Abstract
-
➤
Hip joint capsular ligaments (iliofemoral, ischiofemoral, and pubofemoral) play a predominant role in functional mobility and joint stability.
-
➤
The zona orbicularis resists joint distraction (during neutral positions), and its aperture mechanism stabilizes the hip from adverse edge-loading (during extreme hip flexion-extension).
-
➤
To preserve joint function and stability, it is important to minimize capsulotomy size and avoid disrupting the zona orbicularis, preserve the femoral head size and neck length, and only repair when or as necessary without altering capsular tensions.
-
➤
It is not fully understood what the role of capsular tightness is in patients who have cam femoroacetabular impingement and if partial capsular release could be beneficial and/or therapeutic.
-
➤
During arthroplasty surgery, a femoral head implant that is nearly equivalent to the native head size with an optimal neck-length offset can optimize capsular tension and decrease dislocation risk where an intact posterior hip capsule plays a critical role in maintaining hip stability.
Hip joint capsular ligaments serve a fundamental role in balancing functional mobility and joint stability. Although the anatomy of hip capsular ligaments has been well described in the literature1-4, the knowledge of its characteristics and contributions toward hip mechanics and disease processes are evolving. More importantly, how the hip capsule is managed during surgical interventions (preservation and arthroplasty) and its effects on joint function are increasingly recognized5-8. Several recent laboratory studies have provided new insights into functional mobility and stability of the hip joint that should be carefully considered during surgery9-20. The purpose of this review was to provide a comprehensive summary of the functional anatomy and material characteristics of the hip capsule and the effects of different capsular management techniques during arthroscopic and arthroplasty procedures on joint function.
Characteristics
Anatomy
Human ligaments consist of predominantly type-I collagen (85%) and combinations of type III, V, VI, XI, and XIV (15%)21,22. Within the hip joint, higher ratios of type-III collagen in the ligamentous capsule are associated with hip instability23,24, whereas elevated levels in the cartilage are associated with progressive joint degeneration25,26. The hip joint itself is reinforced by 3 primary fibrous capsular ligaments (iliofemoral, ischiofemoral, and pubofemoral), and each serves distinct functional roles to stabilize the joint5,8. The iliofemoral ligament is composed of lateral (superior) and medial (inferior) fibrous branches, which insert together into the anterior inferior iliac spine of the pelvis, each extending out to attach along the femoral intertrochanteric line, forming the inverted Y-shaped ligament of Bigelow (Fig. 1), to reinforce the capsule during external rotation and extension. The ischiofemoral ligament inserts in the ischium, posteroinferior to the acetabular rim, and attaches to the posterior intertrochanteric line to reinforce the capsule during internal rotation in neutral positions as well as in combined flexion-adduction positions (i.e., FADIR [flexion, adduction, and internal rotation]). The pubofemoral ligament inserts in the superior pubic ramus and converges with the medial iliofemoral and inferior ischiofemoral ligaments to insert into the femur7, reinforcing the inferior capsule to restrict excessive abduction and external rotation during hip extension. Another important structure is the triangular-shaped ligamentum teres, which reinforces between the peripheral inferior acetabular notch and the fovea of the femoral head (Fig. 2). As a small auxiliary ligament overlying the fat pad, the ligamentum teres provides a conduit for small vessels and innervations to the femoral head and plays a critical role in proprioception and structural stability27-32, which may decrease in function with progressive age33. In addition to the longitudinal fibers of the primary capsular ligaments, the circular fibers of the zona orbicularis form a stability-inducing collar, which closes around the femoral neck much like an aperture mechanism. During hip extension, the posteroinferior aspect of the zona orbicularis overlaps to medialize and secure the head anteriorly, while during deep flexion, the anteroinferior aspect of the zona orbicularis medializes and secures the head posteriorly (Fig. 2). It has also been proposed that the zona orbicularis has a role in circulating synovial fluid between the central and peripheral compartments within the capsule2.
Fig. 1.
Anatomy of the capsular ligaments illustrated with a left-sided hip model in neutral position (Fig. 1-A) and showing the anterior view of a cadaveric hip specimen in external rotation (Fig. 1-B) and the posterior view of a cadaveric hip specimen in internal rotation (Fig. 1-C). The lateral and medial branches of the iliofemoral ligament (ILFL), pubofemoral ligament (PBFL), superior and inferior fibers of the ischiofemoral ligament (ISFL), anterior superior iliac spine (ASIS), anterior inferior iliac spine (AIIS), pubis (PB), and greater and lesser trochanters (GTroch and LTroch) are indicated. SUP = superior, ANT = anterior, and LAT = lateral.
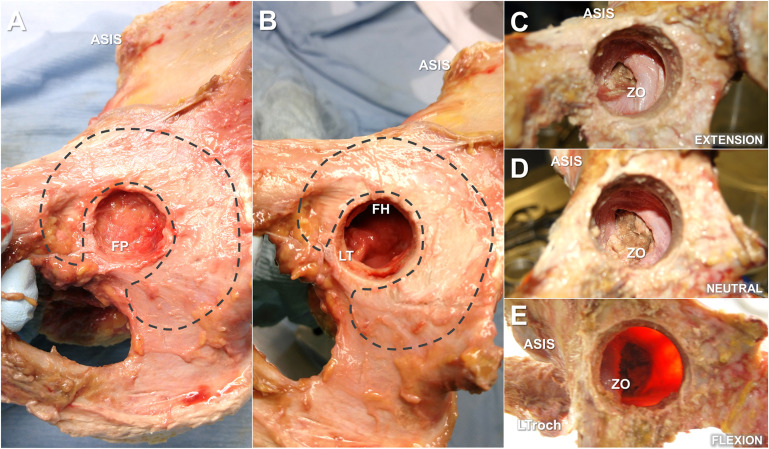
Fig. 2.
Medial-to-lateral view of a right-sided cadaveric hip specimen through progressive portal sizes and depths of the cotyloid fossa and acetabulum, indicating the small portal view of the fat pad (FP), cushioning the innervations and proprioceptors (Fig. 2-A); ligamentum teres (LT) tethering the femoral head (FH) at the fovea pit (with the fat pad removed) (Fig. 2-B); large portal view of the tightened posterior collar of the zona orbicularis (ZO) during hip extension (with ligamentum teres, acetabulum, and femoral head removed) (Fig. 2-C); relaxed ZO during neutral position (Fig. 2-D); and tightened anterior collar of the ZO during deep hip flexion (Fig. 2-E). The acetabular cartilage (dashed lines), anterior superior iliac spine (ASIS), and lesser trochanter (LTroch) are indicated for reference.
Properties
Earlier uniaxial tensile studies of cadaveric hip joint specimens showed that the proximal iliofemoral ligament was larger in cross-sectional area and stiffer than the posterior capsule1,34. This finding emphasizes that the anterior capsule is stronger than the posterior region35, where perhaps the material properties of the iliofemoral ligament may be dependent on age-related changes36.
In addition to mechanical responses, tissue dimensions of capsular ligaments (i.e., thickness and length) can also adapt with progressive arthritis, which can further result in larger cross-sectional areas and tighter capsular ligaments37-39. Since the previous material characteristics were from excised capsules of cadaveric hips without pathology, more imaging modalities evolved to quantify the capsular thickness of hips with pathology using magnetic resonance imaging (MRI)38-40. Weidner et al., in 2012, reviewed imaging data of patients with either symptomatic cam, pincer, or mixed femoroacetabular impingement (FAI) and noted that the anterosuperior capsule (i.e., iliofemoral ligament) was the thickest region (6 mm compared with nonpathological thicknesses of 3.5 to 4.2 mm), and further noted that the zona orbicularis was more prominent in the posterior region, where the capsule was thinner and longer39. Interestingly, as the patients were imaged in a supine position, the thicker regions of the capsule corresponded to shorter capsule lengths, which may explain anterior hip tightness and pain. In terms of functional stability, it further suggests that the aperture mechanism of the zona orbicularis concentrically gathers these posterior thin fibers to create the stability-inducing collar during extreme hip motions. More recently, the MRI study by Rakhra et al. further compared 3 groups: hips with cam FAI, hips with chondrolabral pathology, and healthy control hips38. They indicated that the capsule thickness of the cam FAI group was similar to the chondrolabral pathology group. More importantly, the capsules in both pathological groups (i.e., cam FAI and diseased hips) were thicker (mean [and standard deviation], 6.8 ± 1.6 mm) than the controls (mean, 5.3 ± 2.3 mm; p = 0.026), specifically in the superior regions of the capsule. There was no correlation between alpha angle (i.e., asphericity of cam morphology) and capsule thickness. The implications of capsular dimensions and mechanical properties can help to diagnose the disease process and predict symptoms prior to degeneration. Yet, the previous studies that examined pathological cohorts did not associate capsular dimensions with stiffness41, which could serve as functional biomarkers of hip instability and the degenerative process. It is important to note that the imaging observations were not performed under joint-loading conditions, and earlier mechanical testing was limited to uniaxial tensile testing.
Contributions to Joint Stability
To see how each capsular ligament can reinforce stability and protect the joint from edge-loading, several studies since have devised testing methods to examine the capsule within the hip joint assembly8,30,42-44 (Fig. 3; see Appendix Table I). The first set of tests by Martin et al. analyzed individual contributions of the capsular ligaments by performing stepwise resections8. The analysis provided insights into which ligament was responsible for individual rotational restraints, when release of the lateral (superior) arm of the iliofemoral ligament greatly increased external rotation in flexion and neutral positions, as well as internal rotation in extension. In a similar stepwise resection study, van Arkel et al. devised a custom joint tester and confirmed that the lateral iliofemoral ligament provided predominant external rotational restraint, whereas the pubofemoral ligament restrained external rotation and abduction during hip extension43. In similar studies, the labrum and the ligamentum teres acted as secondary restraints in wider external rotations30-32,42,43, whereas the structures of the capsule, labrum, and zona orbicularis were crucial for rotational and distraction stability16,45. These investigations examined hips without pathology from older donors, but were among the first laboratory studies to collectively provide important clinical insights as to which ligaments were responsible for rotational stability and which to potentially release or avoid during surgery. Finally, the role of the iliocapsularis muscle, which overlies the iliofemoral ligament, cannot be underestimated as it is an important contributor to hip stability, especially in dysplastic hips46,47.
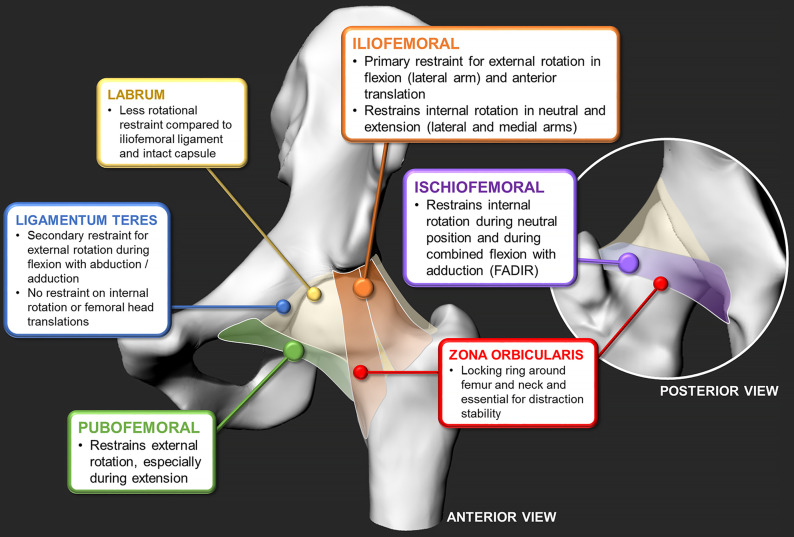
Fig. 3.
The findings of in vitro cadaveric studies on individual capsular ligament contributions to joint stability, outlining iliofemoral, ischiofemoral, and pubofemoral ligaments4,93,44; the zona orbicularis45; ligamentum teres20,94; and labrum93,94. (For a detailed summary for each study’s scope, methods, and observations, see Appendix Table I.)
Surgical Management
Hip Preservation Capsulotomy and Repair
With increasing laboratory evidence, the authors of several studies set off to better understand the mechanical effects of various capsulotomy types, portal sizes, repair strategies, and capsular defects on hip stability (Fig. 4; see Appendix Table II). Several in vitro studies examined conventional interportal-only9,12,14 and T-shaped10,15,18 capsulotomies, with all showing the substantial increases in motion immediately after release of the iliofemoral ligament. This ligament primarily restricts excessive hip extension and external rotation; thus, previous conventional hip arthroscopy and open surgical dislocation involve releasing the iliofemoral ligament to gain greater access to the femoral head and neck. In general, it was suggested that there were marginal differences in stability between common capsulotomy approaches (i.e., interportal and T-capsulotomy)10,15,18, and capsular closure restored motion to more similar intact conditions9,10,12,14,15,18. In studies involving similar stepwise capsular management, Philippon et al. and Baha et al. measured the differences in range of motion after each surgical stage during capsular management15,48. Although both studies demonstrated that common arthroscopic capsulotomy procedures (i.e., portal placement, interportal capsulotomy, and T-capsulotomy) increased the envelope of hip motion (internal-external rotation, abduction-adduction, and flexion-extension), their capsular repair and reconstruction helped to partially restore normative range of motion of the joint. In a similar stepwise capsulotomy and repair study, Weber et al. recently showed that incrementally larger interportal capsulotomies decreased distraction stability18, while converting a smaller interportal capsulotomy to a T-capsulotomy (i.e., an additional incision to the vertical limb) did not affect distraction resistance. Although the aforementioned studies noted substantial differences, they used hip specimens from older donors (age range, 51 to 78 years) without any hip pathologies (e.g., cam morphology and dysplasia), which may not be representative of young patients having early onset hip pain.
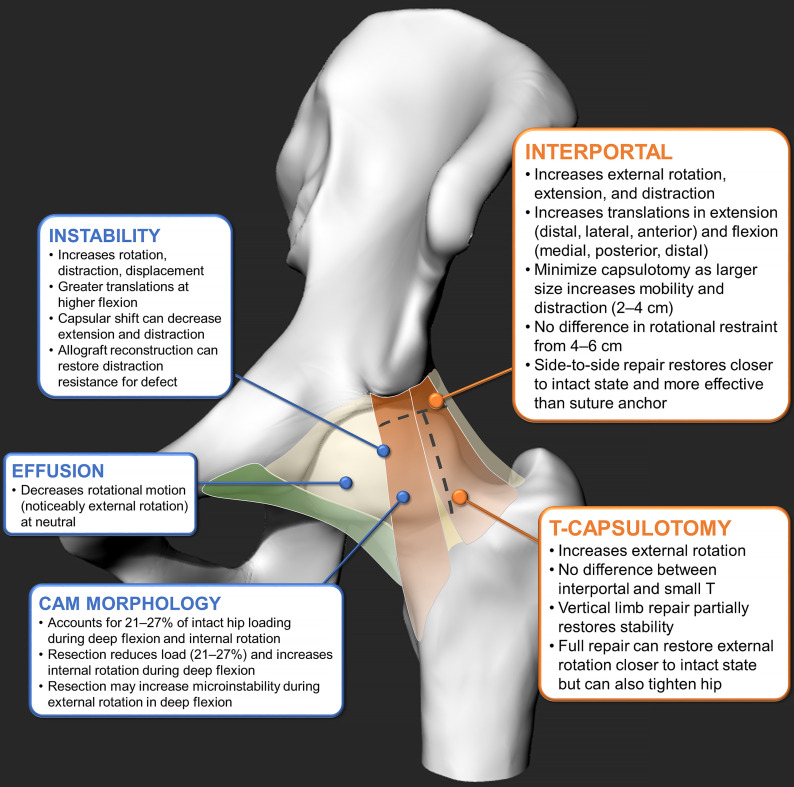
Fig. 4.
The findings of in vitro cadaveric studies on the effects of capsular conditions and surgical stages, outlining the contributions of the interportal capsulotomy5,7,8,10,11,14,46 and T-capsulotomy6,11,14,15,46 and the effects of instability7,11-13,16,47, effusion9, and cam morphology15,16. (For a detailed summary for each study’s scope, methods, and observations, see Appendix Tables II and III.)
In terms of simulating capsular laxity and abnormalities that would warrant the need for repair or plication, Jackson et al. simulated joint instability (subjected hips were stretched in extension under 35 Nm of torque for 1 hour) and suggested that side-to-side repair only partially decreased distraction resistance, while a capsular shift approach restored joint stability11. Although capsular plication may help to restore joint stability in extreme cases of joint subluxation, it perhaps should not be a routine procedure for all capsular closures. More recently, Johannsen et al. examined the effects of capsular laxity by subjecting hips without pathology to anterior capsular stretching (i.e., maximal extension with external rotation), which resulted in overall joint laxity and instability49. They noted that the anterior capsule predominantly controlled rotation and displacement, suggesting that the iliofemoral ligaments should be carefully preserved using more conservative capsulotomies. For capsular defect cases, allograft can be a viable option to restore distraction stability15,16. On the other hand, Hebert et al. compared the effects of hip effusion (simulated with an injection of 10 mL of saline solution) and capsular tears13. They noticed that effusions associated with arthritic conditions decreased hip mobility, while a capsular tear naturally increased instability. Therefore, as many routine surgical hip preservation and arthroplasty procedures seek to restore joint function in the prearthritic or already arthritic hip, it is crucial to consider intracapsular conditions, how inherently tight the hip in question is (i.e., joint effusion and level of degeneration or stiffness)50, or if the hip is too inherently unstable to warrant plication. As the specimens were from donors who were slightly older in age, it may not be appropriate to interpret the mechanical properties without considering age-related changes in the musculoskeletal system36,51. These results from in vitro cadaveric studies should be interpreted with caution, especially if the demographics and pathological groups were not appropriately represented in the experiments (i.e., healthy hips with no pathology were examined instead of those with osseous deformities or pathologies).
It is essential to understand that capsular characteristics and mechanical properties of the hip with pathological conditions are different (i.e., a thicker, stiffer capsule) than a healthy joint38,50,52; thus, the need for full capsular closure may depend on several other confounding factors (e.g., age, sex, osseous anatomy, and muscle function)53-55. More importantly, since unrepaired capsulotomies have been shown to heal within 24 weeks postoperatively56, and completely resecting the iliofemoral ligament does not destabilize the native hip43, there is evidence that not all capsulotomies need to be repaired after arthroscopy, especially when capsular contracture may be part of the pathological process. It is still unclear what leads to inherent or iatrogenic instability; thus, if the native head size is not substantially reduced or altered, capsular repair in the setting of a small arthroscopic capsulotomy may not be necessary in the otherwise congruent and stable hip4,54,56. Recently, a periportal capsulotomy technique (i.e., midanterior and anterolateral portal dilations) showed that it can preserve the iliofemoral ligament, without necessitating capsular closure57,58; however, it is unclear if this applies to dysplastic hips59.
Effects of Hip Preservation Surgery
Although the functional anatomy and biomechanics of the hip joint and encapsulating ligaments have been well described, surgical intervention and capsular management in hip arthroscopy and arthroplasty continue to raise many pressing concerns. With emerging interest in improving capsular management for hip preservation and postoperative joint arthroplasty mechanics, it is imperative to delineate the contribution of each surgical stage toward functional mobility and stability. The following recent in vitro laboratory studies contributed substantially to the understanding of hip arthroscopy and arthroplasty surgery, addressing several issues of demographics, stepwise surgical stages, varying implant parameters (e.g., implant type, head size, neck length, and anterior or posterior approach), and provided detailed insights into capsular function, mechanics, and management (see Appendix Table III).
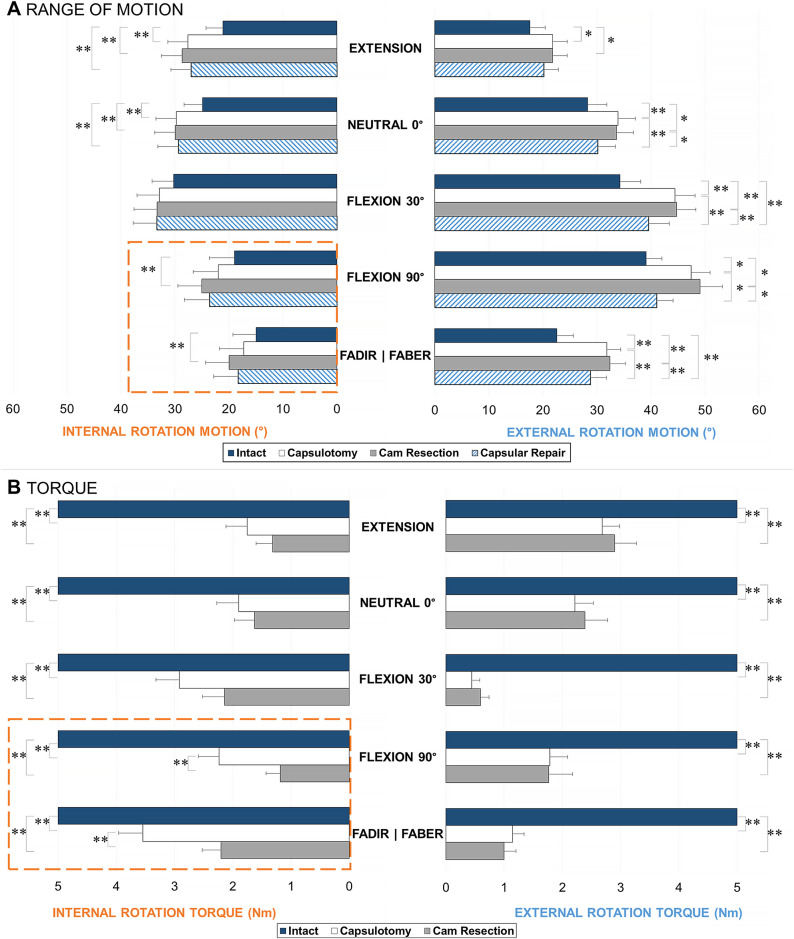
Although it has been well established that surgically resecting the cam morphology can delay the pathomechanical process of subchondral bone stiffening60,61, cartilage degeneration62,63, and adverse loading64,65, it was elusive how much the actual morphology or any of the individual surgical stages contributed to these aspects. In what we believe is the only documented in vitro cadaveric study that has examined a well-represented pathological cohort with cam morphologies, Ng et al. evaluated a large group of hip specimens with moderate-to-high alpha angles (representative of the symptomatic cam population) from young, male donors19. The study examined how the capsulotomy, cam resection, and capsular repair affected passive range of motion and torque loading (Fig. 5), using a 6-degrees-of-freedom robotic testing platform66. The study quantified the contribution of the cam deformity, which accounted for 21% to 27% of the torsional loading of the intact hip in deep flexion and internal rotation (Fig. 6), where the specimens indicated secondary at-risk parameters of smaller femoral neck-shaft67-71 and higher spinopelvic incidence angles72-74. Capsular repairs restrained external rotation during deep flexion and were ineffective in other testing positions, partly because of the inherently large native head that maintained joint stability and partly because the cam deformities were not overresected (i.e., no proximal concavity or “cookie bite”). As the femoral head is naturally conchoidal75 and may be precisely shaped to maintain the labral seal and effectively distribute load76, there may be suboptimal outcomes if a smaller cam morphology is resected. Translations of the hip joint center should be further examined to help characterize microinstability over the series of surgical stages17,20,49. In addition, the balance between capsular repair and plication should be compared with established objective measures to minimize iatrogenic instability in hips with pathology6,19.
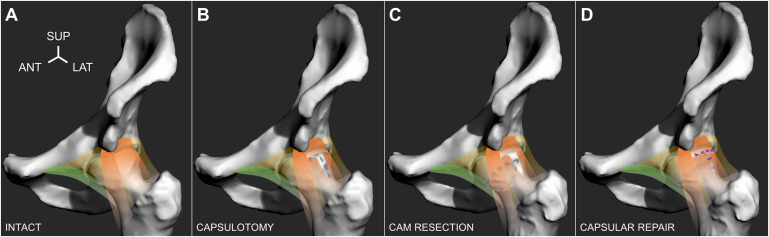
Fig. 5.
Four surgical stages depicted on a left-sided hip, which included the intact hip with cam morphology, were tested (with orange indicating the iliofemoral ligament; green, the pubofemoral ligament; and yellow, the encapsulating tissue) (Fig. 5-A); capsulotomy, in which the iliofemoral ligament was incised to create a T-capsulotomy (dashed lines) (Fig. 5-B); cam resection, in which the cam morphology was resected through the incised capsule (dashed lines) (Fig. 5-C); and capsular repair, in which the incised portal was closed using simple, interrupted sutures (purple knots) (Fig. 5-D). ANT = anterior, LAT = lateral, and SUP = superior. (Adapted, under CC BY 4.0 [https://creativecommons.org/licenses/by/4.0/], from: Ng KCG, El Daou H, Bankes MJK, Rodriguez Y Baena F, Jeffers JRT. Hip joint torsional loading before and after cam femoroacetabular impingement surgery. Am J Sports Med. 2019 Feb;47[2]:420-30. Published by SAGE Publishing. https://doi.org/10.1177/0363546518815159.)
Fig. 6.
Range of motion (Fig. 6-A) and torque loading (Fig. 6-B) in internal and external rotation, at each stage of testing: intact, capsulotomy, cam resection, and capsular repair (range of motion only), reported as the mean and standard error. Cam resection further increased internal rotation in the deep flexion positions (highlighted dashed lines). *The difference is significant (p < 0.05). **The difference is significant (p < 0.01.) FADIR = flexion-adduction and internal rotation, and FABER = flexion-abduction and external rotation. (Adapted, under CC BY 4.0 [https://creativecommons.org/licenses/by/4.0/], from: Ng KCG, El Daou H, Bankes MJK, Rodriguez Y Baena F, Jeffers JRT. Hip joint torsional loading before and after cam femoroacetabular impingement surgery. Am J Sports Med. 2019 Feb;47[2]:420-30. Published by SAGE Publishing. https://doi.org/10.1177/0363546518815159.)
Effects of Hip Arthroplasty Surgery
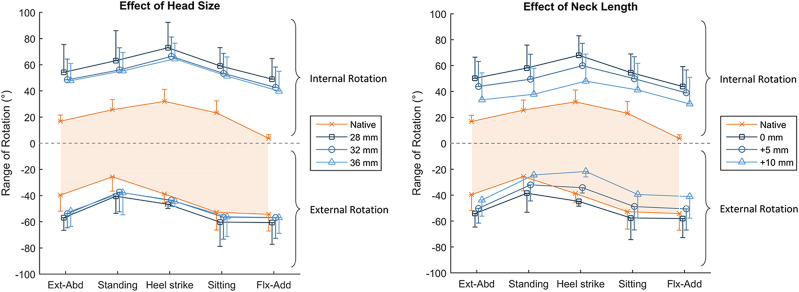
In an effort to characterize capsular function after total hip arthroplasty, van Arkel et al. inserted the femoral head, neck, and cup implants through a cotyloid fossa portal and, by doing so, preserved the entire intact joint capsule77. The authors reported that the smaller head sizes removed the natural tensioning ability of the capsule to restrain rotational motion (Fig. 7). The anterior capsule was less affected, particularly in flexion, as it had less of a dependence on ligament wrapping compared with the posterior ischiofemoral ligament. This further suggests that an intact zona orbicularis, which is more prominent in the posterior region39, can provide more help to medialize and secure the hip during extreme flexion-extension (without abduction-adduction and internal-external rotations) than the primary 3 ligaments. More importantly, a shorter neck length increased hypermobility, whereas a longer neck overtightened the anterior capsule (Fig. 7). These findings highlight the critical interaction between optimizing hip biomechanics and gait mechanics78-81.
Fig. 7.
After total hip arthroplasty, the effects of head size (left), with anatomical neck length, and increasing neck lengths (right) on rotational range of motion are depicted. The x axis denotes the testing positions, and the y axis denotes the internal-external rotation (positive-negative). The shaded orange area dictates the measured range of native hip rotation. Increasing head size had little effect, whereas lengthening the neck tightened the hip capsule and reduced external rotation in some hip positions. The values are given as the mean, and the error bars indicate the standard deviation. Ext-Abd = extension and abduction, and Flx-Add = flexion and adduction. (Reproduced from: van Arkel RJ, Ng KCG, Muirhead-Allwood SK, Jeffers JRT. Capsular ligament function after total hip arthroplasty. J Bone Joint Surg Am. 2018 Jul 18;100[14]:e94.)
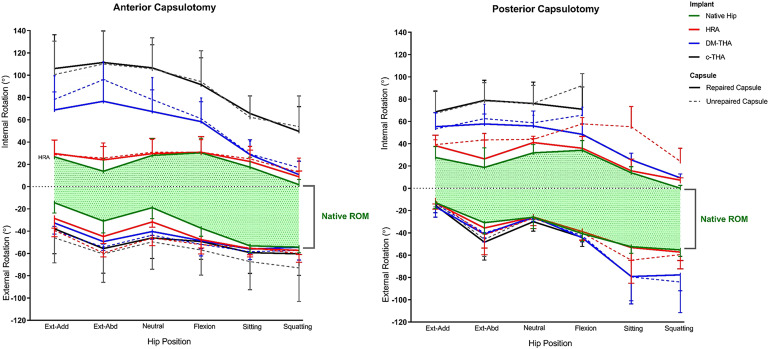
Logishetty et al., using paired hip specimens (n = 16; 8 left and 8 right), compared conventional hip arthroplasty with dual-mobility total hip arthroplasty and hip resurfacing arthroplasty82. The left-sided hips all underwent the direct anterior approach and capsulotomy, while the right-sided hips underwent the posterior surgical approach and capsulotomy. Because hip resurfacing arthroplasty preserved much of the near-native head size and femoral neck, it enabled a range of motion with marginal increases in hypermobility compared with the intact stage. Dual-mobility arthroplasty slightly increased range of motion, while total hip arthroplasty further increased hypermobility and lost most of the inherent capsular function. Although the posterior approach and capsular repair provided more normal function during low hip flexion and extension positions, with a shortened capsule after repair, it was evident that the total hip arthroplasty through the posterior approach demonstrated a higher likelihood of instability during deep flexion (Fig. 8). In contrast, the anterior approach functioned better in deep hip flexion and was not a dislocation risk after total hip arthroplasty. This was attributed not only to the preserved posterior ischiofemoral ligament but also perhaps to the preserved zona orbicularis, which helped to maintain distraction stability45 and highlighted the role of the obturator externus, which can pull taut along the same line as the posterior capsule83,84. That study illustrated the complex interaction between native hip structures in the context of hip arthroplasty (i.e., capsule, ligaments, and muscles) and joint mechanics specific to a surgical approach82. Regardless of approach, the near-native head size of a hip resurfacing arthroplasty and subsequent capsular repair preserved postoperative joint function.
Fig. 8.
The effects of the anterior (left) and posterior approaches (right) are examined with various types of implants: hip resurfacing arthroplasty (HRA; red), dual mobility arthroplasty (DM-THA; blue), and conventional total hip arthroplasty (c-THA; black) after unrepaired (dashed) and repaired conditions (solid). The x axis denotes the testing positions, and the y axis denotes the internal-external rotation (positive-negative). The shaded green area dictates the measured range of native hip rotation. The larger head size of the hip resurfacing arthroplasty demonstrated a range of motion that was more similar to the intact condition. The posterior approach showed higher dislocation risks during deep flexion. The values are given as the mean, and the error bars indicate the standard deviation. Ext-Abd = extension and abduction, Flx-Add = flexion and adduction, and ROM = range of motion. (Reproduced, with permission, from: Logishetty K, van Arkel RJ, Ng KCG, Muirhead-Allwood SK, Cobb JP, Jeffers JRT. Hip capsule biomechanics after arthroplasty: the effect of implant, approach, and surgical repair. Bone Joint J. 2019 Apr;101-B(4):426-34. ©2019 The British Editorial Society of Bone & Joint Surgery).
Overview
Recent research has focused on hip mechanics and our understanding of capsular function after hip preservation and arthroplasty, further highlighting fundamental capsular characteristics in the context of instability as well as optimizing hip function. Most of the work was conducted in in vitro cadaveric studies, which examined material characteristics of capsular ligaments, functional joint mobility and stability, or surgical management techniques. Little in vivo work in human subjects has been published.
In joint preservation surgery, there are ongoing debates as to whether to repair the capsule6,10,54,56,85-87. The decision to repair the capsule should not be a simple yes-or-no choice, as there should not be a general one-size-fits-all solution. Although the unrepaired capsule has been associated with inferior outcomes6,86, several confounding factors should still be considered87,88, such as the size and location of the capsulotomy, osseous morphology, and degree of surgical correction as well as native joint mobility. The effects of these factors are evident in the many cases of iatrogenic instability arising in patients with milder deformities who underwent overcorrection, resulting in ineffective labral seals and load distributions76,89-91, which were further compounded by a deficient capsule92. As capsular repair can substantially decrease external rotation during deep hip flexion, complete capsular repair or augmentation may be most effective for larger capsulotomies or overresected cams18,85; however, it should be cautiously performed to avoid overtightening the joint19.
Since surgical management of FAI and other common hip pathologies in young adults can be effective in minimizing the risks of adverse cartilage loading and degeneration19,61,64,65,70, more research needs to be done to examine where changes occur first (i.e., subchondral bone, cartilage, or capsule) in response to varying joint morphology and mechanics. This is certainly the case for the zona orbicularis. In both arthroscopic and arthroplasty cadaveric studies54,82, the hip joint stability was negatively affected when the vertical limb of the anterior capsulotomy extended past the intertrochanteric line and with a conventional posterior approach. The zona orbicularis is not only important for resisting joint distraction but also for the locking effect of the stability-inducing collar, which seems to play a role in preventing edge-loading (Video 1). Finally, a better understanding of capsular properties and hip biomechanics provides further insight into how implant type (e.g., resurfacing, dual-mobility, and conventional arthroplasty), reconstruction parameters (e.g., head size and offset), and surgical approaches (e.g., anterior or posterior) can impact hip range of motion and stability as well as the critical contribution of the overlying hip musculature.
Video 1.
To view the internal structures of the capsule, the acetabulum and femoral head were removed from the medial cotyloid fossa portal. Similar to the aperture of a camera, the zona orbicularis closes.
Appendix
Supporting material provided by the authors is posted with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJS/F512).
Footnotes
Investigation performed at the Imperial College London, London, United Kingdom, and the Division of Orthopaedic Surgery, University of Ottawa, Ottawa, Ontario, Canada
Disclosure: The authors indicated grant support from the Engineering and Physical Sciences Research Council (EPSRC) (EP/K027549/1 and EP/N006267/1) and the Wellcome Trust (088844/Z/09/Z), during the conduct of the study. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work (http://links.lww.com/JBJS/F511).
References
- 1.Hewitt J, Guilak F, Glisson R, Vail TP. Regional material properties of the human hip joint capsule ligaments. J Orthop Res. 2001. May;19(3):359-64. [DOI] [PubMed] [Google Scholar]
- 2.Malagelada F, Tayar R, Barke S, Stafford G, Field RE. Anatomy of the zona orbicularis of the hip: a magnetic resonance study. Surg Radiol Anat. 2015. January;37(1):11-8. Epub 2014 Apr 29. [DOI] [PubMed] [Google Scholar]
- 3.Wagner FV, Negrão JR, Campos J, Ward SR, Haghighi P, Trudell DJ, Resnick D. Capsular ligaments of the hip: anatomic, histologic, and positional study in cadaveric specimens with MR arthrography. Radiology. 2012. April;263(1):189-98. Epub 2012 Feb 27. [DOI] [PubMed] [Google Scholar]
- 4.Walters BL, Cooper JH, Rodriguez JA. New findings in hip capsular anatomy: dimensions of capsular thickness and pericapsular contributions. Arthroscopy. 2014. October;30(10):1235-45. Epub 2014 Jul 23. [DOI] [PubMed] [Google Scholar]
- 5.Bedi A, Galano G, Walsh C, Kelly BT. Capsular management during hip arthroscopy: from femoroacetabular impingement to instability. Arthroscopy. 2011. December;27(12):1720-31. Epub 2011 Nov 1. [DOI] [PubMed] [Google Scholar]
- 6.Ortiz-Declet V, Mu B, Chen AW, Litrenta J, Perets I, Yuen LC, Domb BG. Should the capsule be repaired or plicated after hip arthroscopy for labral tears associated with femoroacetabular impingement or instability? A systematic review. Arthroscopy. 2018. January;34(1):303-18. Epub 2017 Aug 31. [DOI] [PubMed] [Google Scholar]
- 7.Telleria JJ, Lindsey DP, Giori NJ, Safran MR. A quantitative assessment of the insertional footprints of the hip joint capsular ligaments and their spanning fibers for reconstruction. Clin Anat. 2014. April;27(3):489-97. Epub 2013 Nov 30. [DOI] [PubMed] [Google Scholar]
- 8.Martin HD, Savage A, Braly BA, Palmer IJ, Beall DP, Kelly B. The function of the hip capsular ligaments: a quantitative report. Arthroscopy. 2008. February;24(2):188-95. Epub 2007 Nov 26. [DOI] [PubMed] [Google Scholar]
- 9.Bayne CO, Stanley R, Simon P, Espinoza-Orias A, Salata MJ, Bush-Joseph CA, Inoue N, Nho SJ. Effect of capsulotomy on hip stability-a consideration during hip arthroscopy. Am J Orthop (Belle Mead NJ). 2014. April;43(4):160-5. [PubMed] [Google Scholar]
- 10.Abrams GD, Hart MA, Takami K, Bayne CO, Kelly BT, Espinoza Orías AA, Nho SJ. Biomechanical evaluation of capsulotomy, capsulectomy, and capsular repair on hip rotation. Arthroscopy. 2015. August;31(8):1511-7. Epub 2015 Apr 14. [DOI] [PubMed] [Google Scholar]
- 11.Jackson TJ, Peterson AB, Akeda M, Estess A, McGarry MH, Adamson GJ, Lee TQ. Biomechanical effects of capsular shift in the treatment of hip microinstability: creation and testing of a novel hip instability model. Am J Sports Med. 2016. March;44(3):689-95. Epub 2015 Dec 30. [DOI] [PubMed] [Google Scholar]
- 12.Wuerz TH, Song SH, Grzybowski JS, Martin HD, Mather RC, 3rd, Salata MJ, Espinoza Orías AA, Nho SJ. Capsulotomy size affects hip joint kinematic stability. Arthroscopy. 2016. August;32(8):1571-80. Epub 2016 May 17. [DOI] [PubMed] [Google Scholar]
- 13.Hebert C, Smyth MP, Woodard E, Bills CC, Mihalko MJ, Mihalko WM. Effects of hip joint transverse plane range of motion with a modeled effusion and capsular tear: a cadaveric study. Clin Biomech (Bristol, Avon). 2017. February;42:115-9. Epub 2017 Jan 21. [DOI] [PubMed] [Google Scholar]
- 14.Khair MM, Grzybowski JS, Kuhns BD, Wuerz TH, Shewman E, Nho SJ. The effect of capsulotomy and capsular repair on hip distraction: a cadaveric investigation. Arthroscopy. 2017. March;33(3):559-65. Epub 2016 Dec 22. [DOI] [PubMed] [Google Scholar]
- 15.Philippon MJ, Trindade CAC, Goldsmith MT, Rasmussen MT, Saroki AJ, Løken S, LaPrade RF. Biomechanical assessment of hip capsular repair and reconstruction procedures using a 6 degrees of freedom robotic system. Am J Sports Med. 2017. July;45(8):1745-54. Epub 2017 Apr 3. [DOI] [PubMed] [Google Scholar]
- 16.Fagotti L, Kemler BR, Utsunomiya H, Storaci HW, Krob JJ, Brady AW, Turnbull TL, Philippon MJ. Effects of capsular reconstruction with an iliotibial band allograft on distractive stability of the hip joint: a biomechanical study. Am J Sports Med. 2018. December;46(14):3429-36. Epub 2018 Nov 1. [DOI] [PubMed] [Google Scholar]
- 17.Han S, Alexander JW, Thomas VS, Choi J, Harris JD, Doherty DB, Jeffers JRT, Noble PC. Does capsular laxity lead to microinstability of the native hip? Am J Sports Med. 2018. May;46(6):1315-23. Epub 2018 Mar 5. [DOI] [PubMed] [Google Scholar]
- 18.Weber AE, Neal WH, Mayer EN, Kuhns BD, Shewman E, Salata MJ, Mather RC, Nho SJ. Vertical extension of the T-capsulotomy incision in hip arthroscopic surgery does not affect the force required for hip distraction: effect of capsulotomy size, type, and subsequent repair. Am J Sports Med. 2018. November;46(13):3127-33. Epub 2018 Oct 11. [DOI] [PubMed] [Google Scholar]
- 19.Ng KCG, El Daou H, Bankes MJK, Rodriguez Y Baena F, Jeffers JRT. Hip joint torsional loading before and after cam femoroacetabular impingement surgery. Am J Sports Med. 2019. February;47(2):420-30. Epub 2018 Dec 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ng KCG, El Daou H, Bankes MJK, Rodriguez y Baena F, Jeffers JRT. Hip centre of rotation and microinstability after cam FAI surgery. Presented as a poster exhibit at the Annual Meeting of the Orthopaedic Research Society; 2019. February 2-5; Austin, TX: Poster no. 0172. [Google Scholar]
- 21.Frank CB. Ligament structure, physiology and function. J Musculoskelet Neuronal Interact. 2004. June;4(2):199-201. [PubMed] [Google Scholar]
- 22.Bland YS, Ashhurst DE. The hip joint: the fibrillar collagens associated with development and ageing in the rabbit. J Anat. 2001. January;198(Pt 1):17-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oda H, Igarashi M, Hayashi Y, Karube S, Inoue S, Sakaguchi R, Kimizuka M. Soft tissue collagen in congenital dislocation of the hip. Biochemical studies of the ligamentum teres of the femur and the hip joint capsule. Nihon Seikeigeka Gakkai Zasshi. 1984. March;58(3):331-8. [PubMed] [Google Scholar]
- 24.Jensen BA, Reimann I, Fredensborg N. Collagen type III predominance in newborns with congenital dislocation of the hip. Acta Orthop Scand. 1986. August;57(4):362-5. [DOI] [PubMed] [Google Scholar]
- 25.Hosseininia S, Weis MA, Rai J, Kim L, Funk S, Dahlberg LE, Eyre DR. Evidence for enhanced collagen type III deposition focally in the territorial matrix of osteoarthritic hip articular cartilage. Osteoarthritis Cartilage. 2016. June;24(6):1029-35. Epub 2016 Jan 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Matsumoto F, Trudel G, Uhthoff HK. High collagen type I and low collagen type III levels in knee joint contracture: an immunohistochemical study with histological correlate. Acta Orthop Scand. 2002. June;73(3):335-43. [DOI] [PubMed] [Google Scholar]
- 27.O’Donnell JM, Devitt BM, Arora M. The role of the ligamentum teres in the adult hip: redundant or relevant? A review. J Hip Preserv Surg. 2018. January 10;5(1):15-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cerezal L, Arnaiz J, Canga A, Piedra T, Altónaga JR, Munafo R, Pérez-Carro L. Emerging topics on the hip: ligamentum teres and hip microinstability. Eur J Radiol. 2012. December;81(12):3745-54. Epub 2011 Jul 1. [DOI] [PubMed] [Google Scholar]
- 29.Philippon MJ, Rasmussen MT, Turnbull TL, Trindade CA, Hamming MG, Ellman MB, Harris M, LaPrade RF, Wijdicks CA. Structural properties of the native ligamentum teres. Orthop J Sports Med. 2014. December 12;2(12):2325967114561962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jo S, Hooke AW, An KN, Trousdale RT, Sierra RJ. Contribution of the ligamentum teres to hip stability in the presence of an intact capsule: a cadaveric study. Arthroscopy. 2018. May;34(5):1480-7. Epub 2018 Feb 1. [DOI] [PubMed] [Google Scholar]
- 31.Martin HD, Hatem MA, Kivlan BR, Martin RL. Function of the ligamentum teres in limiting hip rotation: a cadaveric study. Arthroscopy. 2014. September;30(9):1085-91. Epub 2014 Jun 6. [DOI] [PubMed] [Google Scholar]
- 32.Mikula JD, Slette EL, Chahla J, Brady AW, Locks R, Trindade CA, Rasmussen MT, LaPrade RF, Philippon MJ. Quantitative anatomic analysis of the native ligamentum teres. Orthop J Sports Med. 2017. February 24;5(2):2325967117691480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tucker FR. Arterial supply to the femoral head and its clinical importance. J Bone Joint Surg Br. 1949. February;31B(1):82-93. [PubMed] [Google Scholar]
- 34.Hewitt JD, Glisson RR, Guilak F, Vail TP. The mechanical properties of the human hip capsule ligaments. J Arthroplasty. 2002. January;17(1):82-9. [DOI] [PubMed] [Google Scholar]
- 35.Stewart KJ, Edmonds-Wilson RH, Brand RA, Brown TD. Spatial distribution of hip capsule structural and material properties. J Biomech. 2002. November;35(11):1491-8. [DOI] [PubMed] [Google Scholar]
- 36.Schleifenbaum S, Prietzel T, Hädrich C, Möbius R, Sichting F, Hammer N. Tensile properties of the hip joint ligaments are largely variable and age-dependent - an in-vitro analysis in an age range of 14-93 years. J Biomech. 2016. October 3;49(14):3437-43. Epub 2016 Sep 17. [DOI] [PubMed] [Google Scholar]
- 37.Philippon MJ, Michalski MP, Campbell KJ, Rasmussen MT, Goldsmith MT, Devitt BM, Wijdicks CA, LaPrade RF. A quantitative analysis of hip capsular thickness. Knee Surg Sports Traumatol Arthrosc. 2015. September;23(9):2548-53. Epub 2014 May 10. [DOI] [PubMed] [Google Scholar]
- 38.Rakhra KS, Bonura AA, Nairn R, Schweitzer ME, Kolanko NM, Beaule PE. Is the hip capsule thicker in diseased hips? Bone Joint Res. 2016. November;5(11):586-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Weidner J, Büchler L, Beck M. Hip capsule dimensions in patients with femoroacetabular impingement: a pilot study. Clin Orthop Relat Res. 2012. December;470(12):3306-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Blum A, Raymond A, Teixeira P. Strategy and optimization of diagnostic imaging in painful hip in adults. Orthop Traumatol Surg Res. 2015. February;101(1)(Suppl):S85-99. Epub 2015 Jan 15. [DOI] [PubMed] [Google Scholar]
- 41.Devitt BM, Smith BN, Stapf R, Tacey M, O’Donnell JM. Generalized joint hypermobility is predictive of hip capsular thickness. Orthop J Sports Med. 2017. April 19;5(4):2325967117701882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Myers CA, Register BC, Lertwanich P, Ejnisman L, Pennington WW, Giphart JE, LaPrade RF, Philippon MJ. Role of the acetabular labrum and the iliofemoral ligament in hip stability: an in vitro biplane fluoroscopy study. Am J Sports Med. 2011. July;39(Suppl):85S-91S. [DOI] [PubMed] [Google Scholar]
- 43.van Arkel RJ, Amis AA, Cobb JP, Jeffers JR. The capsular ligaments provide more hip rotational restraint than the acetabular labrum and the ligamentum teres: an experimental study. Bone Joint J. 2015. April;97-B(4):484-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Smith MV, Costic RS, Allaire R, Schilling PL, Sekiya JK. A biomechanical analysis of the soft tissue and osseous constraints of the hip joint. Knee Surg Sports Traumatol Arthrosc. 2014. April;22(4):946-52. Epub 2012 Oct 30. [DOI] [PubMed] [Google Scholar]
- 45.Ito H, Song Y, Lindsey DP, Safran MR, Giori NJ. The proximal hip joint capsule and the zona orbicularis contribute to hip joint stability in distraction. J Orthop Res. 2009. August;27(8):989-95. [DOI] [PubMed] [Google Scholar]
- 46.Babst D, Steppacher SD, Ganz R, Siebenrock KA, Tannast M. The iliocapsularis muscle: an important stabilizer in the dysplastic hip. Clin Orthop Relat Res. 2011. June;469(6):1728-34. Epub 2010 Dec 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Haefeli PC, Steppacher SD, Babst D, Siebenrock KA, Tannast M. An increased iliocapsularis-to-rectus-femoris ratio is suggestive for instability in borderline hips. Clin Orthop Relat Res. 2015. December;473(12):3725-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Baha P, Burkhart TA, Getgood A, Degen RM. Complete capsular repair restores native kinematics after interportal and T-capsulotomy. Am J Sports Med. 2019. May;47(6):1451-8. Epub 2019 Apr 4. [DOI] [PubMed] [Google Scholar]
- 49.Johannsen AM, Behn AW, Shibata K, Ejnisman L, Thio T, Safran MR. The role of anterior capsular laxity in hip microinstability: a novel biomechanical model. Am J Sports Med. 2019. April;47(5):1151-8. Epub 2019 Mar 13. [DOI] [PubMed] [Google Scholar]
- 50.Bierma-Zeinstra SMA, Bohnen AM, Verhaar JAN, Prins A, Ginai-Karamat AZ, Laméris JS. Sonography for hip joint effusion in adults with hip pain. Ann Rheum Dis. 2000. March;59(3):178-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Buckwalter JA, Woo SL-Y. Age-related changes in ligaments and joint capsules: implications for participation in sports. Sports Med Arthrosc Rev. 1996. October;4(3):250-62. [Google Scholar]
- 52.Pieroh P, Schneider S, Lingslebe U, Sichting F, Wolfskämpf T, Josten C, Böhme J, Hammer N, Steinke H. The stress-strain data of the hip capsule ligaments are gender and side independent suggesting a smaller contribution to passive stiffness. PLoS One. 2016. September 29;11(9):e0163306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Domb BG, Stake CE, Finley ZJ, Chen T, Giordano BD. Influence of capsular repair versus unrepaired capsulotomy on 2-year clinical outcomes after arthroscopic hip preservation surgery. Arthroscopy. 2015. April;31(4):643-50. Epub 2014 Dec 16. [DOI] [PubMed] [Google Scholar]
- 54.Matsuda DK. Editorial commentary: hip capsule: to repair or not? Arthroscopy. 2017. January;33(1):116-7. [DOI] [PubMed] [Google Scholar]
- 55.Abrams GD. Editorial commentary: the importance of capsular closure in hip arthroscopy: is there a limit to the benefit? Arthroscopy. 2018. March;34(3):864-5. [DOI] [PubMed] [Google Scholar]
- 56.Strickland CD, Kraeutler MJ, Brick MJ, Garabekyan T, Woon JTK, Chadayammuri V, Mei-Dan O. MRI evaluation of repaired versus unrepaired interportal capsulotomy in simultaneous bilateral hip arthroscopy: a double-blind, randomized controlled trial. J Bone Joint Surg Am. 2018. January 17;100(2):91-8. [DOI] [PubMed] [Google Scholar]
- 57.Chambers CC, Monroe EJ, Flores SE, Borak KR, Zhang AL. Periportal capsulotomy: technique and outcomes for a limited capsulotomy during hip arthroscopy. Arthroscopy. 2019. April;35(4):1120-7. Epub 2019 Mar 11. [DOI] [PubMed] [Google Scholar]
- 58.Monroe EJ, Chambers CC, Zhang AL. Periportal capsulotomy: a technique for limited violation of the hip capsule during arthroscopy for femoroacetabular impingement. Arthrosc Tech. 2019. January 28;8(2):e205-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Aoki SK. Editorial commentary: hip arthroscopy capsular approaches: periportal, puncture, interportal, T-cut… does it really matter? Arthroscopy. 2019. April;35(4):1128-9. [DOI] [PubMed] [Google Scholar]
- 60.Speirs AD, Beaulé PE, Rakhra KS, Schweitzer ME, Frei H. Increased acetabular subchondral bone density is associated with cam-type femoroacetabular impingement. Osteoarthritis Cartilage. 2013. April;21(4):551-8. Epub 2013 Jan 26. [DOI] [PubMed] [Google Scholar]
- 61.Speirs AD, Rakhra KS, Weir Weiss MJ, Beaulé PE. Bone density changes following surgical correction of femoroacetabular impingement deformities. Osteoarthritis Cartilage. 2018. December;26(12):1683-90. Epub 2018 Sep 6. [DOI] [PubMed] [Google Scholar]
- 62.McGuffin WS, Melkus G, Rakhra KS, Beaulé PE. Is the contralateral hip at risk in patients with unilateral symptomatic cam femoroacetabular impingement? A quantitative T1ρ MRI study. Osteoarthritis Cartilage. 2015. August;23(8):1337-42. Epub 2015 Mar 25. [DOI] [PubMed] [Google Scholar]
- 63.Anwander H, Melkus G, Rakhra KS, Beaulé PE. T1ρ MRI detects cartilage damage in asymptomatic individuals with a cam deformity. J Orthop Res. 2016. June;34(6):1004-9. Epub 2015 Dec 2. [DOI] [PubMed] [Google Scholar]
- 64.Beaulé PE, Speirs AD, Anwander H, Melkus G, Rakhra K, Frei H, Lamontagne M. Surgical correction of cam deformity in association with femoroacetabular impingement and its impact on the degenerative process within the hip joint. J Bone Joint Surg Am. 2017. August 16;99(16):1373-81. [DOI] [PubMed] [Google Scholar]
- 65.Beaulé PE, Grammatopoulos G, Speirs A, Geoffrey Ng KC, Carsen S, Frei H, Melkus G, Rakhra K, Lamontagne M. Unravelling the hip pistol grip/cam deformity: origins to joint degeneration. J Orthop Res. 2018. December;36(12):3125-35. Epub 2018 Sep 21. [DOI] [PubMed] [Google Scholar]
- 66.El Daou H, Ng KCG, Van Arkel R, Jeffers JRT, Rodriguez Y Baena F. Robotic hip joint testing: development and experimental protocols. Med Eng Phys. 2019. January;63:57-62. Epub 2018 Nov 9. [DOI] [PubMed] [Google Scholar]
- 67.Ng KCG, Lamontagne M, Adamczyk AP, Rakhra KS, Beaulé PE. Patient-specific anatomical and functional parameters provide new insights into the pathomechanism of cam FAI. Clin Orthop Relat Res. 2015. April;473(4):1289-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ng KCG, Lamontagne M, Beaulé PE. Differences in anatomical parameters between the affected and unaffected hip in patients with bilateral cam-type deformities. Clin Biomech (Bristol, Avon). 2016. March;33:13-9. Epub 2016 Feb 2. [DOI] [PubMed] [Google Scholar]
- 69.Ng KCG, Mantovani G, Lamontagne M, Labrosse MR, Beaulé PE. Increased hip stresses resulting from a cam deformity and decreased femoral neck-shaft angle during level walking. Clin Orthop Relat Res. 2017. April;475(4):998-1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ng KCG, Mantovani G, Lamontagne M, Labrosse MR, Beaulé PE. Cam FAI and smaller neck angles increase subchondral bone stresses during squatting: a finite element analysis. Clin Orthop Relat Res. 2019. May;477(5):1053-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bardakos NV, Villar RN. Predictors of progression of osteoarthritis in femoroacetabular impingement: a radiological study with a minimum of ten years follow-up. J Bone Joint Surg Br. 2009. February;91(2):162-9. [DOI] [PubMed] [Google Scholar]
- 72.Ng KCG, Lamontagne M, Jeffers JRT, Grammatopoulos G, Beaulé PE. Anatomic predictors of sagittal hip and pelvic motions in patients with a cam deformity. Am J Sports Med. 2018. May;46(6):1331-42. Epub 2018 Mar 8. [DOI] [PubMed] [Google Scholar]
- 73.Ng KCG, Mantovani G, Modenese L, Beaulé PE, Lamontagne M. Altered walking and muscle patterns reduce hip contact forces in individuals with symptomatic cam femoroacetabular impingement. Am J Sports Med. 2018. September;46(11):2615-23. Epub 2018 Aug 3. [DOI] [PubMed] [Google Scholar]
- 74.Grammatopoulos G, Speirs AD, Ng KCG, Rivière C, Rakhra KS, Lamontagne M, Beaule PE. Acetabular and spino-pelvic morphologies are different in subjects with symptomatic cam femoro-acetabular impingement. J Orthop Res. 2018. July;36(7):1840-8. Epub 2018 Feb 7. [DOI] [PubMed] [Google Scholar]
- 75.Menschik F. The hip joint as a conchoid shape. J Biomech. 1997. September;30(9):971-3. [DOI] [PubMed] [Google Scholar]
- 76.Bullough P, Goodfellow J, O’Conner J. The relationship between degenerative changes and load-bearing in the human hip. J Bone Joint Surg Br. 1973. November;55(4):746-58. [PubMed] [Google Scholar]
- 77.van Arkel RJ, Ng KCG, Muirhead-Allwood SK, Jeffers JRT. Capsular ligament function after total hip arthroplasty. J Bone Joint Surg Am. 2018. July 18;100(14):e94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Queen RM, Butler RJ, Watters TS, Kelley SS, Attarian DE, Bolognesi MP. The effect of total hip arthroplasty surgical approach on postoperative gait mechanics. J Arthroplasty. 2011. September;26(6)(Suppl):66-71. Epub 2011 Jun 24. [DOI] [PubMed] [Google Scholar]
- 79.Chamnongkich S, Asayama I, Kinsey TL, Mahoney OM, Simpson KJ. Difference in hip prosthesis femoral offset affects hip abductor strength and gait characteristics during obstacle crossing. Orthop Clin North Am. 2012. November;43(5):e48-58. Epub 2012 Sep 15. [DOI] [PubMed] [Google Scholar]
- 80.Bahl JS, Nelson MJ, Taylor M, Solomon LB, Arnold JB, Thewlis D. Biomechanical changes and recovery of gait function after total hip arthroplasty for osteoarthritis: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2018. July;26(7):847-63. Epub 2018 Feb 21. [DOI] [PubMed] [Google Scholar]
- 81.Flecher X, Ollivier M, Argenson JN. Lower limb length and offset in total hip arthroplasty. Orthop Traumatol Surg Res. 2016. February;102(1)(Suppl):S9-20. Epub 2016 Jan 18. [DOI] [PubMed] [Google Scholar]
- 82.Logishetty K, van Arkel RJ, Ng KCG, Muirhead-Allwood SK, Cobb JP, Jeffers JRT. Hip capsule biomechanics after arthroplasty: the effect of implant, approach, and surgical repair. Bone Joint J. 2019. April;101-B(4):426-34. Epub 2019 Feb 15. [DOI] [PubMed] [Google Scholar]
- 83.Hogervorst T, Vereecke EE. Evolution of the human hip. Part 2: muscling the double extension. J Hip Preserv Surg. 2014. October 28;2(1):3-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Gudena R, Alzahrani A, Railton P, Powell J, Ganz R. The anatomy and function of the obturator externus. Hip Int. 2015. Sep-Oct;25(5):424-7. Epub 2015 Apr 27. [DOI] [PubMed] [Google Scholar]
- 85.Frank RM, Lee S, Bush-Joseph CA, Kelly BT, Salata MJ, Nho SJ. Improved outcomes after hip arthroscopic surgery in patients undergoing T-capsulotomy with complete repair versus partial repair for femoroacetabular impingement: a comparative matched-pair analysis. Am J Sports Med. 2014. November;42(11):2634-42. Epub 2014 Sep 11. [DOI] [PubMed] [Google Scholar]
- 86.Domb BG, Chaharbakhshi EO, Perets I, Walsh JP, Yuen LC, Ashberg LJ. Patient-reported outcomes of capsular repair versus capsulotomy in patients undergoing hip arthroscopy: minimum 5-year follow-up-a matched comparison study. Arthroscopy. 2018. March;34(3):853-863.e1. Epub 2018 Jan 17. [DOI] [PubMed] [Google Scholar]
- 87.Dippmann C, Kraemer O, Lund B, Krogsgaard M, Hölmich P, Lind M, Briggs K, Philippon M, Mygind-Klavsen B. Multicentre study on capsular closure versus non-capsular closure during hip arthroscopy in Danish patients with femoroacetabular impingement (FAI): protocol for a randomised controlled trial. BMJ Open. 2018. February 10;8(2):e019176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Naal FD, Müller A, Varghese VD, Wellauer V, Impellizzeri FM, Leunig M. Outcome of hip impingement surgery: does generalized joint hypermobility matter? Am J Sports Med. 2017. May;45(6):1309-14. Epub 2017 Jan 31. [DOI] [PubMed] [Google Scholar]
- 89.Aoki SK, Beckmann JT, Wylie JD. Arthroscopic femoral osteochondroplasty for cam-type femoroacetabular impingement: the trough technique. Arthrosc Tech. 2016. July 18;5(4):e743-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zingg PO, Ulbrich EJ, Buehler TC, Kalberer F, Poutawera VR, Dora C. Surgical hip dislocation versus hip arthroscopy for femoroacetabular impingement: clinical and morphological short-term results. Arch Orthop Trauma Surg. 2013. January;133(1):69-79. Epub 2012 Oct 14. [DOI] [PubMed] [Google Scholar]
- 91.Mansor Y, Perets I, Close MR, Mu BH, Domb BG. In search of the spherical femoroplasty: cam overresection leads to inferior functional scores before and after revision hip arthroscopic surgery. Am J Sports Med. 2018. July;46(9):2061-71. Epub 2018 Jun 20. [DOI] [PubMed] [Google Scholar]
- 92.Frank JM, Chahla J, Mitchell JJ, Soares E, Philippon MJ. Remplissage of the femoral head-neck junction in revision hip arthroscopy: a technique to correct excessive cam resection. Arthrosc Tech. 2016. October 24;5(6):e1209-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Goldsmith MT, Rasmussen MT, Lee Turnbull T, Trindade CA, LaPrade RF, Philippon MJ, Wijdicks CA. Validation of a six degree-of-freedom robotic system for hip in vitro biomechanical testing. J Biomech. 2015. November 26;48(15):4093-100. Epub 2015 Oct 19. [DOI] [PubMed] [Google Scholar]
- 94.Colbrunn RW, Bottros JJ, Butler RS, Klika AK, Bonner TF, Greeson C, van den Bogert AJ, Barsoum WK. Impingement and stability of total hip arthroplasty versus femoral head resurfacing using a cadaveric robotics model. J Orthop Res. 2013. July;31(7):1108-15. Epub 2013 Mar 13. [DOI] [PubMed] [Google Scholar]