To the Editor:
Although there has been much coverage of the vulnerable populations and risk factors of coronavirus disease 2019 (COVID-19), attention to hospitalized populations with severe disabilities has been limited. We retrospectively analyzed the infection features of inpatients with brain damage (BD) in one rehabilitation ward of a large general hospital with natural exposure to COVID-19 at the beginning of the outbreak in Wuhan. This rehabilitation ward is responsible for improving the functional status of a large number of patients with severe neurological injuries in the subacute phase for reasonable transfer to other institutions.1 We analyzed the demographic characteristics, major injuries, comorbidities, dysfunctions, and daily activity levels of COVID-19 patients with BD from this ward and further explored the differences between these patients and noninfected subjects with BD.
From December 30, 2019 to February 17, 2020, 38 patients with subacute neurological disorders (25 with BD and 13 with spinal cord injuries) were admitted to this rehabilitation ward. A series of strict measures related to COVID-19 were implemented for all personnel in this ward starting on January 22, 2020. In addition to daily environmental disinfection, hand hygiene and mask protection were also required for all members. Patients with fever were isolated immediately. Blood tests, computed tomography (CT), and real-time polymerase chain reaction were performed as soon as possible. Finally, four patients were diagnosed with COVID-19 infection by polymerase chain reaction assay and transferred to the designated medical institution during this period. There were no reports of COVID-19 in staff and caregivers.
The four male patients who were diagnosed with COVID-19 pneumonia all experienced BD, accounting for 16% of all BD patients (21 male/4 female) in this ward. The median ages of the noninfected and infected BD patients were 50 yrs (IQR, 37.5–63 yrs) and 60.5 yrs (IQR, 48.5–68 yrs), respectively. The COVID-19 patients with BD showed a higher prevalence rate of tracheotomy (75% vs 9.5%, P = 0.016) and underlying pulmonary infection (100% vs 38.1%, P = 0.039). Their modified Barthel Index scores were significantly lower than those of noninfected subjects with BD (7.5 ± 9.6 vs 29.5 ± 26.4, P = 0.011). These four people were the only inpatients under double supervision with two caregivers in the ward. The detailed clinical characteristics of the infected and noninfected patients with BD, including demographics, primary diagnosis, invasive intervention history, underlying diseases, dysfunctions, and activity levels, were compared and are presented in Table 1.
TABLE 1.
Features of the infected and noninfected inpatients with BD including the four COVID-19 patients

All four patients developed fever first, three had cough, and one had dyspnea. One 65-yr-old man (case 1) experienced nausea, vomiting, diarrhea, and chills but no dyspnea. The hemoglobin and albumin levels of these four patients were lower than or equal to the threshold value. Only case 3 showed a significant increase in white blood cell count (13.49 × 109/L) and neutrophil count (11.02 × 109/L) simultaneously with fever and cough. No other symptoms were reported. In addition to treatment for BD, these patients received antiviral treatment, antibiotics, corticosteroids, intravenous immunoglobulin, and oxygen therapy. Unfortunately, the oldest of the four patients (case 4) died within a week after diagnosis, two of the other three patients were classified as severely infected, and one was mildly infected. As of April 15, 2020, two patients were discharged home, and one patient still needed hospitalization. The detailed information of these patients is shown in Table 1. The most notable features of these four patients were impaired airway, reduced activity, previous pulmonary infection, and a variety of other underlying diseases and dysfunctions. The median modified Barthel Index score of 5 (full score, 100) indicates extremely impaired daily activity levels.2
Unlike the emergency diagnosis procedure for COVID-19, which advocated for CT at that time, the first symptom of these patients was fever, and the subsequent CT scan did not suggest typical changes. The blood tests also found no obvious reduction in lymphocyte count. Finally, these patients were quickly isolated as suspected cases after the appearance of clinical symptoms such as fever and cough and then confirmed by real-time polymerase chain reaction. The patients’ underlying pulmonary infections may make the CT manifestation of COVID-19 pneumonia atypical, and the images of old and new lesions superimposed on each other increase the difficulty of imaging diagnosis. In Figure 1, we show the CT images of case 1 in the early stage, disease progression stage, and recovery stage of COVID-19. A recent study on COVID-19 patients who underwent thoracic surgery also suggests that changes after thoracic surgery obscure the typical CT imaging features of early COVID-19 infection.3 Therefore, for these patients, we need to pay more attention to their clinical symptoms and dynamic changes on CT images and confirm the diagnosis by polymerase chain reaction in time for corresponding treatment.
FIGURE 1.
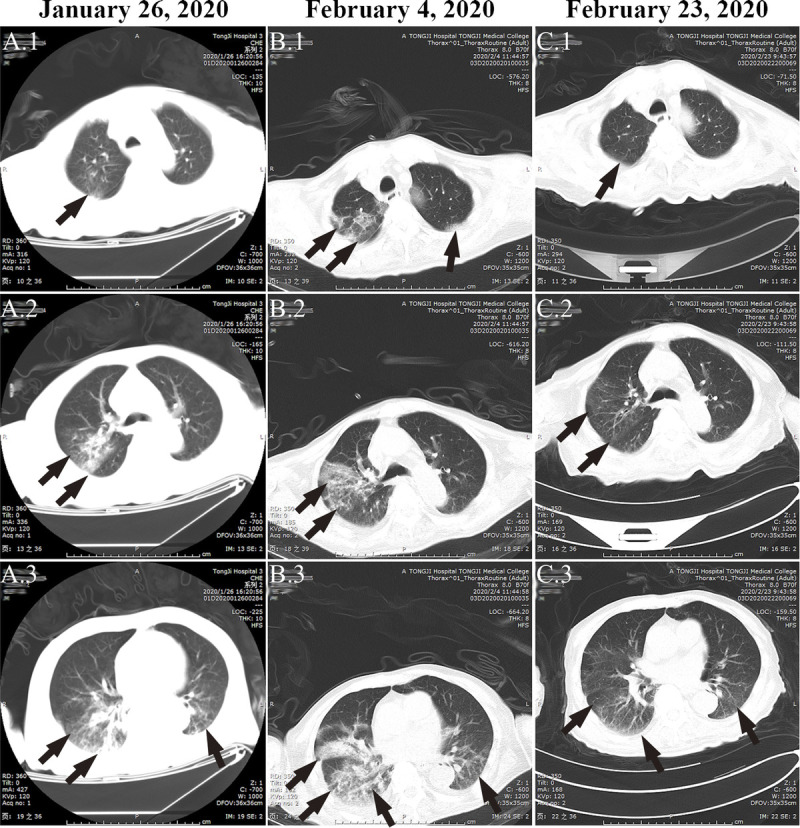
The evolution process of COVID-19 pneumonia in case 1. For case 1, on the day of onset on January 26, 2020, CT images indicated pneumonia (as indicated by arrows), but there were no typical manifestations of peripheral subpleural ground-glass opacities (A.1–A.3). A rapid progression of pneumonia was observed on the CT image 9 days after onset (B.1–B.3). Computed tomography re-examination indicated significant improvement on February 23, 2020 (C.1–C.3).
The reasons why such patients are so susceptible to COVID-19 may be as follows. First, impaired airways due to tracheotomy without precautions provide a very convenient way to inhale and exhale severe acute respiratory syndrome coronavirus 2 droplets. In a hospital environment with a high incidence of nosocomial infections, a large number of severe acute respiratory syndrome coronavirus 2 particles may flood the air and adhere to the surface of items. Second, the hemoglobin and albumin levels of these four patients suggested that their overall nutritional status was not ideal. Poor nutritional status and a variety of underlying diseases and dysfunctions leave patients in an extremely vulnerable state. The subsequent development of COVID-19 may be fatal. Third, because of low activity, frequent contact with multiple caregivers may further increase the chance of cross-infection. Therefore, in the context of the COVID-19 pandemic, healthcare institutions may need to provide a stricter isolation environment as well as visitation management for patients with impaired airways and low daily activity levels after BD.
The retrospective data analysis in the manner of case series within single center inevitably has some limitations. On the one hand, we failed to compare the COVID-19 infection status in rehabilitation ward with characteristics-matched patient groups in other wards in our hospital. Patients in the rehabilitation ward had just survived severe neurological injuries, thus requiring frequent contact with rehabilitation professionals in the nursing and rehabilitation programs. This kind of necessary contact may increase the chance of infection. The heterogeneity of diseases and routine protection levels adopted by different wards before taking comprehensive strict protection measures also led to the incomparability among wards at the same institution. On the other hand, the analysis of risk factors for COVID-19 infection, such as BD, low modified Barthel Index, combined underlying diseases, and tracheotomy, still needs much evidence to support. At last, further data collection and complete analysis about all COVID-19–infected subjects in the rehabilitation delivery system in Wuhan are still needed. The much comprehensive understanding of the COVID-19 infection status and risk factors of BD inpatients in the rehabilitation ward of general hospitals depend on a comprehensive analysis in the future.
In conclusion, BD inpatients with impaired airways and low activity levels are more susceptible to COVID-19 and can easily become severely ill or even die. We look forward to the results of this retrospective analysis, which can provide useful information for other institutions that care for high-risk populations such as patients with BD.
Xiaohua Han, MD
Nan Xia, MS
Zejian Chen, BS
Department of Rehabilitation Medicine
Tongji Hospital, Tongji Medical College
Huazhong University of Science and
Technology, Wuhan
Hubei, China
Chu Pan, MD
Department of Radiology
Tongji Hospital, Tongji Medical College
Huazhong University of Science and
Technology, Wuhan
Hubei, China
Xiaolin Huang, PhD
Department of Rehabilitation Medicine
Tongji Hospital, Tongji Medical College
Huazhong University of Science and
Technology, Wuhan
Hubei, China
Footnotes
X. Han, NX, and ZC contributed equally to this study.
REFERENCES
- 1.Xiao Y Zhao K Ma ZX, et al. : Integrated medical rehabilitation delivery in China. Chronic Dis Transl Med 2017;3:75–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leung SO, Chan CC, Shah S: Development of a Chinese version of the modified Barthel Index—validity and reliability. Clin Rehabil 2007;21:912–22 [DOI] [PubMed] [Google Scholar]
- 3.Peng S Huang L Zhao B, et al. : Clinical course of coronavirus disease 2019 in 11 patients after thoracic surgery and challenges in diagnosis. J Thorac Cardiovasc Surg 2020;160:585–92.e2 [DOI] [PMC free article] [PubMed] [Google Scholar]


