Abstract
Objective: The COVID-19 pandemic necessitated drastic and rapid changes throughout the field of radiation oncology, some of which were unique to the discipline of radiosurgery. Guidelines called for reduced frame use and reducing the number of fractions. Our institution implemented these guidelines, and herein we show the resultant effect on patient treatments on our Gamma Knife Icon program.
Methods: In early March 2020 we rapidly implemented suggested changes according to ASTRO and other consensus guidelines as they relate to stereotactic radiosurgery in the COVID-19 era. We reviewed the GK Icon schedule at our institution between January 01 and April 30, 2020. We documented age, condition treated, technique (frame vs. mask), and number of fractions. We then tabulated and graphed the number of patients, framed cases, and fractions delivered.
Results: Seventy-seven patients were treated on the GK Icon over that period, for a total of 231 fractions. The number of unique patients varied from 18 (April) to 22 (January). Of the 77 patients only 5 were treated using a frame. The number of fractions per month decreased significantly over time, from 70 in January to 36 in April. Likewise, the percentage of single fraction cases increased from 4.5% per month in January to 67% in April.
Conclusions: The results presented here show that it is possible to quickly and efficiently change work flows to allow for reduced fractionation and frame use in the time of a global pandemic. Multidisciplinary cooperation and ongoing communication are integral to the success of such programs.
Keywords: Radiosurgery, Gamma Knife, COVID-19, pandemic
Introduction
A novel coronavirus (COVID-19) emerged from the city of Wuhan in the Huebei province of China in late 2019, spreading to Europe and eventually America, creating a global pandemic (1). The effects of the virus were widespread, with projected American deaths of up to 2 million if no mitigation techniques were implemented (2). In response, sweeping changes were enacted including social distancing, school closures, mandatory masking in some states, and telecommuting when possible (3). As an essential sector of health care, oncology, and more specifically radiation oncology, was effected as well. Guidelines were quickly put in place by ASCO and ASTRO in terms of patient workflow, delaying care when possible, and personal protective equipment (PPE) usage (4, 5). In addition, guidelines in reference to stereotactic radiosurgery (SRS) programs were also published and widely available in early April (6). The authors present here the results of rapid adoption of those guidelines, and the resultant effect on our Gamma Knife (GK) Icon SRS program.
Methods
Our institution installed and began treatment with the Gamma Knife Icon system (Elekta, Stockholm, Sweden) in May 2019. The GK Icon is unique in that this latest iteration includes on board imaging in the form of cone beam CT (CBCT), the ability to treat patients in a frameless manner using a thermoplastic mask, and intrafraction motion monitoring (IFMM) (7). As our GK Icon policies were developed in 2019 it was decided to utilize the Leksell Coordinate© Frame G for any functional cases and any treatments delivered in a single fraction based on expert opinion and training experience (8). When hypofractionation (3-5 fractions) was employed, for example with larger targets or at patient discretion, the mask was used. The full treatment planning process is outlined below.
As mentioned above, with the spread of COVID-19 several guidelines have been published, with one such set addressing SRS programs (6). The highlights of those guidelines include favoring mask-based treatment over frame-based given less face-to-face exposure with mask fabrication as opposed to frame placement. In addition, avoidance of frame placement helps limit the number of staff which would have close contact with the patient and promotes social/clinical distancing. Moreover, not needing sedation or local anesthesia helps reduce the use of personal protective equipment which is in high demand during the pandemic. The authors also advocate for decreased number of fractions, which in turn leads to a decrease in number of trips to the medical center for patients. Lastly, they recommended single fraction frameless treatment for patients with brain metastases, in lieu of whole brain radiation therapy, citing the aforementioned logic/reasons. In response to the pandemic and after review of those guidelines our division created a response team including physicians, physicists, nurses, radiation therapists, and administrators. The committee made the decision to limit frame based cases when possible, delay non-urgent functional cases, and to move to a single fraction frameless technique for brain metastases when feasible (i.e. cases less than 40-45 minutes). This change in policy was executed in late March 2020 and early April 2020. At the end of April 2020, the GK Icon treatment schedule was reviewed back to January 2020 and characteristics including diagnosis, technique (frame vs. mask), and number of fractions were tabulated and graphed over time. A univariate logistic regression was also used with single fraction treatment as the endpoint and month as the independent variable to generate odds ratios.
All patients were treated on the GK Icon and planned using Gammaplan treatment planning software (version 11.1.1). All patients had 1 mm slice thickness, contrast enhanced, volumetric, axial MRI scans for targeting and planning. For patients unable to undergo MRI (i.e. a patient with a pacemaker or defibrillator) a thin slice (1 mm) head CT with contrast was obtained in diagnostic radiology and used for targeting. MRI was obtained the day of frame placement, or within 2-4 days of frameless cases. For patients treated with a mask, a custom headrest is made on the GK Icon and a thermoplastic mask is formed to the patients head/face with pressure applied over the forehead and chin. The nose is left open to allow for placement of the reflective marker. After allowing the mask to cool and cure over 15 minutes a CBCT is done with a CT dose index of 6.3 mGy as reference for patient localization in the subsequent treatment. This CBCT creates the stereotactic space and is able to be co-registered to the thin slice MRI (or contrast enhanced thin slice CT) and allow for completion of planning. For intact tumors and meningioma cases the planning target volume (PTV) was defined as the gross tumor volume (GTV) as seen on contrast enhanced imaging with no margin. For post operative metastases cases the PTV was the resection cavity with a 1 mm margin. Planning was completed in a team based approach with a physicist, radiation oncologist, and neurosurgeon typically using a combination of forward and inverse planning. The ideal plan had 99-100% coverage to the specified PTV(s). Dosing was picked based on type of case, number of lesions, and size of target (9, 10).
At the time of treatment (both frame and mask) a 2.5 mGy CBCT was obtained to check frame placement, dose distribution, and any shifts. If dose was maintained and there were no aberrant shifts treatment was initiated. During mask-based treatment intrafraction motion monitoring (IFMM) was done throughout treatment, tracking the reflective marker on the nose and gating treatment if motion exceeded 1.5 mm for fractionated cases and 1.0 mm for single fraction frameless cases. If motion stayed outside that threshold for over 30 seconds the treatment was paused and the patient was given a break prior to resumption of treatment. As this study seeks to determine the effectiveness of an adaptive policy and all treatments were only recently completed, follow up was not included nor available for analysis. Similarly, given the quality improvement nature of this study, it was exempt from institutional review board (IRB) oversight.
Results
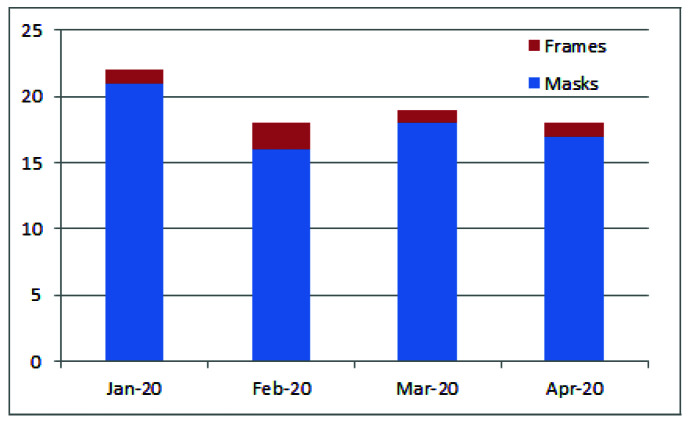
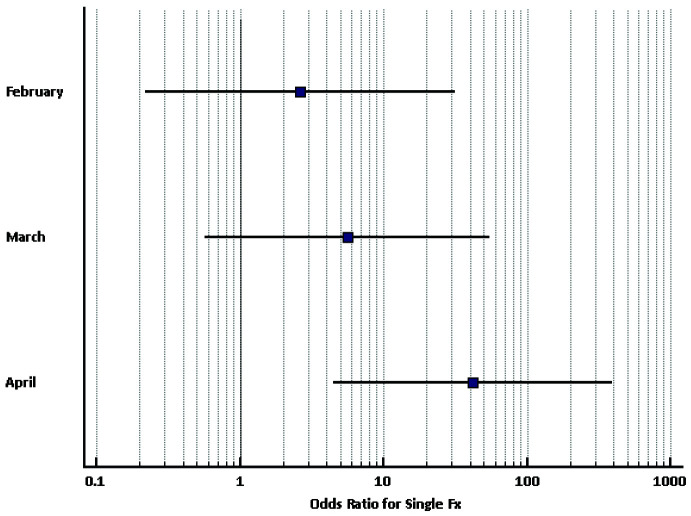
Seventy-seven patients were treated on the GK Icon between January 01, 2020 and April 30, 2020 for a total of 231 fractions. One patient, a nursing home resident with trigeminal neuralgia was scheduled for frame-based SRS in late March but was postponed due to the non-urgent nature of his condition. The median age was 63 (30-87) and the majority were female (66%). The vast majority of patients (79%) were treated for brain metastases. Table 1 outlines baseline characteristics, fractionation, and dosing. Only 5 patients (6.67%) were treated with a frame-based technique from January to April (meningioma patient in January, 2 metastases cases in February, trigeminal neuralgia case in March, and multiple metastases patient in April) (Figure 1). The number of patients was relatively steady across the study time period, hovering around 20 (18-22), but was at its lowest in April 2020. The number of fractions dropped significantly across the time frame, from 70 in January down to 36 in April (Figure 2). Conversely, the percentage of single fraction cases increased significantly, from 4.5% in January 2020 to 67% in April 2020 (Figure 3). The odds ratio for single fraction treatment in April 2020 was 42.56 (95% CI: 4.50-391.65, p=0.001). It was not significant for the other months (Figure 4).
Table 1.
Patient Characteristics (n=77)
| Patient Characteristic | n (% or range) |
| Gender | |
| Male | 26 (34) |
| Female | 51 (66) |
| Median Age | 63 (30-87) |
| Diagnosis | |
| Metastases | 61 (79) |
| Meningioma | 4 (5) |
| Trigeminal Neuralgia | 1 (1.5) |
| Schwannoma | 1 (1.5) |
| Glioma | 10 (13) |
| Technique | |
| Mask | 72 (94) |
| Frame | 5 (6) |
| Fractionation Scheme | |
| One | 19 (25) |
| Three | 39 (50) |
| Five | 19 (25) |
| Median Dose and Fractions per Diagnosis | |
| Metastases | 27 Gy/3 fx (16-30 Gy/1-5 fx) |
| Meningioma | 25 Gy/5 fx (14-25 Gy/1-5 fx) |
| Trigeminal Neuralgia | 80 Gy/1 fx (80 Gy/1 fx) |
| Schwannoma | 25 Gy/5 fx (25 Gy/5 fx) |
| Glioma | 25 Gy/5 fx (24-30 Gy/3-5 fx) |
Figure 1.
Breakdown of treatment course by month and whether a mask or frame was utilized.
Figure 2.
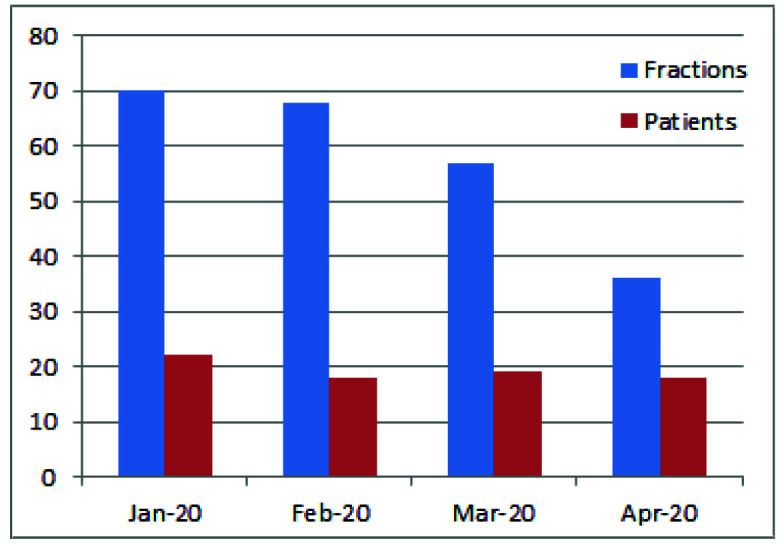
Number of patients and GK Icon fractions per month.
Figure 3.
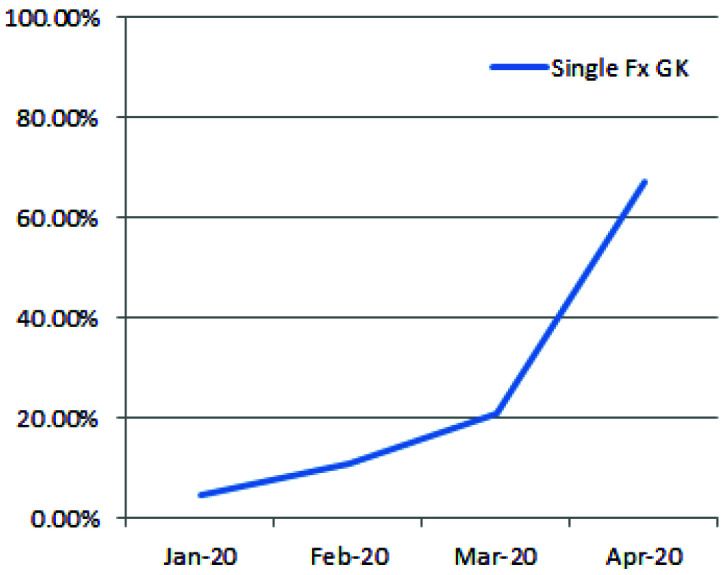
Percentage of single fraction GK Icon cases over time. Rates rose from under 5% in January 2020 to close to 70% by April 2020.
Figure 4.
Forest plot showing odds ratios and respective 95% confidence intervals for likelihood of single fraction treatment. OR for single fraction treatment in April 2020 was 42.56 (95% CI: 4.50-391.65, p=0.001). It was not significant for the other months.
Discussion
The findings presented here demonstrate the ability to quickly adapt an SRS program in the time of unprecedented change. By having leadership in place that was in tune with the constantly changing healthcare landscape in the setting of a pandemic, our institution was able to rapidly shift from a mainly frameless hypofractionated approach to that of a single fraction frameless GK Icon technique (67% by April 2020). It is noteworthy that the number of patients remained mostly stable, while a significant decrease in the number of delivered fractions was achieved. It must be noted that our approach is very “mask-heavy” to begin with, as only 5 framed cases occurred across the 4 month period, and as such, shifting to a frameless approach was relatively easy and did not require a learning curve. The ability to attain such a swift change in a safe and effective manner was due to open communication and a true multi-disciplinary approach which engaged nursing, physics, and physicians across multiple specialties. Our team plans to continue to utilize a single fraction frameless approach, when feasible, moving forward.
The framework for such change has been available for over a month now in the form of guidelines and suggestions from multiple specialty organizations. ASCO released their recommendations in March focusing on the duty to maximize health care outcomes, even in the setting of limited resources, with a strong emphasis on communication between practitioners and with their patients (4). In turn, ASTRO released myriad guidelines across all disease sites ranging from head and neck, lymphoma, breast, and prostate cancer (5). Their summary guidelines focus on treatment using the shortest possible course of radiotherapy (e.g., single-fraction treatment for bone pain, hypofractionation where appropriate, e.g., breast, prostate) (11). The American College of Surgeons also published a helpful set of recommendations which assigned various priority levels to breast cancer patients based on their disease stage and status, allowing for safe and effective delay of care when feasible (12).
Certainly, the concepts of hypofractionation and delay of non-urgent care are easily translated to radiosurgery. A group of neurosurgeons and radiation oncologists published a set of guidelines in mid-April 2020 (6). Those guidelines mention maintaining a multidisciplinary approach through teleconferencing to maintain social distancing. In addition, the guidelines are similar to those of ASTRO in supporting as few fractions as possible to limit patient trips to the medical center. Moreover, the authors mention a preference for mask-based treatment over frame to help reduce exposure to additional staff that is necessary for frame placements. Our data certainly fall in line with most or all of these recommendations. The limitations of the present study which must be mentioned include that those centers which rely heavily on frame-based SRS or lack the GK Icon may not as easily transition to a primarily mask-based approach. In addition, as our institution was comfortable with mask-based treatment based on past linac-based SRS experience, the transition was rather simple as evidenced by the minority of cases being frame-based. It remains to be seen which changes the pandemic has brought will be in place for years to come; however, our approach will be to maintain a mask-based approach, with as few fractions as possible, when feasible.
Conclusions
The implementation of guidelines for SRS in the setting of the COVID-19 pandemic can be achieved in a rapid fashion through open communication and an ongoing multidisciplinary approach that focuses on patient and staff member safety.
Acknowledgments
Funding: None.
Authors’ disclosure of potential conflicts of interest
The authors have nothing to disclose.
Author contributions
Conception and design: Rodney E. Wegner
Data collection: Rodney E. Wegner
Data analysis and interpretation: Athanasios Colonias, Zachary D. Horne, Rodney E. Wegner
Manuscript writing: Athanasios Colonias, Russell Fuhrer, Matthew Goss, Zachary D. Horne, Stephen M. Karlovits, Yun Liang, Jason Sohn, Rodney E. Wegner, Linda Xu, Alexander Yu
Final approval of manuscript: Stephen M. Karlovits
References
- 1. CDC. 2019 Novel coronavirus, Wuhan, China. Information for Healthcare Professionals. 2020. [Available from: https://www.cdc.gov/coronavirus/2019-nCoV/hcp/index.html. [Google Scholar]
- 2. Verity R, Okell LC, Dorigatti I, Winskill P, Whittaker C, Imai N, Cuomo-Dannenburg G, Thompson H, Walker PGT, Fu H, Dighe A, Griffin JT, Baguelin Bhatia S, Boonyasiri A, Cori A, Cucunubá Z, FitzJohn R, Gaythorpe K, Green W, Hamlet A, Hinsley W, Laydon D, Nedjati-Gilani G, Riley S, van Elsland S, Volz E, Wang H, Wang Y, Xi X, Donnelly CA, Ghani AC, Ferguson NM. Estimates of the severity of coronavirus disease 2019: A model-based analysis. Lancet Infect Dis. 2020. doi: 10.1016/S1473-3099(20)30243-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. CDC. Recommendation regarding the use of cloth face coverings, especially in areas of significant community-based transmission 2020. [Available from: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cloth-face-cover.html.
- 4. Marron JM, Joffe S, Jagsi R, Spence RA, Hlubocky FJ. Ethics and resource scarcity: ASCO recommendations for the oncology community during the COVID19 pandemic. J Clin Oncol. 2020; (published online April 9.).DOI: 10.1200/JCO.20.00960 [DOI] [PubMed] [Google Scholar]
- 5. ASTRO. COVID-19 Clinical Guidance 2020. [cited 2020 4/27/2020]. Available from: https://www.astro.org/Daily-Practice/COVID-19-Recommendations-and-Information/Clinical-Guidance. [Google Scholar]
- 6. Pannullo SCCS, Brandmaier A, Knisely J, Adler JR., Jr Clinical considerations in neurosurgical radiosurgery in the time of COVID-19. Cureus. 2020;12(4):e7671. doi: 10.7759/cureus.7671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Carminucci A, Nie K, Weiner J, Hargreaves E, Danish SF. Assessment of motion error for frame-based and noninvasive mask-based fixation using the Leksell Gamma Knife Icon radiosurgery system. J Neurosurg. 2018;129(Suppl1):133-9. [DOI] [PubMed] [Google Scholar]
- 8. Lunsford LD, Niranjan A, Fallon K, Kim JO. Frame versus frameless Leksell stereotactic radiosurgery. Prog Neurol Surg. 2019;34:19-27. [DOI] [PubMed] [Google Scholar]
- 9. Shaw E, Scott C, Souhami L, Dinapoli R, Kline R, Loeffler J, Farnan N. Single dose radiosurgical treatment of recurrent previously irradiated primary brain tumors and brain metastases: Final report of RTOG protocol 90-05. Int J Radiat Oncol Biol Phys. 2000;47(2):291-8. [DOI] [PubMed] [Google Scholar]
- 10. Colaco RJ, Yu JB, Bond JS, Bindra RS, Contessa JN, Knisely JPS, Chiang VL. A contemporary dose selection algorithm for stereotactic radiosurgery in the treatment of brain metastases An initial report. J Radiosurg SBRT. 2016;4:43-52. [PMC free article] [PubMed] [Google Scholar]
- 11. ASTRO. ASTRO COVID-19 summary and guidelines. 2020. [Available from: https://www.astro.org/Daily-Practice/COVID-19-Recommendations-and-Information/Summary. [Google Scholar]
- 12. ACS. Recommendations for prioritization, treatment and triage of breast cancer patients during the COVID-19 pandemic: Executive summary 2020. [Available from: https://www.facs.org/quality-programs/cancer/executive-summary. [DOI] [PMC free article] [PubMed]