Abstract
Coronavirus disease 2019 (COVID-19) was first detected in December 2019 in Wuhan, China, with 11,669,259 positive cases and 539,906 deaths globally as of July 8, 2020. The objective of the present study was to determine whether meteorological parameters and air quality affect the transmission of COVID-19, analogous to SARS. We captured data from 29 provinces, including numbers of COVID-19 cases, meteorological parameters, air quality and population flow data, between Jan 21, 2020 and Apr 3, 2020. To evaluate the transmissibility of COVID-19, the basic reproductive ratio (R0) was calculated with the maximum likelihood “removal” method, which is based on chain-binomial model, and the association between COVID-19 and air pollutants or meteorological parameters was estimated by correlation analyses. The mean estimated value of R0 was 1.79 ± 0.31 in 29 provinces, ranging from 1.08 to 2.45. The correlation between R0 and the mean relative humidity was positive, with coefficient of 0.370. In provinces with high flow, indicators such as carbon monoxide (CO) and 24-h average concentration of carbon monoxide (CO_24 h) were positively correlated with R0, while nitrogen dioxide (NO2), 24-h average concentration of nitrogen dioxide (NO2_24 h) and daily maximum temperature were inversely correlated to R0, with coefficients of 0.644, 0.661, −0.636, −0.657, −0.645, respectively. In provinces with medium flow, only the weather factors were correlated with R0, including mean/maximum/minimum air pressure and mean wind speed, with coefficients of −0.697, −0.697, −0.697 and −0.841, respectively. There was no correlation with R0 and meteorological parameters or air pollutants in provinces with low flow. Our findings suggest that higher ambient CO concentration is a risk factor for increased transmissibility of the novel coronavirus, while higher temperature and air pressure, and efficient ventilation reduce its transmissibility. The effect of meteorological parameters and air pollutants varies in different regions, and requires that these issues be considered in future modeling disease transmissibility.
Keywords: COVID-19, Basic reproductive ratio, Meteorological parameter, Air pollutant
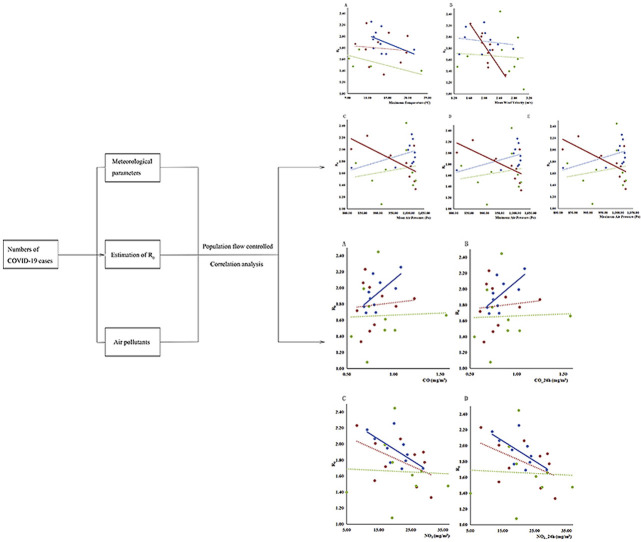
Graphical abstract
Highlights
-
•
COVID-19 is a worldwide pandemic, with transmission parameters largely remaining unknown.
-
•
We provide insight into the role of meteorological factors and air pollutants on COVID-19 transmissibility.
-
•
CO is positively while NO2 is inversely correlated with R 0.
-
•
Daily maximal temperature, wind speed and air pressure are inversely correlated with R 0.
-
•
Correlations vary by region.
1. Introduction
Coronavirus disease 2019 (COVID-19) was first detected in early December 2019 in Wuhan, China. The World Health Organization declared COVID-19 as a pandemic on March 11, 2020 (WHO, 2020b). As of July 8, 2020, 11,669,259 positive cases have been confirmed and 539,906 deaths reported globally (WHO, 2020c).
Although several studies have addressed various epidemic trends of COVID-19, its clinical characteristics, diagnostic tests, and therapeutic modalities, there is dearth of information on transmission dynamics of this novel virus. A previous study has estimated the outbreak size in Wuhan and the transmissibility of COVID-19 from confirmed cases in Wuhan to other cities in China (Wu et al., 2020). However, few studies have systematically assessed the correlation between the virus and meteorological conditions and air quality.
Exposure to climate changes and air pollution have been shown to be associated with the spread and prevalence of infectious diseases, hand-foot-mouth disease (HFMD) (Yu et al., 2019) and mumps (Hao et al., 2019), to name a few. Yet, whether these factors contribute to the transmissibility of the novel coronavirus has yet to be determined. Here, we addressed the impact of meteorological factors and air quality in several regions of Mainland China on COVID-19 transmissibility. We collected meteorological parameters and air quality indices between Jan 21, 2020 and Apr 3, 2020 in a number of Chinese provinces. The study objective was to analyze the relationship between these factors and the basic reproductive ratio (R 0) of COVID-19.
2. Methods
2.1. Source of data
The time interval required to calculate R 0 is from the first positive case confirmed until the number of cases returned to zero. Therefore, the numbers of confirmed positive cases, suspected cases, recovered cases and deaths due to COVID-19 were collected from January 21, 2020, to April 3, 2020, showing province-specific variations (Table A.1). The above data were extracted from websites of the National Health Commission of China(https://github.com/canghailan/Wuhan-2019-nCoV), and sorted out by province. Concomitantly, we collected meteorological data and air quality data for the same provinces.
Daily meteorological data included mean/maximum/minimum air pressure (kPa), mean/maximum/minimum temperature (°C), mean/minimum relative humidity (%), cumulative precipitation (mm), mean/maximum/extreme wind velocity (m/s), duration of sunshine (h), mean/maximum/minimum surface temperature (°C). The data above were extracted from daily datasets of climate from Chinese surface stations, downloaded from the National Meteorological Information Center (Version 3.0) (http://data.cma.cn/data/cdcdetail/dataCode/SURF_CLI_CHN_MUL_CES_V3.0.html).
Daily air quality data were listed in Table A.2. Provincial air quality data were obtained from the China National Urban Air Quality Real-time DAY e Publishing Platform, which belongs to China National Environmental Monitoring Center. Air quality data for Beijing were provided by the Beijing Environmental Protection Monitoring Center (http://beijingair.sinaapp.com/).
In addition, we collected information about Wuhan's population flow, including the provinces where Wuhan's population exported to and the corresponding proportions. The information was provided by the Baidu Migration (https://qianxi.baidu.com/2020/), and was collected between January 10, 2020 and January 24, 2020. It was a time period corresponding to festivities associated with the Chinese Spring Festival travel rush, and was also inclusive of a COVID-19 incubation period prior to the Government's imposed Wuhan's lockdown.
2.2. Statistical analysis
To evaluate the transmissibility of COVID-19, we used the basic reproductive ratio, R 0, which was calculated by the model developed by Ferrari et al. (2005), who proposed a maximum likelihood “removal” method for estimating R 0 for the simple epidemic based on the so-called “chain-binomial” model of infectious disease dynamics. The chain-binomial model is a discrete-time, stochastic alternative to the continuous-time, deterministic SIR model. The 95% confidence interval (CI) of R 0 was also estimated in this study. All analyses were completed by R soft version 3.6.2 (R Foundation for Statistical Computing). The correlations of R 0 and meteorological data, air quality data were described by Pearson Correlation Coefficient (r), or Spearman Correlation Coefficient (r s, if the data were not normally distributed), and the trend of R 0 with meteorological factors and air quality factors was plotted. All statistical analyses were performed using IBM SPSS Statistics version 23.0, and the figures were drawn with Microsoft Excel 2019. P values were 2-tailed with statistical significance set at P < 0.05.
3. Results
We used data from 29 provinces in mainland China. The Tibet Autonomous Region and Qing Hai Province were not included in the analyses as no COVID-19 positive cases were reported during the data collection period.
3.1. Estimation of R0 for COVID-19
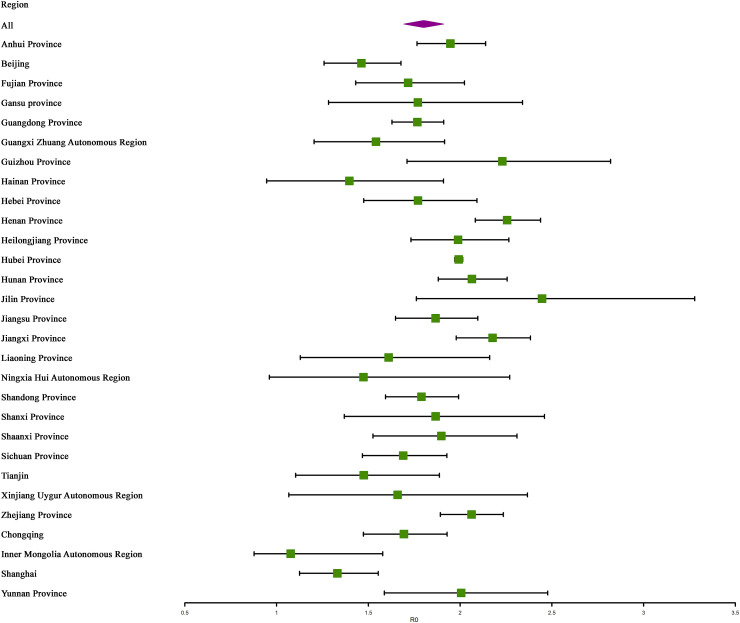
As depicted in Fig. 1 , the mean R 0 in the 29 provinces was 1.79 ± 0.31, ranging from 1.08 to 2.45. The 3 provinces with the highest R 0 were Jilin, Henan, and Guizhou, with mean R 0 of 2.45, 2.26, and 2.23, respectively.
Fig. 1.
The values of R0 in 29 provinces, China.
3.2. Correlations of daily meteorological, air quality data with R0 for COVID-19
There was a positive correlation between R 0 and the mean relative humidity, with a correlation coefficient of 0.370. No other meteorological parameters (Table 1 ) or air quality indices (Table 2 ) had a significant correlation with R 0.
Table 1.
Correlation analysis between R0 and daily meteorological data (n = 29).
| Index | Coefficient | P |
|---|---|---|
| Mean air pressure of the station | -0.122 | 0.528 |
| Maximum air pressure of the station | -0.129 | 0.505 |
| Minimum air pressure of the station | -0.129 | 0.576 |
| Mean temperature | -0.017a | 0.928 |
| Maximum temperature | −0.061a | 0.753 |
| Minimum temperature | 0.019a | 0.921 |
| Mean relative humidity | 0.370 | 0.048 |
| Minimum relative humidity | 0.229 | 0.232 |
| Cumulative precipitation | 0.221 | 0.249 |
| Mean wind velocity | −0.337a | 0.074 |
| Maximum wind speed | −0.336a | 0.075 |
| Extreme wind speed | −0.272a | 0.153 |
| Duration of sunshine | −0.196a | 0.307 |
| Mean surface temperature | −0.024a | 0.900 |
| Maximum surface temperature | −0.220a | 0.252 |
| Minimum surface temperature | 0.104a | 0.590 |
| Pressure difference | −0.123a | 0.524 |
| Temperature difference | −0.185a | 0.336 |
| Surface temperature difference | −0.370a | 0.048 |
The correlations were quantified by Pearson correlation coefficient (designated with “a”) or with Spearman correlation coefficient (no letter designation).
Table 2.
Correlation analysis between R0 and daily air quality data (n = 29).
| Index | Coefficient | P |
|---|---|---|
| AQI | 0.006a | 0.974 |
| CO | 0.145 | 0.452 |
| CO_24 h | 0.141 | 0.464 |
| NO2 | −0.320a | 0.090 |
| NO2_24 h | −0.318a | 0.092 |
| O3 | −0.171a | 0.375 |
| O3_24 h | −0.166 | 0.389 |
| O3_8 h | −0.166a | 0.389 |
| O3_8 h_24 h | −0.164a | 0.390 |
| PM10 | −0.013a | 0.948 |
| PM10_24 h | −0.002a | 0.990 |
| PM2.5 | 0.064a | 0.741 |
| PM2.5_24 h | 0.070a | 0.719 |
| SO2 | -0.064 | 0.741 |
| SO2_24 h | -0.063 | 0.745 |
The correlations were quantified by Pearson correlation coefficient (designated with “a”) or with Spearman correlation coefficient (no letter designation).
3.3. Factors associated with R0 for COVID-19 in different regions
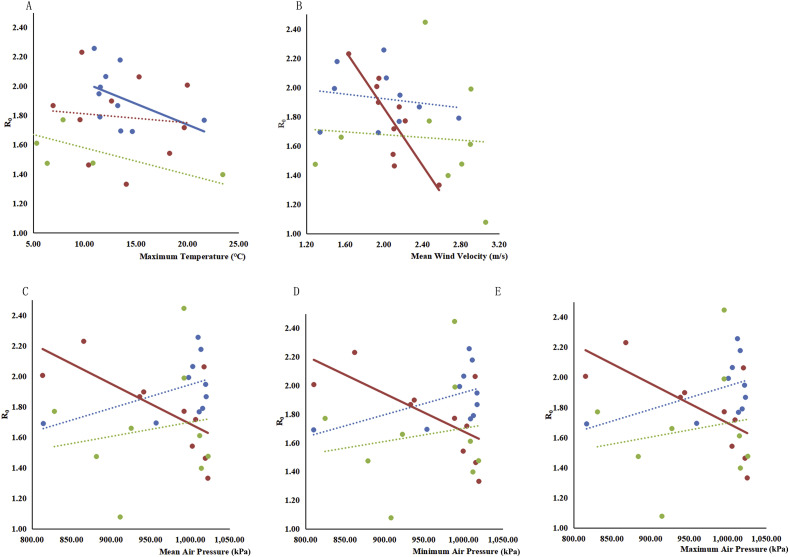
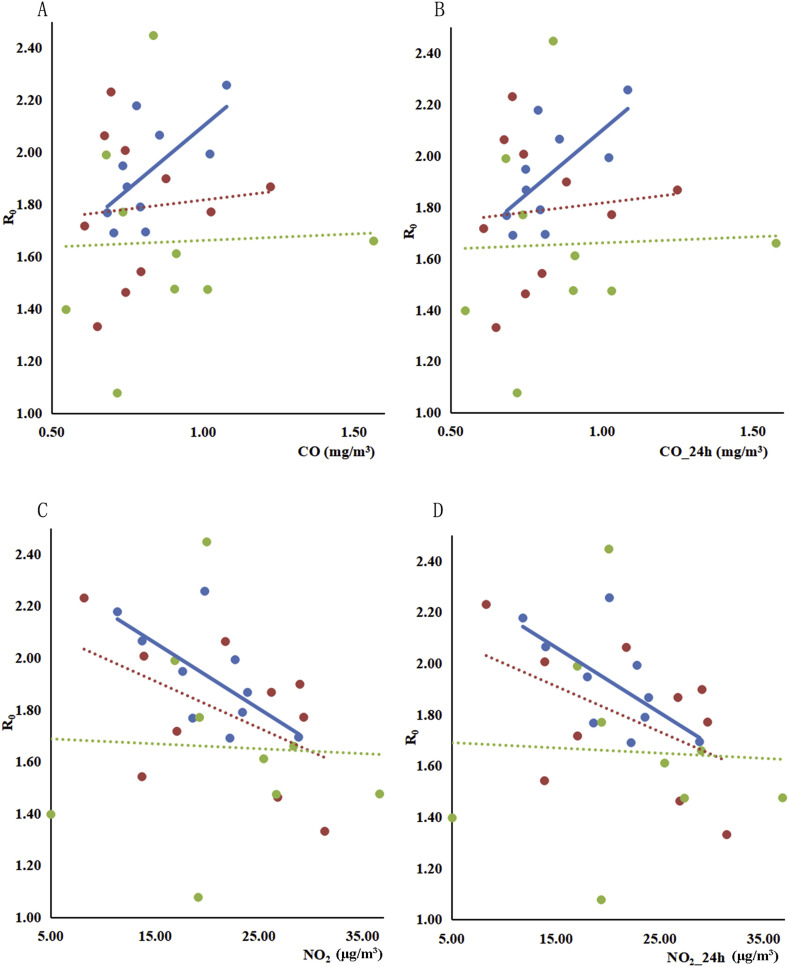
Based on the population export from Wuhan, we divided the 29 provinces into three subgroups, high, medium and low flow (Table A3), based on the percentile of the flow ratio; similar grouping methods have been previously reported (Yang et al., 2020). Air pollutants and meteorological parameters related to R 0 varied in the medium and high flow subgroups. In the high flow, indicators such as CO and CO_24 h were positively correlated with R 0, while NO2, NO2 24 h and daily maximum temperature were inversely related to R 0, with coefficients of 0.644, 0.661, −0.636, −0.657, and −0.645, respectively. With respect to the medium flow, only weather factors were associated with R 0, including mean/maximum/minimum air pressure and mean wind speed, with coefficients of −0.697, −0.697, −0.697, and −0.841, respectively. There was no association between R 0 and meteorological or air quality factors in the low flow subgroup (Table 3 and Table 4 ). The trend for R 0 and meteorological parameters or air pollutants noted above is also shown in Fig. 2 A–E and Fig. 3 A–D.
Table 3.
Correlation analysis between R0 and meteorological factors in the low, medium and high flow subgroups.
| Meteorological factors | Low flow(n = 9) |
Medium flow(n = 10) |
High flow(n = 10) |
|||
|---|---|---|---|---|---|---|
| Coefficient | P | Coefficient | P | Coefficient | P | |
| Mean air pressure of the station | 0.165a | 0.672 | −0.697 | 0.025 | 0.273 | 0.446 |
| Maximum air pressure of the station | 0.166a | 0.670 | −0.697 | 0.025 | 0.273 | 0.446 |
| Minimum air pressure of the station | 0.163a | 0.676 | −0.697 | 0.025 | 0.273 | 0.446 |
| Mean temperature | −0.400 | 0.286 | −0.118a | 0.746 | −0.321 | 0.365 |
| Maximum temperature | −0.370a | 0.327 | −0.100a | 0.784 | −0.636 | 0.048 |
| Minimum temperature | −0.400 | 0.286 | −0.079a | 0.829 | −0.269a | 0.453 |
| Mean relative humidity | 0.097a | 0.803 | 0.169a | 0.641 | 0.442 | 0.200 |
| Minimum relative humidity | 0.007a | 0.985 | 0.200 | 0.580 | 0.202a | 0.576 |
| Cumulative precipitation | 0.003a | 0.994 | −0.122a | 0.736 | 0.309 | 0.385 |
| Mean wind velocity | −0.217 | 0.576 | −0.841a | 0.002 | −0.173a | 0.633 |
| Maximum wind speed | −0.078a | 0.842 | −0.502a | 0.139 | −0.322a | 0.364 |
| Extreme wind speed | −0.183 | 0.637 | −0.264a | 0.461 | −0.294a | 0.410 |
| Duration of sunshine | 0.346a | 0.361 | −0.098a | 0.787 | −0.184a | 0.611 |
| Mean surface temperature | −0.267 | 0.488 | −0.074a | 0.839 | −0.527 | 0.117 |
| Maximum surface temperature | −0.503a | 0.167 | −0.036a | 0.922 | −0.624 | 0.054 |
| Minimum surface temperature | 0.150 | 0.700 | −0.025a | 0.945 | −0.237a | 0.510 |
| Pressure difference | 0.280a | 0.465 | −0.429a | 0.216 | −0.505a | 0.137 |
| Temperature difference | 0.012a | 0.976 | 0.008a | 0.983 | −0.125a | 0.732 |
| Surface temperature difference | −0.544a | 0.130 | −0.015a | 0.967 | −0.224 | 0.533 |
The correlations were quantified by Pearson's correlation coefficient (designated with “a”) or with Spearman correlation coefficient (no letter designation).
Table 4.
Correlation analysis between R0 and air quality factors in low, medium and high flow.
| Air quality factors | Low flow (n = 9) | Medium flow (n = 10) | High flow (n = 10) | |||
|---|---|---|---|---|---|---|
| Coefficient | P | Coefficient | P | Coefficient | P | |
| AQI | 0.019a | 0.961 | −0.149a | 0.681 | 0.401a | 0.251 |
| CO | 0.038a | 0.923 | 0.095a | 0.794 | 0.644a | 0.044 |
| CO_24 h | 0.036a | 0.927 | 0.100a | 0.784 | 0.661a | 0.038 |
| NO2 | −0.043a | 0.913 | −0.512a | 0.131 | −0.657a | 0.039 |
| NO2_24 h | −0.047a | 0.905 | −0.509a | 0.133 | −0.645a | 0.044 |
| O3 | 0.114a | 0.770 | −0.143a | 0.693 | 0.042a | 0.909 |
| O3_24 h | 0.004a | 0.991 | −0.135a | 0.711 | −0.213a | 0.555 |
| O3_8 h | 0.128a | 0.743 | −0.146a | 0.686 | 0.048a | 0.896 |
| O3_8 h_24 h | 0.176a | 0.650 | −0.157a | 0.665 | 0.014a | 0.970 |
| PM10 | 0.005a | 0.990 | −0.067 | 0.855 | 0.230a | 0.522 |
| PM10_24 h | 0.012a | 0.976 | −0.067 | 0.855 | 0.241a | 0.502 |
| PM2.5 | 0.053a | 0.893 | −0.152a | 0.675 | 0.459a | 0.182 |
| PM2.5_24 h | 0.052a | 0.894 | −0.141a | 0.697 | 0.469a | 0.171 |
| SO2 | 0.069a | 0.861 | 0.370 | 0.293 | −0.118a | 0.744 |
| SO2_24 h | 0.066a | 0.867 | 0.370 | 0.293 | −0.099a | 0.786 |
The correlations were quantified by Pearson correlation coefficient (designated with “a”) or with Spearman correlation coefficient (no letter designation).
Fig. 2.
The trend between R0 and meteorological factors. A. R0 and maximum temperature; B. R0 and mean wind velocity; C. R0 and mean air pressure; D. R0 and minimum air pressure; E. R0 and maximum air pressure. Blue, high flow; red, medium flow; green, low flow. Solid line means significant association between observation variable and COVID-19, dotted line means no significant association between observation variable and COVID-19. . (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Fig. 3.
The trend between R0 and air quality factors. A. R0 and CO; B. R0 and CO_24 h; C. R0 and NO2; D. R0 and NO2_24 h; Blue, high flow; red, medium flow; green, low flow. Solid line means significant association between observation variable and COVID-19, dotted line means no significant association between observation variable and COVID-19. . (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
4. Discussion
The COVID-19 pandemic continues to pose an urgent and enormous challenge worldwide. In this study, meteorological factors, such as relative humidity, air pressure, temperature, and air pollutants such as CO and NO2 were evaluated to determine their regional impact on the transmission of COVID-19.
R 0 is an important epidemiological value, which predicts the spreading potential of an infectious disease from a positive individual to an expected number of secondary cases. It quantifies the contagiousness or transmissibility of infectious agents. However, it has yet to be defined globally. Herein, the values of R 0 were similar to those reported on January 23, 2020 by the WHO (WHO, 2020a) and Yao et al. (2020), ranging between 1.4 and 2.5, and 0.6 to 2.5, respectively. Our values are lower than those obtained by Wu et al. (2020) and Zhao et al. (2020), who reported R 0 values of 2.68 (2.47, 2.86) and 3.58 (2.89, 4.39), respectively. Considering the longer observation time in our study (Jan 21, 2020 to Apr 3, 2020) vs. the others, the transmissibility may be subject to modification dependent upon the study duration (Steven Riley et al., 2003).
It is noteworthy, the R 0 in Hubei, where the province Wuhan is located, was 1.99, which is not in the top 3 highest values reported in China. R 0 is a threshold parameter representing the expected number of secondary cases generated, and generally, the larger the R 0, the more difficult it becomes to curtail the outbreak. However, R 0 is also modified by the contact rate (Steven Riley et al., 2003), which may explain why the Hubei R 0 was not within the highest range. Faced with the epidemic, the Chinese Authorities have implemented response measures nationwide, and more stringent public health interventions in Hubei province, especially in Wuhan. We analyzed the difference in the R 0 in the Hubei province pre- and post-lockdown, with corresponding R 0 of 3.20 vs. 1.85, respectively, corroborating this speculation. Moreover, in considering whether different interventions in Hubei vs. other provinces affect the correlation of R 0 values and meteorological or air quality factors, we compared the results with or without inclusion of Hubei province. The significant variables and the direction of their correlation coefficients were consistent in both cases.
In addition to the magnitude of the transmissibility, concern has been raised regarding the propensity of meteorological conditions to impact the transmissibility of COVID-19. Our findings establish that lower relative humidity, higher temperature, higher air pressure and higher wind speed decrease the spread of COVID-19.
Based on findings in previous studies, many infectious diseases have seasonal prevalence (Morawska et al., 2020), especially respiratory viral infections (Moriyama et al., 2020). For example, in 2003, when the weather turned warmer SARS infections decreased (Yuan et al., 2006). Our results showed a similar trend in provinces belonging to high flow, where an inverse association between R 0 and daily maximum temperature was found. In general, viruses are sensitive to high temperatures, making it more difficult for them to survive, consistent with our observations. In addition, colder weather favors human indoor activities, increasing the risk of infection (Bunker et al., 2016). Analogous conclusions to ours on the relationship between virus persistence in the environment and ambient temperature have been noted in several studies (Ma et al., 2020; Mohammad M. Sajadi et al., 2020). The incidence rate of positive case of COVID-19 ranged from 0 to 60% with daily maximal temperature between 12.2 °C and 22.8 °C; for an average increase of 1 °C in maximum temperature, the incidence rate decreased by −7.5% on the same day (Aurelio et al., 2020). However, other studies have noted contradictory findings, pointing to positive correlations between diurnal temperature range and COVID-19 daily deaths (Ma et al., 2020). Consistent with our findings, an earlier study (Liu et al., 2020) addressing the impact of meteorological factors on covid-19 transmission, after controlling for population migration in provincial capital cities in China, showed that low temperature, mild diurnal temperature range and low humidity favored COVID-19 transmission. In contrast, in a study performed in 122 Chinese cities, there was no evidence to support that COVID-19 case numbers decline with warmer weather (Xie and Zhu., 2020).
Humidity is another environmental factor that contributes to the seasonal nature of respiratory viral infections, including COVID-19 (Ma et al., 2020). In our analysis, mean relative humidity was correlated to R 0, but this relationship was not maintained after controlling for regional variables.
Average wind velocity and air pressure are also relevant weather parameters to the spread of COVID-19. Higher wind velocity is reflected in shorter suspension time of droplets in outdoor air, and better ventilation in indoor environments (Morawska et al., 2020), reducing the likelihood of infection. Air pressure is also a factor affecting COVID-19 transmissibility. For example, daily average air pressure has been shown to be inversely associated with secondary attack rate of SARS, OR = 0.53 (95% CI: 0.42 to 0.66) (Cai et al., 2007). The study inferred high air pressure may shorten the suspension time of droplets in air, analogous to wind velocity, reducing the transmissibility of SARS. But a contradictory study showed that increased maximum/minimum/mean atmospheric pressure may aggravate the epidemics of dengue (Zhu, 2019).
Air pollutants have been reported to correlate with several diseases, such as those of the cardiovascular (Zhang et al., 2019; Andersson et al., 2020) and respiratory systems (N. Chen et al., 2020), including COVID-19 (Martelletti et al., 2020). Exposure to air pollutants has been demonstrated to induce pulmonary oxidative stress, leading to production of free radicals, in turn injurying the respiratory system and reducing viral resistance (Ciencewicki et al., 2007). These correlations were also inherent to our study, showing regional characteristics (Ogen et al., 2020), analogous to the climate factors noted above. Subgroup analysis showed that frequent flow group CO, CO_24 h and R 0 were positively correlated,while NO2, NO2_24 h and R 0 were negatively correlated. No correlation was found between the air quality factors and R 0 in the medium flow group or the low flow group.
The production of CO is closely related to the incomplete combustion of fossil fuels, and is a ubiquitous environmental gaseous pollutant (Wu et al., 2005). Increased CO concentrations in the air were accompanied by increased R 0. Previous studies have indicated that CO exposure is associated with respiratory symptoms (Zhao et al., 2019; North et al., 2019; Lawin et al., 2018). Therefore, COVID-19 as a respiratory disease may be associated with high level CO exposure. CO exposure is associated with increased concentrations of endogenous CO, producing carboxyhemoglobin (COHb) and airway inflammatory diseases (Burnett et al., 1998; Zayasu et al., 1997). Recent studies have shown that high environmental CO concentrations trigger reactive oxygen species (ROS) generation and impaired myoglobin function (Piantadosi et al., 1995, 2008). In contrast, it has been reported that ambient CO is negatively- (Tian et al., 2014) or not-correlated with respiratory diseases (Chen et al., 2011), contradicting our findings. However, existing research cannot determine the association between ambient CO levels and human health, and further research on this issue is warranted.
However, different from CO, we observed a negative relationship between NO2 and COVID-19. In published studies, most results have shown no significant relationship with COVID-19; only a few found a positive correlation between NO2 and COVID-19 confirmed cases or death (Ogen et al., 2020; Zhu et al., 2020). In contrast, our study focused on the transmissibility of this virus, which has not been found to correlate with NO2 yet. NO2 was found to be negatively correlated with laboratory-confirmed influenza (Liu et al., 2018), corroborating in part our results. In addition, NO has been shown to inhibit the replication cycle of the severe acute respiratory syndrome coronavirus (SARS CoV) in vitro (Akerström et al., 2005). Thus, a similar mechanism may exist for NO2 and the novel Coronavirus. Additional research is needed to determine the biological mechanisms associated with this phenomenon.
Our study is divided into three subgroups of population movement between January10 to 24, 2020. No correlations were found between air quality and R 0 in the medium and low flow subgroups. This may reflect the fact that the population that exported from Wuhan was the main infection source in other cities and provinces (Z. L. Chen et al., 2020), causing frequent flow groups to have a larger R 0 (Spearman correlation analysis results suggest that R 0 is positively correlated with different flow areas r s = 0.392, P = 0.035). On the other hand, although the improvement of air quality may reduce the R 0, the impact caused by the flow of people may be sufficiently great, and therefore mask the impact in air quality of the improvement. Further it may contribute to the impression that R 0 is rising although the environmental conditions are improving,(reduced CO and NO2 levels, etc. (Dutheil et al., 2020, NASA, 2020, Tobías et al., 2020).
5. Limitations
The present study has several limitations. First, exposure to meteorological environment or air pollution at individual level is difficult to obtain and quantified. The results are presented at the group level, which may lead to an ecological fallacy, which arises when an inference is made about an individual based on analyses of group data, to which a given individual belongs. However, considering the current urgency in understanding the novel coronavirus, ecological studies are necessary and invaluable tools. Second, since COVID-19 is caused by the virus SARS CoV-2, more factors are needed to be investigated, such as viral resistance, population mobility, population immunity level, public interventions, medical resources, among others. It is noteworthy, public health interventions implemented by the Chinese government such as traffic restriction, social distancing measures, home isolation and centralized quarantine, extensive health education, as well as rigorous measures in public places, played an important role in mitigating the spread of COVID-19 (Pan et al., 2020; Maier et al., 2020). Considering that all provinces have quickly adopted first-level response measures to the virus, we believe the impacts of these interventions were comparable across provinces. Nevertheless, this study aimed to highlight the impact of air pollutants and meteorological parameters on COVID-19, thus it is important and acceptable to focus on these factors. Furthermore, we have selected the most representative indicator R 0 to describe the transmission capacity, and as one of the main indicators of infectious disease, we have partially considered population mobility by conducting subgroup analysis. Finally, the information on comorbidities in these populations were not collected in our study, which should also be considered in the observed differences between regions. However, this study is just a preliminary analysis. For sounder conclusions, additional studies will require analysis over a more protracted time with bigger data sets. Overall, this study has shown that meteorological factors such as relative humidity, air pressure, temperature, and air pollutants such as CO and NO2 may affect the transmission of COVID-19, differing among various provinces. Nonetheless, we emphasize the need for further investigation on the transmissibility of COVID-19 and its relationship to meteorological factors and air pollutants.
6. Conclusion
We conducted an observational study on the correlation between COVID-19 and ecological indicators such as meteorological parameters and air quality, reflecting the most comprehensive study to date on the role of meteorological parameters and air quality factors in COVID-19. We conclude that high carbon monoxide concentration is a risk factor, whilst higher temperatures, increased air pressure and better ventilation may reduce the transmissibility of the novel coronavirus. The effect of meteorological parameters and air pollutants varies in different Chinese provinces and should be considered in future studies on COVID-19 transmissibility.
Author statement
Shaowei Lin: Software, Writing - original draft. Donghong Wei: Software, Writing - original draft, Investigation. Yi Sun: Software, Writing - original draft, Investigation. Kun Chen: Data curation, Investigation. Le Yang: Data curation, Investigation. Bang Liu: Data curation, Investigation. Qing Huang: Data curation, Investigation. Monica Maria Bastos Paoliello: Writing- Reviewing and Editing. Huangyuan Li: Conceptualization, Methodology, Writing- Reviewing and Editing. Siying Wu: Conceptualization, Methodology, Writing- Reviewing and Editing. All authors contributed to critical revision of the final manuscript and approved the final version of the manuscript.
Declaration of competing interest
The authors declare that they have no conflict of interest.
Acknowledgement
This study was supported by Joint Funds for the Innovation of Science and Technology, Fujian Province (2018Y9089; 2017Y9105) and National Natural Science Foundation of China (81973083).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ecoenv.2020.111035.
Consent for publication
Not applicable.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Akerström S. Nitric oxide inhibits the replication cycle of severe acute respiratory syndrome coronavirus. J. Virol. 2005;79(3):1966–1969. doi: 10.1128/JVI.79.3.1966-1969.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson E.M. Road traffic noise, air pollution and cardiovascular events in a Swedish cohort. Environ. Res. 2020;185:109446. doi: 10.1016/j.envres.2020.109446. [DOI] [PubMed] [Google Scholar]
- Aurelio T. Is temperature reducing the transmission of COVID-19? Environ. Res. 2020;186:109553. doi: 10.1016/j.envres.2020.109553. https://linkinghub.elsevier.com/retrieve/pii/S0013935120304461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunker A. Effects of air temperature on climate-sensitive mortality and morbidity outcomes in the elderly; a systematic review and meta-analysis of epidemiological evidence. EBioMedicine. 2016;6:258–268. doi: 10.1016/j.ebiom.2016.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnett R.T. The association between ambient carbon monoxide levels and daily mortality in Toronto, Canada. J. Air Waste Manag. Assoc. 1998;48:689–700. doi: 10.1080/10473289.1998.10463718. [DOI] [PubMed] [Google Scholar]
- Cai Q.C. Influence of meteorological factors and air pollution on the outbreak of severe acute respiratory syndrome. Publ. Health. 2007;121:258–265. doi: 10.1016/j.puhe.2006.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen N. Impact of air pollutants on pediatric admissions for Mycoplasma pneumonia: a cross-sectional study in Shanghai, China. BMC Publ. Health. 2020;20:447. doi: 10.1186/s12889-020-8423-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen R. Ambient carbon monoxide and daily mortality in three Chinese cities: the China air pollution and health effects study (CAPES) Sci. Total Environ. 2011;409:4923–4928. doi: 10.1016/j.scitotenv.2011.08.029. [DOI] [PubMed] [Google Scholar]
- Chen Z.L. Distribution of the COVID-19 epidemic and correlation with population emigration from wuhan, China. Chin Med J (Engl) 2020 doi: 10.1097/CM9.0000000000000782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciencewicki J. Air pollution and respiratory viral infection. Inhal. Toxicol. 2007;19:1135–1146. doi: 10.1080/08958370701665434. [DOI] [PubMed] [Google Scholar]
- Dutheil F. COVID-19 as a factor influencing air pollution? Environ. Pollut. 2020;263:114466. doi: 10.1016/j.envpol.2020.114466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrari M.J. Estimation and inference of R0 of an infectious pathogen by a removal method. Math. Biosci. 2005;198:14–26. doi: 10.1016/j.mbs.2005.08.002. [DOI] [PubMed] [Google Scholar]
- Hao J. The association between short-term exposure to ambient air pollution and the incidence of mumps in Wuhan, China: a time-series study. Environ. Res. 2019;177:108660. doi: 10.1016/j.envres.2019.108660. [DOI] [PubMed] [Google Scholar]
- Lawin H. Comparison of motorcycle taxi driver's respiratory health using an air quality standard for carbon monoxide in ambient air: a pilot survey in Benin. Pan Afr Med J. 2018;30:113. doi: 10.11604/pamj.2018.30.113.14975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J.T. Impact of meteorological factors on the COVID-19 transmission: a multi-city in China. Sci. Total Environ. 2020;726:138513. doi: 10.1016/j.scitotenv.2020.138513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X.X. Effects of air pollutants on occurrences of influenza-like illness and laboratory-confirmed influenza in Hefei, China. Int. J. Biometeorol. 2018;63:1. doi: 10.1007/s00484-018-1633-0. [DOI] [PubMed] [Google Scholar]
- Maier B.F. Effective containment explains subexponential growth in recent confirmed COVID-19 cases in China. Science. 2020;368:6492. doi: 10.1126/science.abb4557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martelletti L. Air pollution and the novel Covid-19 disease: a putative disease risk factor. SN Compr Clin Med. 2020 doi: 10.1007/s42399-020-00274-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morawska L. Airborne transmission of SARS-CoV-2: the world should face the reality. Environ. Int. 2020;139:105730. doi: 10.1016/j.envint.2020.105730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moriyama M. Seasonality of respiratory viral infections. Annu Rev Virol. 2020 doi: 10.1146/annurev-virology-012420-022445. [DOI] [PubMed] [Google Scholar]
- NASA . 2020. Airborne Nitrogen Dioxide Plummets over China. [Google Scholar]
- North C.M. Personal carbon monoxide exposure, respiratory symptoms, and the potentially modifying roles of sex and HIV infection in rural Uganda: a cohort study. Environ. Health. 2019;18:73. doi: 10.1186/s12940-019-0517-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogen Y. Assessing nitrogen dioxide (NO) levels as a contributing factor to coronavirus (COVID-19) fatality. Sci. Total Environ. 2020;726:138605. doi: 10.1016/j.scitotenv.2020.138605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan A. Association of public health interventions with the epidemiology of the COVID-19 outbreak in wuhan, China. J. Am. Med. Assoc. 2020 doi: 10.1001/jama.2020.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piantadosi C.A. Carbon monoxide, reactive oxygen signaling, and oxidative stress. Free Radic. Biol. Med. 2008;45:562–569. doi: 10.1016/j.freeradbiomed.2008.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piantadosi C.A. Hydroxyl radical production in the brain after CO hypoxia in rats. Free Radic. Biol. Med. 1995;18:603–609. doi: 10.1016/0891-5849(95)00168-w. [DOI] [PubMed] [Google Scholar]
- Riley S. Transmission dynamics of the etiological agent of SARS in Hong Kong: impact of public health interventions. Science. 2003;300:1961–1966. doi: 10.1126/science.1086478. [DOI] [PubMed] [Google Scholar]
- Sajadi M.M. Temperature, humidity and latitude analysis to predict potential spread and seasonality for COVID-19. 2020. https://ssrn.com/abstract=3550308 Available at: SSRN: [DOI] [PMC free article] [PubMed]
- Tian L. Ambient carbon monoxide and the risk of hospitalization due to chronic obstructive pulmonary disease. Am. J. Epidemiol. 2014;180:1159–1167. doi: 10.1093/aje/kwu248. [DOI] [PubMed] [Google Scholar]
- Tobías A. Changes in air quality during the lockdown in Barcelona (Spain) one month into the SARS-CoV-2 epidemic. Sci. Total Environ. 2020;726:138540. doi: 10.1016/j.scitotenv.2020.138540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Coronavirus disease 2019 (COVID-19) situation report-3. 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200123-sitrep-3-2019-ncov.pdf?sfvrsn=d6d23643_8
- WHO Coronavirus disease 2019 (COVID-19) situation report-51. 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10
- WHO Coronavirus disease 2019 (COVID-19) situation report-98. 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200708-covid-19-sitrep-170.pdf?sfvrsn=bca86036_2
- Wu J.T. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020;395:689–697. doi: 10.1016/S0140-6736(20)30260-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu L. Carbon monoxide: endogenous production, physiological functions, and pharmacological applications. Pharmacol. Rev. 2005;57:585–630. doi: 10.1124/pr.57.4.3. [DOI] [PubMed] [Google Scholar]
- Xie J.G. Assciation between ambient temperature and COVID-19 infection in 122 cities from China. Sci. Total Environ. 2020;724:138201. doi: 10.1016/j.scitotenv.2020.138201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang L. Prevalence of incorrect posture among children and adolescents: finding from a large population-based study in China. IScience. 2020;23:101043. doi: 10.1016/j.isci.2020.101043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao Y. No association of COVID-19 transmission with temperature or UV radiation in Chinese cities. Eur. Respir. J. 2020 doi: 10.1183/13993003.00517-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu G. Short-term effects of meteorological factors and air pollution on childhood hand-foot-mouth disease in Guilin, China. Sci. Total Environ. 2019;646:460–470. doi: 10.1016/j.scitotenv.2018.07.329. [DOI] [PubMed] [Google Scholar]
- Yuan J. A climatologic investigation of the SARS-CoV outbreak in Beijing, China. Am. J. Infect. Contr. 2006;34:234–236. doi: 10.1016/j.ajic.2005.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zayasu K. Increased carbon monoxide in exhaled air of asthmatic patients. Am. J. Respir. Crit. Care Med. 1997;156:1140–1143. doi: 10.1164/ajrccm.156.4.96-08056. [DOI] [PubMed] [Google Scholar]
- Zhang J.Y. The acute health effects of ozone and PM2.5 on daily cardiovascular disease mortality: a multi-center time series study in China. Ecotoxicol. Environ. Saf. 2019;174:218–223. doi: 10.1016/j.ecoenv.2019.02.085. [DOI] [PubMed] [Google Scholar]
- Zhao Y. Ambient carbon monoxide and increased risk of daily hospital outpatient visits for respiratory diseases in Dongguan, China. Sci. Total Environ. 2019;668:254–260. doi: 10.1016/j.scitotenv.2019.02.333. [DOI] [PubMed] [Google Scholar]
- Zhu B.H. Prediction model for dengue fever based on interactive effects between multiple meteorological factors in Guangdong, China (2008–2016) PLoS ONE. 2019;14(12) doi: 10.1371/journal.pone.0225811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y.J. Association between short-term exposure to air pollution and COVID-19 infection: evidence from China. Sci. Total Environ. 2020;727 doi: 10.1016/j.scitotenv.2020.138704. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.