 19 in men and women in Italy and China
| Number of patients/Covid+ patients | ICU/severe cases | Deceased | Median age of severe/deceased patients | References | |
|---|---|---|---|---|---|
| Total Covid+ | 131,751 | ‐ | 14,860 | 80 | https://www.iss.it/coronavirus |
| Men | 69,960 (53.1%) | ‐ | 10,062 (67.7%) | 78 | |
| Women | 61,791 (46.9%) | ‐ | 4,798 (32.3%) | 82 | |
| Total of patients | 1,096 | 173 | ‐ | 52 | Guan et al. (2020) |
| Men | 637(58.1%) | 100 (57.8%) | ‐ | ‐ | |
| Women | 459 (41.9%) | 73 (42.2%) | ‐ | ‐ | |
| Total of patients | 191 | ‐ | 54 | 69 | Zhou, Yu, et al. (2020) |
| Men | 119 (62%) | ‐ | 38 (70%) | ‐ | |
| Women | 72 (38%) | ‐ | 16 (30%) | ‐ | |
| Total of patients | 99 | 23 (23%) | 11 (11%) | 55.5 | Chen, Zhou, et al. (2020) |
| Men | 67 (68%) | ‐ | ‐ | ‐ | |
| Women | 32 (32%) | ‐ | ‐ | ‐ | |
| Total of patients | 138 | 36 | 6 (4.3%) | 56 | Wang et al. (2020) |
| Men | 75 (54%) | 22 (64.1%) | ‐ | ‐ | |
| Women | 63 (45.7%) | 14 (38.9%) | ‐ | ‐ | |
| Total of patients | 41 | 13 | 6 (15%) | 49 | Huang et al. (2020) |
| Men | 30 (73%) | 11 (85%) | ‐ | ‐ | |
| Women | 11 (27%) | 2 (15%) | ‐ | ‐ | |
| Total of patients | 274 | 113 | 68 | Chen, Wu, et al. (2020) | |
| Men | 171 (62%) | 83 (73%) | |||
| Women | 103 (38%) | 30 (27%) |
Although these are cumulative/raw data, they confirm that there is a reduced susceptibility of women to severe outcomes from COVID‐19 infection. Due to the differences between pre‐ and post‐menopausal phases (Horstman, Dillon, Urban, & Sheffield‐Moore, 2012), it is reasonable to speculate that there may be a role played by sex hormones in protecting against severe outcome, but it is not the only factor. Therefore, we need to consider other possible reasons for this difference in sex‐related lethality. First, is this difference confirmed also in populations from other countries? According to the latest publications, such differences in lethality between the two sexes have been shown elsewhere (see Table 1 and https://globalhealth5050.org/covid19/). For instance, in a number of different articles from China, similar data are reported (Chen, Zhou, et al., 2020, Chen, Wu, et al., 2020; Guan et al., 2020; Huang et al., 2020; Wang et al., 2020; Zhou, Yu, et al., 2020). In these studies, severe or deceased patients admitted to intensive care units (ICUs) were predominantly men, while women ranged between 30% (Huang et al., 2020) and 42.2% (Guan et al., 2020). In the largest study available from China (Guan et al., 2020), quite similar percentages to those reported for deceased women in Italy have been observed. Yet, in this latter study, the median age of patients was 47 years (IQR, 35–58), and the distribution between sexes according to age was not reported. For the United States, sex disaggregated data on case fatality are not available, but deaths were 57% for males and 43% for women (https://globalhealth5050.org/covid19/, accessed on May 13, 2020).
To sum up, currently available studies suggest that both young and older women are less susceptible to severe infection outcomes, regardless of their nationality. Both hospitalizations in ICUs and death rates are different between sexes (https://globalhealth5050.org/covid19/ and Table 1). Similar observations were already reported for other coronavirus epidemics (Alghamdi et al., 2014; Karlberg, Chong, & Lai, 2004; Leong et al., 2006).
Despite this striking evidence for this infection, very few studies consider different therapeutic approaches for the two sexes. As no specific antiviral drugs are yet proposed to treat COVID‐19 and control disease evolution, a better understanding of the pathogenic mechanisms in the two sexes induced by SARS‐CoV‐2 is mandatory to characterize new targets.
2. WHY ARE FEWER WOMEN THAN MEN DYING OF COVID‐19?
Fewer women, both young and old, are dying than age‐matched males. Beside hormone differences, which, however, do not appear to be the only factor, there are different potential mechanisms that may explain why women are less prone to severe COVID‐19 infections.
First of all, the expression and activity of two important factors may be considered, namely, ACE2 and the transmembrane protease, serine 2 (TMPRSS2; Cheng et al., 2015; Kuba et al., 2005). While ACE2 is the receptor for the spike (S) protein of coronaviruses, TMPRSS2 splits the S‐protein at sites S1/S2 and S2, favouring the attachment and fusion of the virus to cell membranes, respectively. ACE2 is largely expressed in organs mainly targeted and damaged by SARS‐CoV‐2 (Pagliaro & Penna, 2005). Both ACE2 and TMPRSS2 have been proposed as modulators of the different susceptibility to SARS‐CoV in both sexes (Hoffmann et al., 2020).
2.1. Is there a role for ACE/ACE2 ratio in sex difference in COVID‐19?
ACE2 is located on the X chromosome and is one of the genes escaping X inactivation (Tukiainen et al., 2017). Therefore, it is likely that this plays an important role in determining protection in women. It can be hypothesized that the second X chromosome could protect females from fatal polymorphisms that make the COVID‐19 more aggressive in males, for example, by favouring coronavirus binding. Indeed, in a recent study, worse outcome in older COVID‐19 patients has been attributed to the presence of lower ACE‐2 levels and the subsequent up‐regulation of angiotensin II (Ang II) proinflammatory pathways throughout the body, which could make patients more prone to systemic “deleterious” effects of Ang II (AlGhatrif, Cingolani, & Lakatta, 2020). ACE and ACE2 and their major products, Ang II and Ang‐1‐7, respectively, are linked in almost a ying/yang process, when one decreases the other increases and vice versa (Koni & Miyamori, 2007; Pagliaro & Penna, 2005; Wang et al., 2015; Wang, Zhang, Yuan, Wu, & Li, 2016).
Clearly, ACE2 permits virus entry into cells, but ACE2 overexpression may protect against damage (by reducing Ang II and forming Ang‐1‐7; Bukowska et al., 2017; Cheng, Wang, & Wang, 2020; Patel, Zhong, Grant, & Oudit, 2016). However, ACE2 can be “shed” from endothelial cells, by a disintegrin and metalloproteinase 17 (ADAM17) resulting in the release of a soluble circulating ACE2‐ectodomain with catalytic function (Patel et al., 2016). Therefore, the picture is complicated by a different ACE/ACE2 ratio in various tissues and by different roles of membrane‐bound and soluble ACE2. For example, it has been proposed that soluble ACE2 could quench the coronavirus by limiting its attachment to cellular ACE2 (Monteil et al., 2020). However, Sama and colleagues (Sama et al., 2020) demonstrated that male sex is correlated with elevated plasma ACE2 in heart failure (HF) COVID‐19 patients. Nevertheless, the authors recognize they have no evidence of a correlation between the levels of membrane‐bound ACE2 and enzyme shedding in the two sexes. Actually, soluble ACE2 is increased in HF with preserved and reduced ejection fraction (Patel et al., 2016). Moreover, the expression of ACE2 seems reduced in post‐menopausal women (Gagliardi, Tieri, Ortona, & Ruggieri, 2020; Hilliard, Sampson, Brown, & Denton, 2013). Interestingly, transgender males exposed to oestrogen (estradiol) and androgen deprivation (spironolactone) therapies display significantly higher ACE2 expression levels and a higher number of ACE2‐expressing Sertoli cells in the testis. As both oestrogens and androgens decrease with age (Horstman et al., 2012), this decline in hormones is likely to contribute to the reduction of ACE2 expression in both sexes with ageing. However, a 2017 study showed no differences in ACE and ACE2 serum activity between the two sexes, while a lower ACE2 serum activity was observed in younger compared to older women (Fernández‐Atucha et al., 2017). Overall, it appears that differences in the expression of ACE and ACE2 may be organ‐specific and age‐dependent in both sexes, in animals (Xie, Chen, Wang, Zhang, & Liu, 2006) and humans (Gagliardi et al., 2020; Hilliard et al., 2013) with a less clear role for soluble ACE2 (Monteil et al., 2020; Patel et al., 2016; Sama et al., 2020).
Whether ACE2 levels in the lung are related to the susceptibility and severity of COVID‐19 infection is a matter of investigation (Gheblawi et al., 2020). In a preprint paper, it is reported that men may have higher expression of ACE2 in the lungs compared to women (Zhao et al., 2020), with potentially important consequences for COVID‐19 infections, as the respiratory tract is the entry route for SARS‐CoV‐2. However, polymorphisms in both ACE and ACE2 genes can explain the increased capillary permeability, coagulation, fibrosis, and apoptosis of alveolar cells, observed in SARS and COVID‐19 (Gemmati et al., 2020; Tikellis & Thomas, 2012). These effects can explain lung damage and respiratory failure (see also below Section 3).
All in all, the role of ACE2 in the pathophysiology of COVID‐19 is not completely clear: it may act as a Trojan horse, but most evidence indicates that a low membrane‐bound ACE/ACE2 ratio may be beneficial. Indeed, ACE may be pro‐inflammatory and pro‐oxidant, whereas ACE2 may mediate antioxidant and anti‐inflammatory effects (Pagliaro & Penna, 2005, 2020). Soluble ACE2 is higher in HF; whether this is protective or dangerous or is just an epiphenomenon is not clear yet. Nevertheless, the inhibition of ACE2 shedding, by regulating the activity of ADAM17 enzyme, has been suggested as a potential therapeutic approach in HF (Patel et al., 2016).
Throughout the body, because the expression of ACE2 on the X chromosome can be influenced by oestrogens, the ACE/ACE2 ratio may be shifted towards the ACE2/Ang‐1‐7/MAS receptor axis more in women than in men (Chappell, Marshall, Alzayadneh, Shaltout, & Diz, 2014; Hilliard et al., 2013; Li, Zhou, Yang, & You, 2020; Tukiainen et al., 2017). This might explain why women are protected against severe COVID‐19 outcome. However, we have to acknowledge that there are tissue‐ and organ‐specific differences of the ACE/ACE2 ratio, which can be also influenced by exercise (Crisafulli & Pagliaro, 2020) and medical conditions (Chappell et al., 2014; Colucci et al., 2011; Li et al., 2020; Yuan et al., 2015). Whether the lethality of SARS‐CoV‐2 is mainly due to virus entry and replication or to exaggerated inflammatory response is not clear yet. Nevertheless, the beneficial effects by anti‐inflammatory drugs (see below) suggest an important role for inflammation and “cytokine storm” in COVID‐19 lethality (see below).
2.2. Is there a role for TMPRSS2 in sex differences in COVID‐19?
Although some studies suggest that TMPRSS2 is involved in determining severity of influenza in animals and humans (Cheng et al., 2015; Sakai et al., 2015), its role during coronavirus infections and in the modulation of COVID‐19 severity is still unclear. Nevertheless, we have to consider that TMPRSS2 is mainly a testosterone‐regulated gene and may have a higher expression in men than in women (Tomlins et al., 2005), thus suggesting that COVID‐19 severity could be partially explained by TMPRSS2 up‐regulation in males (McCoy et al., 2020; Sharifi & Ryan, 2020; Wambier & Goren, 2020). Nevertheless, TMPRSS2 expression levels and function are also regulated by oestrogen‐dependent signalling (Setlur et al., 2008). Intriguingly, an age‐dependent, different and overlapping expression of ACE2 and TMPRSS2 has been recently described in bronchial cells (Lukassen et al., 2020), but whether this may explain sex differences is still unknown. Therefore, the role of TMPRSS2 in determining sex differences in COVID‐19 severity needs to be further studied, as protease inhibitors seem effective in limiting SARS‐CoV‐2 cell entry (Hoffmann et al., 2020).
2.3. Is there a role for other X or Y‐linked genes in sex difference in COVID‐19?
Several other X‐linked genes (such as those for the ILs, FOXP3, XIST, and TLR7/8) and Y‐linked genes (SRY and SOX9) may also explain sex differences (Ghosh & Klein, 2017). These and other immune regulatory genes encoded by the X and Y chromosomes may explain lower viral loads and reduced inflammation in women compared to men (Conti & Younes, 2020; Márquez, Trowbridge, Kuchel, Banchereau, & Ucar, 2020; Table 2). In particular, the two X chromosomes seem to regulate the immune system even if one of them is inactive. The X chromosome regulates the immune system also modulating other proteins, including CD40L, CXCR3, and TLR8. These can be up‐regulated in women and can determine the response to viral infections as well as to vaccinations. A differentially expressed genes (DEGs) network was constructed to identify a specific gene signature characterizing SARS‐CoV‐2 infection (Fagone et al., 2020). Intriguingly, 10 DEGs were modulated by sex hormones. Six DEGs were androgen receptor‐regulated, with genes for CCL20 and CXCL1 being up‐regulated, whereas those for THBD, HEY2, BBOX1 and MYLK were down‐regulated. Four DEGs were regulated by oestrogen receptor‐α, with C3 and EDN1 genes being up‐regulated and PDK4 and VTCN1 down‐regulated. Moreover, sex differences in the immune response, determined by genes and hormones (Ghosh & Klein, 2017; Klein & Flanagan, 2016), may play an important role in modulating the severity of COVID‐19. Also, the number of CD4+ T cells differs between sexes, being higher in women with a better immune response (Conti & Younes, 2020). Finally, the number of sex‐independent, non‐genetic factors that can change susceptibility and mortality is enormous, and many other factors are likely to be considered, including gender and cultural habits in different countries. For example, an outbreak in the Republic of Korea exhibited a high incidence of cases in women due to social and religious events occurring at the time (Report on the Epidemiological Features of Coronavirus Disease 2019 [COVID‐19] Outbreak in the Republic of Korea from January 19 to March 2, 2020). Smoking can be another gender‐related habit and independent risk factor for COVID‐19 exacerbation. Nevertheless, the role of smoking on ACE/ACE2 ratio and function is not clear. In different studies, both an increase in ACE2 expression (Cai, 2020) and a decrease in enzyme activity have been described (Yuan et al., 2015). We can speculate that higher levels of ACE2 (more virus receptors) may allow for more virus entry, while ACE2 down‐regulation (less protection conferred by ACE2 anti‐inflammatory function) may explain, at least in part, COVID‐19 severity in smokers.
TABLE 2.
Summary of factors that may be involved in the different response to SARS‐CoV‐2 between sexes
| Gene | Function/role in viral infection | References |
|---|---|---|
| X‐linked | ||
| ACE2 | Antioxidant anti‐inflammatory enzyme‐receptor of Sars‐Covs | Pagliaro and Penna (2005); Cheng et al. (2015); Ghosh and Klein (2017); Márquez et al. (2020) |
| ILs | Cytokines involved in the regulation of the immune response | |
| FOXP3 | Transcription factor involved in the development and function of regulatory T cells | |
| XIST | ||
| TLRs | Receptor involved in pathogen recognition and activation of the innate immunity | |
| CXCR3 | ||
| Y‐linked | ||
| TMPRSS2 | Transmembrane protease promotes cell entrance of coronavirus | Tomlins et al. (2005); Ghosh and Klein (2017); Márquez et al. (2020) |
| SRY | Encodes for proteins involved in the immune response during viral infections | |
| SOX9 | Encodes for proteins involved in the immune response to viral infections | |
| Genes regulated by sexual hormones | Effects | |
| Oestrogens | Setlur et al. (2008); Bukowska et al. (2017); Fagone et al. (2020) | |
| ACE2 | Up‐regulation in several tissues (e.g., lungs and heart) | |
| TMPRSS2 | Fusion of the promoter region of TMPRSS2 gene to the coding region of ERG | |
| DEGs | Up‐regulation of C3 and EDN1 | |
| Down‐regulation of PDK4 and VTCN1 | ||
| Androgens | Tomlins et al. (2005); Fagone et al. (2020) | |
| TMPRSS2 | Up‐regulation in several tissues (e.g., prostate cancer) | |
| DEGs | Up‐regulation of CCL20 and CXCL1 | |
| Down‐regulation of THBD, HEY2, BBOX1, and MYLK |
Abbreviations: BBOX1, γ‐butyrobetaine hydroxylase 1; C3, complement C3; DEGs, differentially expressed genes; EDN1, endothelin 1; ERG, v‐ets erythroblastosis virus E26 oncogene homolog (avian); FOXP3, forkhead box transcription factor; HEY2, hairy/enhancer‐of‐split related with YRPW motif protein; MYLK, myosin light chain kinase; PDK4, pyruvate dehydrogenase lipoamide kinase isozyme 4; SOX9, sex‐determining region Y box 9; SRY, sex‐determining region Y; THBD, thrombomodulin; TLRs, Toll‐like receptors; TMPRSS2, transmembrane protease serine 2; VTCN1, V‐set domain containing T cell activation inhibitor 1; XIST, X inactive specific transcript.
3. SEX, PULMONARY DISEASE AND COVID‐19
Respiratory droplets that spread every time while breathing, coughing, or sneezing are the main route of transmission of SARS‐CoV‐2. Therefore, attachment of the virus to ACE2 expressed on the respiratory tract is the first step enabling entry into host cells. Therefore, COVID‐19 primarily affects the respiratory system and secondary acute respiratory distress syndrome (ARDS) is quite prevalent in COVID‐19 patients (Cheng et al., 2020; Zhou, Yang, et al., 2020). In this respect, the comparison with epidemiological evidence from influenza outbreaks and pandemics is very interesting. Opposite to COVID‐19, in influenza, morbidity and mortality are often higher for women than men. Moreover, during influenza, “cytokine storms” do not clearly differ between men and women (Klein, Hodgson, & Robinson, 2012). On the other hand, COVID‐19 elderly male patients have a greater inflammatory reaction, with higher levels of interleukins, TNF‐α, LDH, ferritin and hsCRP, thus developing a “cytokine storm,” which may lead to ARDS, multiple organ failure and, ultimately, death (Moccia et al., 2020; Qin et al., 2020). Of note, serum levels of interleukins (sIL‐2R, IL‐6, IL‐8, and IL‐10) and TNF‐α were measured in women and men with and without apparent comorbidities. Male COVID‐19 patients displayed an exaggerated production of inflammatory cytokines and proteins (Qin et al., 2020), including the anti‐inflammatory IL‐10 (Iyer & Cheng, 2012).
Epigenetics may play a role in the different response to the virus. Indeed, some studies suggest that different viruses utilize different epigenetic mechanisms to mediate antigen presentation and gene expression (Menachery et al., 2018). Sex hormones influence epigenetic regulation of gene expression in the immune response (Klein & Flanagan, 2016). Epigenetic compounds (Kiss et al., 2019; Moccia et al., 2020; Pooladanda et al., 2019) could then restore the stress resilience of both epithelial and cardiac cells in COVID‐19 patients. However, dietary intake of functional foods and regular physical exercise (Crisafulli & Pagliaro, 2020; Lionetti, Tuana, Casieri, Parikh, & Pierce, 2019) may activate Nrf2 in a variety of tissues and could be suggested to patients who present with only a few symptoms, in order to reduce the risk of major complications from COVID‐19. Indeed, exercise is a natural way to increase the expression of ACE2 and to reduce the ACE/ACE2 ratio also in the respiratory tract (Crisafulli & Pagliaro, 2020).
Importantly, ACE2 may be protective against ARDS. In mice, ACE2 down‐regulation favoured more severe lung failure (Cheng et al., 2020; Hanff, Harhay, Brown, Cohen, & Mohareb, 2020; Kuba et al., 2005). Another study (Xie et al., 2006) in rats showed that lung expression of ACE2 is drastically reduced with ageing in both sexes. As mentioned, the binding of SARSCoV‐2 spike to ACE2 down‐regulates ACE2, thus decreasing bradykinin and Ang II catabolism, as well as Ang‐1‐7 formation. The dysregulation of these factors may explain the pathogenesis of respiratory failure and pulmonary hypertension (Gurwitz, 2020; Horn, Chakinala, Oudiz, Joseloff, & Rosenzweig, 2020). Moreover, bradykinin accumulation may explain inflammatory processes, cough and fever. Bradykinin also favours both the complement system and coagulation, mechanisms typical of angioedema, sepsis, and cardiovascular dysfunction, as found in COVID‐19 patients (Colarusso, Terlizzi, Pinto, & Sorrentino, 2020). Actually, a large number of COVID‐19 patients exhibit severe cardiovascular damage (Moccia et al., 2020) and, as reported above, patients with pre‐existing cardiovascular diseases (CVDs) appear to have an increased risk of death (also see below).
4. SEX, CARDIOVASCULAR DISEASE AND COVID‐19
Cardiovascular disease is more prevalent in males, and subjects with cardiovascular dysfunction infected with SARS‐CoV‐2 have a worse prognosis. As already discussed, the poor prognosis of patients with COVID‐19 is related to factors such as male sex, ageing, and underlying diseases, especially dysmetabolic and CVDs (see AlGhatrif et al., 2020; Moccia et al., 2020). For example, among the deceased COVID‐19 patients in Italy, less than 4% had no comorbidity, while more than 60% had three or more comorbidities. Among these, cardiovascular comorbidities were the most represented and included arterial hypertension (about 70% of deceased patients), followed by ischaemic heart disease (about 30%), atrial fibrillation (about 20%), and HF (about 15%; https://www.iss.it/coronavirus, accessed on May 13, 2020). Most of the deceased patients were elderly (over 65 years) and obese (in the Italian report, obesity is present in 12% of the deceased patients). All these conditions are characterized by an abnormal ACE/ACE2 ratio in humans and animals (Colucci et al., 2011; Koni & Miyamori, 2007; Santos et al., 2013; Wang et al., 2015, 2016). It appears that an abnormal ACE/ACE2 ratio is responsible, not only for a high incidence of severe ARDS but also for cardiovascular complications and the high lethality of COVID‐19. Oestrogens up‐regulate the expression of ACE2 in human atrial tissue (Bukowska et al., 2017), explaining the higher ACE2 expression in the heart of women. As early as 2002, immediately after the discovery of ACE2, a sex‐dependent role of ACE2 in HF, with less severe impairment in female than in male mice, has been described and subsequently confirmed (Crackower et al., 2002; Patel et al., 2016). SARS‐CoV‐2 down‐regulates ACE2, and this may favour the ACE/AT1 receptor axis and may predispose to CVDs (Horn et al., 2020). Indeed, down‐regulation of ACE2 has been observed in pulmonary arterial hypertension. ACE2 down‐regulation and inflammatory response may favour endothelial dysfunction and coagulopathy, thus worsening the CVD (Guzik et al., 2020; Moccia et al., 2020). Therefore, the lower ACE/ACE2 ratio in the female heart may limit coagulopathy and COVID‐19‐induced exacerbation of CVD (Gemmati et al., 2020; Moccia et al., 2020).
Therefore, re‐establishing an adequate ACE/ACE2 ratio may lead to better outcomes in COVID‐19. Indeed, COVID‐19 depletes and down‐regulates ACE2 (Moccia et al., 2020). Therefore, the anti‐inflammatory effect of drugs that activate ACE2 may be exploited as a potential therapy in this setting (Figure 1). Of note, oestrogens significantly down‐regulate ACE levels while up‐regulating ACE2 and MAS receptor expression, thus shifting from the classical RAS/ACE/AT1 receptor axis to the protective RAS/ACE2/MAS axis (Bukowska et al., 2017). Already in 2017, it was proposed that oestrogens have a protective role in SARS by regulating immune response and limiting SARS‐CoV replication directly (Channappanavar et al., 2017). Therefore, exogenous oestrogen administration has been proposed for both male and female COVID‐19 patients (Cutolo, Smith, & Paolino, 2020; Suba, 2020), and a couple of Clinical Trials on the role of sex hormones in COVID‐19 patients are already ongoing (NCT04359329 and NCT04365127). Animal studies on drugs that can limit SARS‐CoV‐2 effects are lacking. Preliminary studies report that this virus may infect ferrets, hamsters, and cats, inducing mild symptoms, but not pigs or birds (Chan et al., 2020; Shi et al., 2020). Interestingly, a very recent preliminary study shows that mice overexpressing human ACE2 may develop COVID‐19‐like signs in response to infection with SARS‐CoV‐2 (Jiang et al., 2020). These animals showed different susceptibility and, intriguingly, the male mice showed a higher death rate than the females.
FIGURE 1.
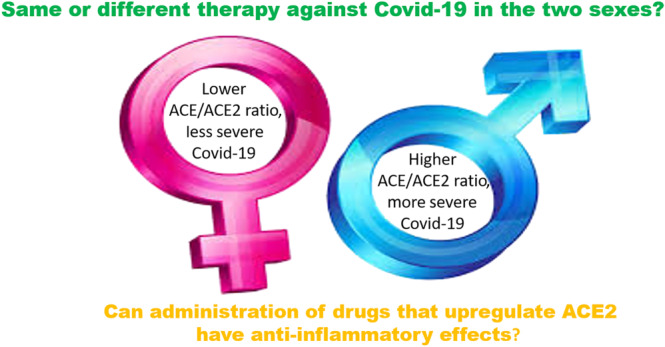
Possible role of ACE/ACE2 ratio in therapies against COVID‐19 in the two sexes. It has been proposed that pathological conditions presenting with a high ACE/ACE2 ratio predispose towards worse COVID‐19 outcomes (Gemmati et al., 2020; Pagliaro & Penna, 2020). ACE2 is a membrane‐bound enzyme, whose gene lies on the X chromosome and is up‐regulated by oestrogens in males and females. Throughout the body, the ACE/ACE2 ratio may be lower in women than in men, and this is theoretically protective because of the anti‐inflammatory properties of ACE2. However, it must be kept in mind that ACE2 in the lung may act as the entry gate for COVID‐19, and the ACE/ACE2 ratio may be different in tissues and organs, and that this ratio is influenced by many factors including, exercise, ageing, and diseases (Crisafulli & Pagliaro, 2020). Therefore, more studies are necessary to clarify the role of the ACE/ACE2 ratio in the two sexes
5. OTHER PROPOSED DRUGS
Drugs that can increase ACE2 activity include losartan (NCT04312009, NCT04311177, NCT04340557, and NCT04343001; clinicaltrials.gov), diminazene diaceturate, resorcinol naphthalein, and xantenone (Li et al., 2020). Also, AT1 receptor antagonists have been considered as anti‐COVID‐19 therapeutics (Gurwitz, 2020). Furthermore, recombinant ACE2 has been proposed in both pneumonia (Khan et al., 2017) and COVID‐19 (Monteil et al., 2020).
Currently, remdesivir, used against Ebola, and chloroquine/hydroxychloroquine, used against malaria (Luo et al., 2020; Yazdany & Kim, 2020), are being used for COVID‐19 patients. Between the submission and revision of this review article, safety concerns have been raised about the chloroquine/hydroxylchloroquine use in COVID‐19, and the discussion is still open (Paliani & Cardona, 2020).
A “cytokine storm” has been proposed several times as responsible for COVID‐19 lethality (e.g., Moccia et al., 2020; Qin et al., 2020) and, consequently, the anti‐IL‐6 receptor antibody, tocilizumab (used for the treatment of rheumatoid arthritis and CRS after CAR‐T therapies; Alvi et al., 2019), has been proposed in many clinical studies, and it is now in Phase II and Phase III studies in COVID‐19 patients (Lu, Chen, & Chang, 2020; Luo et al., 2020). Monoclonal antibodies, anti‐IL‐1 and anti‐IL‐6, and plasma derived from COVID‐19 recovered patients have been proposed (https://www.sciencenews.org/article/coronavirus-covid-19-can-plasma-recovered-patients-treat-sick). Other anti‐inflammatory drugs, including JAK inhibitors, and glucocorticoids may also be useful (Zhang et al., 2020). Indeed, a preliminary study showed that dexamethasone was able to reduce 28‐day mortality among COVID‐19 patients receiving invasive mechanical ventilation (Horby et al., 2020). Also, blockade of the kallikrein‐kinin system, upstream of bradykinin, by lanadelumab (already used in hereditary angioedema) has been proposed for COVID‐19 patients (Colarusso et al., 2020). Promising drugs are blockers of TMPRSS2, such as camostat mesylate and nafamostat mesylate (see Zhou, Fang, et al., 2020).
Coagulopathies are also a prominent aspect of severe Covid‐19 patients. Thus, anticoagulant treatments may decrease mortality (Kollias et al., 2020; Tang et al., 2020) in an ACE/ACE2 dependent and sex‐related way (Gemmati et al., 2020). While waiting for vaccines and new therapeutic strategies to fight this terrible pandemic, different antiviral options are under clinical trial as combination therapies. These include hydroxylchloroquine alone or in combination with azithromycin, and remdesivir, as well as lopinavir/ritonavir alone or with interferon (ClinicalTrials.gov identifier: NCT04332094, NCT04332107, NCT04322123, NCT04335552, NCT04336332, and NCT04339816). To the best of our knowledge, none of these studies considered different therapeutic approaches for men and women. Moreover, for many of these drugs, the effects on ACE/ACE2 ratio are unknown. Even in vaccination, sex is a variable that should be considered. Indeed, pathogen‐specific and non‐specific effects of vaccines present differences between sexes that can be exploited in fighting COVID‐19 (Aaby et al., 2020). Of note, the antibody response to vaccinations is actually thought to be greater in women than men, and possibly, this might underlie future protection. However, women display more adverse events than men following vaccinations (Fischinger, Boudreau, Butler, Streeck, & Alter, 2019).
A recent study (Fagone et al., 2020) investigated the transcriptomic profile in primary human lung cells upon infection with SARS‐CoV‐2. In this study, the transcriptomic profile of lung tissue from healthy men and women were compared with the transcriptomic induced by the virus. It emerged that at ages 40–60 years, the transcriptomic feature of female lung tissue was more similar to those induced by SARS‐CoV‐2 than in male tissue. The authors suggest that a lower threshold of acute response to SARS‐CoV‐2 infection in men may, at least partly, explain the lower lethality in women. Nevertheless, the potential factors that might induce this “COVID‐19‐resistant lung phenotype” in middle‐aged women is not clear. In this study, targeting the mammalian target of rapamycin (mTOR) pathway using sirolimus appeared to be a promising therapeutic approach to fight COVID‐19. Also MAPK kinase (MEK), IκB kinase (IKK), and Akt inhibitors have been proposed as candidate drugs (Fagone et al., 2020). Of note, some of these enzymes are linked to ACE2 anti‐inflammatory action (Dhawale et al., 2016). Nevertheless, this study does not envisage different therapeutic approaches for men and women.
6. CONCLUSIONS
Significant sex‐related differences are present in the rate of severe cases of COVID‐19. Several potential factors underlying these differences in pathogenic mechanisms are identified at the molecular level. All the above‐mentioned drugs, targeting these mechanisms, would warrant clinical studies. In particular, the ACE/ACE2 ratio must be considered (Figure 1) and drugs that positively influence this ratio should be taken into account. Beside a wide range of factors that may influence outcome, sex should be one of the criteria to consider in order to select the appropriate therapies for the appropriate patients. Indeed, given the striking differences in lethality between the two sexes, we believe that studying sex differences may help to find appropriate therapies for all patients. Only large unbiased studies considering all factors and hypotheses mentioned here concerning sex differences may explain why women are less at risk of dying from COVID‐19 and might help to find patient‐tailored therapies. It is, therefore, recommended that sex‐disaggregated data are provided for all COVID19 studies.
6.1. Nomenclature of targets and ligands
Key protein targets and ligands in this article are hyperlinked to corresponding entries in http://www.guidetopharmacology.org, the common portal for data from the IUPHAR/BPS Guide to PHARMACOLOGY (Harding et al., 2018), and are permanently archived in the Concise Guide to PHARMACOLOGY2019/20 (Alexander, Christopoulos, et al., 2019; Alexander, Fabbro, et al., 2019a, 2019b).
CONFLICT OF INTEREST
Relationship: Dr. Tocchetti has a Canadian Patent No. 2,613,477, issued on December 3, 2013 Inventors: Nazareno Paolocci, David A Kass, Carlo G Tocchetti. Owner: Johns Hopkins University Entitled: THIOL‐SENSITIVE POSITIVE INOTROPES JHU Ref.: C04755‐P04755‐05 with royalties paid. No other relationships/conditions/circumstances that present a potential conflict of interest.
ACKNOWLEDGEMENTS
P.P. and C.G.T. are Members of COST Action EU‐CARDIOPROTECTION CA16225. C.P. and P.P. report grants from the University of Torino, Ricerca Locale Ex‐60% (Grants: PAGP_RILO_16_01; PENC_RILO) and from MIUR (PAGP_FFABR_17_01 and by PENC_FFABR_17_01). C.G.T. reports personal fees from Alere, outside the submitted work. V.M. reports a grant from SIC/MSD, outside the submitted work.
Penna C, Mercurio V, Tocchetti CG, Pagliaro P. Sex‐related differences in COVID‐19 lethality. Br J Pharmacol. 2020;177:4375–4385. 10.1111/bph.15207
Contributor Information
Carlo G. Tocchetti, Email: carlogabriele.tocchetti@unina.it.
Pasquale Pagliaro, Email: pasquale.pagliaro@unito.it.
REFERENCES
- Aaby, P. , Benn, C. S. , Flanagan, K. L. , Klein, S. L. , Kollmann, T. R. , Lynn, D. J. , & Shann, F. (2020). The non‐specific and sex‐differential effects of vaccines. Nature Reviews. Immunology, 27, 1–7. 10.1038/s41577-020-0338-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander, S. P. H. , Christopoulos, A. , Davenport, A. P. , Kelly, E. , Mathie, A. , Peters, J. A. , … CGTP Collaborators . (2019). THE CONCISE GUIDE TO PHARMACOLOGY 2019/20: G protein‐coupled receptors. British Journal of Pharmacology, 176, S21–S141. 10.1111/bph.14748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander, S. P. H. , Fabbro, D. , Kelly, E. , Mathie, A. , Peters, J. A. , Veale, E. L. , … CGTP Collaborators . (2019a). THE CONCISE GUIDE TO PHARMACOLOGY 2019/20: Catalytic receptors. British Journal of Pharmacology, 176, S247–S296. 10.1111/bph.14751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander, S. P. H. , Fabbro, D. , Kelly, E. , Mathie, A. , Peters, J. A. , Veale, E. L. , … CGTP Collaborators . (2019b). THE CONCISE GUIDE TO PHARMACOLOGY 2019/20: Enzymes. British Journal of Pharmacology, 176, S297–S396. 10.1111/bph.14752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alghamdi, I. G. , Hussain, I. I. , Almalki, S. S. , Alghamdi, M. S. , Alghamdi, M. M. , & El‐Sheemy, M. A. (2014). The pattern of Middle East respiratory syndrome coronavirus in Saudi Arabia: A descriptive epidemiological analysis of data from the Saudi Ministry of Health. Int J Gen Med, 7, 417–423. 10.2147/IJGM.S67061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- AlGhatrif, M. , Cingolani, O. , & Lakatta, E. G. (2020). The dilemma of coronavirus disease 2019, aging, and cardiovascular disease: Insights from cardiovascular aging science. JAMA Cardiology, 5, 747 10.1001/jamacardio.2020.1329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvi, R. M. , Frigault, M. J. , Fradley, M. G. , Jain, M. D. , Mahmood, S. S. , Awadalla, M. , … Neilan, T. G. (2019). Cardiovascular events among adults treated with chimeric antigen receptor T‐cells (CAR‐T). Journal of the American College of Cardiology, 74(25), 3099–3108. 10.1016/j.jacc.2019.10.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bukowska, A. , Spiller, L. , Wolke, C. , Lendeckel, U. , Weinert, S. , Hoffmann, J. , … Goette, A. (2017). Protective regulation of the ACE2/ACE gene expression by estrogen in human atrial tissue from elderly men. Experimental Biology and Medicine (Maywood, N.J.), 242(14), 1412–1423. 10.1177/1535370217718808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai, H. (2020). Sex difference and smoking predisposition in patients with COVID‐19. The Lancet Respiratory Medicine, 8, e20 10.1016/S2213-2600(20)30117-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan, J. F. , Zhang, A. J. , Yuan, S. , Poon, V. K. , Chan, C. C. , Lee, A. C. , … Yuen, K. Y. (2020). Simulation of the clinical and pathological manifestations of coronavirus disease 2019 (COVID‐19) in golden Syrian hamster model: Implications for disease pathogenesis and transmissibility. Clinical Infectious Diseases, 26, ciaa325 10.1093/cid/ciaa325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Channappanavar, R. , Fett, C. , Mack, M. , Ten Eyck, P. P. , Meyerholz, D. K. , & Perlman, S. (2017). Sex‐based differences in susceptibility to severe acute respiratory syndrome coronavirus infection. Journal of Immunology, 198, 4046–4053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chappell, M. C. , Marshall, A. C. , Alzayadneh, E. M. , Shaltout, H. A. , & Diz, D. I. (2014). Update on the angiotensin converting enzyme 2‐angiotensin (1‐7)‐MAS receptor axis: Fetal programing, sex differences, and intracellular pathways. Front Endocrinol (Lausanne), 4, 201 10.3389/fendo.2013.00201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, N. , Zhou, M. , Dong, X. , Qu, J. , Gong, F. , Han, Y. , … Zhang, L. (2020). Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet, 395(10223), 507–513. 10.1016/S0140-6736(20)30211-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, T. , Wu, D. , Chen, H. , Yan, W. , Yang, D. , Chen, G. , … Ning, Q. (2020). Clinical characteristics of 113 deceased patients with coronavirus disease 2019: Retrospective study. BMJ, 368, m1091 10.1136/bmj.m1091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng, H. , Wang, Y. , & Wang, G. Q. (2020). Organ‐protective effect of angiotensin‐converting enzyme 2 and its effect on the prognosis of COVID‐19. Journal of Medical Virology, 92(7), 726–730. 10.1002/jmv.25785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng, Z. , Zhou, J. , To, K. K. , Chu, H. , Li, C. , Wang, D. , … Yuen, K. Y. (2015). Identification of TMPRSS2 as a susceptibility gene for severe 2009 pandemic A(H1N1) influenza and A(H7N9) influenza. The Journal of Infectious Diseases, 212, 1214–1221. 10.1093/infdis/jiv246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colarusso, C. , Terlizzi, M. , Pinto, A. , & Sorrentino, R. (2020). A lesson from a saboteur: High molecular weight kininogen (HMWK) impact in COVID‐19. British Journal of Pharmacology. 10.1111/bph.15154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colucci, J. A. , Yuri Arita, D. , Sousa Cunha, T. , Seno Di Marco, G. , Vio, C. P. , Pacheco‐Silva, A. , & Casarini, D. E. (2011). Renin‐angiotensin system may trigger kidney damage in NOD mice. Journal of the Renin‐Angiotensin‐Aldosterone System, 12, 15–22. 10.1177/1470320310375456. PMID: 20627940 [DOI] [PubMed] [Google Scholar]
- Conti, P. , & Younes, A. (2020). Coronavirus COV‐19/SARS‐CoV‐2 affects women less than men: clinical response to viral infection. Journal of Biological Regulators and Homeostatic Agents, 34(2), 71 10.23812/Editorial-Conti-3 [DOI] [PubMed] [Google Scholar]
- Crackower, M. A. , Sarao, R. , Oudit, G. Y. , Yagil, C. , Kozieradzki, I. , Scanga, S. E. , … Penninger, J. M. (2002). Angiotensin‐converting enzyme 2 is an essential regulator of heart function. Nature, 417(6891), 822–828. 10.1038/nature00786 [DOI] [PubMed] [Google Scholar]
- Crisafulli, A. , & Pagliaro, P. (2020). Physical activity/inactivity and COVID‐19. European Journal of Preventive Cardiology, 18, 2047487320927597 10.1177/2047487320927597 [DOI] [Google Scholar]
- Cutolo, M. , Smith, V. , & Paolino, S. (2020). Understanding immune effects of oestrogens to explain the reduced morbidity and mortality in female versus male COVID‐19 patients. Comparisons with Autoimmunity and Vaccination. Clinical and Experimental Rheumatology, 38, 383–386. [PubMed] [Google Scholar]
- Dhawale, V. S. , Amara, V. R. , Karpe, P. A. , Malek, V. , Patel, D. , & Tikoo, K. (2016). Activation of angiotensin‐converting enzyme 2 (ACE2) attenuates allergic airway inflammation in rat asthma model. Toxicology and Applied Pharmacology, 306, 17–26. 10.1016/j.taap.2016.06.026 [DOI] [PubMed] [Google Scholar]
- Fagone, P. , Ciurleo, R. , Lombardo, S. D. , Iacobello, C. , Palermo, C. I. , Shoenfeld, Y. , … Nicoletti, F. (2020). Transcriptional landscape of SARS‐CoV‐2 infection dismantles pathogenic pathways activated by the virus, proposes unique sex‐specific differences and predicts tailored therapeutic strategies. Autoimmunity Reviews, 3, 102571 10.1016/j.autrev.2020.102571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernández‐Atucha, A. , Izagirre, A. , Fraile‐Bermúdez, A. B. , Kortajarena, M. , Larrinaga, G. , Martinez‐Lage, P. , … Gil, J. (2017). Sex differences in the aging pattern of renin‐angiotensin system serum peptidases. Biology of Sex Differences, 8, 5 10.1186/s13293-017-0128-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischinger, S. , Boudreau, C. M. , Butler, A. L. , Streeck, H. , & Alter, G. (2019). Sex differences in vaccine‐induced humoral immunity. Seminars in Immunopathology, 41(2), 239–249. 10.1007/s00281-018-0726-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gagliardi, M. C. , Tieri, P. , Ortona, E. , & Ruggieri, A. (2020). ACE2 expression and sex disparity in COVID‐19. Cell Death Discov, 6, 37 10.1038/s41420-020-0276-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gemmati, D. , Bramanti, B. , Serino, M. L. , Secchiero, P. , Zauli, G. , & Tisato, V. (2020). COVID‐19 and individual genetic susceptibility/receptivity: Role of ACE1/ACE2 genes, immunity, inflammation and coagulation. Might the double X‐chromosome in females be protective against SARS‐CoV‐2 compared to the single X‐chromosome in males? International Journal of Molecular Sciences, 21(10), E3474 10.3390/ijms21103474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gheblawi, M. , Wang, K. , Viveiros, A. , Nguyen, Q. , Zhong, J. C. , Turner, A. J. , … Oudit, G. Y. (2020). Angiotensin converting enzyme 2: SARS‐CoV‐2 receptor and regulator of the renin‐angiotensin system. Circulation Research, 126(10), 1456–1474. 10.1161/CIRCRESAHA.120.317015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghosh, S. , & Klein, R. S. (2017). Sex drives dimorphic immune responses to viral infections. Journal of Immunology, 198(5), 1782–1790. 10.4049/jimmunol.1601166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan, W. J. , Ni, Z. Y. , Hu, Y. , Liang, W. H. , Ou, C. Q. , He, J. X. , … China Medical Treatment Expert Group for Covid‐19 . (2020). Clinical characteristics of coronavirus disease 2019 in China. The New England Journal of Medicine, 382, 1708–1720. 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurwitz, D. (2020). Angiotensin receptor blockers as tentative SARSCoV‐2 therapeutics. Drug Development Research. 10.1002/ddr.21656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guzik, T. J. , Mohiddin, S. A. , Dimarco, A. , Patel, V. , Savvatis, K. , Marelli‐Berg, F. M. , … McInnes, I. B. (2020). COVID‐19 and the cardiovascular system: Implications for risk assessment, diagnosis, and treatment options. Cardiovascular Research, 116(10), 1666–1687. 10.1093/cvr/cvaa106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanff, T. C. , Harhay, M. O. , Brown, T. S. , Cohen, J. B. , & Mohareb, A. M. (2020). Is there an association between COVID‐19 mortality and the renin‐angiotensin system—A call for epidemiologic investigations. Clinical Infectious Diseases: an official publication of the Infectious Diseases Society of America, 71(15), 870–874. 10.1093/cid/ciaa329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harding, S. D. , Sharman, J. L. , Faccenda, E. , Southan, C. , Pawson, A. J. , Ireland, S. , … NC‐IUPHAR . (2018). The IUPHAR/BPS guide to PHARMACOLOGY in 2018: Updates and expansion to encompass the new guide to IMMUNOPHARMACOLOGY. Nucleic Acids Research, 46, D1091–D1106. 10.1093/nar/gkx1121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilliard, L. M. , Sampson, A. K. , Brown, R. D. , & Denton, K. M. (2013). The “his and hers” of the renin‐angiotensin system. Current Hypertension Reports, 15(1), 71–79. 10.1007/s11906-012-0319-y [DOI] [PubMed] [Google Scholar]
- Hoffmann, M. , Kleine‐Weber, H. , Schroeder, S. , Krüger, N. , Herrler, T. , Erichsen, S. , … Pöhlmann, S. (2020). SARS‐CoV‐2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell, 181(2), 271–280.e8. 10.1016/j.cell.2020.02.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horby, P. , Lim, W. S. , Emberson, J. , Mafham, M. , Bell, J. , Linsell, L. , … RECOVERY Collaborative Group . (2020). Effect of dexamethasone in hospitalized patients with COVID‐19: Preliminary report. medRxiv. 10.1101/2020.06.22.20137273 [DOI] [Google Scholar]
- Horn, E. M. , Chakinala, M. , Oudiz, R. , Joseloff, E. , & Rosenzweig, E. B. (2020). Could pulmonary arterial hypertension patients be at a lower risk from severe COVID‐19? Pulm Circ, 10, 204589402092279 10.1177/2045894020922799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horstman, A. M. , Dillon, E. L. , Urban, R. J. , & Sheffield‐Moore, M. (2012). The role of androgens and estrogens on healthy aging and longevity. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 67, 1140–1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, C. , Wang, Y. , Li, X. , Ren, L. , Zhao, J. , Hu, Y. , … Cao, B. (2020). Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet, 395(10223), 497–506. 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iyer, S. S. , & Cheng, G. (2012). Role of interleukin 10 transcriptional regulation in inflammation and autoimmune disease. Critical Reviews in Immunology, 32(1), 23–63. 10.1615/critrevimmunol.v32.i1.30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang, R. D. , Liu, M. Q. , Chen, Y. , Shan, C. , Zhou, Y. W. , Shen, X. R. , … Shi, Z. L. (2020). Pathogenesis of SARS‐CoV‐2 in transgenic mice expressing human angiotensin‐converting enzyme 2. Cell, 21, S0092‐8674(20)30622‐X 10.1016/j.cell.2020.05.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlberg, J. , Chong, D. S. , & Lai, W. Y. (2004). Do men have a higher case fatality rate of severe acute respiratory syndrome than women do? American Journal of Epidemiology, 159, 229–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan, A. , Benthin, C. , Zeno, B. , Albertson, T. E. , Boyd, J. , Christie, J. D. , … Lazaar, A. L. (2017). A pilot clinical trial of recombinant human angiotensin‐converting enzyme 2 in acute respiratory distress syndrome. Critical Care, 21(1), 234 10.1186/s13054-017-1823-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiss, T. , Balasubramanian, P. , Valcarcel‐Ares, M. N. , Tarantini, S. , Yabluchanskiy, A. , Csipo, T. , … Ungvari, Z. (2019). Nicotinamide mononucleotide (NMN) treatment attenuates oxidative stress and rescues angiogenic capacity in aged cerebromicrovascular endothelial cells: A potential mechanism for the prevention of vascular cognitive impairment. Geroscience, 41(5), 619–630. 10.1007/s11357-019-00074-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein, S. L. , & Flanagan, K. L. (2016). Sex differences in immune responses. Nature Reviews. Immunology, 16(10), 626–638. 10.1038/nri.2016.90 [DOI] [PubMed] [Google Scholar]
- Klein, S. L. , Hodgson, A. , & Robinson, D. P. (2012). Mechanisms of sex disparities in influenza pathogenesis. Journal of Leukocyte Biology, 92(1), 67–73. 10.1189/jlb.0811427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kollias, A. , Kyriakoulis, K. G. , Dimakakos, E. , Poulakou, G. , Stergiou, G. S. , & Syrigos, K. (2020). Thromboembolic risk and anticoagulant therapy in COVID‐19 patients: Emerging evidence and call for action. British Journal of Haematology, 189(5), 846–847. 10.1111/bjh.16727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koni, I. , & Miyamori, I. (2007). Synergistic expression of angiotensin‐converting enzyme (ACE)and ACE2 in human renal tissue and confounding effects of hypertension on the ACE to ACE2 ratio. Endocrinology, 148, 2453–2457. 10.1210/en.2006-1287 [DOI] [PubMed] [Google Scholar]
- Kuba, K. , Imai, Y. , Rao, S. , Gao, H. , Guo, F. , Guan, B. , … Penninger, J. M. (2005). A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus‐induced lung injury. Nature Medicine, 11(8), 875–879. 10.1038/nm1267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leong, H. N. , Earnest, A. , Lim, H. H. , Chin, C. F. , Tan, C. , Puhaindran, M. E. , … Leo, Y. S. (2006). SARS in Singapore—Predictors of disease severity. Annals of the Academy of Medicine, Singapore, 35, 326–331. [PubMed] [Google Scholar]
- Li, Y. , Zhou, W. , Yang, L. , & You, R. (2020). Physiological and pathological regulation of ACE2, the SARS‐CoV‐2 receptor. Pharmacological Research, 157, 104833 10.1016/j.phrs.2020.104833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lionetti, V. , Tuana, B. S. , Casieri, V. , Parikh, M. , & Pierce, G. N. (2019). Importance of functional food compounds in cardioprotection through action on the epigenome. European Heart Journal, 40(7), 575–582. 10.1093/eurheartj/ehy597 [DOI] [PubMed] [Google Scholar]
- Lu, C.‐C. , Chen, M.‐Y. , & Chang, Y.‐L. (2020). Potential therapeutic agents against COVID‐19: What we know so far. Journal of the Chinese Medical Association, 83(6), 534–536. 10.1097/JCMA.0000000000000318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lukassen, S. , Chua, R. L. , Trefzer, T. , Kahn, N. C. , Schneider, M. A. , Muley, T. , … Eils, R. (2020). SARS‐CoV‐2 receptor ACE2 and TMPRSS2 are primarily expressed in bronchial transient secretory cells. EMBO J 2020, 39(10), e105114 10.15252/embj.20105114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo, P. , Liu, Y. , Qiu, L. , Liu, X. , Liu, D. , & Li, J. (2020). Tocilizumab treatment in COVID‐19: A single center experience. Journal of Medical Virology, 92(7), 814–818. 10.1002/jmv.25801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Márquez, E. J. , Trowbridge, J. , Kuchel, G. A. , Banchereau, J. , & Ucar, D. (2020). The lethal sex gap: COVID‐19. Immunity & Ageing, 17, 13–18. 10.1186/s12979-020-00183-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCoy, J. , Wambier, C. G. , Vano‐Galvan, S. , Shapiro, J. , Sinclair, R. , Müller Ramos, P. , … Goren, A. (2020). Racial variations in COVID‐19 deaths may be due to androgen receptor genetic variants associated with prostate cancer and androgenetic alopecia. Are anti‐androgens a potential treatment for COVID‐19? Journal of Cosmetic Dermatology, 19, 1542–1543. 10.1111/jocd.13455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menachery, V. D. , Schäfer, A. , Burnum‐Johnson, K. E. , Mitchell, H. D. , Eisfeld, A. J. , Walters, K. B. , … Baric, R. S. (2018). MERS‐CoV and H5N1 influenza virus antagonize antigen presentation by altering the epigenetic landscape. Proceedings of the National Academy of Sciences of the United States of America, 115(5), E1012–E1021. 10.1073/pnas.1706928115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moccia, F. , Gerbino, A. , Lionetti, V. , Miragoli, M. , Munaron, L. M. , Pagliaro, P. , … Angelone, T. (2020). COVID‐19‐associated cardiovascular morbidity in older adults: A position paper from the Italian Society of Cardiovascular Researches. Geroscience, 42(4), 1021–1049. 10.1007/s11357-020-00198-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monteil, V. , Kwon, H. , Prado, P. , Hagelkrüys, A. , Wimmer, R. A. , Stahl, M. , … Penninger, J. M. (2020). Inhibition of SARS‐CoV‐2 infections in engineered human tissues using clinical‐grade soluble human ACE2. Cell, 181(20), 30398–30399. 10.1016/j.cell.2020.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagliaro, P. , & Penna, C. (2005). Rethinking the renin‐angiotensin system and its role in cardiovascular regulation. Cardiovascular Drugs and Therapy, 19(1), 77–87. 10.1007/s10557-005-6900-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagliaro, P. , & Penna, C. (2020). ACE/ACE2 ratio: A key also in 2019 coronavirus disease (Covid‐19)? Frontiers in Medicine, 7, 335 10.3389/fmed.2020.00335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paliani, U. , & Cardona, A. (2020). COVID‐19 and hydroxychloroquine: Is the wonder drug failing? European Journal of Internal Medicine, 78, 1–3. 10.1016/j.ejim.2020.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel, V. B. , Zhong, J. C. , Grant, M. B. , & Oudit, G. Y. (2016). Role of the ACE2/angiotensin 1‐7 axis of the renin‐angiotensin system in heart failure. Circulation Research, 118, 1313–1326. 10.1161/CIRCRESAHA.116.307708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pooladanda, V. , Thatikonda, S. , Bale, S. , Pattnaik, B. , Sigalapalli, D. K. , Bathini, N. B. , … Godugu, C. (2019). Nimbolide protects against endotoxin‐induced acute respiratory distress syndrome by inhibiting TNF‐α mediated NF‐κB and HDAC‐3 nuclear translocation. Cell Death & Disease, 10(2), 81 10.1038/s41419-018-1247-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin, L. , Li, X. , Shi, J. , Yu, M. , Wang, K. , Tao, Y. , … Xie, M. (2020). Gendered effects on inflammation reaction and outcome of COVID‐19 patients in Wuhan. Journal of Medical Virology. 10.1002/jmv.26137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakai, K. , Sekizuka, T. , Ami, Y. , Nakajima, N. , Kitazawa, M. , Sato, Y. , … Takeda, M. (2015). A mutant H3N2 influenza virus uses an alternative activation mechanism in TMPRSS2 knockout mice by loss of an oligosaccharide in the hemagglutinin stalk region. Journal of Virology, 89, 5154–5158. 10.1128/JVI.00124-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sama, I. E. , Ravera, A. , Santema, B. T. , van Goor, H. , Ter Maaten, J. M. , Cleland, J. G. F. , … Voors, A. A. (2020). Circulating plasma concentrations of angiotensin‐converting enzyme 2 in men and women with heart failure and effects of renin‐angiotensin‐aldosterone inhibitors. European Heart Journal, 41(19), 1810–1817. 10.1093/eurheartj/ehaa373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos, S. H. , Andrade, J. M. , Fernandes, L. R. , Sinisterra, R. D. , Sousa, F. B. , Feltenberger, J. D. , … Santos, R. A. (2013). Oral angiotensin‐(1‐7) prevented obesity and hepatic inflammation by inhibition of resistin/TLR4/MAPK/NF‐κB in rats fed with high‐fat diet. Peptides, 46, 47–52. 10.1016/j.peptides.2013.05.010 [DOI] [PubMed] [Google Scholar]
- Setlur, S. R. , Mertz, K. D. , Hoshida, Y. , Demichelis, F. , Lupien, M. , Perner, S. , … Rubin, M. A. (2008). Estrogen‐dependent signaling in a molecularly distinct subclass of aggressive prostate cancer. Journal of the National Cancer Institute, 100(11), 815–825. 10.1093/jnci/djn150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharifi, N. , & Ryan, C. J. (2020). Androgen hazards with COVID‐19. Endocrine‐Related Cancer, 27(6), E1–E3. 10.1530/ERC-20-0133 [DOI] [PubMed] [Google Scholar]
- Shi, J. , Wen, Z. , Zhong, G. , Yang, H. , Wang, C. , Huang, B. , … Bu, Z. (2020). Susceptibility of ferrets, cats, dogs, and other domesticated animals to SARS‐coronavirus 2. Science, 368(6494), 1016–1020. 10.1126/science.abb7015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suba, Z. (2020). Prevention and therapy of COVID‐19 via exogenous estrogen treatment for both male and female patients; an opinion paper. Journal of Pharmacy & Pharmaceutical Sciences, 23(1), 75–85. 10.18433/jpps31069 [DOI] [PubMed] [Google Scholar]
- Tang, N. , Bai, H. , Chen, X. , Gong, J. , Li, D. , & Sun, Z. (2020). Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. Journal of Thrombosis and Haemostasis, 18(5), 1094–1099. 10.1111/jth.14817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tikellis, C. , & Thomas, M. C. (2012). Angiotensin‐converting enzyme 2 (ACE2) is a key modulator of the renin angiotensin system in health and disease. International Journal of Peptide, 2012, 256294 10.1155/2012/256294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomlins, S. A. , Rhodes, D. R. , Perner, S. , Dhanasekaran, S. M. , Mehra, R. , Sun, X. W. , … Chinnaiyan, A. M. (2005). Recurrent fusion of TMPRSS2 and ETS transcription factor genes in prostate cancer. Science, 310(5748), 644–648. 10.1126/science.1117679 [DOI] [PubMed] [Google Scholar]
- Tukiainen, T. , Villani, A. C. , Yen, A. , Rivas, M. A. , Marshall, J. L. , Satija, R. , … MacArthur, D. G. (2017). Landscape of X chromosome inactivation across human tissues. Nature, 550(7675), 244–248. 10.1038/nature24265 Erratum in: Nature. 2018 Mar 7;555(7695):274 [DOI] [PubMed] [Google Scholar]
- Wambier, C. G. , & Goren, A. (2020). SARS‐COV‐2 infection is likely to be androgen mediated. Journal of the American Academy of Dermatology, 83(1), 308–309. 10.1016/j.jaad.2020.04.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, D. , Hu, B. , Hu, C. , Zhu, F. , Liu, X. , Zhang, J. , … Peng, Z. (2020). Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus‐infected pneumonia in Wuhan, China. JAMA, 323(11), 1061–1069. 10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, G. , Zhang, Q. , Yuan, W. , Wu, J. , & Li, C. (2016). Enalapril protects against myocardial ischemia/reperfusion injury in a swine model of cardiac arrest and resuscitation. International Journal of Molecular Medicine, 38(5), 1463–1473. 10.3892/ijmm.2016.2737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, J. , Li, N. , Gao, F. , Song, R. , Zhu, S. , & Geng, Z. (2015). Balance between angiotensin converting enzyme and angiotensin converting enzyme 2 in patients with chronic heart failure. Journal of the Renin‐Angiotensin‐Aldosterone System, 16, 553–558. 10.1177/1470320315576257 [DOI] [PubMed] [Google Scholar]
- Xie, X. , Chen, J. , Wang, X. , Zhang, F. , & Liu, Y. (2006). Age‐ and gender‐related difference of ACE2 expression in rat lung. Life Sciences, 78(19), 2166–2171. 10.1016/j.lfs.2005.09.038 Erratum in: Life Sci 2006 Nov 25;79(26):2499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yazdany, J. , & Kim, A. H. J. (2020). Use of hydroxychloroquine and chloroquine during the COVID‐19 pandemic: What every clinician should know. Annals of Internal Medicine, 172(11), 754–755. 10.7326/M20-1334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan, Y. M. , Luo, L. , Guo, Z. , Yang, M. , Ye, R. S. , & Luo, C. (2015). Activation of renin‐angiotensin‐aldosterone system (RAAS) in the lung of smoking‐induced pulmonary arterial hypertension (PAH) rats. Journal of the Renin‐Angiotensin‐Aldosterone System, 16, 249–253. 10.1177/1470320315576256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, W. , Zhao, Y. , Zhang, F. , Wang, Q. , Li, T. , Liu, Z. , … Zhang, S. (2020). The use of anti‐inflammatory drugs in the treatment of people with severe coronavirus disease 2019 (COVID‐19): The perspectives of clinical immunologists from China. Clinical Immunology, 214, 108393 10.1016/j.clim.2020.108393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao, Y. , Zhao, Z. , Wang, Y. , Zhou, Y. , Ma, Y. , & Zuo, W. (2020). Single‐cell RNA expression profiling of ACE2, the receptor of SARS‐CoV‐2. bioRxiv. 10.1101/2020.01.26.919985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou, F. , Yu, T. , Du, R. , Fan, G. , Liu, Y. , Liu, Z. , … Cao, B. (2020). Clinical course and risk factors for mortality of adult inpatients with COVID‐19 in Wuhan, China: A retrospective cohort study. Lancet, 395(10229), 1054–1062. 10.1016/S0140-6736(20)30566-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou, H. , Fang, Y. , Xu, T. , Ni, W. J. , Shen, A. Z. , & Meng, X. M. (2020). Potential therapeutic targets and promising drugs for combating SARS‐CoV‐2. British Journal of Pharmacology, 177, 3147–3161. 10.1111/bph.15092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou, P. , Yang, X. L. , Wang, X. G. , Hu, B. , Zhang, L. , Zhang, W. , … Shi, Z. L. (2020). A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature, 579(7798), 270–273. 10.1038/s41586-020-2012-7 Epub 2020 Feb 3. PMID: 32015507; PMCID: PMC7095418 [DOI] [PMC free article] [PubMed] [Google Scholar]


