Abstract
BACKGROUND
Malaria pathogenicity is determined, in part, by the adherence of Plasmodium falciparum–infected erythrocytes to the microvasculature mediated via specific interactions between P. falciparum erythrocyte membrane protein (PfEMP1) variant domains and host endothelial receptors. Naturally acquired antibodies against specific PfEMP1 variants can play an important role in clinical protection against malaria.
METHODS
We evaluated IgG responses against a repertoire of PfEMP1 CIDR domain variants to determine the rate and order of variant-specific antibody acquisition and their association with protection against febrile malaria in a prospective cohort study conducted in an area of intense, seasonal malaria transmission.
RESULTS
Using longitudinal data, we found that IgG antibodies against the pathogenic domain variants CIDRα1.7 and CIDRα1.8 were acquired the earliest. Furthermore, IgG antibodies against CIDRγ3 were associated with reduced prospective risk of febrile malaria and recurrent malaria episodes.
CONCLUSION
This study provides evidence that acquisition of IgG antibodies against PfEMP1 variants is ordered and demonstrates that antibodies against CIDRα1 domains are acquired the earliest in children residing in an area of intense, seasonal malaria transmission. Future studies will need to validate these findings in other transmission settings and determine the functional activity of these naturally acquired CIDR variant–specific antibodies.
TRIAL REGISTRATION
ClinicalTrials.gov NCT01322581.
FUNDING
Division of Intramural Research, National Institute of Allergy and Infectious Diseases, NIH.
Keywords: Immunology, Infectious disease
Keywords: Adaptive immunity, Immunoglobulins, Malaria
A prospective study in Mali revealed early acquisition of IgG to PfEMP1 CIDRα1.7 and CIDRα1.8 and an association of IgG to CIDRγ3 with malaria protection.
Introduction
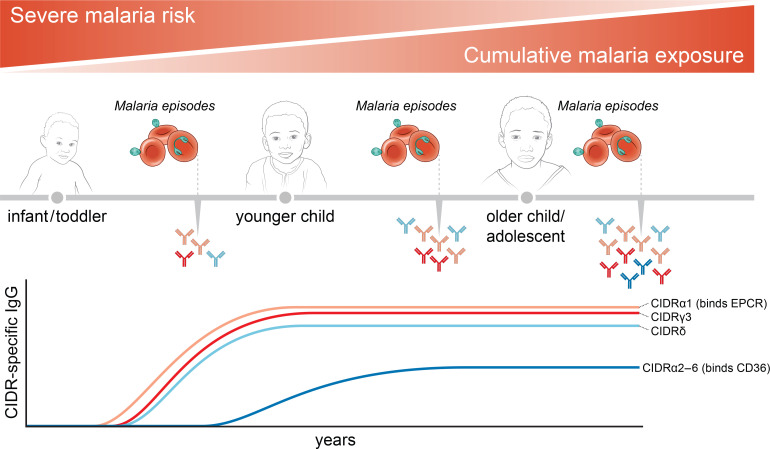
Malaria due to Plasmodium falciparum causes more than 400,000 deaths per year (1). Severe clinical manifestations of P. falciparum malaria are precipitated by widespread sequestration of infected erythrocytes (IEs) in host microvasculature, including in the brain and placenta, which can lead to cerebral malaria and placental malaria, respectively (2). Cytoadherence of IEs occurs via specific interactions between host endothelial receptors and P. falciparum erythrocyte membrane protein (PfEMP1), a parasite-derived protein expressed on the surface of IEs that is a major target of naturally acquired immunity to malaria (3–5). The PfEMP1 adhesins are encoded by approximately 60 var gene variants that differ within and between parasite genomes and that are expressed in a mutually exclusive manner within each IE (6–8). Switching between var genes aids in parasite immune evasion and functional diversification of the PfEMP1 family has resulted in mutually exclusive receptor-binding phenotypes correlated with differences in clinical severity (9, 10).
Members of the PfEMP1 family vary in the size and number of extracellular Duffy-binding-like (DBL) and cysteine-rich interdomain region (CIDR) domains (11). DBL and CIDR domains are classified based on sequence similarity into 6 (α, β, γ, δ, ε, ξ) and 4 (α, β, γ, δ) main classes, respectively, of which some can be further divided into subclasses (e.g., CIDRα1.1) (12, 13). PfEMP1 generally has a semiconserved head structure near the N-terminus consisting of a tandem DBLα-CIDR domain. This can be followed by a second DBLδ-CIDR tandem domain or additional other types of DBL domains in larger proteins. Notably, however, the VAR2CSA PfEMP1 variants do not contain typical CIDR domains and bind placental chondroitin sulfate A via specialized DBL domains (14, 15). PfEMP1 has diversified to bind the endothelial protein C receptor (EPCR) (10), the scavenger receptor CD36 (16), or yet undermined receptors via head structure CIDR domains. These phenotypes are maintained by the chromosomal organization of the var genes (17). Among the subtelomeric var genes, group A genes transcribed toward the telomere encode DBLα1-CIDRα1 head structures binding to EPCR or DBLα1-CIDRβ/γ/δ head structures, with unknown endothelial receptor specificities. Subtelomeric group B var genes transcribed toward the centromere as well as centromeric group C var genes encode DBLα0-CIDRα2-6 head structures binding to CD36. In addition to this, chimeric group B/A var genes encode EPCR-binding DBLα0-CIDRα1 head structures. The EPCR-binding phenotype has been implicated in severe malaria (18–21), whereas CD36 binding has been associated with uncomplicated malaria (22, 23). Severe malaria has been associated with rosetting, a phenomenon with unclear clinical significance that involves binding between an IEs and several uninfected erythrocytes. A set of group A PfEMP1 with DBLα1-CIDRβ/γ/δ domains has been shown to mediate rosettes.
Immunity to severe malaria is generally acquired after only 1 or 2 severe episodes (24), with naturally acquired antibodies specific for PfEMP1 variants likely playing an important role in clinical protection (25). Antibodies against group A PfEMP1 variants tend to be acquired before antibodies against group B and C variants (26) and are associated with protection from severe malaria (27). Similarly, antibodies against EPCR-binding CIDRα1 domains are acquired more rapidly than antibodies against other CIDR domains in areas of high malaria transmission intensity and are boosted by severe malaria but not uncomplicated malaria (28, 29). However, a recent study showed that antibodies against both rosetting-associated DBLα variants and CD36-binding CIDR domains predicted reduced risk of severe malaria to a similar extent as antibodies against EPCR-binding CIDR domains (30). The same study also showed that antibodies against group 2 DBLα variants, which are associated with rosetting (31), also predicted protection from uncomplicated malaria.
To gain further insight into the role of PfEMP1-variant specific antibodies, we assessed IgG responses against a repertoire of PfEMP1 CIDR domains to determine the rate and order of variant-specific antibody acquisition and their association with protection against uncomplicated febrile malaria in a prospective cohort study conducted in a Malian village with intense and seasonal malaria transmission.
Results
IgG antibodies specific for CIDRα1, CIDRδ, and CIDRγ domain variants are acquired rapidly.
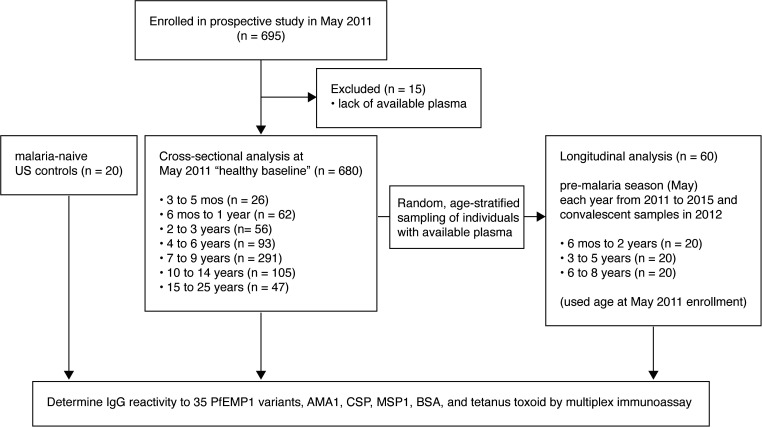
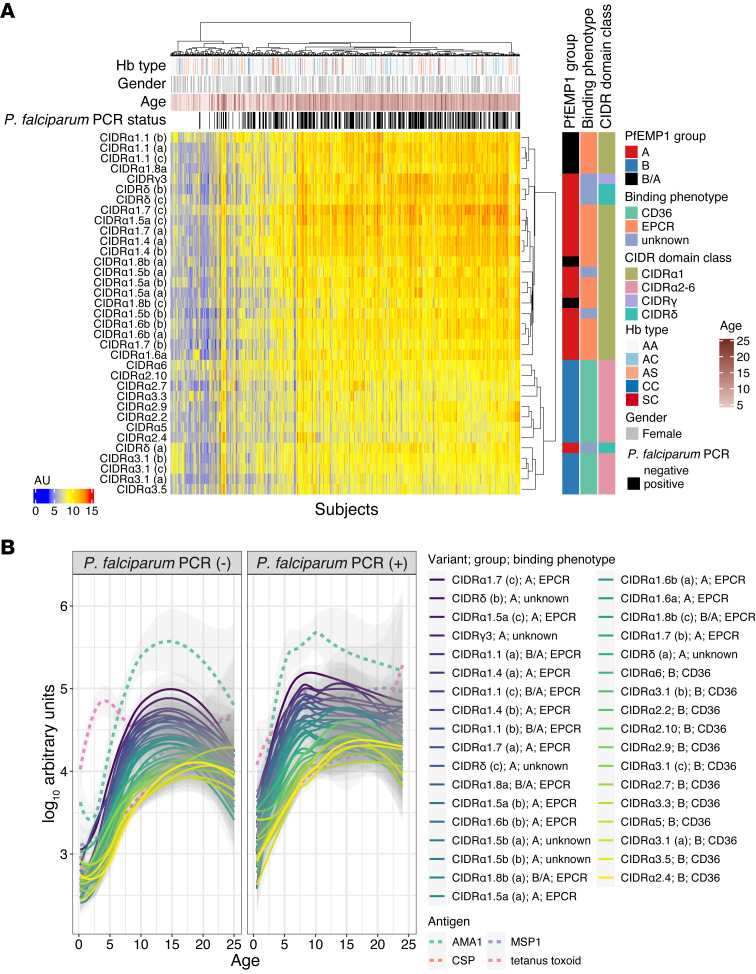
Naturally acquired IgG antibody responses to 35 PfEMP1 CIDR domain variants representing subtypes α, γ, and δ CIDR as well as 3 well-studied P. falciparum antigens (circumsporozoite protein [PfCSP], apical membrane protein 1 [PfAMA1], and merozoite surface protein 1 [PfMSP1]), tetanus toxoid (nonmalaria positive control), and BSA (nonspecific background control; Supplemental Table 1; supplemental material available online with this article; https://doi.org/10.1172/jci.insight.137262DS1) were determined by multiplex bead–based immunoassay in 680 children and adults from the Kalifabougou, Mali, cohort at their healthy baseline in May 2011 (Figure 1). Hierarchical clustering of baseline PfEMP1-specific IgG reactivity revealed distinct clustering of samples by age and by the presence of PCR-documented, asymptomatic P. falciparum infection as well as clustering of antigen targets by group (A, B, or B/A), binding phenotype (EPCR, CD36, or unknown), and CIDR domain class (Figure 2A), suggesting differential rates of acquisition of IgG between PfEMP1 variants with cumulative P. falciparum exposure and the acquisition of clinical immunity to malaria. PfEMP1-specific IgG reactivity increased rapidly up to 8 years of age, and within each age stratum, P. falciparum PCR–positive individuals exhibited greater variant-specific IgG reactivity than uninfected individuals (Figure 2B).
Figure 1. Study design.
Participants and time points for used for “healthy baseline” and longitudinal analysis.
Figure 2. IgG antibodies against PfEMP1 variants belonging to the A or B/A groups or having the EPCR-binding phenotype are rapidly acquired during childhood.
(A) Hierarchical clustering heatmap showing IgG reactivity to each of the 35 PfEMP1 variants in 680 subjects at enrollment (May 2011 healthy baseline). Clustering was performed using the Ward.D method and the Pearson distance metric. AU refers to arbitrary concentration units, which were calculated by fitting data to a dilutional standard curve of pooled hyperimmune plasma from malaria-exposed Malian adults. (B) IgG reactivity obtained at May 2011 healthy baseline versus age for each PfEMP1 variant (solid lines) or control antigen (dotted lines) with loess fit curves and 95% confidence intervals by P. falciparum PCR status determined at enrollment.
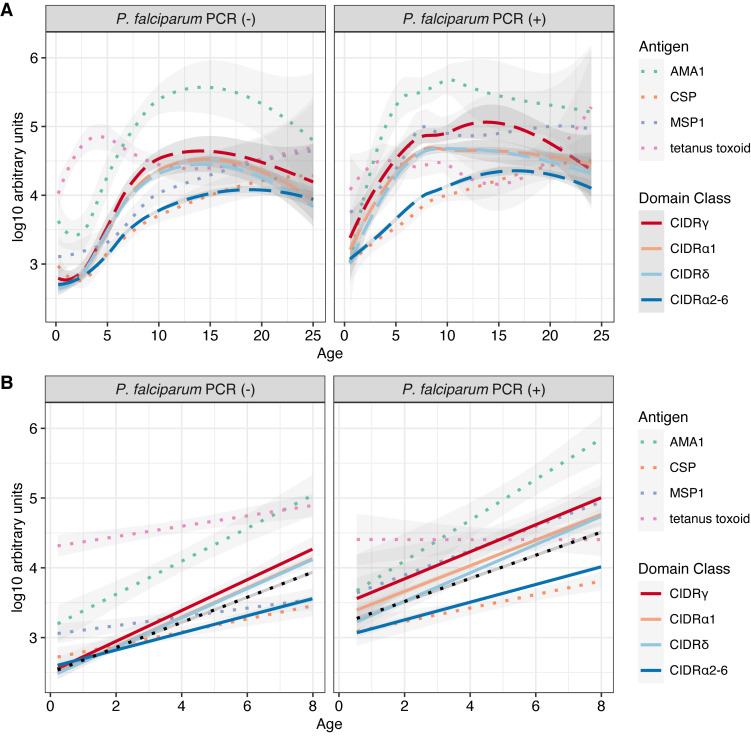
Categorization of PfEMP1 variants by CIDR domain class suggested that IgG specific for variants in the CIDRγ, CIDRα1, and CIDRδ classes was acquired rapidly, whereas IgG specific for group B variants of the CIDRα2-6 class was acquired slowly irrespective of P. falciparum infection status (Figure 3A). Indeed, when compared with variants of other domain classes within the linear range of the fit curves (<8 years of age), IgG specific for variants within each of the CIDRγ, CIDRα1, and CIDRδ classes increased significantly more rapidly with age, whereas IgG specific for variants of the CIDRα2-6 classes increased significantly more slowly with age, independent of P. falciparum infection status (Figure 3B and Supplemental Table 2). To test whether acquisition of IgG was different between each CIDR class, we compared the slopes for each CIDR directly in a pairwise manner and found significant differences in slopes between CIDRα2-6 and each of the other 3 classes but not between any of the CIDRγ, CIDRα1, and CIDRδ classes (Supplemental Table 3). Of note, IgG specific for AMA1, CSP, and MSP1 increased predictably with age in early childhood and plateaued in adolescence or young adulthood, which is similar to what we previously observed in this cohort (32, 33) (Figure 2B and Figure 3A). As we observed previously by ELISA in a separate cohort in Mali (34), increases in tetanus toxoid–specific IgG in early childhood and adolescence corresponded with the primary childhood vaccine series (diphtheria, tetanus, pertussis) and a subsequent booster of a tetanus toxoid–containing vaccine in females of child-bearing age (Figure 2B and Figure 3A).
Figure 3. IgG antibodies against CIDRα2-6 variants are acquired more slowly during childhood.
(A) IgG reactivity obtained at May 2011 healthy baseline versus age for each CIDR domain class (dashed lines) or control antigen (dotted lines) with loess fit curves and 95% confidence intervals by P. falciparum PCR status determined at enrollment. (B) Linear portion of plot in A (age range 3 months to 8 years), with regression lines and 95% confidence intervals (see Supplemental Table 2). For comparison, a regression line for all variants together is represented by the black dotted line.
With the exclusion of the youngest children (<6 months), whose IgG is most likely maternally derived, ranking of antigens by decreasing seropositivity within each age group revealed immunodominance of CIDRα1 domain classes, which are all either of the A or B/A var group, in early childhood (<7 years) that is maintained to a large degree in adolescence and early adulthood (Supplemental Figure 1). Notably, the most prevalent PfEMP1-specific IgG reactivity among individuals aged more than 1 year was against CIDRα1.7(c), with seroprevalence rapidly rising from 25% in 2- to 3-year-old children to 60% in 4- to 6-year-old children and surpassing 95% in older children and adults (Supplemental Figure 1). However, the majority of individuals within the oldest age group (15–25 years) were also seropositive for several variants within the CIDRα2-6 domain classes, suggesting that IgG antibodies against these variants are eventually acquired with additional years of malaria exposure.
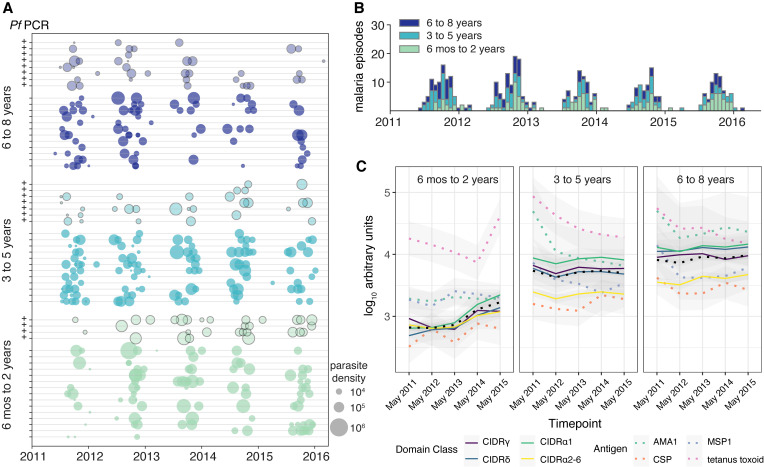
To assess the longitudinal acquisition of variant-specific IgG, we determined variant-specific IgG reactivity across 5 annual cross-sectional surveys conducted just before each malaria transmission season for an age-stratified random sample of 60 children from the entire cohort (Figure 1). Children in this subset experienced a median of 6 febrile malaria episodes (interquartile range, 4−9 episodes) with a broad range of parasite densities and a wide distribution (Figure 4A) punctuated by clear seasonal peaks in the number of episodes during the 5-year surveillance period (Figure 4B). In the youngest children (6 months to 2 years), IgG specific for variants of the CIDRα1 and CIDRδ domain classes began low and then increased rapidly over 4 malaria seasons, whereas IgG specific for CIDRγ initially decreased during the first 2 years before rising during the third year of surveillance (Figure 4C). In contrast, older children (3–8 years) appeared to maintain stable levels of IgG specific for all PfEMP1 variants over 4 malaria seasons (Figure 4C). Children in the youngest age group never achieved the same levels of PfEMP1-specific antibodies by the end of the surveillance period (May 2015) as children who began the study as 3- to 5-year-olds (Figure 4C), which may be indicative of decreased malaria incidence during the surveillance period compared with before the start of the cohort study. This observation may be attributable to either intensive active and passive case detection during the study period or due to natural decreases in malaria transmission.
Figure 4. Longitudinal analysis of PfEMP1 variant–specific IgG over multiple malaria seasons.
IgG reactivity specific to PfEMP1 variants was determined for 60 children ages 6 months to 8 years at 5 cross-sectional surveys before the malaria season. (A) Malaria incidence over 5 malaria seasons for 60 children aged 6 months to 2 years; 3–5 years; and 6–8 years (n = 20 per age group). Plus signs along the left margin indicate subjects with asymptomatic P. falciparum parasitemia at enrollment. The bubble area is proportional to parasite density determined at each visit. (B) The number of malaria episodes per 2-week period by age group over 5 malaria seasons. (C) Longitudinal IgG reactivity at 5 cross-sectional surveys in the same children.
Acquisition of IgG antibodies against CIDR domain classes is highly ordered, with IgG against EPCR-binding domain variants CIDRα1.7 and CIDRα1.8 acquired first.
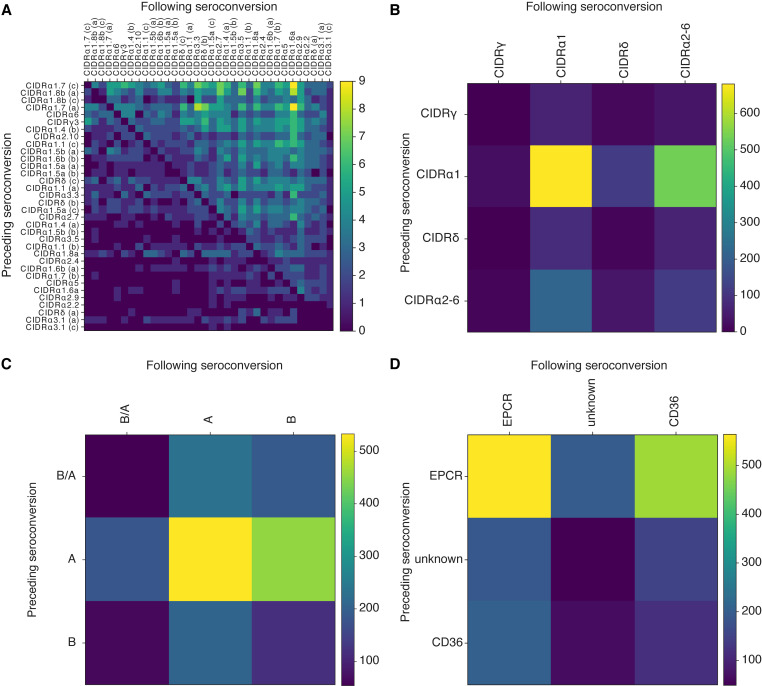
We next asked whether IgG antibodies against individual PfEMP1 variants were acquired in a particular order. We computed a consensus order of acquisition of antibodies of PfEMP1 variants across all subjects using an approach called minimum violations ranking (MVR; see Methods). This approach produced both a consensus order and a score representing how well the data align with that consensus. We then repeatedly randomized the order of antibody acquisition within each subject and recomputed the best-fit consensus and score. We observed that the consensus score was significantly stronger using real seroconversion data than under randomizations, which highly suggests a hierarchical exposure to different parasite CIDR domains in this population (Figure 5 and Supplemental Figure 2, A–D). At the variant level, IgG specific to CIDRα1.7(c) was acquired first, followed by IgG specific to CIDRα1.8b(a), CIDRα1.8b(c), CIDRα1.7(a), CIDRα6, and CIDRγ3 (Figure 5A). Grouped by CIDR domain class, IgG was acquired against CIDRγ first, followed by CIDRα1, CIDRδ, and CIDRα2-6 (Figure 5B). Grouped on the basis of upstream sequence, IgG was acquired against B/A first, followed by A and B (Figure 5C). Finally, when variants were grouped by binding phenotype, IgG against EPCR-binding domains was acquired first, followed by domains with unknown binding phenotypes and CD36-binding domains (Figure 5D). Whether this reflects differential prevalence of variants in the parasite population or age-specific expression patterns remains an open question.
Figure 5. Longitudinal acquisition of IgG antibodies against specific PfEMP1 variants is hierarchical.
Using longitudinal data, seropositivity was determined for each variant within each subject at each time point to determine the year of seroconversion. Seroconversion year was then used to generate a matrix representing the number of times that seroconversion for a variant (rows) precedes another variant (column) across all subjects. Consensus orderings were determined by sorting each matrix to minimize the total count of consensus-violating seroconversions. The color scale represents the number of times that 1 seroconversion is observed preceding another seroconversion. Analysis was performed at the level of (A) individual variants, (B) CIDR domain class, (C) upstream sequence group, and (D) binding phenotype. Note that heatmap diagonal is 0 in A by definition, because seroconversion to a specific antigen cannot precede itself. In B–D, diagonal counts indicate seroconversions to 1 class, group, or phenotype that are followed by another distinct member of the same class, group, or phenotype.
CIDRγ-specific IgG associates with protection from uncomplicated, febrile malaria.
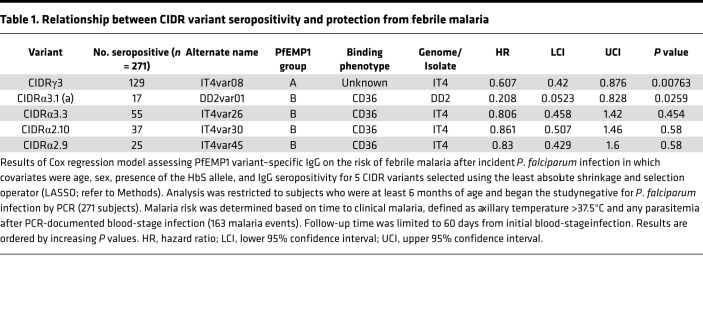
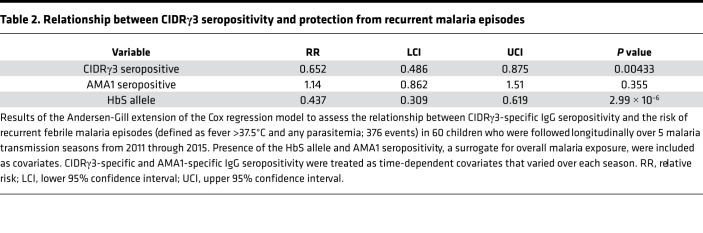
We focused on the risk of uncomplicated malaria given that severe malaria was rarely observed in the Kalifabougou cohort due to early diagnosis and treatment. We specifically evaluated whether baseline seropositivity for each variant could predict protection from febrile malaria after subsequent PCR-confirmed P. falciparum parasitemia in individuals who began the study PCR negative using a Cox regression model that included age, presence of the malaria-protective HbS allele, sex, IgG reactivity to AMA1 (as a surrogate for prior malaria exposure), and seropositivity to each of the 35 PfEMP1 variants as covariates. Notably, seropositivity to CIDRγ3 (IT4var08), which has an unknown binding phenotype, was significantly associated with reduced risk of febrile malaria (Table 1). CIDRγ domains have been associated with rosetting of erythrocytes (11), a phenomenon associated with severe forms of malaria (35), except in individuals with blood group O erythrocytes, which appear to exhibit reduced rosetting (36). We therefore hypothesized that the reduced risk afforded by CIDRγ-specific IgG might occur via the inhibition of rosette formation and may therefore be negatively affected by blood group O. When included as a covariate in a reduced Cox regression model, group O blood type affected neither malaria risk itself nor the association between CIDRγ-specific IgG and risk of febrile malaria (Supplemental Table 4). Notably, baseline CIDRγ3-specific IgG reactivity did not significantly correlate with decreased parasite density at the first malaria episode after controlling for age and the presence of the HbS allele (data not shown), suggesting that CIDRγ-specific IgG may not have antiparasitic activity. Given the association between CIDRγ-specific IgG and delay in malaria fever during the first year of the study, we specifically examined whether CIDRγ3 serostatus at the beginning of each malaria season affected the risk of recurrent malaria episodes in the 60 children who were longitudinal evaluated for PfEMP1 IgG responses over 5 malaria seasons. The presence of CIDRγ3-specific IgG before each season predicted a reduction in febrile malaria episodes, even after controlling for AMA1-specific IgG serostatus and the HbS allele (Table 2).
Table 1. Relationship between CIDR variant seropositivity and protection from febrile malaria.
Table 2. Relationship between CIDRγ3 seropositivity and protection from recurrent malaria episodes.
Discussion
PfEMP1 variants containing domains of the CIDRα1 class generally bind to EPCR on endothelial cells and are associated with severe malaria (10), whereas variants containing domains of the CIDRα2-6 classes bind to CD36 present on several host cell types, including microvascular endothelial cells, mononuclear phagocytes, and platelets (16, 37). Antibodies targeting these PfEMP1 domains can potentially disrupt adhesion of IEs to host receptors but can also facilitate IE clearance via opsonization and phagocytosis or antibody-mediated cytotoxicity (10, 38, 39). Consistent with a prior study conducted in a Tanzanian cohort (28), we observed early acquisition of IgG antibodies against EPCR-binding PfEMP1 variants of the CIDRα1 domain class relative to CD36-binding variants in both age-stratified cross-sectional and longitudinal analyses. This is also consistent with studies that investigated acquisition of antibodies against PfEMP1 classified by upstream sequence group and found that antibodies against DBL and CIDR domains belonging to group A and B/A are acquired earlier in life than group B and C variants among individuals living in malaria-endemic settings (26, 40). Importantly, the antigen panel used in the current study contained CIDR domains not covered by these prior studies.
Among the 35 distinct CIDR domains evaluated here, CIDRα1.7(c) elicited the most robust and prevalent IgG responses in early childhood, eventually approaching 100% seroprevalence in adolescents and adults in this cohort. Longitudinal analysis to assess hierarchical acquisition confirmed that IgG antibodies specific for CIDRα1.7(c) were acquired first, with IgG against the related CIDRα1.7(a) variant acquired fourth. Transcripts encoding CIDRα1.7 domains have been found to predominate among the most severe cases of pediatric cerebral malaria — those that lead to brain swelling and death (19). The immunodominance of CIDRα1.7(c) may be a consequence of epitopes targeted by cross-reactive CIDRα1 antibodies (41, 42). Moreover, PfEMP1 with CIDRα1.4 and CIDRα1.7 domains frequently contain ICAM1-binding DBLβ domains (43). The dual EPCR- and ICAM1-binding phenotype is thought to be particularly pathogenic, and antibodies against these DBLβ domains have been associated with reduced risk of clinical malaria, with parasite densities of ≥10,000 parasites/μl (44). We also observed early acquisition of IgG specific for CIDRα1.8 domains. Expression of these domains, as well as EPCR-binding CIDRα1 domains in general, is associated with severe malaria, including cerebral malaria in African children (18–21, 45) and Indian adults (46).
Given that all CIDRα1 variants have been linked to severe malaria in African children, the early acquisition of IgG specific to CIDRα1.7 and CIDRα1.8 domains may just be a reflection of local parasite population dynamics rather than enhanced pathogenicity conferred by these specific CIDR variants. However, the potential lethality of parasites expressing CIDRα1 in general underscores why a vigorous host antibody response against these variant domains in early childhood may be advantageous. This study builds on older work (4, 47, 48) showing an age-specific acquisition of antibodies against particular parasite strains, and we are able to statistically confirm this pattern for the first time to our knowledge and identify key genetic underpinnings of those observations. We still cannot address the slippery problem of whether this order reflects the circulation of genotypes with different transmissibility; under this scenario, high fitness genotypes lead to high prevalence and therefore low age of first infection and coincidentally cause more disease in relatively nonimmune children compared with low fitness genotypes as a result. In contrast, it is possible that the ordered expression of PfEMP1 variants across strains, potentially in response to the immune status of the parasite’s immediate host, leads to the hierarchical acquisition of antibodies observed.
Due to the low incidence of severe disease in the cohort, we could not assess the effect of CIDRα1.7-specific or CIDRα1.8-specific antibodies on the risk of severe malaria in the study. However, when all 35 CIDRs were assessed for association with the prospective risk of uncomplicated, febrile malaria, IgG specific to CIDRγ3 (IT4var08) was significantly associated with reduced malaria risk. PfEMP1 variants encoding CIDRβ, CIDRγ, or CIDRδ domains have been associated with rosetting (11, 46), which can enhance microvasculature obstruction, thereby increasing malaria severity. However, direct evidence that any of these CIDR domains have intrinsic rosetting properties is lacking (49). Rather, their association with rosetting may be related to their tandem expression with an adjacent DBLα1 at the N-terminal head (50). Rosetting frequency has been correlated with severity of malaria, with the highest levels in cerebral malaria (35, 51, 52), but is still commonly observed in uncomplicated malaria. Thus, the role of rosetting in severity of malarial disease remains unclear. Nevertheless, disruption of rosettes by targeting DBL1α has been used as a vaccine strategy (53), and antibodies against rosetting-associated group 2 DBLα domains predicted protection from uncomplicated malaria, suggesting a protective role for these antibodies in less severe disease (30, 31). Although speculative, it is possible that naturally acquired CIDRγ-specific IgG confers protection from febrile malaria by blocking rosette formation. However, this mechanism is not supported by the current study, given that the protection attributable to CIDRγ-specific IgG is unchanged after controlling for blood group O, which has been shown to be protective against severe falciparum malaria through the reduction of rosetting (36). It also must be noted that reduced malaria risk was not observed for IgG-specific variants of the CIDRδ class, which is also predicted to have rosetting activity. Furthermore, as CIDRγ3 was the only CIDRγ domain variant tested in this study, it remains unknown whether the protective effect observed here would be generalizable to IgG targeting other CIDRγ variants.
A limitation of the study is that we did not sequence var transcripts from individuals with P. falciparum infections in the longitudinal analysis. This may have allowed us to prospectively assess whether seroconversion against specific CIDRs, such as CIDRα1.7, CIDRα1.8, or CIDRγ, reliably led to the absence of parasites expressing the corresponding var transcript during clinical malaria episodes. In addition to our limited assessment of CIDRγ domains, we also did not evaluate CIDRβ domains, which also have been associated with the rosetting phenotype.
In summary, this longitudinal study provides evidence that acquisition of IgG antibodies against PfEMP1 variants is ordered and demonstrates that antibodies against CIDRα1 domains, specifically the pathogenic domain variants CIDRα1.7 and CIDRα1.8, are acquired the earliest in children residing in an area of intense, seasonal malaria transmission. We also show that IgG antibodies against the rosetting-associated CIDRγ3 domain are acquired early and are associated with protection from febrile malaria. Future studies will need to validate these findings in other transmission settings and determine the functional activity of these naturally acquired CIDR variant–specific antibodies.
Methods
Study site
The study was conducted in the village of Kalifabougou, Mali, which is located 40 km northwest of Bamako, Mali, within the savanna ecoclimatic zone. Within this community, Bambara is the predominant ethnic group, and approximately 90% of residents engage in subsistence farming. Malaria transmission is intense and seasonal, reliably occurring from June through December, with the vast majority of malaria cases caused by P. falciparum (54).
Study population and study design
Recruitment and enrollment procedures of participants for this study have been previously described (55). Briefly, exclusion criteria at enrollment included a hemoglobin level <7 g/dL, axillary temperature ≥37.5°C, acute systemic illness, underlying chronic disease, use of antimalarial or immunosuppressive medications in the past 30 days, or pregnancy. The study design and selection of subjects are summarized in Figure 1.
Human samples
At the beginning and end of each malaria-transmission season, blood samples were drawn by venipuncture into sodium citrate–containing Vacutainer tubes (BD). Plasma was separated by centrifugation and cryopreserved. Hemoglobin typing was performed using a D-10 instrument (Bio-Rad). Blood for ABO typing was collected in EDTA-containing microtainers (BD). ABO typing was conducted with forward typing using Cypress Diagnostics Reagents. Anti-A, anti-B, and anti-AB IgM reagents were mixed with the sample, and blood type was determined by agglutination. During the first malaria season, blood was collected by finger prick onto 903 filter paper (Whatman) for PCR analysis at each scheduled clinic visit (occurring at 2-week intervals for 7 months) and sick visit for subsequent molecular diagnostics.
Diagnosis and treatment of infections
Clinical malaria episodes.
Individuals were initially enrolled in May 2011 and have been followed continuously since unless withdrawn or lost to follow-up. During the first malaria season, clinical malaria episodes were detected prospectively by self-referral and weekly active clinical surveillance visits, which alternated between the study clinic and the participants’ homes. Passive malaria surveillance and premalaria and postmalaria season cross-sectional surveys have continued during subsequent years. All individuals with signs and symptoms of malaria and any level of Plasmodium parasitemia detected by light microscopy were treated according to the National Malaria Control Program guidelines in Mali. For the current study, a clinical malaria episode was defined as any parasitemia on contemporaneous blood smear, an axillary temperature of ≥37.5°C within 24 hours, and no other cause of fever discernible by physical exam.
Blood smears.
Thick blood smears were stained with Giemsa and counted against 300 leukocytes. Parasite densities were recorded as the number of asexual parasites/μl of blood based on a mean leukocyte count of 7500 cells/μl. Each smear was read in blinded manner by 2 certified microscopists of the laboratory team.
Molecular detection.
For each participant, the first P. falciparum infection of the initial malaria season was detected retrospectively by PCR analysis of the longitudinally collected dried blood spots (54). First malaria episodes were determined from the clinical visit data.
Protein expression and multiplex immunoassays
The 35 recombinant His-tagged CIDR domains (Supplemental Table 1) were expressed in baculovirus-transfected insect cells and purified by nickel affinity chromatography as previously described (28, 42, 56). AMA1, CSP, and MSP1 recombinant proteins were provided by David Narum (Laboratory of Malaria Immunology and Vaccinology, NIAID, NIH). AMA1 and CSP were expressed from P. falciparum 3D7 in P. pastoris as previously described (57, 58). MSP1 was expressed from P. falciparum 3D7 in E. coli as previously described (59). Purified tetanus toxoid was provided the staff at Biologic Laboratories, University of Massachusetts Medical School, Worcester, Massachusetts, USA. BSA was obtained from MilliporeSigma. These proteins were coupled to MagPlex-C microspheres (Luminex) and mixed to form a protein bead array in which IgG reactivity to each antigen could be measured in multiplex, as previously described (60), with minor modifications. Briefly, plasma samples were diluted 1:500 and 1:2000 (to better assess highly reactive antigens) in Assay Buffer E (ABE: 0.1% BSA, 0.05% Tween-20 in PBS, pH 7.4). For each plate, pooled malaria-hyperimmune plasma was serially diluted in ABE at 1:50, 1:158, 1:500, 1:1580, 1:5000, 1:1580, 1:50,000, and 1:158,000 to generate an 8-point dilutional standard curve. 50 μl beads and 50 μl diluted plasma were added to 96-well microtiter plates (MSBVS 1210, MilliporeSigma) prewetted with ABE. 50 μl phycoerythrin-conjugated Goat Anti-Human IgG (AB_2337681; Jackson ImmunoResearch Laboratories), diluted 1:3000, was added, and mean fluorescent intensities were measured using the Luminex 200 system. To account for plate-to-plate variation, fluorescence intensities were normalized using the median reactivity for each antigen on each plate. Normalized intensities were then scaled to the mean reactivity for each antigen to allow comparison between antigens. Using the nCal function within the nCal package (61), IgG concentrations were interpolated from the standard curves generated from serial diluted–pooled malaria-immune plasma and reported as arbitrary units (AU), which were then used for statistical analysis and visualization.
Ordered acquisition analysis
This analysis first found a best-fit consensus of ordered seroconversion from the patterns of individuals’ seroconversions. It then randomized the order of seroconversions for each individual, recomputed the consensus ordering, and determined whether the consensus order in the real data was significant by using a consensus goodness-of-fit metric.
If seroconversion to CIDR domains occurs in a stereotypical order, then each individual’s sequence of seroconversions in this longitudinal study should be congruent with that order. Of course, we do not know such an order a priori, so we found it by searching over all orderings to find the one that minimizes the number of order-violating seroconversions. This MVR consists of both the ordinal ranking itself and a corresponding number of rank violations, v. These outputs can be visualized by plotting a heatmap, with indices ordered by the minimizing ranking, as in Figure 5A. Clear triangular structure indicates the strength of the ordering, and v is equal to the sum of the sparser triangle.
Note that the more that individuals’ seroconversions occur strictly in their rank order, the smaller v will be. In this way, the number of violations, v, provides a convenient test statistic for a standard 1-tailed P value test: our null hypothesis is that there is no meaningful order to seroconversions, and thus, randomly permuting the order of seroconversions for each individual and recomputing v should make no difference. In other words, the null hypothesis is that the number of violations, v, in the real data is statistically indistinguishable from the number of violations in the time-randomized data vrandom. The P value can be computed then as the probability that v < vrandom. When actual seroconversions are significantly more orderable than random seroconversions (while preserving the seroconversion counts per individual and seroconversions per CIDR domain), it indicates the presence of a statistically significant stereotypical ordering, as in Supplemental Figure 2A.
Computations were performed according to the following details. Let matrix entry Aij be the number of times, over each individual, that a seroconversion to i was observed before a seroconversion to j. If the matrix’s rows and columns are sorted according to some reordering, r, then the number of violations, v, can be computed as the sum of the lower triangle of A(r). Finding the r that minimizes v can be done by beginning from a random r and then sequentially proposing swaps of pairs of indices, in which any swap that increases v is rejected and otherwise swaps are accepted. This MVR algorithm exits after a large number of proposed swaps have been rejected without any decrease in v, and the output is both v and the order of seroconversion that corresponds to that v. Permutation tests were then performed by shuffling the seroconversions and years, independently for each individual, and then applying the computation above.
Statistics
The use of specific statistical tests and methods is indicated in the Results and/or legends. Statistical significance was defined as a 2-tailed P value of less than 0.05. Analyses were performed in R version 3.6.1 (http://www.R-project.org). Plots were generated with the ggplot2 package. Cox regression was performed using the survival and glmnet packages. For the time to febrile malaria analysis (Table 1), variable selection from among the 35 CIDR seropositivity variables, age, sex, AMA1 seroreactivity, and the presence of the HbS allele, was determined using regularized Cox regression fit with the least absolute shrinkage and selection operator (LASSO) penalty using 10-fold cross validation with 1000 iterations (62). Here, penalized regression with LASSO was used to reduce the number of predictors and avoid overfitting. The follow-up period after initial blood-stage infection was 60 days. For the final Cox regression model, age, sex, and the presence of the HbS allele were included as covariates along with the LASSO-selected CIDR variables. For the recurrent event analysis, the Andersen-Gill extension of the Cox regression model was used to determine the relative risk of malaria over 5 malaria seasons using presence of the HbS allele as a covariate and AMA1-specific IgG seropositivity (a surrogate for overall malaria exposure) and CIDRγ3-specific IgG seropositivity as time-dependent covariates that varied over each season.
Study approval
The ethics committee of the Faculty of Medicine, Pharmacy and Dentistry at the University of Sciences, Techniques and Technology of Bamako, and the Institutional Review Board of NIAID NIH approved this study (ClinicalTrials.gov NCT01322581). Written, informed consent was obtained from the parents or guardians of participating children or from adult participants.
Author contributions
NOA, LHM, SKP, LT, TL, PDC, and TMT conceived the study. AO, SD, KK, and BT were responsible for the cohort study and collection of samples. NOA, LT, SL, and TBY conducted the experiments. NOA, DBL, and TMT analyzed the data. TMT, TL, COB, DBL, and PDC wrote the manuscript with contributions from NOA, LT, LHM, and SKP. All authors read and approved the manuscript.
Supplementary Material
Acknowledgments
We thank all the participants in the Kalifabougou cohort and the field team for making this study possible. We also thank Chiung-Yu Huang (University of California, San Francisco) for her critical review and suggestions regarding the survival and recurrent event analysis. The authors thank Alan Hoofring for his assistance with the graphical abstract. This project was supported with federal funds from the Division of Intramural Research, NIAID, NIH, and the Department of Health and Human Services. TMT was supported by grant K08AI125682 (NIAID) and the Doris Duke Charitable Foundation Clinical Scientist Development Award.
Version 1. 05/19/2020
In-Press Preview
Version 2. 06/18/2020
Electronic publication
Footnotes
NOA’s present address is: GlaxoSmithKline, Collegeville, Pennsylvania, USA.
Conflict of interest: The authors have declared that no conflict of interest exists.
Copyright: © 2020, American Society for Clinical Investigation.
Reference information: JCI Insight. 2020;5(12):e137262.https://doi.org/10.1172/jci.insight.137262.
Contributor Information
Nyamekye Obeng-Adjei, Email: obengadjein@gmail.com.
Daniel B. Larremore, Email: daniel.larremore@colorado.edu.
Louise Turner, Email: lturner@sund.ku.dk.
Aissata Ongoiba, Email: ongoiba@icermali.org.
Shanping Li, Email: lishanping@niaid.nih.gov.
Safiatou Doumbo, Email: sdoumbo@icermali.org.
Takele B. Yazew, Email: tyazew@umd.edu.
Kassoum Kayentao, Email: kayentao@icermali.org.
Boubacar Traore, Email: Bouba.traore@icermali.org.
Susan K. Pierce, Email: spierce@nih.gov.
Caroline O. Buckee, Email: cbuckee@hsph.harvard.edu.
Thomas Lavstsen, Email: thomasl@sund.ku.dk.
Peter D. Crompton, Email: pcrompton@niaid.nih.gov.
Tuan M. Tran, Email: tuan.tran@alumni.emory.edu.
References
- 1. [No authors listed]. World Malaria Report 2019. World Health Organization. https://www.who.int/publications-detail/world-malaria-report-2019 Published December 4, 2019. Accessed May 19, 2020.
- 2.Jensen AR, Adams Y, Hviid L. Cerebral Plasmodium falciparum malaria: The role of PfEMP1 in its pathogenesis and immunity, and PfEMP1-based vaccines to prevent it. Immunol Rev. 2020;293(1):230–252. doi: 10.1111/imr.12807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baruch DI, et al. Cloning the P. falciparum gene encoding PfEMP1, a malarial variant antigen and adherence receptor on the surface of parasitized human erythrocytes. Cell. 1995;82(1):77–87. doi: 10.1016/0092-8674(95)90054-3. [DOI] [PubMed] [Google Scholar]
- 4.Bull PC, Lowe BS, Kortok M, Molyneux CS, Newbold CI, Marsh K. Parasite antigens on the infected red cell surface are targets for naturally acquired immunity to malaria. Nat Med. 1998;4(3):358–360. doi: 10.1038/nm0398-358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chan JA, et al. Targets of antibodies against Plasmodium falciparum-infected erythrocytes in malaria immunity. J Clin Invest. 2012;122(9):3227–3238. doi: 10.1172/JCI62182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Su XZ, et al. The large diverse gene family var encodes proteins involved in cytoadherence and antigenic variation of Plasmodium falciparum-infected erythrocytes. Cell. 1995;82(1):89–100. doi: 10.1016/0092-8674(95)90055-1. [DOI] [PubMed] [Google Scholar]
- 7.Gardner MJ, et al. Genome sequence of the human malaria parasite Plasmodium falciparum. Nature. 2002;419(6906):498–511. doi: 10.1038/nature01097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen Q, et al. Developmental selection of var gene expression in Plasmodium falciparum. Nature. 1998;394(6691):392–395. doi: 10.1038/28660. [DOI] [PubMed] [Google Scholar]
- 9.Smith JD, et al. Switches in expression of Plasmodium falciparum var genes correlate with changes in antigenic and cytoadherent phenotypes of infected erythrocytes. Cell. 1995;82(1):101–110. doi: 10.1016/0092-8674(95)90056-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Turner L, et al. Severe malaria is associated with parasite binding to endothelial protein C receptor. Nature. 2013;498(7455):502–505. doi: 10.1038/nature12216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smith JD, Rowe JA, Higgins MK, Lavstsen T. Malaria’s deadly grip: cytoadhesion of Plasmodium falciparum-infected erythrocytes. Cell Microbiol. 2013;15(12):1976–1983. doi: 10.1111/cmi.12183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rask TS, Hansen DA, Theander TG, Gorm Pedersen A, Lavstsen T. Plasmodium falciparum erythrocyte membrane protein 1 diversity in seven genomes--divide and conquer. PLoS Comput Biol. 2010;6(9):e1000933. doi: 10.1371/journal.pcbi.1000933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Otto TD, et al. Evolutionary analysis of the most polymorphic gene family in falciparum malaria. Wellcome Open Res. 2019;4:193. doi: 10.12688/wellcomeopenres.15590.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fried M, Duffy PE. Adherence of Plasmodium falciparum to chondroitin sulfate A in the human placenta. Science. 1996;272(5267):1502–1504. doi: 10.1126/science.272.5267.1502. [DOI] [PubMed] [Google Scholar]
- 15.Buffet PA, et al. Plasmodium falciparum domain mediating adhesion to chondroitin sulfate A: a receptor for human placental infection. Proc Natl Acad Sci USA. 1999;96(22):12743–12748. doi: 10.1073/pnas.96.22.12743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Robinson BA, Welch TL, Smith JD. Widespread functional specialization of Plasmodium falciparum erythrocyte membrane protein 1 family members to bind CD36 analysed across a parasite genome. Mol Microbiol. 2003;47(5):1265–1278. doi: 10.1046/j.1365-2958.2003.03378.x. [DOI] [PubMed] [Google Scholar]
- 17.Lavstsen T, Salanti A, Jensen AT, Arnot DE, Theander TG. Sub-grouping of Plasmodium falciparum 3D7 var genes based on sequence analysis of coding and non-coding regions. Malar J. 2003;2:27. doi: 10.1186/1475-2875-2-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jespersen JS, et al. Plasmodium falciparum var genes expressed in children with severe malaria encode CIDRα1 domains. EMBO Mol Med. 2016;8(8):839–850. doi: 10.15252/emmm.201606188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kessler A, et al. Linking EPCR-binding PfEMP1 to brain swelling in pediatric cerebral malaria. Cell Host Microbe. 2017;22(5):601–614.e5. doi: 10.1016/j.chom.2017.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mkumbaye SI, et al. The severity of Plasmodium falciparum infection is associated with transcript levels of var genes encoding endothelial protein c receptor-binding P. falciparum erythrocyte membrane protein 1. Infect Immun. 2017;85(4):e00841-16. doi: 10.1128/IAI.00841-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shabani E, Hanisch B, Opoka RO, Lavstsen T, John CC. Plasmodium falciparum EPCR-binding PfEMP1 expression increases with malaria disease severity and is elevated in retinopathy negative cerebral malaria. BMC Med. 2017;15(1):183. doi: 10.1186/s12916-017-0945-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cabrera A, Neculai D, Kain KC. CD36 and malaria: friends or foes? A decade of data provides some answers. Trends Parasitol. 2014;30(9):436–444. doi: 10.1016/j.pt.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 23.Ochola LB, et al. Specific receptor usage in Plasmodium falciparum cytoadherence is associated with disease outcome. PLoS One. 2011;6(3):e14741. doi: 10.1371/journal.pone.0014741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gupta S, Snow RW, Donnelly CA, Marsh K, Newbold C. Immunity to non-cerebral severe malaria is acquired after one or two infections. Nat Med. 1999;5(3):340–343. doi: 10.1038/6560. [DOI] [PubMed] [Google Scholar]
- 25.Wahlgren M, Goel S, Akhouri RR. Variant surface antigens of Plasmodium falciparum and their roles in severe malaria. Nat Rev Microbiol. 2017;15(8):479–491. doi: 10.1038/nrmicro.2017.47. [DOI] [PubMed] [Google Scholar]
- 26.Cham GK, et al. Hierarchical, domain type-specific acquisition of antibodies to Plasmodium falciparum erythrocyte membrane protein 1 in Tanzanian children. Infect Immun. 2010;78(11):4653–4659. doi: 10.1128/IAI.00593-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Duffy MF, et al. Differences in PfEMP1s recognized by antibodies from patients with uncomplicated or severe malaria. Malar J. 2016;15(1):258. doi: 10.1186/s12936-016-1296-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Turner L, et al. IgG antibodies to endothelial protein C receptor-binding cysteine-rich interdomain region domains of Plasmodium falciparum erythrocyte membrane protein 1 are acquired early in life in individuals exposed to malaria. Infect Immun. 2015;83(8):3096–3103. doi: 10.1128/IAI.00271-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rambhatla JS, et al. Acquisition of antibodies against endothelial protein c receptor-binding domains of Plasmodium falciparum erythrocyte membrane protein 1 in children with severe malaria. J Infect Dis. 2019;219(5):808–818. doi: 10.1093/infdis/jiy564. [DOI] [PubMed] [Google Scholar]
- 30.Tessema SK, et al. Protective immunity against severe malaria in children is associated with a limited repertoire of antibodies to conserved PfEMP1 variants. Cell Host Microbe. 2019;26(5):579–590.e5. doi: 10.1016/j.chom.2019.10.012. [DOI] [PubMed] [Google Scholar]
- 31.Bull PC, et al. Plasmodium falciparum variant surface antigen expression patterns during malaria. PLoS Pathog. 2005;1(3):e26. doi: 10.1371/journal.ppat.0010026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tran TM, et al. Naturally acquired antibodies specific for Plasmodium falciparum reticulocyte-binding protein homologue 5 inhibit parasite growth and predict protection from malaria. J Infect Dis. 2014;209(5):789–798. doi: 10.1093/infdis/jit553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bustamante LY, et al. Synergistic malaria vaccine combinations identified by systematic antigen screening. Proc Natl Acad Sci USA. 2017;114(45):12045–12050. doi: 10.1073/pnas.1702944114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Weiss GE, et al. The Plasmodium falciparum-specific human memory B cell compartment expands gradually with repeated malaria infections. PLoS Pathog. 2010;6(5):e1000912. doi: 10.1371/journal.ppat.1000912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Doumbo OK, et al. High levels of Plasmodium falciparum rosetting in all clinical forms of severe malaria in African children. Am J Trop Med Hyg. 2009;81(6):987–993. doi: 10.4269/ajtmh.2009.09-0406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rowe JA, et al. Blood group O protects against severe Plasmodium falciparum malaria through the mechanism of reduced rosetting. Proc Natl Acad Sci USA. 2007;104(44):17471–17476. doi: 10.1073/pnas.0705390104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Silverstein RL, Febbraio M. CD36, a scavenger receptor involved in immunity, metabolism, angiogenesis, and behavior. Sci Signal. 2009;2(72):re3. doi: 10.1126/scisignal.272re3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chan JA, et al. Patterns of protective associations differ for antibodies to P. falciparum-infected erythrocytes and merozoites in immunity against malaria in children. Eur J Immunol. 2017;47(12):2124–2136. doi: 10.1002/eji.201747032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Arora G, et al. NK cells inhibit Plasmodium falciparum growth in red blood cells via antibody-dependent cellular cytotoxicity. Elife. 2018;7:e36806. doi: 10.7554/eLife.36806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cham GK, et al. Sequential, ordered acquisition of antibodies to Plasmodium falciparum erythrocyte membrane protein 1 domains. J Immunol. 2009;183(5):3356–3363. doi: 10.4049/jimmunol.0901331. [DOI] [PubMed] [Google Scholar]
- 41.Turner L, Theander TG, Lavstsen T. Immunization with recombinant Plasmodium falciparum erythrocyte membrane protein 1 CIDRα1 domains induces domain subtype inhibitory antibodies. Infect Immun. 2018;86(11):e00435-18. doi: 10.1128/IAI.00435-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lau CK, et al. Structural conservation despite huge sequence diversity allows EPCR binding by the PfEMP1 family implicated in severe childhood malaria. Cell Host Microbe. 2015;17(1):118–129. doi: 10.1016/j.chom.2014.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lennartz F, et al. Structure-guided identification of a family of dual receptor-binding PfEMP1 that is associated with cerebral malaria. Cell Host Microbe. 2017;21(3):403–414. doi: 10.1016/j.chom.2017.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tessema SK, et al. Antibodies to intercellular adhesion molecule 1-binding Plasmodium falciparum erythrocyte membrane protein 1-DBLβ are biomarkers of protective immunity to malaria in a cohort of young children from Papua New Guinea. Infect Immun. 2018;86(8):e00485-17. doi: 10.1128/IAI.00485-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Storm J, et al. Cerebral malaria is associated with differential cytoadherence to brain endothelial cells. EMBO Mol Med. 2019;11(2):e9164. doi: 10.15252/emmm.201809164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bernabeu M, et al. Severe adult malaria is associated with specific PfEMP1 adhesion types and high parasite biomass. Proc Natl Acad Sci USA. 2016;113(23):E3270–E3279. doi: 10.1073/pnas.1524294113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gupta S, Day KP. A theoretical framework for the immunoepidemiology of Plasmodium falciparum malaria. Parasite Immunol. 1994;16(7):361–370. doi: 10.1111/j.1365-3024.1994.tb00361.x. [DOI] [PubMed] [Google Scholar]
- 48.Bull PC, Lowe BS, Kortok M, Marsh K. Antibody recognition of Plasmodium falciparum erythrocyte surface antigens in Kenya: evidence for rare and prevalent variants. Infect Immun. 1999;67(2):733–739. doi: 10.1128/IAI.67.2.733-739.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rowe JA, Moulds JM, Newbold CI, Miller LH. P. falciparum rosetting mediated by a parasite-variant erythrocyte membrane protein and complement-receptor 1. Nature. 1997;388(6639):292–295. doi: 10.1038/40888. [DOI] [PubMed] [Google Scholar]
- 50.Ghumra A, et al. Induction of strain-transcending antibodies against Group A PfEMP1 surface antigens from virulent malaria parasites. PLoS Pathog. 2012;8(4):e1002665. doi: 10.1371/journal.ppat.1002665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Carlson J, Helmby H, Hill AV, Brewster D, Greenwood BM, Wahlgren M. Human cerebral malaria: association with erythrocyte rosetting and lack of anti-rosetting antibodies. Lancet. 1990;336(8729):1457–1460. doi: 10.1016/0140-6736(90)93174-N. [DOI] [PubMed] [Google Scholar]
- 52.Ho M, Davis TM, Silamut K, Bunnag D, White NJ. Rosette formation of Plasmodium falciparum-infected erythrocytes from patients with acute malaria. Infect Immun. 1991;59(6):2135–2139. doi: 10.1128/IAI.59.6.2135-2139.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chen Q, et al. Immunization with PfEMP1-DBL1alpha generates antibodies that disrupt rosettes and protect against the sequestration of Plasmodium falciparum-infected erythrocytes. Vaccine. 2004;22(21-22):2701–2712. doi: 10.1016/j.vaccine.2004.02.015. [DOI] [PubMed] [Google Scholar]
- 54.Tran TM, et al. An intensive longitudinal cohort study of Malian children and adults reveals no evidence of acquired immunity to Plasmodium falciparum infection. Clin Infect Dis. 2013;57(1):40–47. doi: 10.1093/cid/cit174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Doumbo S, et al. Co-infection of long-term carriers of Plasmodium falciparum with Schistosoma haematobium enhances protection from febrile malaria: a prospective cohort study in Mali. PLoS Negl Trop Dis. 2014;8(9):e3154. doi: 10.1371/journal.pntd.0003154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hsieh FL, Turner L, Bolla JR, Robinson CV, Lavstsen T, Higgins MK. The structural basis for CD36 binding by the malaria parasite. Nat Commun. 2016;7:12837. doi: 10.1038/ncomms12837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Plassmeyer ML, et al. Structure of the Plasmodium falciparum circumsporozoite protein, a leading malaria vaccine candidate. J Biol Chem. 2009;284(39):26951–26963. doi: 10.1074/jbc.M109.013706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ellis RD, et al. Phase 1 study in malaria naïve adults of BSAM2/Alhydrogel®+CPG 7909, a blood stage vaccine against P. falciparum malaria. PLoS One. 2012;7(10):e46094. doi: 10.1371/journal.pone.0046094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Shimp RL, et al. Production and characterization of clinical grade Escherichia coli derived Plasmodium falciparum 42 kDa merozoite surface protein 1 (MSP1(42)) in the absence of an affinity tag. Protein Expr Purif. 2006;50(1):58–67. doi: 10.1016/j.pep.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 60.Cham GK, Kurtis J, Lusingu J, Theander TG, Jensen AT, Turner L. A semi-automated multiplex high-throughput assay for measuring IgG antibodies against Plasmodium falciparum erythrocyte membrane protein 1 (PfEMP1) domains in small volumes of plasma. Malar J. 2008;7:108. doi: 10.1186/1475-2875-7-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fong Y, Sebestyen K, Yu X, Gilbert P, Self S. nCal: an R package for non-linear calibration. Bioinformatics. 2013;29(20):2653–2654. doi: 10.1093/bioinformatics/btt456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Simon N, Friedman J, Hastie T, Tibshirani R. A sparse-group Lasso. J Comput Graph Stat. 2013;22(2):231–245. doi: 10.1080/10618600.2012.681250. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.