Abstract
High-grade sinonasal carcinomas are a cohort of malignant epithelial neoplasms arising in the sinonasal cavities with distinct, ominous morphologic features or lacking well-differentiated features that might otherwise classify them as less biologically worrisome. Recent advances in molecular profiling have led to the identification of several distinct tumor entities previously grouped together. These molecularly distinct lesions include NUT (midline) carcinoma, INI1 (SMARCB1)-deficient carcinoma, SMARCA4-deficient sinonasal carcinoma, and novel IDH-mutant sinonasal undifferentiated carcinoma, in addition to the previously described lymphoepithelial carcinoma that may also be included in the differential diagnosis. The discovery of these distinct molecular tumor profiles may have significant clinical impact as targeted molecular-based therapeutics continue to evolve, and they may offer some respite for patients who have these highly aggressive cancers.
Sinonasal undifferentiated carcinoma (SNUC) is a rare entity comprising less than 3% of sinonasal malignancies and is estimated at 0.02 cases per 100 000 people.1 The World Health Organization (WHO) Classification of Head and Neck Tumours defines this entity as a highly aggressive undifferentiated carcinoma of the sinonasal cavity, and its diagnosis requires the absence of cell lineage differentiation, such as glandular or squamous features.2 The diagnosis of SNUC is one of exclusion, rendered once all other potential high-grade sinonasal carcinomas have been eliminated as diagnostic candidates. Rational treatment strategies for SNUC continue to be suboptimal, and standard multimodality therapy usually includes a combination of surgery, radiation, and chemotherapy. In fact, chemotherapeutic combinations continue to be inconsistently applied across large tertiary referral centers.2,3 Despite aggressive management, the 2-year survival rates in reported series vary from 25% to 67%.3 The arrival of next-generation sequencing platforms into clinical practice has allowed for further subclassification of tumors previously grouped together. High-grade sinonasal carcinomas, including entities presently and previously categorized as SNUC, are a heterogeneous group of malignancies. Discovery of several unique molecular tumor subsets has opened the door to potential therapeutic targets.4 These targetable molecular subsets include NUT (midline) carcinoma (NMC), INI1 (SMARCB1)–deficient carcinoma, SMARCA4-deficient sinonasal carcinoma, and novel isocitrate dehydrogenase (IDH)-mutant SNUC.5–10
NUT (MIDLINE) CARCINOMA
NUT (midline) carcinoma is a rare, aggressive malignancy that recently appeared in the World Health Organization classification of sinonasal tumors.2 It is characterized as a poorly differentiated carcinoma with frequent squamous differentiation occurring most commonly along the midline axis, especially in the head and neck and the mediastinum.11 Rearrangement of the NUT-BRD4 gene fusion involving t(15;19) chromosomes is detected in approximately 75% of cases.11,12 A minority of NMC cases harboring BRD3-NUT or NUT-variant fusions have also been documented.2,13 It is believed that NUT gene rearrangement could modify chromatin so as to silence the gene expression needed for epithelial differentiation and lead to differentiation arrest.11,13 The result is unregulated growth of undifferentiated neoplastic cells seen histologically as sheetlike growth of poorly differentiated to undifferentiated cells with necrosis and conspicuous mitotic figures (Figure 1, A). The neoplastic cells are commonly immunoreactive for pancytokeratin, p63, and p40.5,13 The diagnosis of NMC requires diffuse, greater than 50%, nuclear labeling with monoclonal antibody targeting NUT mutation (Figure 1, B).2 Despite aggressive multimodality treatment that combines surgery, radiation therapy, and chemotherapy, the prognosis is poor, with an overall median survival of less than 1 year.2,11,13 Recent evidence suggests that targeted treatment with bromodomain (NUT) inhibitors may represent enhanced treatment for patients with NMC.5,14
Figure 1.
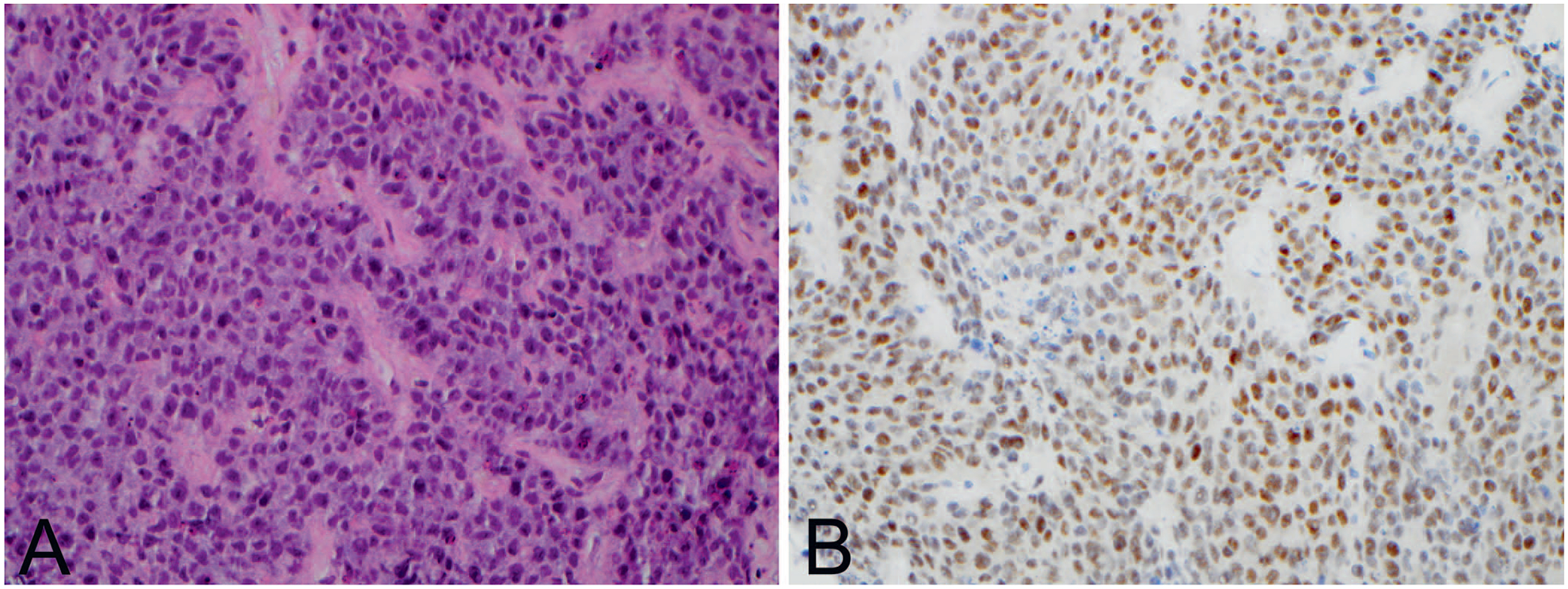
NUT midline carcinoma. A, Tumor is composed of sheets of monomorphic poorly differentiated cells with scattered apoptotic bodies. B, Immunohistochemistry reveals positive nuclear expression with NUT antibody (hematoxylin-eosin, original magnification ×40 [A]; original magnification ×40 [B]).
INI1 (SMARB1)–DEFICIENT SINONASAL CARCINOMA
INI1 (SMARCB1)–deficient sinonasal carcinoma is an uncommon malignancy, accounting for fewer than 60 cases reported in current literature.15,16 These aggressive tumors involve the sinuses, with a predilection for the ethmoid sinus, and occur equally in both sexes, with a mean age of 52 years.8 This carcinoma is characterized by large, deeply infiltrative masses, with an occasional exophytic surface.8 Histologically, lesions are poorly differentiated, monomorphic, basaloid neoplasms, with irregular nuclei and often prominent nucleoli, reminiscent of “round blue cells” (Figure 2, A). Rarely, plasmacytoid and rhabdoid morphologies with eccentrically placed eosinophilic cytoplasm have been reported.8,17 Prominent areas of necrosis and increased mitotic activity are consistently seen. Loss of nuclear expression for INI1 (SMARCB1) antibody remains a diagnostic feature (Figure 2, B).2,16 SMARCB1, located on chromosome 22q11.2, is a member of the switch/sucrose non-fermentable (SWI/SNF) complex and functions as a tumor suppressor gene.18 In its normal state, SMARCB1 plays a role in chromatin remodeling, gene expression, cell proliferation, and differentiation.15,18 SMARCB1 mutation is implicated in the pathogenesis of several malignancies, including atypical teratoid rhabdoid tumor (AT/RT), malignant rhabdoid tumor, epithelioid sarcoma, renal medullary carcinoma, myoepithelial carcinoma, epithelioid malignant peripheral nerve sheath tumor, and extraskeletal myxoid chondrosarcoma.16 Although these diverse neoplasms exhibit divergent clinicopathologic features, they tend to share “rhabdoid” cytomorphology, at least in some cases.16,19 As for other high-grade sinonasal carcinomas, SMARCB1-deficient carcinoma often requires trimodality treatment and, despite aggressive therapy, is associated with a poor prognosis and a mean survival of 22 months.16
Figure 2.
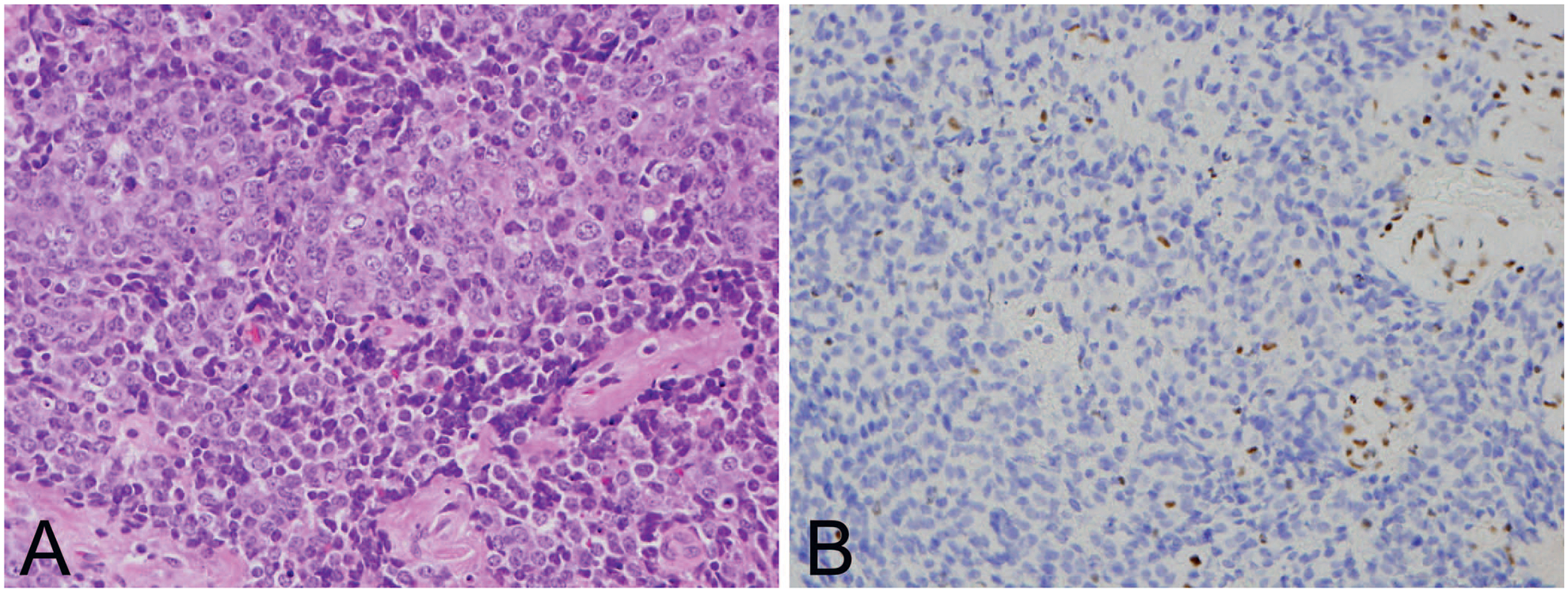
SMARCB1 (INI1)–deficient sinonasal carcinoma. A, The carcinoma has basaloid morphology with hyperchromatic-to-vesicular chromatin and occasional prominent nucleoli. B, Tumor shows complete loss of SMARCB1 by immunohistochemistry (hematoxylin-eosin, original magnification ×40 [A]; original magnification ×40 [B]).
SMARCA4-DEFICIENT SINONASAL CARCINOMA
SMARCA4-deficient sinonasal carcinoma is another rare but distinct entity previously rendered as a SNUC, with only 2 cases reported thus far.7,20 The initial clinical case presented was a 40-year-old woman with a large nasal mass extending into the skull and orbit.7 Histologic assessment revealed a poorly differentiated small-to-intermediate size round blue cell malignancy, with immunoreactivity limited to diffuse expression of pancytokeratin and focal immunoreactivity to neuroendocrine markers.7 Both cases revealed complete nuclear loss of SMARCA4 labeling.7,20 SMARCA4 is a catalytic subunit part of the SWI/SNF complex that includes SMARCB1. The inactivation of SMARCA4 interferes with chromatin remodelling and cell transcription and has been implicated as the sole driver mutation in a subset of small cell carcinomas of the ovary, hypercalcemic type, as well as non–small cell lung carcinoma.18
IDH-MUTANT SNUC
IDH-mutant SNUC is a recently discovered molecular subtype with fewer than 25 reported cases.6,20 Establishing an adequate clinical profile of patients with IDH-mutant SNUC is limited by small cohort sizes. Jo et al20 have reported that patients with IDH-mutated tumors were younger, with a median age of 57 years, whereas those lacking the mutation were older, with a median age of 71 years. Regardless of mutation, most patients receive a diagnosis at an advanced stage, with half revealing neoplastic involvement of multiple sinuses and tumor extension into the orbit and cranial structures. From a pathology standpoint, no morphologic or immunohistochemical differences are observed among both groups, with the exception of cytoplasmic expression of a polyclonal antibody targeting IDH type 1 and IDH type 2 (IDH1/2) R132/ R172 genetic alterations in IDH-mutant SNUC.20 Recent studies have identified mutation of IDH2 along the R172 hotspot, including R172S, R172T, and R172 M.6,20 Although IDH mutation has not previously been documented in the sinonasal cavity, it has been described in other malignancies, such as acute myeloid leukemia, myelodysplastic syndrome, glioma, glioblastoma, melanoma, adenocarcinoma of the lungs and colon, chondrosarcoma, and cholangiocarcinoma.20–22 Because of its identification in several cancers, pathways linking IDH to tumorigenesis are well understood.23 IDH1 and IDH2 encode metabolic enzymes involving the Krebs cycle.21 The IDH1 gene product is in the cytoplasm of the cell, whereas that of IDH2 is in the mitochondria. In their normal state, these enzymes degrade isocitrate into hydroxyglutarate, a nutrient used to generate energy for the cell.23 When mutated, the aberrant enzymatic function of isocitrate dehydrogenase leads to an overproduction of hydroxyglutarate, a potent oncometabolite. This oncometabolite is transported to the cell nucleus, where it causes widespread hypermethylation in gene promoter regions, thus silencing genes involved in cell differentiation. As a consequence, the cells remain in their primitive state and proliferate quickly.21,23 In addition to their defining IDH mutation, several SNUCs harbor concomitant oncogenic alterations along the SOX9, SOX2, PIK3CA, and MTOR pathways. Coexistence of loss-of-function mutation involving TP53, CDKN2A/2B, and RB1, along with MYC amplification, was also documented.6,20 Although the small number of patients precludes comparison of the median survival between mutant and nonmutant SNUCs, altogether the overall median survival is calculated at 23 months.20 Testing for IDH mutation should be considered because these patients might also benefit from targeted IDH inhibitors.6,20,21
LYMPHOEPITHELIAL CARCINOMA
Sinonasal lymphoepithelial carcinoma is a rare tumor with approximately 40 reported cases in the literature.2 Lymphoepithelial carcinoma most commonly affects men in their fifth to seventh decades and frequently arises within the nasal cavity. These tumors are morphologically similar to nonkeratinizing nasopharyngeal undifferentiated carcinomas. To be considered a sinonasal primary, extension from an adjacent nasopharyngeal site must be excluded clinically.24 Lymphoepithelial carcinomas are composed of variably sized nests comprising polygonal- to spindle-shaped cells with large vesicular nuclei often associated with prominent nucleoli and abundant amphophilic to light eosinophilic cytoplasm (Figure 3, A). The neoplastic cells have a syncytial growth pattern and may be obscured by an important nonneoplastic lymphoplasmacytic cell infiltrate present between and around tumor nests.24,25 The tumor cells are immunoreactive for pancytokeratin, cytokeratin 5/6 (Figure 3, B), p63, and p40. More than 90% harbor Epstein-Barr virus, which can easily be detected by Epstein Barr virus–encoded small RNA by in situ hybridization.2,24 With prompt recognition and intense therapeutic management, regardless of the disease stage the 5-year overall survival is estimated at 70% and disease-specific survival at 78%.25
Figure 3.
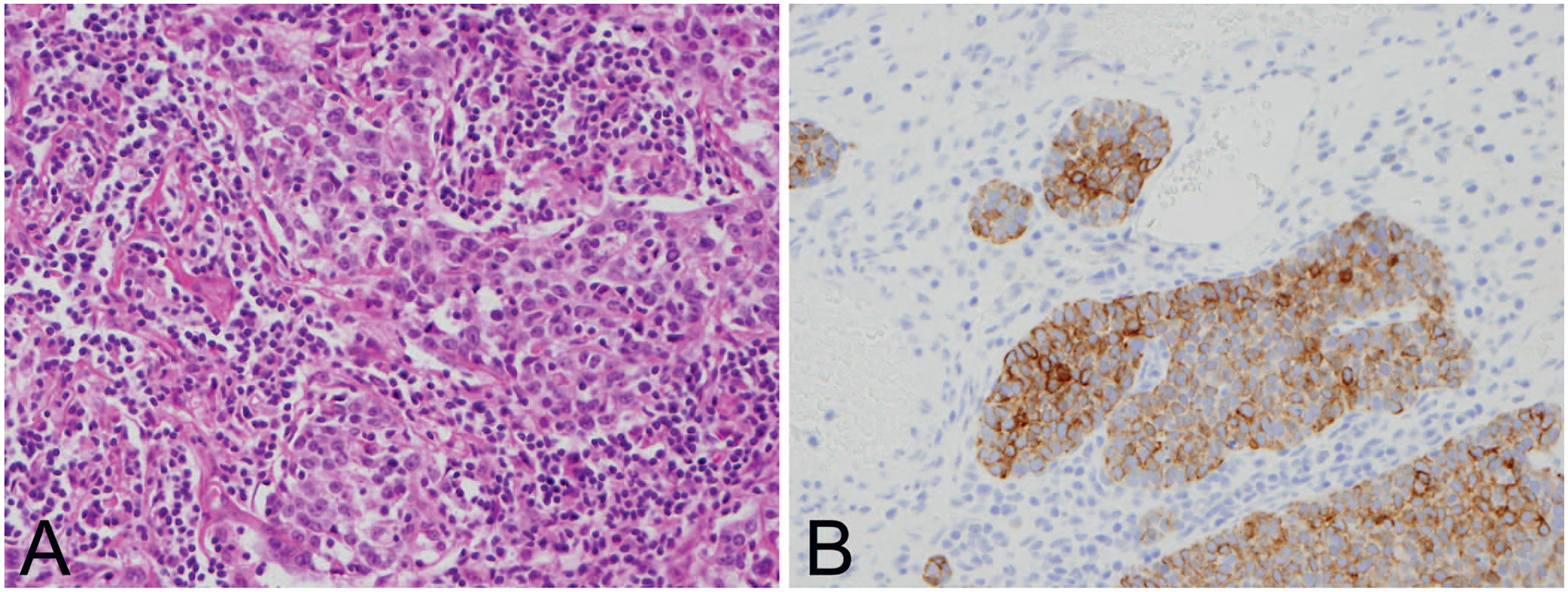
Sinonasal lymphoepithelial carcinoma. A, Tumor nests are composed of syncytial polygonal cells with vesicular nuclei and prominent nucleoli obscured by a nonneoplastic lymphoplasmacytic infiltrate. B, Tumor nests are immunoreactive for cytokeratin 5/6 antibody (hematoxylin-eosin, original magnification ×40 [A]; original magnification ×40 [B]).
CONCLUSIONS
Recent advances in molecular profiling have led to major updates and revision in the classification of high-grade sinonasal carcinomas. The discovery of novel mutations allows for the introduction of several new genetically defined entities, including NMC, SMARCB1-deficient sinonasal carcinoma, SMARCA4-deficient sinonasal carcinoma, and IDH-mutant sinonasal carcinoma. Although most of these tumors are characterized by aggressive biologic behavior, the identification of these mutations could lead to potentially improved targeted therapeutic options and improved overall disease-specific survival.
Acknowledgments
This manuscript was funded by intradepartmental funding at Massachusetts General Hospital.
Footnotes
The authors have no relevant financial interest in the products or companies described in this article.
References
- 1.Llorente JL, López F, Suárez C, Hermsen MA. Sinonasal carcinoma: clinical, pathological, genetic and therapeutic advances. Nat Rev Clin Oncol. 2014;11(8): 460–472. [DOI] [PubMed] [Google Scholar]
- 2.Slootweg P, Chan JKC, Stelow EB, et al. Carcinomas In: El-Naggar AK, Chan JKC, Grandis J, Takata T, Slootweg P, eds. WHO Classification of Head and Neck Tumours. 4th ed. Lyon, France: IARC Press; 2017:14–23. [Google Scholar]
- 3.Gelbard A, Hale KS, Takahashi Y, et al. Molecular profiling of sinonasal undifferentiated carcinoma. Head Neck. 2014;36(1):15–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reiersen DA, Pahilan ME, Devaiah AK. Meta-analysis of treatment outcomes for sinonasal undifferentiated carcinoma. Otolaryngol Head Neck Surg. 2012;147:7–14. [DOI] [PubMed] [Google Scholar]
- 5.Thompson LDR, Franchi A. New tumor entities in the 4th edition of the World Health Organization classification of head and neck tumors: nasal cavity, paranasal sinuses and skull base. Virchows Arch. 2017;475(3):315–330. [DOI] [PubMed] [Google Scholar]
- 6.Dogan S, Chute DJ, Xu B, et al. Frequent IDH2 R172 mutations in undifferentiated and poorly-differentiated sinonasal carcinomas. J Pathol. 2017; 242(4):400–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Agaimy A, Weichert W. SMARCA4-deficient sinonasal carcinoma. Head Neck Pathol. 2017;11(4):541–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Agaimy A, Hartmann A, Antonescu CR, et al. SMARCB1 (INI-1)-deficient sinonasal carcinoma: a series of 39 cases expanding the morphologic and clinicopathologic spectrum of a recently described entity. Am J Surg Pathol. 2017;41(4):458–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bishop JA. Newly described tumor entities in sinonasal tract pathology. Head Neck Pathol. 2016;10(1):23–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bell D, Hanna EY. Sinonasal undifferentiated carcinoma: morphological heterogeneity, diagnosis, management and biological markers. Expert Rev Anticancer Ther. 2013;13(3):285–296. [DOI] [PubMed] [Google Scholar]
- 11.French C NUT midline carcinoma. Nat Rev Cancer. 2014;14(3):149–150. [DOI] [PubMed] [Google Scholar]
- 12.Stelow EB. A review of NUT midline carcinoma. Head Neck Pathol. 2011; 5(1):31–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Edgar M, Caruso AM, Kim E, et al. NUT midline carcinoma of the nasal cavity. Head Neck Pathol. 2017;11(3):389–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.French CA. The importance of diagnosing NUT midline carcinoma. Head Neck Pathol. 2013;7(1):11–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rooper LM, Westra WH. A protein lost, a diagnosis gained: a review of SMARCB1-deficient sinonasal carcinomas. Am J Surg Pathol. 2018;23:13–18. [Google Scholar]
- 16.Bishop JA, Antonescu CR, Westra WH. SMARCB1 (INI-1)-deficient carcinomas of the sinonasal tract. Am J Surg Pathol. 2014;38(9):1282–1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Agaimy A, Koch M, Lell M, et al. SMARCB1(INI1)-deficient sinonasal basaloid carcinoma: a novel member of the expanding family of SMARCB1-deficient neoplasms. Am J Surg Pathol. 2014;38(9):1274–1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barutcu AR, Lajoie BR, Fritz AJ, et al. SMARCA4 regulates gene expression and higher-order chromatin structure in proliferating mammary epithelial cells. Genome Res. 2016;26(9):1188–1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bishop JA. Recently described neoplasms of the sinonasal tract. Semin Diagn Pathol. 2016;33(2):62–70. [DOI] [PubMed] [Google Scholar]
- 20.Jo VY, Chau NG, Hornick JL, et al. Recurrent IDH2 R172X mutations in sinonasal undifferentiated carcinoma. Mod Pathol. 2017;30(5):650–659. [DOI] [PubMed] [Google Scholar]
- 21.Dang L, Yen K, Attar EC. IDH mutations in cancer and progress toward development of targeted therapeutics. Ann Oncol. 2016;27(4):599–608. [DOI] [PubMed] [Google Scholar]
- 22.Dunn GP, Andronesi OC, Cahill DP. From genomics to the clinic: biological and translational insights of mutant IDH1/2 in glioma. Neurosurg Focus. 2013; 34(2):E2–E15. [DOI] [PubMed] [Google Scholar]
- 23.Ye D, Xiong Y, Guan KL. The mechanisms of IDH mutations in tumorigenesis. Cell Res. 2012;22(7):1102–1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jeng YM, Sung MT, Fang CL, et al. Sinonasal undifferentiated carcinoma and nasopharyngeal-type undifferentiated carcinoma: two clinically, biologically, and histopathologically distinct entities. Am J Surg Pathol. 2002;26(3):371–376. [DOI] [PubMed] [Google Scholar]
- 25.Chan J, Wong E, Ng S, et al. Non-nasopharyngeal head and neck lymphoepithelioma-like carcinoma in the United States: a population-based study. Head Neck. 2015;38(suppl 1):E1294–E1300. [DOI] [PubMed] [Google Scholar]


