On December 31, 2019, a cluster of respiratory illness of unknown origin in the Wuhan, Hubei province of China was reported to the World Health Organization (WHO). The causative agent was unknown at that time, but the 44 patients reported in Wuhan had some form of contact with a seafood market. Subsequently, the cause of the pneumonia was identified as a novel coronavirus (2019 novel coronavirus) to which humans had never been exposed. Almost a month after the first report, the outbreak was declared a Public Health Emergency of International Concern.1 The novel coronavirus was renamed SARS-CoV-2 indicating its similarity with the SARS 2003 outbreak, and the disease was named COVID-19.1, 2 As of the time of this writing, a total number of 14,205,282 cases and 599,716 deaths have been reported globally. India, one of the world's most populated countries, engaged in an early rigorous attempt to control the pandemic. Herein, we describe this country's strategy and summarize the challenges encountered due to the size of its population and its fragmented healthcare system.
The first case of coronavirus in India was reported at the end of January in the southern state of India, Kerala.3 The following week, three more active infections were identified in the same state. With the emergence of the virus, the Ministry of Health and Family Welfare (MoHFW) took responsibility for monitoring the spread of the virus. The number of active cases including recovered/discharged patients and deaths were updated with state /district statistics on the MoHFW website on a daily basis. MoHFW designated the Indian Institute of Medical Research (ICMR) and the National Institute of Virology (NIV) (in the state of Maharashtra) for the rapid development of diagnostic and research methodologies to tackle the COVID-19 pandemic. In the following months, more cases surfaced in different parts of the country including Delhi, Mumbai, but most of them were imported with people returning to India from European regions.4 , 5 The threat of a communicable contagion of this degree in a country with inherent high density of population, high burden of communicable diseases like HIV and Tuberculosis, and a relatively weak health care system is unparalleled. Below, we succinctly describe limitations inherent in India's healthcare system followed by a summary of the public health interventions implemented to address the pandemic.
Healthcare system in India
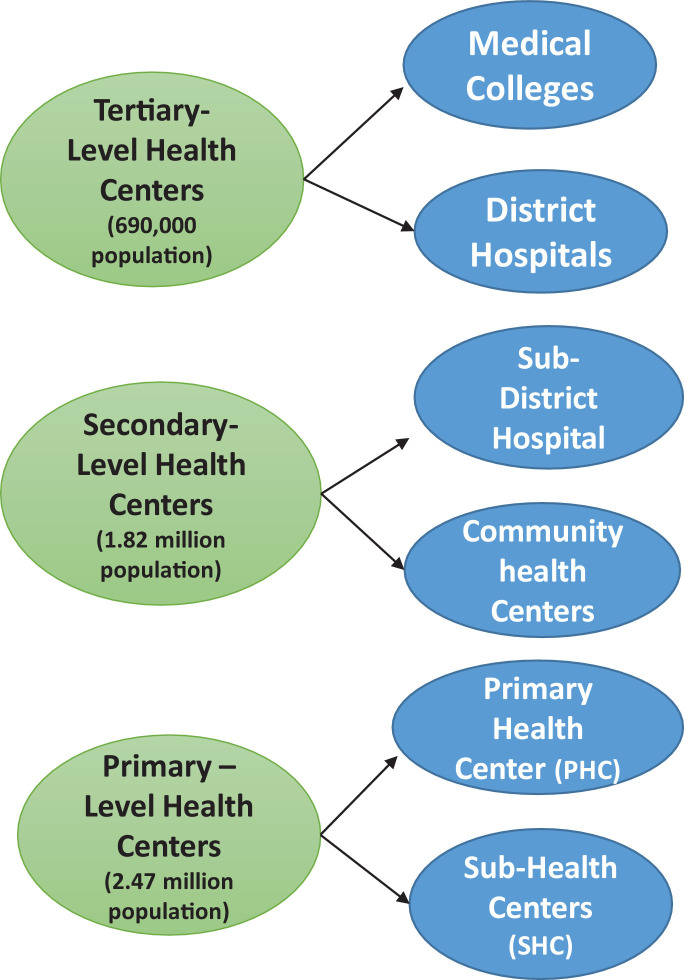
The health care system in India is primarily divided into public (government) and private sectors. Despite widespread urbanization in recent years, 68.84% of the Indian population still lives in rural areas.6 Private sector hospitals are concentrated in urban areas, while there is widespread discrepancy and deficiency in the distribution of healthcare services in rural areas, which are mainly served by the public sector in the form of health care centers (Fig. 1 ). The number of health care centers are often limited and lack adequate resources.7 In urban areas, both private and public healthcare systems are available, but there is mistrust in public hospitals, as they often lack advanced diagnostics and sophisticated treatment options, and in private hospitals because of exorbitant medical expenses and occasional inappropriate medical treatments provided. Adding additional complexity is the presence of alternative forms of medicine like Ayurveda, Homeopathy and Siddha with varying degrees of beliefs among the people.
Figure 1.
India's three tier health care system. Numbers represent population covered per center.7
The fragmentation of the health care system and the presence of numerous alternate medicinal practices have long caused a sense of confusion and mistrust on the different health care delivery systems and doctors. To address this, there have been attempts in recent years for comprehensive strengthening of the system by expanding collaborations between the public and private sectors; by accrediting public health centers (Primary Health Centers), private hospitals and laboratories; and by increasing access to health care across regional and socioeconomic boundaries.8 Despite these efforts, India's multi-tiered fragmented healthcare system hampered the public health measures implemented to “flatten the curve” and did not contain the spread of the virus in this country.
Public health interventions triggered by the pandemic
With the emergence of the contagion at the end of January, it was not until mid-March that awareness about the virus gained momentum. Public health interventions focused on massive awareness generation including the implementation of strict social distancing norms, updating clinical guidelines for state governments and local authorities, mobilization of appropriate resources from the private sector, and the implementation of the most severe form of movement restriction (national lockdown).
Awareness materials about “Do's and Don'ts” were posted in all regional languages on the MoHFW website (mohfw.gov.in). The materials included posters about social distancing, hand washing, and cough etiquette. This was followed by the widespread dissemination of information through all forms of media. The efforts were tiered at national, state, and district levels. MoHFW coordinated the awareness efforts at the national level and oversaw the uniform implementation of guidelines at the level of the states, which were held responsible for overseeing the dissemination of information for the containment of disease at regional/district levels. Notably, all cellular networks in the country contained a “coronavirus awareness ring tone” that plays each time the owner receives a call. This ring tone explains cough etiquette, reiterates symptoms of COVID-19, lists the helpline number to seek medical attention, and warns against the discrimination of health care workers and patients infected with SARS-CoV-2.
Not surprisingly, social media and other information outlets were loaded early on with false information including support for unproven therapies by homeopathy doctors and others (e.g., using urine from cows as remedy, consuming excessive ethyl alcohol as cure, drinking ginger tea and eating raw garlic in the morning as cure, eating Indian gooseberry (rich in vitamin C) as cure, chanting holy “slokas” and lighting lamps to protect from the virus). To address this, the government issued regulations with penalties for the spread of false information, and the MoHFW website incorporated blogs and materials to address “fact checks and myth busters.” To promote communication and answer queries promptly, the government introduced the @CovidIndiaSeva platform on Twitter. Meanwhile, the gram panchayats (local authorities in villages) were empowered to spread awareness in remote villages.
Travel advisories and quarantine during the pandemic
The Aviation Ministry of India issued travel advisories and imposed travel restrictions in January. Entry screenings with self-declaration forms were initiated for all travelers returning from China. The screening process was expanded in February to include Thailand, South Korea, Japan, Hong Kong, Indonesia, Malaysia and Vietnam, among other countries. With Italy and Republic of Korea becoming hot spots in the world, the government of India issued a requirement for a COVID-19 negative certificate for all travelers returning from these countries.9 The implementation of this mandatory clause caused chaos among Indians returning home. Soon after the WHO declared COVID-19 a pandemic, several visa restrictions were introduced by the Indian government. Passengers with travel history were monitored for 14 days upon arrival to the country either at home or in quarantine facilities depending on the presence of symptoms or history of high-risk exposures. Later travel restrictions were expanded with the closure of border checkpoints of neighboring countries including Nepal, Bangladesh, Myanmar and Bhutan.9 Eventually, India closed its borders on March 25, 2020.
Social distancing and national lockdown
In comparison to countries like Italy, United Kingdom, and the United States, India was very quick to implement strict social distancing policies. With only 360 active cases in the whole country at the end of March, a nationwide curfew was imposed to prevent the local transmission of the virus. The “Janata Curfew” was implemented by Prime Minister Narendra Modi to draw public attention (and public involvement) in what was called the “War Against Coronavirus”. Under Disaster Management Act 2005, the Prime Minister implemented the world's largest lockdown for 21 days (Table 1 ) grounding all international and domestic flights as well as interstate and intrastate travel. All forms of public transportation (mainly buses and railways) were halted. Only essential travel for provisions provided by hospitals, pharmacies, and grocery shops were allowed to remain open. Police officials closely monitored adherence to the rules with several thousand people booked under law, and vehicles seized for violating lockdown orders. Social distancing practices including facemasks were implemented in grocery shops, gas stations, banks, and hospitals. Various methodologies including group tracing via apps and drone surveillance continue to be employed to ensure adherence to social distancing. Despite these interventions, the infection continued to increase and the first lockdown failed to “flatten the curve”. The national lockdown was later extended in view of the number of cases increasing beyond 10,000. This was termed as “Lockdown 2.0″, which further underwent two more extensions (Table 1).
TABLE 1.
Evolution from “Lockdown 1 to Lockdown 5”.
| Feb 2020 – Introducing travel ban and mandatory quarantine for specific international travelers |
| March 25, 2020 – Lockdown 1, National lockdown for 21 days was implemented by the Indian Prime minister and India closed its borders |
| April 14, 2020 – Lockdown 2, Extension of strict national lockdown |
| May 4, 2020 – Lockdown 3, Extension of strict national lockdown for 15 days |
| May 18, 2020 – Lockdown 4, Extension of lockdown for most metropolitan cities, red and orange zones with phased reopening plans for green zones |
| June 1, 2020 – Lockdown 5/Unlock 1, Extension of lockdown for 30 days with phased reopening plans in certain states |
| July – August 2020 - Unlock 3 and Unlock 4, Phased reopening with plans to open schools and colleges |
In a country were interstate migration is ubiquitous and migrant workers make up the majority of the workforce in urban cities, the implementation of the national lockdown left millions of migrant workers stranded in different parts of the nation with no means of transportation to reach hometowns. As a result, millions of migrant workers started walking over 100 miles by foot, deprived of adequate water and food supplies, to reach their families. The plight of migrant workers drew widespread criticism and a month after the lockdown was initiated, special arrangements were made to transport migrants back home. The Indian Railways began operating special trains called the “Shramik trains” to ferry stranded migrants. By the third week of May, around 1600 “Shramik trains” were transporting more than 2 million migrant workers. All migrant workers returning home were required to undergo mandatory health screening and 14-day quarantine at designated quarantine centers.
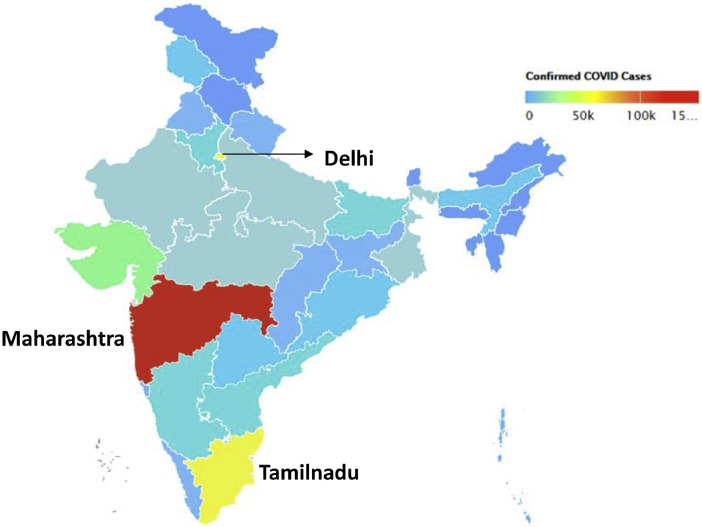
In the end, and despite the series of lockdowns, the number of active infections continued to increase with more than 410,461 cases and 15,413 deaths in mid-June. Hospitals and health care workers became stretched to a breaking point, especially in major hot spots like Maharashtra and Tamil Nadu. Figure 2, Figure 3 demonstrate the extent and hotspots of coronavirus in India.
Figure 2.
Map of India and confirmed cases. The image depicts the State of Maharashtra as the most affected (red) followed by the State of Tamil Nadu and Delhi (yellow).19
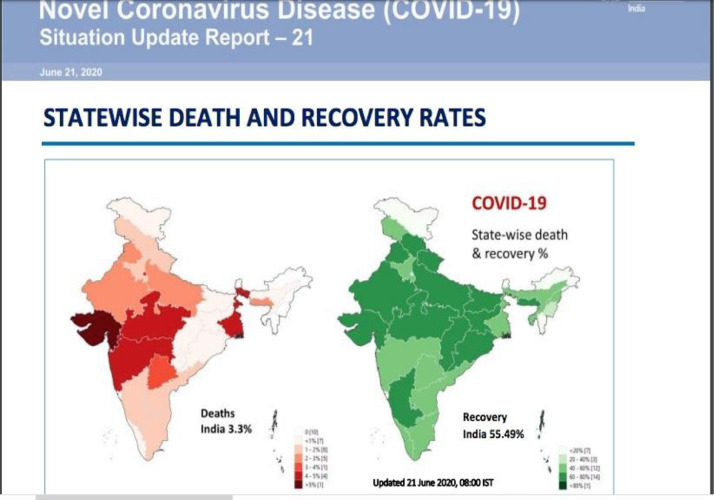
Figure 3.
COVID-19 deaths and recovery rates. Data based on WHO India Situation report 21, June 21, 2020.3,17
Testing and contact tracing
In January, the only laboratory in India authorized and equipped to test for COVID-19 was the National Institute of Virology (NIV) located in Pune, Maharashtra. However, the testing capacity in India expanded with the number of government laboratories authorized for conducting Real time PCR/ TrueNat /CBNAAT for COVID-19 increasing to 298 by the end of April. In addition to government laboratories, there are at least 99 private laboratories functional for testing across the country. By the end of June, 215,446 tests were being conducted daily, and a total of 7,776,228 samples had been tested since the start of the pandemic. Although this increase in testing capacity is commendable, it fell short for a population of 1.3 billion. Hence, the true spread of the infection is considered to remain grossly underestimated.
It is notable that ICMR and MoFHW maintained that there is no community transmission of SARS-CoV-2 in India. Persons affected either had travel history or local transmission secondary to high risk contact exposure.10 Hence, ICMR consistently stated that individuals did not need testing, but COVID-19 testing was and is being offered free of cost to all individuals who meet the following specific testing criteria11: a) all individuals with history of travel within last two weeks who are symptomatic, b) all patients with contact to confirmed cases exhibiting symptoms, c) all healthcare workers providing for COVID-19 patients who exhibit symptoms, d) asymptomatic contacts with confirmed cases to be tested once between 5 and 14 days, and e) all patients admitted with fevers, cough, and with or without shortness of breath. In clusters, containment zones, hot spots, and evacuation centers, recommendations urged for testing of all symptomatic individuals within 7 days with real time-PCR and re-tested after 7 days.
As an effort to improve contact tracing, tracking, and empowering individuals, India introduced a mobile application called “Aarogya Setu”. Amenable to be downloaded in the majority of cellphones, this app helps individuals become aware of personal risk of infection and prevalence of COVID-19 in their vicinity. India has advised every individual to download the application. Similarly, all operational offices mandated its employees to download the application. It is currently unclear as to how the healthcare associated data (e.g., presence of Diabetes Mellitus, Hypertension and other risk factors) included in the application will be utilized in the future, and privacy concerns have been raised.
Containment zones
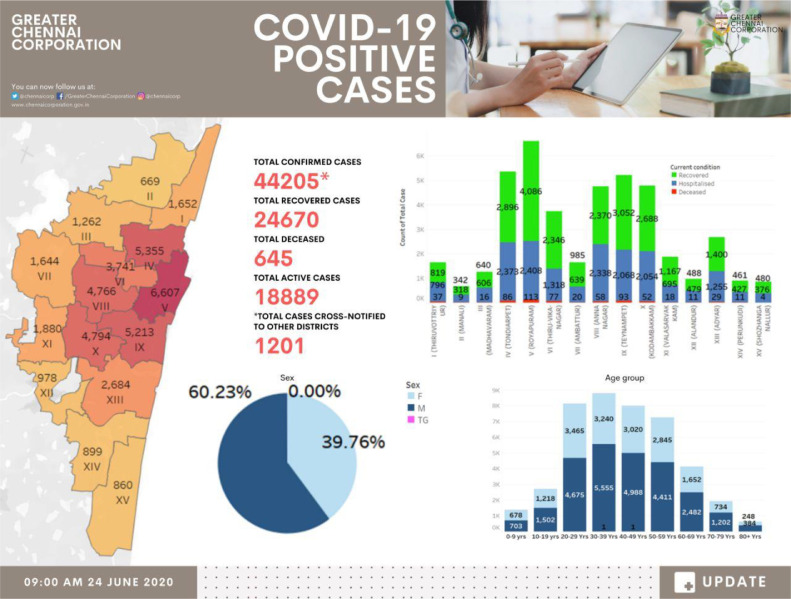
India has witnessed clusters of infections after mass gatherings, including religious gatherings and largescale open vegetable markets. Strategic planning to contain the spread of the virus led to the formation of “red, orange and green zones” and the development of containment plans. The zones are identified based on new cases, caseload, and doubling rates. Most of the large metropolitan cities, including Delhi, Mumbai, Calcutta, Chennai, and Ahmedabad, have been classified as red zones (defined as areas that contribute to 80% of the caseload of the state and with a doubling time of less than four days) (Table 2 ). This zone demarcation defined a major exit strategy out of the lockdown, where each state is expected to convert all red zones to orange and then to green zones. Fig. 4 demonstrates the various zones in the major metropolitan city Chennai.
TABLE 2.
Zones classification.
| Zones | Definition |
|---|---|
| Red zones | Areas that contribute to 80% of the caseload of the state and with a doubling time of less than 4 days. |
| Orange zones | No new cases in the last 14 days. |
| Green zones | No new cases in the prior 28 days |
Figure 4.
COVID-19 positive cases. Red and Orange zones in Chennai. Note that there are no Green zones in the major metropolitan city of Chennai.18
The initial containment plan emphasized the rapid identification of cases and clusters. A rapid response team was assigned by the government and deployed to the areas affected to identify the epicenter (first case or cluster identified), map all possible contacts, and outline a geographical border for all possible contacts, hence forming a containment zone and a buffer zone.12 The containment area usually involves a closed residential colony/school district with a buffer zone of 5 km. The entire process is time sensitive and ideally required to be completed within 12–24 h. Designated health officers and social workers were assigned for aggressive contact tracing and surveillance. Severe movement restrictions were imposed on containment zones for 14 days with no entry of non-essential services/personnel into the area. All identified contacts were quarantined for 14 days and tested, per the testing guidelines mentioned above.
Social and potential long-term health impact
The awareness created about the contagion has caused a sense of panic and anxiety amongst people of all geographic and socioeconomic status in India. The stigma associated with the virus caused widespread isolation in a discriminatory manner, especially when quarantined personnel were required to be marked by stamps on their hands. Doctors and other health care personnel were isolated and subjected to physical and/or emotional abuse to the extent of opposition to cremation in case of death. Few notable incidents include a mob throwing stones attacking and injuring two female doctors who were contact tracing in a village in Indore, located in the central part of India. In another incident, patients under quarantine were found walking naked and verbally assaulting (and spitting on) female doctors.13 Reports of doctors being verbally and physically abused to vacate from the residences became rampant. Although discrimination against health care professionals has been prevalent in India, it surfaced more prominently during the pandemic. The increasing incidents of violence and discrimination against health care professionals led the Indian government to declare any act of such degree a criminal and punishable offense, and through the “Epidemic Diseases (Amendment) Ordinance, 2020″, it solidified the definition of violence against healthcare professionals, while making it an offense for which no bail is allowed.14
In addition to the above, COVID-19 isolation has caused a widespread decrease in people seeking essential health services due to concerns for contracting the virus in health centers. The stigma associated with “fever” and the lack of transportation have also been major barriers in seeking essential health care. Reduced prenatal care and childhood immunizations are particularly concerning. The exact impact of the COVID-19 pandemic on childhood immunizations is currently unknown with WHO & UNICEF estimating around 117 million children being affected by lack of immunization against measles. India harbors the largest children population in the world and has low immunization rates of ~54% at 12 months of age. The National Family Health Survey-4 (2015–2016) reported that the Under Five Mortality Rate (U-5MR) in India is 50 deaths per 1000 live births, and emphasized the paramount importance of immunizations in reducing preventable causes of childhood death like pneumonia and meningitis.15 Hence, any delay or disruption in immunization amidst the pandemic can have disastrous effects. Another vulnerable population is women, especially during pregnancy with regards to prenatal care/immunization and institutional deliveries. Even though the public is encouraged to pursue essential health services and vaccinations during pregnancy, there is no denying that lack of transportation, loss of pay, poverty, and the above-mentioned barriers amidst the pandemic have caused major disruption in delivering standard prenatal care. It is likely that patients suffering from chronic conditions and cancer, and those pending elective surgical procedures have been equally affected.
Current state of affairs
Over the last five months, the capacity for triaging and treating suspected and confirmed COVID-19 cases in India has expanded to include a total of 2033 dedicated COVID facilities with over 19,000 isolation beds, over 24,000 ICU beds, and over 12,000 ventilators.16 Seven months after the appearance of the virus, India opened the largest COVID facility in the country, “The Sardar Patel COVID Care centre”, with a bed capacity of 10,000 located in New Delhi. However, as of this writing, India is only one of three countries (with the U.S. and Brazil) with over 1 million cases. Some would consider this a relatively low case rate compared to its population of 1.3 billion. In fact, many health experts across the nation have claimed that the national lockdown and early interventions promoting dissemination of information and social distancing slowed the doubling rate and delayed the peak of the virus. It is also possible that the relatively low number of cases in India is partially due to the number of tests being conducted, which is significantly lower when compared to other countries like the United Kingdom, Italy, Germany, and the United States. It is important to note that, even with the implementation of more than four months of a strict national lockdown and the public health measures described above, the cases in India continue to rise and a clear path to exit the lockdown remains uncertain. Even though many states are proposing widespread testing to create a safe exit from the lockdown, while some even propose to extend the lockdown further, widespread confusion remains. To complicate the affairs, the pandemic has resulted in a tremendous economic crisis affecting millions of daily wageworkers, migrant workers, and small businesses across nation, with more than 100 million people having lost their jobs in the month of April. Not surprisingly, the previously highlighted concerns for discrimination and healthcare disparities faced by migrants and the poor remain. Like many other nations, India is attempting to safely exit from the lockdown, while saving lives, yet a clear exit path from the lockdown continues to be debated.
Final word
There are many aspects of India's response to the pandemic that are similar to the responses of other countries. Differences include the early and extended implementation of a national lockdown, rather than few travel restrictions, and the strict national policies developed to contain the advance of the virus. Whether these early interventions effectively helped curtail the spread of the virus is debatable, but they were undoubtedly hampered by challenges unique to India including its large population (with a sizeable migrant population), large geography, overcrowded cities, undereducated rural population, poverty, it's fragmented and often mistrusted healthcare system, and the relatively common occurrence of discrimination and even violence against healthcare workers. Addressing such challenges in a country already affected by suboptimal vaccination rates, chronic illnesses, and high prevalence of HIV and tuberculosis seems daunting. Nevertheless, despite the many unknowns about the virus, the accompanying economic downturn, and difficulties inherent in quantifying the impact of the pandemic on the psyche of the population, the country is expected to overcome this crisis. Only time will tell if India will take advantage of current events and turn the challenge into an opportunity to improve health literacy, decrease health disparities, and create the infrastructure needed to combat the next pandemic.
Many countries around the globe, including the United States, share challenges that have delayed and continue to hamper progress against the pandemic including rampant misinformation, missteps in the implementation of early testing strategies, ineffective travel advisories, unfocused messaging, premature ‘re-openings’, and ineffective leadership remain challenges to overcome. As observed in India, the pandemic has yet again shed a light onto healthcare disparities with predominant effects in the elderly and among minorities. It is the impression of the authors that these challenges can be best overcome by world leaders coming together to formulate effective healthcare and socioeconomic support systems for all.
Note by the authors: MV-S was born in Chennai, Tamil Nadu, India, where her family resides and where she spent most of the pandemic due to travel restrictions.
References
- 1.World Health Organization. Coronavirus (COVID-19) events as they happen. 2020. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen. Accessed August 30, 2020.
- 2.World Health Organization. Global Surveillance for human infection with coronavirus disease (COVID-19). Interim Guidance, (February), 27-29. 2020. Available at: https://www.who.int/publications-detail/global-surveillance-for-human-infection-with-novel-coronavirus-(2019-ncov). Accessed August 30, 2020.
- 3.World Health Organization. Naming the coronavirus (COVID-19) and the virus that causes it. 2020. Available at:https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it. Accessed August 30, 2020.
- 4.Asia, S. World health organization. (2020). India Situation, (May), 10–11. 2020. Available at: https://www.who.int/india/emergencies/india-situation-report. Accessed August 30, 2020.
- 5.Sarkale P., Patil S., Yadav P.D., et al. First isolation of SARS-CoV-2 from clinical samples in India. Indian J Med Res. 2020;151:244–250. doi: 10.4103/ijmr.IJMR_1029_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Census of India: provisional population totals India: paper1: census 2011. 2020. Available at: https://censusindia.gov.in/2011-prov-results/prov_results_paper1_india.html. Accessed August 30, 2020.
- 7.Chokshi M., Patil B., Khanna R., et al. Health systems in India. J Perinatol. 2016;36:S9–12. doi: 10.1038/jp.2016.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mossialos E., Wenzl M., Osborn R., Sarnak D. 2015 International profiles health care systems. Commonw Fund. 2016 doi: 10.1056/nejmp1410790. [DOI] [Google Scholar]
- 9.WHO. India Situation Report. 2020. Available at: https://www.who.int/docs/default-source/wrindia/situation-report/india-situation-report-7.pdf?sfvrsn=cf4a7312_2. Accessed August 30, 2020.
- 10.MOHFW. ICMR testing strategy for COVID-19 tetsing in India. 2020. Available at: https://www.mohfw.gov.in/pdf/ICMRstrategyforCOVID19testinginIndia.pdf. Accessed August 30, 2020.
- 11.MOHFW. ICMR strategy for COVID19 testing in India(Version 3, Dated 03/20/2020). 2020. Available at: https://www.mohfw.gov.in/pdf/ICMRrevisedtestingstrategyforCOVID.pdf. Accessed August 30, 2020.
- 12.MoHFW. Containment plan: novel coronavirus disease 2019, ministry of health & family welfare, government of India (pp. 1–18). 2020. Available at: https://ncdc.gov.in/showfile.php?lid=528https://www.mohfw.gov.in/pdf/Containmentplan16052020.pdf. Accessed August 30, 2020.
- 13.Pandey V. Coronavirus: India doctors “spat at and attacked”. BBC NEWS. 2020 https://www.bbc.com/news/world-asia-india-52151141 Available at: [Google Scholar]
- 14.Ministry of Law and Justice, the epidemic diseases (amendment) ordinance, 2020. Ministry of law and justice, the epidemic diseases (amendment) ordinance, 2020, New Delhi, the 22nd April 2020/Vaisakha 2, 1942 (Saka). Available at: http://egazette.nic.in/WriteReadData/2020/219108.pdf. Accessed August 30, 2020.
- 15.International Institute for Population Sciences - IIPS/India and ICF . IIPS and ICF; Mumbai, India: 2017. India National Family Health Survey NFHS-4 2015-16.http://dhsprogram.com/pubs/pdf/FR339/FR339.pdf Available at. [Google Scholar]
- 16.WHO. World health organization, MoFHW. India Situation Report-13; 2020. Available at: https://www.who.int/docs/default-source/wrindia/situation-report/india-situation-report-13.pdf?sfvrsn=a8bb461c_2. Accessed August 30, 2020.
- 17.WHO. World Health Organization, MoFHW. India Situation Report-21. 2020. Available at:https://www.who.int/docs/default-source/wrindia/situation-report/india-situation-report-21.pdf?sfvrsn=f96effa5_2. Accessed August 30, 2020.
- 18.Greater Chennai Corporation Coronavirus Disease (COVID-19). 2020. Available at: https://twitter.com/chennaicorp/status/1275639817011855361/photo/1. Accessed August 30, 2020.
- 19.COVID-19 Tracker Updates For India For State Wise & District Wise Data; 2020. Available at: https://covidindia.org/#. Accessed August 30, 2020.