Graphical abstract
Keywords: COVID-19, SARS-CoV-2, Protection Motivation Theory, Extended Theory of Planned Behavior, Lockdown
Highlights
-
•
PMT and ETPB were utilized to evaluate perceived effectiveness of COVID-19 prevention measures.
-
•
Understanding COVID-19 had effects on perceived vulnerability and perceived severity.
-
•
Perceived vulnerability and perceived severity had effects on intention to follow.
-
•
Intention to follow had a significant effect on perceived effectiveness.
-
•
Understanding of COVID-19 had a significant effect on perceived effectiveness.
Abstract
Objective
The current study integrated Protection Motivation Theory (PMT) and extended Theory of Planned Behavior (TPB) to evaluate factors affecting the perceived effectiveness of COVID-19 prevention measures among Filipinos during Enhanced Community Quarantine (ECQ) in Luzon, Philippines.
Methods
A total of 649 Filipinos answered an online questionnaire, which contained 63 questions. Structural Equation Modeling (SEM) was utilized to derive the causal relationships of the latent variables construct.
Results
SEM showed that understanding of COVID-19 had significant direct effects on perceived vulnerability and perceived severity. Also, perceived vulnerability and perceived severity had significant indirect effects on intention to follow. Intention to follow had significant direct effects on actual behavior and adapted behavior, which subsequently led to perceived effectiveness. Of note, an understanding of COVID-19 was found to have a significant indirect effect on perceived effectiveness.
Conclusions
The current study is one of the first studies to analyze factors affecting the perceived effectiveness of COVID-19 prevention measures during the global pandemic. It is proposed that the integrated PMT and extended TPB of this study can be applied and extended to evaluate the perceived effectiveness of COVID-19 measures in other countries that are currently dealing with COVID-19 pandemic.
Introduction
Coronavirus (COVID-19), a highly transmittable disease that threatens the human population worldwide, is considered to be the third pandemic in the 21st century (Perlman, 2020). After the emergence of Middle East respiratory syndrome coronavirus (MERS-CoV) in Saudi Arabia and severe acute respiratory syndrome coronavirus (SARS-CoV) in China, a new SARS-like coronavirus was discovered last December 2019 (Zhou et al., 2020). The virus was linked to a wholesale seafood market in Wuhan, China, when an unknown pathogen was identified by the local hospitals in a group of patients who are accustomed to pneumonia (Zhu et al., 2020, Fan et al., 2020). Adnan Shereen et al. (2020) initially mentioned that patients who have been infected by the coronavirus in China might have gone to Wuhan where live animals were being sold. Later, Chinese researchers determined a human to human transmission of the virus and initially named the novel virus Wuhan coronavirus or 2019 novel coronavirus (2019-nCoV) (Adam et al., 2020).
The International Committee on Taxonomy of Viruses (ICTV) recently named the novel coronavirus SARS coronavirus 2 (SARS-COV-2), which is now generally called coronavirus disease 19 (COVID-19) (Gorbalenya et al., 2020a, Gorbalenya et al., 2020b). Details about this epidemic were released by the National Health Commission of China on January 12, 2020 (Wang et al., 2020). This virus outbreak has grown extensively to infect 13,575,158 people worldwide and has lead to 584,940 death cases as of July 17, 2020 (WHO, 2020a, WHO, 2020b). On March 11, 2020, the World Health Organization listed COVID-19 as a global pandemic.
Due to the global pandemic of COVID-19, several prevention measures were taken. A massive lockdown has been implemented by governments in several countries. In addition, “#StayAtHome" was promoted by the media to prevent the spread of COVID-19. Researchers are currently developing a vaccine; as yet, there is no effective medicine that has been invented for the treatment of COVID-19 infections (Paital et al., 2020). At the moment, the only remedial option is hospitalization and thorough care management. With few initial treatment medications, predicting the duration and final size of the virus in every country becomes critical for policymakers and public health authorities to prevent further spread of the outbreak.
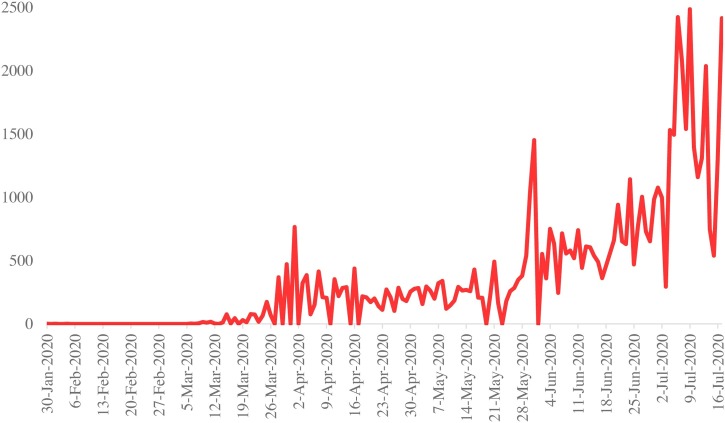
Despite the availability of different studies about preventive measures in other countries, there is a significant lack of academic research addressing the COVID-19 situation in the Philippines. On March 17, 2020, the country was placed under community quarantine for six months (CSIS, 2020). However, on July 16, 2020, the Philippines was declared to have the highest number of active cases in Southeast Asia (Table 1 ). The Department of Health of the Philippines (DoH) reported 61,266 confirmed cases of the infection and 1643 deaths in the Philippines as of July 17, 2020 (Figure 1 ).
Table 1.
COVID-19 cases in Southeast Asia as of July 17, 2020 (https://www.worldometers.info/coronavirus/).
| Rank | Country | Total cases | New cases | Total deaths | New deaths | Total recovered | Active cases |
|---|---|---|---|---|---|---|---|
| 1 | Philippines | 63,001 | 1841 | 1660 | 17 | 21,748 | 39,593 |
| 2 | Indonesia | 83,130 | 1462 | 3957 | 84 | 41,834 | 37,339 |
| 3 | Singapore | 47,453 | 327 | 27 | 0 | 43,256 | 4170 |
| 4 | Malaysia | 8755 | 18 | 122 | 0 | 8541 | 92 |
| 5 | Thailand | 3239 | 3 | 58 | 0 | 3096 | 85 |
| 6 | Myanmar | 339 | 0 | 6 | 0 | 270 | 63 |
| 7 | Cambodia | 171 | 5 | 0 | 0 | 133 | 38 |
| 8 | Vietnam | 382 | 1 | 0 | 0 | 356 | 26 |
| 9 | Brunei | 141 | 0 | 3 | 0 | 138 | 0 |
| 10 | East Timor | 24 | 0 | 0 | 0 | 24 | 0 |
| 11 | Laos | 19 | 0 | 0 | 0 | 19 | 0 |
Figure 1.
Confirmed COVID-19 cases in the Philippines as of July 17, 2020 (https://covid19.who.int/).
On March 16, 2020, The Philippine government imposed a total lockdown in Luzon, known as the Enhanced Community Quarantine (ECQ), as a preventive measure to minimize the COVID-19 outbreak. This ECQ is widely known as one of the longest lockdown in the world. Under the ECQ, all modes of domestic travel, including ground, air, and sea, were suspended. Residents were not allowed to leave their homes except in case of emergencies. Border closures and entry bans were also enforced. Thousands of police officers and military personnel were deployed at checkpoints to ensure that people complied with the lockdown. The administration also implemented, through several platforms as preventive measures, strict social distancing (Duddu, 2020, CSIS, 2020) and educated the community on healthy lifestyles.
The purpose of this study was to evaluate factors affecting the perceived effectiveness of COVID-19 prevention measures among Filipinos during ECQ in Luzon, Philippines, by integrating Protection Motivation Theory (PMT) and extended Theory of Planned Behavior (TPB). The current study is one of the first studies to have analyzed factors affecting the perceived effectiveness of COVID-19 prevention measures during the 2020 global pandemic. Finally, the integrated PMT and extended TPB of this study can be applied and extended to evaluate the perceived effectiveness of COVID-19 measures in other countries that are currently dealing with the COVID-19 pandemic.
Theoretical Research Framework
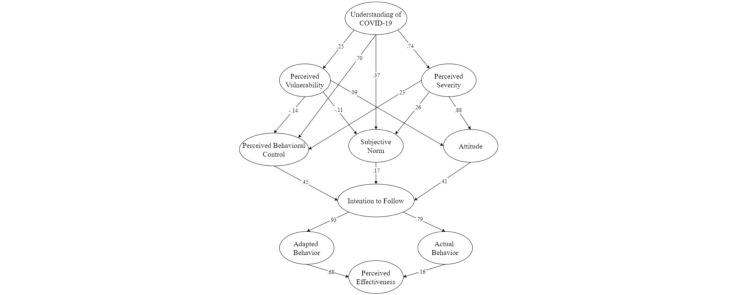
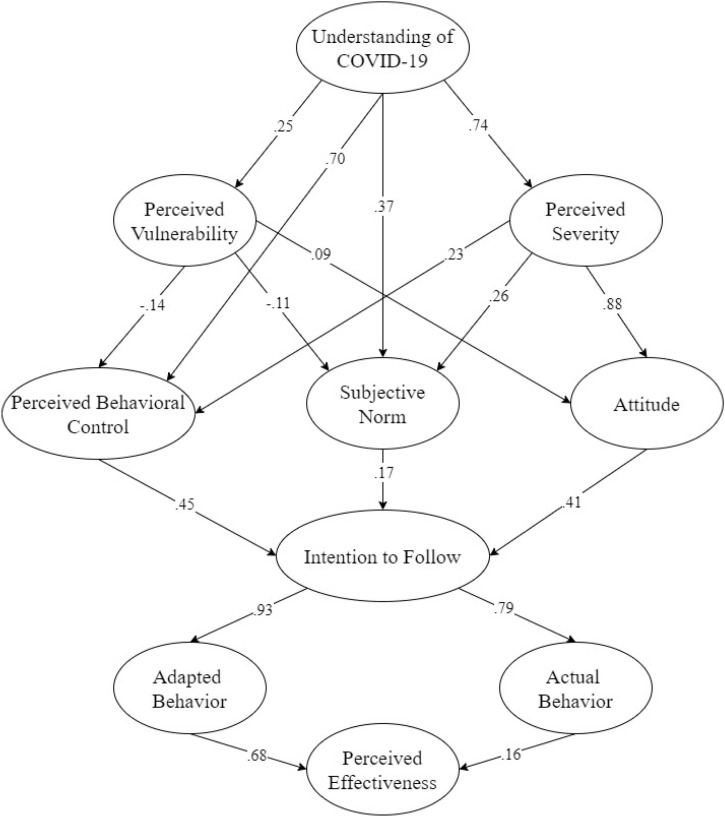
Figure 2 represents the Theoretical Research Framework of the current study. Unlike a previous study that only utilized PMT related to COVID-19 (Barati et al., 2020), we integrated the PMT and extended TPB to determine the causal relationships between determined variables and latent assemblies. The final goal was to evaluate factors affecting the perceived effectiveness of COVID-19 prevention measures among Filipinos during ECQ in Luzon.
Figure 2.
Theoretical research framework.
Based on PMT, when individuals encounter a threatening event, they are primarily motivated to engage in protective behavior (Janmaimool, 2017). According to previous research, individuals believe that performing preventive behavior can reduce the threat that comes with a lack of action (Hung et al., 2014). During a global crisis, providing reliable and accurate information is essential. In 2009, the public believed that the H1N1 virus was more lethal than H5N1 human avian flu and SARS because various forms of new infectious diseases were merged together (Lau et al., 2009). Early knowledge of the outbreak can help to illustrate the public’s risk behavior and how they perceived it (Balkhy et al., 2010). Moreover, Johnson and Hariharan (2017) highlighted that providing health education and creating awareness during an outbreak is an effective measure to help prevent the spread of the disease. Thus, we hypothesized the following:
H1
Understanding of COVID-19 had a significant direct effect on perceived vulnerability.
H2
Understanding of COVID-19 had a significant direct effect on perceived severity.
Health understanding and perceived behavioral control have been frequently identified as predictors of individuals' tendency to follow the prescribed prescription, and subsequently conform to treatment procedures (Davis et al., 2006). Bandura (1977) stated that the essential predictor of various medical behaviors, including medication adherence, is perceived behavioral control. However, Cameron et al. (2010) point out that taking medication as prescribed is the patient's responsibility. It is not an unusual occurrence if, due to inadequate knowledge, a patient fails to understand how to properly administer medication, either misuse, or non-adherence (Cameron et al., 2010). Moreover, this pivotal dispute of misconception and ignorance of directions for prescribed pharmaceutical products, particularly for people with poor health literacy (Cameron et al., 2010), is associated with avoidance of preventive care and worse outcomes in many chronic medical conditions (Berkman et al., 2011). Thus, we hypothesized the following:
H3
Understanding of COVID-19 had a significant direct effect on the perceived behavioral control of an individual.
Based on the Theory of Planned Behavior, a person’s behavioral intent is profoundly affected by the behavioral norms of his social community (Ajzen, 2011). A critical stage in this approach is a thorough exposition of the problem that was accomplished by intensive engagement with the various communities, leading to stronger cultural norms (Biglan and Taylor, 2000). Thus, it is logical to conclude that the stronger the group standards, the higher the level of understanding among the social community members. Hence, we proposed:
H4
Understanding of COVID-19 had a significant direct effect on subjective norms about the preventive measures implemented in the Philippines.
Mishra et al., (2016) mentioned that healthcare professionals exhibit a greater understanding of pandemic, optimistic attitudes towards the pandemic, and frequently exhibit low rates of anxiety. On the contrary, research from Ethiopia recommended intensive preparation for healthcare practitioners due to their inadequate knowledge and erroneous beliefs about the Ebola virus (Abebe et al., 2016). During the H1N1 pandemic in 2016, a study conducted in Trinidad and Tobago reported that a substantial proportion of the general population was oblivious of the severity of, and the prevention measures for coping with the epidemic (Johnson and Hariharan, 2017). A related study found that most respondents among secondary school- children in Nigeria had insufficient awareness and had a negative approach to the Ebola virus (Ilesanmi and Alele, 2016). Along with hypotheses 1 and 2, we also hypothesized the following:
H5
Understanding of Covid-19 had a significant direct effect on an individual’s attitude towards the ongoing global outbreak.
Most studies about health-related behaviors have utilized TPB (Gabriel et al., 2019, Hagger et al., 2016, Huang et al., 2020) or PMT separately (Barati et al., 2020). TPB specifies that attitudes, subjective norms, and perceived behavioral control are the essential components of behavioral intent and actual health-related behavior (Kam et al., 2008). However, there is little to no discussion of a relationship between TPB and PMT. Hence, the current model attempts to correlate factors associated with PMT to the key determinants of TPB. Thus, we hypothesized the following:
H6
Perceived vulnerability had a significant direct effect on perceived behavioral control.
H7
Perceived severity had a significant direct effect on perceived behavioral control.
H8
Perceived vulnerability had a significant direct effect on subjective norms.
H9
Perceived severity had a significant direct effect on subjective norms.
H10
Perceived vulnerability had a significant direct effect on an individual’s attitude towards COVID-19.
H11
Perceived severity had a significant direct effect on an individual’s attitude towards COVID-19.
Lau et al. (2010) mentioned that the variables of behavioral intention are directly correlated to the factors derived from the TPB. According to Ajzen (1991), self-efficacy is an element that is common to both TPB and PMT, which has the same concept of perceived behavioral control. It highlights the skills and competencies of a person handling the task or decision making (Bandura, 1998; Bandura, 1978). Workman et al. (2008) also showed that self-efficacy has a significant effect on the capability of a person to perform task behavior. Hence, we hypothesize the following:
H12
Perceived behavioral control had a significant direct effect on the intention to follow the preventive measures of COVID-19.
Subjective norm is defined as the normative rewards, values, and desires to adhere to a specific act, which is primarily expressed by observing others' behaviors (Ajzen, 1991, Aronson et al., 2020). Past study (Chan et al., 2005) has reported that the behavior of an individual is affected by the norm in their community. In the context of the individual’s compliance in organizations, Chan et al. (2005) stated that when supervisors and employees confer, cooperate and follow the guidelines, employees are most likely to comply with the organization’s guidelines. Also, most studies have proven that there is a strong relationship between subjective norms and compliance in organizations (Ho et al., 2017, Schepers and Wetzels, 2007, Grimes and Marquardson, 2019). However, some studies mentioned that the subjective norms construct is usually a poor indicator of behavioral intention since a person's behavior may be affected by societal influences and personal choices (Armitage and Conner, 2001). Thus, we hypothesized the following:
H13
Subjective norms had a significant direct effect on an individual’s behavioral intention to follow the preventive measures of COVID-19.
Attitude towards behavior refers to the perception of the individual performing a particular behavior. Most studies have confirmed that people will comply with rules, requirements, and guidelines when they have a positive attitude (Mcmillan and Conner, 2003, Sasse et al., 2020, Ng et al., 2009, Herath and Rao, 2009, Bulgurcu et al., 2010). On the other hand, people who disregard certain desirable habits do not adhere readily to the implemented guidelines (Pahnila et al., 2007, Myyry et al., 2009). Hence, we hypothesized that:
H14
Attitude had a significant direct effect on an individual’s behavioral intention to follow the preventive measures of COVID-19.
Behavioral intent is defined as the subjective probability that an individual will execute a particular behavior (Mahardika et al., 2020). It is depicted as the best possible predictor of an individual's action, despite the many factors that may affect the effectiveness of the intention-behavior relationship (Bentler and Speckart, 1979). Previously, Bentler and Speckart (1979) proposed a model that complements the Hill et al. (1977) theory in predicting behavior. Thus, we hypothesized the following:
H15
Behavioral intention had a significant direct effect on the actual behavior of individuals.
H16
Behavioral intention had a significant direct effect on the adapted behavior of individuals.
Previous studies emphasized that the feeling that individuals can only have a negligible impact on a larger scale is a major barrier for socially responsible behavior (Ellen et al., 1991). According to Owens (2000), individuals may perceive their actions as irrelevant on a larger scale even if they have an awareness of the situation and desire to contribute to society. Consequently, in addition to maintaining prosocial values, the perception that one's actions will make a difference is a necessary precursor to socially responsible behavior. For example, in a study of social activism, only those who perceived their actions as effective, acted on their beliefs (Hinkle et al., 1996). Hence, we hypothesized the following:
H17
Actual behavior had a significant direct effect on the perceived effectiveness of COVID-19 preventive measures implemented in Luzon, Philippines.
H18
Adapted behavior had a significant direct effect on the perceived effectiveness of COVID-19 preventive measures implemented in Luzon, Philippines.
Methodology
Participants
The current study utilized a cross-sectional design. An online questionnaire was distributed from May 7 to May 11, 2020, since it was not possible to do a community-based sampling during ECQ in Luzon, Philippines. A total of 649 Filipinos between 15–75 years old (mean: 27.76; standard deviation: 10.64) answered the online questionnaire, which contained 63 questions.
Table 2 represents the descriptive statistics of the respondents. Among the 649 respondents, 57% of them were female, and 43% were male. Most respondents were between 15−24 years of age (60.9%). About 18.2% of the respondents were between the ages of 25 and 34, 10.8% were between 35 and 44 years, 6.6% were between 45 and 54 years, 2.9% were between 55 and 64 years, and only 0.6% were over 64 years. Approximately 1.2% of the respondents were elementary school graduates, 18.2% were high school graduates, 8.9% were college graduates, 4.2% were master graduates, and only 0.6% were doctoral graduates. Most of the respondents have a monthly salary/allowance of less than PHP15,000 (40.8%). About 31.1% of the respondents have a monthly salary/allowance of PHP15,000–PHP30,000, 7.6% of them have a monthly salary/allowance of PHP30,000–PHP45,000, 4.9% have a salary/allowance of PHP45,000–PHP60,000 monthly, 2.8% have a monthly salary/allowance of PHP60,000–PHP75,000, and 12.8% of the respondents have a salary/allowance of more than PHP75,000 monthly. Most respondents answered that they are currently enrolled in health insurance (56.9%), while only 43.1% were not.
Table 2.
Descriptive statistics of the respondents (n = 649).
| Characteristics | Category | N | % |
|---|---|---|---|
| Gender | Male | 279 | 43 |
| Female | 370 | 57 | |
| Age | 15−24 | 395 | 60.9 |
| 25−34 | 118 | 18.2 | |
| 35−44 | 70 | 10.8 | |
| 45−54 | 43 | 6.6 | |
| 55−64 | 19 | 2.9 | |
| More than 64 | 4 | 0.6 | |
| Educational Background | Elementary graduate | 8 | 1.2 |
| High school graduate | 118 | 18.2 | |
| Senior high school graduate | 58 | 8.9 | |
| Technical-vocational graduate | 7 | 1.1 | |
| College graduate | 427 | 65.8 | |
| Master graduate | 27 | 4.2 | |
| PhD graduate | 4 | 0.6 | |
| Monthly Salary/ Allowance | <15.000 PHP | 265 | 40.8 |
| 15.000–30.000 PHP | 202 | 31.1 | |
| 30.000–45.000 PHP | 49 | 7.6 | |
| 45.000–60.000 PHP | 32 | 4.9 | |
| 60.000–75.000 PHP | 18 | 2.8 | |
| >75.000 PHP | 83 | 12.8 | |
| Enrolled in health insurance? | Yes | 369 | 56.9 |
| No | 280 | 43.1 |
Questionnaire
Following our theoretical framework, a self-administered questionnaire was developed for this study to evaluate factors affecting the perceived effectiveness of COVID-19 prevention measures during the ECQ in Luzon, Philippines (Table 3 ). The questionnaire consists of eleven sections: (1) Demographic Information (gender, age, educational attainment, monthly income/allowance, and health insurance), (2) Perceived Vulnerability, (3) Perceived Severity, (4) Understanding of COVID-19, (5) Attitude, (6) Subjective Norm, (7) Perceived Behavioral Control, (8) Intention to Follow, (9) Actual Behavior, (10) Adapted behavior, and (11) Perceived Effectiveness. All latent constructs included in the SEM were measured by utilizing a 5-point Likert scale.
Table 3.
The constructs and measurement items.
| Construct | Items | Measures | Supporting References |
|---|---|---|---|
| Understanding of COVID-19 | U1 | I do understand the transmission of COVID-19 | Liu (2020); Shim et al. (2020); Nicola et al. (2020) |
| U2 | I do understand the incubation period of COVID -19 | Coccia (2020) | |
| U3 | I do understand the symptoms of COVID -19 | Li et al. (2020) | |
| U4 | I do understand the protocol if I have symptoms that might lead to COVID-19 | ||
| U5 | I do understand which hospital can treat COVID -19 patients. | Nicola et al. (2020) | |
| Perceived Vulnerability | PV1 | I think I am very vulnerable to COVID -19. | Díaz et al. (2016) |
| PV2 | I think my neighborhood is very vulnerable to COVID -19. | Coccia (2020) | |
| PV3 | My past experiences make me believe that I am likely to get sick when my friends are sick. | Díaz et al. (2016) | |
| PV4 | I have a history of susceptibility to infectious diseases. | Díaz et al. (2016) | |
| PV5 | I think there is a chance that my family will be infected by COVID -19 | Nicola et al. (2020); Coccia (2020) | |
| Perceived Severity | PS1 | I find COVID -19 is a serious disease. | Paital et al. (2020); Basheti et al. (2020) |
| PS2 | I find COVID -19 can lead to death. | Barati et al. (2020) | |
| PS3 | I find COVID -19 is more severe than any other disease. | Barati et al. (2020) | |
| PS4 | I find COVID -19 can affect mental health. | Burgelt et al. (2009); Tanoue et al. (2020); Grover et al. (2020) | |
| PS5 | I think it’s very expensive to pay the medical expenses for COVID -19. | ||
| PS6 | I think the COVID -19 outbreak will continue at least until the following 3 months. | Cássaro and Pires (2020) | |
| PS7 | I think the COVID-19 outbreak in my country is more severe than in other countries. | ||
| Attitude | AT1 | I worry about the number of people infected by COVID -19. | Sarkodie and Owusu (2020); Mi et al. (2020) |
| AT2 | I feel stressed during the COVID-19 outbreak. | Shader (2020) | |
| AT3 | I am afraid that one of my family members will get infected. | Dariya and Nagaraju (2020) | |
| AT4 | I feel anxious during COVID -19 outbreak. | Roy et al. (2020) | |
| AT5 | I feel insecure if someone stands too close to me during COVID -19 outbreak. | Roy et al. (2020) | |
| AT6 | I feel insecure if someone is not wearing a mask during the COVID-19 outbreak. | D’Amours (2020) | |
| AT7 | I feel insecure if someone sneezes or coughs next to me. | Centers for Diseases Control and Prevention (2020) | |
| Subjective Norm | SN1 | Most people I know are following the preventive protocols given by the government. | Centers for Diseases Control and Prevention (2020) |
| SN2 | Most people I know are wearing face masks outside. | Conner (2020); Rubio-Romero et al. (2020) | |
| SN3 | Most people I know are staying at home and work from home. | Yancey-Bragg and Bravo (2020) | |
| SN4 | Most people I know are using hand sanitizer | USA Food and Drug Administration (2020) | |
| SN5 | Most people I know, are doing physical distancing. | Adam (2020) | |
| Perceived Behavioral Control | PBC1 | The preventive protocols are completely up to me. | Sato (2018) |
| PBC2 | I think preventive protocols are easy to be implemented. | Shen et al. (2020) | |
| PBC3 | I am confident that I can prevent getting infected by COVID -19. | Veldhuijzen et al. (2006) | |
| PBC4 | I am confident that I have enough knowledge about COVID -19. | Barati et al. (2020) | |
| Intention to Follow | IF1 | I am willing to follow the recommended precautions until the end of the COVID-19 outbreak. | Barati et al. (2020) |
| IF2 | I am willing to stay at home during COVID -19 outbreak. | Sen-Crowe et al. (2020) | |
| IF3 | I am willing to follow every rule made by my government during the COVID-19 outbreak. | Oyeniran and Chia (2020) | |
| IF4 | I am willing to reschedule my travel plans. | Lee et al. (2020); World Health Organization (2020a; World Health Organization (2020b) | |
| IF5 | I am willing to follow my government to lock down the country, city, and community. | University of Michigan School of Public Health (2020) | |
| Actual Behavior | AB1 | I am practicing proper handwashing to prevent the spread of the virus. | UNICEF (2020); Luo et al. (2020) |
| AB2 | I use hand sanitizer more often during the COVID-19 outbreak. | Pradhan et al. (2020) | |
| AB3 | I always wash my hands whenever I go outside. | New Zealand Government (2020) | |
| AB4 | I practice 1-meter social distancing to reduce unnecessary infections. | Wu and Mcgoogan (2020) | |
| AB5 | The company/school where I work/study implements work from home to prevent the spread of COVID-19. | Public Health of England (2020) | |
| AB6 | I always wear a face mask whenever I go outside during the COVID-19 outbreak. | Shaw et al. (2020) | |
| AB7 | I always dispose of my face mask properly. | Feng et al. (2020) | |
| Adapted Behavior | AD1 | I maintain a healthy lifestyle during the COVID-19 outbreak. | FAO (2020) |
| AD2 | I keep working from home during the COVID-19 outbreak. | Gorlick (2020) | |
| AD3 | I don't smoke during the COVID-19 outbreak. | Taghizadeh-Hesary and Akbari (2020) | |
| AD4 | I don't drink alcohol during the COVID-19 outbreak. | Feuer (2020) | |
| AD5 | I sleep at least 7 h per day during the COVID-19 outbreak. | Medalie (2020) | |
| Perceived Effectiveness | PE1 | I think the preventive protocols for the COVID-19 outbreak in my country are effective. | WHO (2020a) |
| PE2 | I think the preventive protocols for the COVID-19 outbreak in my community are informative. | WHO (2020b) | |
| PE3 | I think a healthy lifestyle will enhance my immunity. | Rula (2020) | |
| PE4 | I think social distancing can prevent the transmission of COVID-19. | Matrajt and Leung (2020) | |
| PE5 | I think a face mask can prevent the transmission of COVID-19. | Geggel (2020) | |
| PE6 | I think proper hygiene can prevent the transmission of COVID-19. | Centers for Diseases Control and Prevention (2020) | |
| PE7 | I think lockdown is an effective way to prevent COVID-19. | Sasikumar (2020) |
Structural Equation Modeling
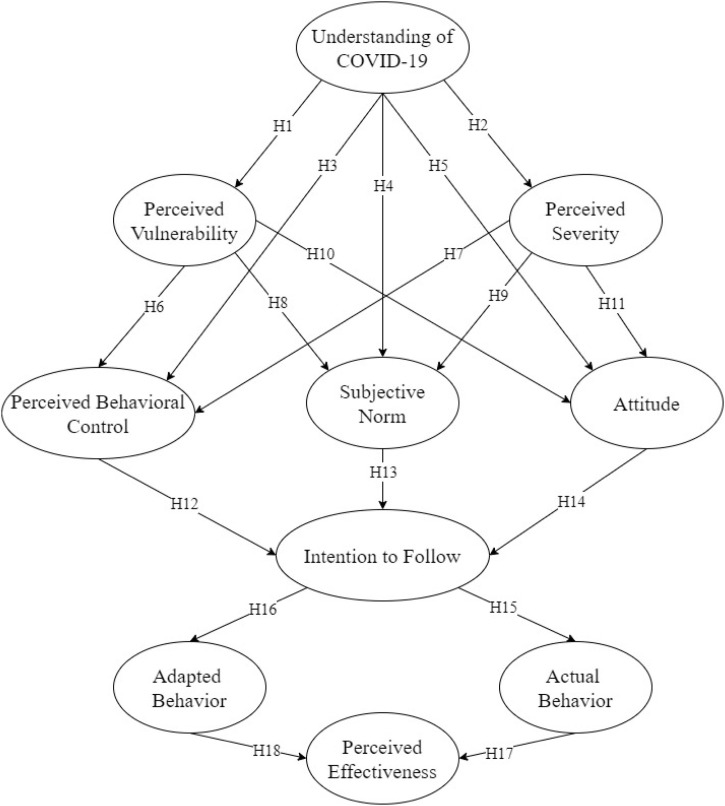
Structural Equation Modeling (SEM) is an advanced statistical approach mainly designed to describe causal relationships between the latent variables construct (Hair, 2010; Martinez et al., 2019, Torres et al., 2019). AMOS 22 with the Maximum Likelihood estimation approach was utilized to run the SEM. Figure 3 demonstrates that the SEM construct had ten latent variables with one exogenous latent variable (Understanding of COVID-19) and nine endogenous latent variables (Perceived Vulnerability, Perceived Severity, Perceived Behavioral Control, Subjective Norms, Intention to Follow, Adapted Behavior, Actual Behavior, and Perceived Effectiveness).
Figure 3.
Initial SEM with indicators for evaluating the perceived effectiveness of COVID-19 prevention measures during ECQ in Luzon, Philippines.
Following some previous studies (Chin et al., 2018, Lin et al., 2017, Nadlifatin et al., 2016), six sets of measurements were used to analyze the model’s fit: Incremental Fit Index (IFI), Tucker Lewis Index (TLI), Comparative Fit Index (CFI), Goodness of Fit Index (GFI), Adjusted Goodness of Fit Index (AGFI), and Root Mean Square Error of Approximation (RMSEA). For IFI, TLI, and CFI, a value greater than 0.90 indicates a good model fit (Hair, 2010, Hu and Bentler, 1999). Similar to R2 in the multiple linear regression (Lin et al., 2019a), a value greater than 0.80 is the minimum indication of a good model fit for GFI and GFI (Gefen et al., 2000). Finally, a value smaller than 0.07 is also an indication of a good model fit for RMSEA (Steiger, 2007).
Results
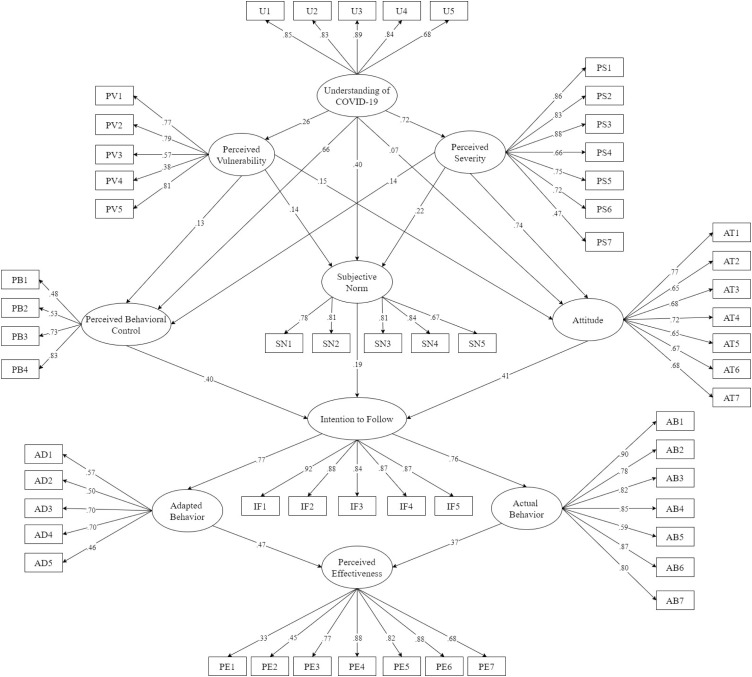
Figure 3 demonstrates the initial SEM for evaluating the perceived effectiveness of COVID-19 prevention measures among Filipinos during ECQ in Luzon, Philippines. According to the figure below, one hypothesis was not significant: Understanding of COVID-19 to Attitude (Hypothesis 5). Therefore, a revised SEM was derived by removing this hypothesis. Following some of our previous studies that utilized the SEM approach (Lin et al., 2018, Lin et al., 2019b, Miraja et al., 2019), some modification indices were applied to enhance the model fit. Figure 4 demonstrates the final SEM for evaluating the perceived effectiveness of COVID-19 prevention measures during ECQ in Luzon, Philippines, and Table 4 demonstrates the descriptive statistic results of each indicator. As presented in Table 5 , the IFI, TLI, and CFI values were greater than the suggested cutoff of 0.90, indicating that the specified model's hypothesized construct was an excellent representation of the observed data. In addition, the GFI and AGFI values were 0.842 and 0.820, respectively, indicating that the model was also good. The RMSEA value was 0.044, which is also lower than the recommended value. Finally, the direct, indirect, and total effects are presented in Table 6 .
Figure 4.
The Final SEM for evaluating the perceived effectiveness of COVID-19 prevention measures during ECQ in Luzon, Philippines.
Table 4.
Descriptive statistic results.
| Factor | Item | Mean | StDev | Factor Loading |
|
|---|---|---|---|---|---|
| Initial Model | Final Model | ||||
| Understanding of COVID-19 | U1 | 4.30 | 0.80 | 0.85 | 0.87 |
| U2 | 4.20 | 0.81 | 0.83 | 0.80 | |
| U3 | 4.30 | 0.74 | 0.89 | 0.88 | |
| U4 | 4.28 | 0.75 | 0.84 | 0.86 | |
| U5 | 3.90 | 0.95 | 0.68 | 0.69 | |
| Perceived Vulnerability | PV1 | 3.08 | 1.05 | 0.77 | 0.68 |
| PV2 | 3.28 | 1.03 | 0.79 | 0.64 | |
| PV3 | 2.89 | 1.13 | 0.57 | 0.58 | |
| PV4 | 2.23 | 1.09 | 0.38 | 0.41 | |
| PV5 | 2.85 | 1.15 | 0.81 | 0.67 | |
| Perceived Severity |
PS1 | 4.60 | 0.73 | 0.86 | 0.87 |
| PS2 | 4.42 | 0.79 | 0.83 | 0.80 | |
| PS3 | 3.84 | 1.00 | 0.88 | 0.55 | |
| PS4 | 4.14 | 0.90 | 0.66 | 0.64 | |
| PS5 | 4.38 | 0.88 | 0.75 | 0.72 | |
| PS6 | 4.26 | 0.85 | 0.72 | 0.71 | |
| PS7 | 3.66 | 1.12 | 0.47 | 0.42 | |
| Attitude | AT1 | 4.34 | 0.84 | 0.77 | 0.84 |
| AT2 | 3.81 | 0.94 | 0.65 | 0.57 | |
| AT3 | 4.16 | 0.98 | 0.68 | 0.66 | |
| AT4 | 3.88 | 0.96 | 0.72 | 0.62 | |
| AT5 | 3.85 | 0.97 | 0.65 | 0.52 | |
| AT6 | 4.03 | 0.94 | 0.67 | 0.57 | |
| AT7 | 4.20 | 0.91 | 0.68 | 0.62 | |
| Subjective Norm | SN1 | 3.91 | 0.91 | 0.78 | 0.79 |
| SN2 | 4.14 | 0.86 | 0.81 | 0.82 | |
| SN3 | 4.08 | 0.89 | 0.81 | 0.81 | |
| SN4 | 4.00 | 0.90 | 0.84 | 0.82 | |
| SN5 | 3.86 | 0.97 | 0.67 | 0.80 | |
| Perceived Behavioral Control | PBC1 | 3.79 | 1.15 | 0.48 | 0.45 |
| PBC2 | 3.61 | 1.04 | 0.53 | 0.41 | |
| PBC3 | 3.87 | 0.93 | 0.73 | 0.56 | |
| PBC4 | 4.06 | 0.81 | 0.83 | 0.75 | |
| Intention to Follow | IF1 | 4.51 | 0.74 | 0.92 | 0.91 |
| IF2 | 4.43 | 0.80 | 0.88 | 0.84 | |
| IF3 | 4.33 | 0.87 | 0.84 | 0.79 | |
| IF4 | 4.53 | 0.77 | 0.87 | 0.87 | |
| IF5 | 4.40 | 0.84 | 0.87 | 0.82 | |
| Actual Behavior | AB1 | 4.47 | 0.77 | 0.90 | 0.91 |
| AB2 | 4.35 | 0.85 | 0.78 | 0.79 | |
| AB3 | 4.51 | 0.75 | 0.82 | 0.92 | |
| AB4 | 4.39 | 0.79 | 0.85 | 0.84 | |
| AB5 | 4.31 | 1.01 | 0.59 | 0.61 | |
| AB6 | 4.55 | 0.77 | 0.87 | 0.90 | |
| AB7 | 4.39 | 0.83 | 0.80 | 0.79 | |
| Adapted Behavior | AD1 | 3.98 | 0.95 | 0.57 | 0.54 |
| AD2 | 3.95 | 1.12 | 0.50 | 0.59 | |
| AD3 | 4.48 | 0.99 | 0.70 | 0.56 | |
| AD4 | 4.43 | 0.98 | 0.70 | 0.57 | |
| AD5 | 3.79 | 1.16 | 0.46 | 0.35 | |
| Perceived Effectiveness | PE1 | 3.09 | 1.17 | 0.33 | 0.29 |
| PE2 | 3.41 | 1.05 | 0.45 | 0.41 | |
| PE3 | 4.31 | 0.81 | 0.77 | 0.85 | |
| PE4 | 4.27 | 0.83 | 0.88 | 0.82 | |
| PE5 | 4.15 | 0.87 | 0.82 | 0.77 | |
| PE6 | 4.44 | 0.78 | 0.88 | 0.94 | |
| PE7 | 4.11 | 0.99 | 0.68 | 0.71 | |
Table 5.
Model Fit.
| Goodness of fit measures of the SEM | Parameter Estimates | Minimum cutoff |
Suggested by |
|---|---|---|---|
| Incremental Fit Index (IFI) | 0.928 | >0.90 | Hair (2010) |
| Tucker Lewis Index (TLI) | 0.920 | >0.90 | Hu and Bentler (1999) |
| Comparative Fit Index (CFI) | 0.927 | >0.90 | Hair (2010) |
| Goodness of Fit Index (GFI) | 0.842 | >0.80 | Gefen et al. (2000) |
| Adjusted Goodness of Fit Index (AGFI) | 0.820 | >0.80 | Gefen et al. (2000) |
| Root Mean Square Error of Approximation (RMSEA) | 0.044 | <0.07 | Steiger (2007) |
Table 6.
Direct effect, indirect effect, and total effect.
| No | Variables | Direct effect | P-value | Indirect effect | P-value | Total effect | P-value |
|---|---|---|---|---|---|---|---|
| 1 | U → PS | 0.739 | 0.001 | – | – | 0.739 | 0.001 |
| 2 | U → PV | 0.247 | 0.001 | – | – | 0.247 | 0.001 |
| 3 | U → AT | – | – | 0.670 | 0.001 | 0.670 | 0.001 |
| 4 | U → SN | 0.366 | 0.001 | 0.165 | 0.003 | 0.531 | 0.001 |
| 5 | U → PBC | 0.700 | 0.001 | 0.137 | 0.066 | 0.837 | 0.001 |
| 5 | U → IF | – | – | 0.746 | 0.001 | 0.746 | 0.001 |
| 6 | U → AB | – | – | 0.593 | 0.001 | 0.593 | 0.001 |
| 7 | U → AD | – | – | 0.692 | 0.001 | 0.692 | 0.001 |
| 8 | U → PE | – | – | 0.567 | 0.001 | 0.567 | 0.001 |
| 9 | PS → AT | 0.876 | 0.001 | – | – | 0.876 | 0.001 |
| 10 | PS → SN | 0.260 | 0.003 | – | – | 0.260 | 0.003 |
| 11 | PS → PBC | 0.231 | 0.028 | – | – | 0.231 | 0.028 |
| 12 | PS → IF | – | – | 0.510 | 0.001 | 0.510 | 0.001 |
| 13 | PS → AB | – | – | 0.405 | 0.001 | 0.405 | 0.001 |
| 14 | PS → AD | – | – | 0.473 | 0.001 | 0.473 | 0.001 |
| 15 | PS → PE | – | – | 0.387 | 0.001 | 0.387 | 0.001 |
| 16 | PV → AT | 0.092 | 0.018 | – | – | 0.092 | 0.018 |
| 17 | PV→ SN | −0.111 | 0.033 | – | – | −0.111 | 0.033 |
| 18 | PV → PBC | −0.136 | 0.009 | – | – | −0.136 | 0.009 |
| 19 | PV→IF | – | – | −0.043 | 0.255 | −0.043 | 0.255 |
| 20 | PV → AB | – | – | −0.034 | 0.238 | −0.034 | 0.238 |
| 21 | PV → AD | – | – | −0.040 | 0.248 | −0.040 | 0.248 |
| 22 | PV → PE | – | – | −0.032 | 0.243 | −0.032 | 0.243 |
| 23 | AT → IF | 0.413 | 0.001 | – | – | 0.413 | 0.001 |
| 24 | AT → AB | – | – | 0.328 | 0.001 | 0.328 | 0.001 |
| 25 | AT → AD | – | – | 0.383 | 0.001 | 0.383 | 0.001 |
| 26 | AT → PE | – | – | 0.313 | 0.001 | 0.313 | 0.001 |
| 27 | SBN → IF | 0.168 | 0.001 | – | – | 0.168 | 0.001 |
| 28 | SBN →IF | – | – | 0.134 | 0.001 | 0.134 | 0.001 |
| 29 | SBN → AB | – | – | 0.156 | 0.001 | 0.156 | 0.001 |
| 30 | SBN → AD | – | – | 0.128 | 0.001 | 0.128 | 0.001 |
| 31 | PBC → IF | 0.454 | 0.001 | – | – | 0.454 | 0.001 |
| 32 | PBD→AB | – | – | 0.361 | 0.001 | 0.361 | 0.001 |
| 33 | PBC→AD | – | – | 0.422 | 0.001 | 0.422 | 0.001 |
| 34 | PBC → PE | – | – | 0.345 | 0.001 | 0.345 | 0.001 |
| 35 | IF → AB | 0.794 | 0.001 | – | – | 0.794 | 0.001 |
| 36 | IF → AD | 0.928 | 0.001 | – | – | 0.928 | 0.001 |
| 37 | IF → PE | – | – | 0.759 | 0.001 | 0.759 | 0.001 |
| 38 | AB →PE | 0.163 | 0.011 | – | – | 0.163 | 0.011 |
| 39 | AD → PE | 0.679 | 0.001 | – | – | 0.679 | 0.001 |
Discussion
The current study integrated Protection Motivation Theory (PMT) and extended Theory of Planned Behavior (TPB) to evaluate factors affecting the perceived effectiveness of COVID-19 prevention measures among Filipinos during Enhanced Community Quarantine (ECQ) in Luzon, Philippines. SEM was utilized to analyze the interrelationship among understanding of COVID-19 (U), perceived vulnerability (PV), perceived severity (PS), attitude (AT), subjective norm (SBN), perceived behavioral control (PBC), intention to follow (IF), actual behavior (AB), adapted behavior (AD), and perceived effectiveness (PE). An online questionnaire was utilized and a total of 649 data samples were collected.
SEM indicated that understanding of COVID-19 had significant direct effects on PV (β:0.247, p = 0.001) and PS (β:0.739, p = 0.001). Khosravi (2020) stated that the public's assessment of the disease's danger is influenced by their understanding of a specific health hazard by perceived severity and vulnerability. Understanding of COVID-19, which is related to the transmission and incubation periods of the virus, the protocol when they catch symptoms that may lead to COVID-19, and the hospitals which can treat COVID-19 patients, would positively affect the perceived vulnerability and perceived severity. However, Reuben et al. (2020) mentioned in their study that under-privileged people and vulnerable people, especially the older adults, unemployed, illiterates, farmers, rural and semi-urban residents, are more likely to have poor knowledge about the COVID-19 due to limited or no access to gadgets and the internet. Hence, policymakers have to make sure that the community fully understands the virus and its symptoms as it can also enhance the perceived vulnerability and perceived severity of the disease.
As discussed before, the current study integrated the extended TPB wherein it was classified into three elements, perceived behavioral control (PB), subjective norm (SN), and attitude (AT). Based on the results, it proved that understanding of COVID-19 had significant direct effects on SN (β:0.366; p = 0.001) and PBC (β:0.700; p = 0.001). It could be interpreted that people can understand the virus if they are surrounded by people who are following the preventive protocols given by the government, such as wearing face masks outside, staying and working from home, using a hand sanitizer frequently, and practicing social distancing during the outbreak. Moreover, people are more confident if they understand the symptoms of COVID-19. Apart from the significant direct effects, the current model surprisingly showed that understanding COVID-19 had no significant direct effect on attitude, but it was found to have a significant indirect effect.
Regarding the perceived vulnerability, SEM indicated that PV had significant negative effects on PBC (β:-0.136; p = 0.009) and SN (β:-0.111; p = 0.033). It could be considered that individuals who are confident with their knowledge about COVID-19 and are surrounded by a community that is aware of a healthy lifestyle are most likely to think they are not vulnerable to the disease. Meanwhile, PV had a significant effect on AT (β:0.092, p = 0.018), which supports the claim of Prokop and Kubiatko (2014) that perceived vulnerability to disease is positively correlated with attitude. Hence, people who are worried about the number of people infected by COVID-19 are most likely to think they are vulnerable to it. On the other hand, PS was found to have positive effects on PBC (β: 0.231, p = 0.028), SN (β:0.260; p = 0.003), and AT (β:0.876; p = 0.001). The result indicates that people who perceived the severity of COVID-19 are more likely to have enough knowledge about the virus. Moreover, an individual who is surrounded by a community that is aware of a healthy lifestyle will help them understand how severe COVID-19 is.
Regarding the intention to follow, the current model proved the Lau et al. (2010) statement that factors derived from the TPB were significantly associated with behavioral intention. The result showed that intention to follow was significantly affected by PBC (β:0.454; p = 0.001), SBN (β:0.168; p = 0.001), and AT (β:0.413; p = 0.001) which has several implications. First, based on PBC, people with enough knowledge are more likely to stay at home and comply with the lockdown implementation of the country, city, and community. In a similar study by Seale et al. (2020), it was observed that strategies implemented by the government to subsidize the outbreak, such as social distancing and lowering the score if people do not fully understand the government strategy, could influence the wellbeing of the community. Second, based on SBN, individuals who are surrounded by people that are frequently using hand sanitizers are more likely to follow the recommended precautions during the COVID-19 outbreak. Lastly, based on AT, people who are worried about the number of infected people are most likely to follow every rule implemented by the government during the outbreak.
Meanwhile, it was found that the intention to follow had significant effects on AB (β:0.794; p = 0.001) and AD (β:0.928; p = 0.001). The result implies that the people's willingness to follow leads to a healthy behavior towards the recommended precautions. In addition, intention to follow tends to affect a few implications, such as proper hygiene and a healthy lifestyle. People are more likely to wash their hands, wear face masks, and avoid activities that would affect their immunity during the COVID-19 outbreak.
Subsequently, the results showed that AB was found to have a significant effect on PE (β: 0.163; p = 0.001). These make an implication that proper hand washing, use of microbial solutions, and social distancing would enhance the PE. Policymakers should implement these to create awareness and to prevent panic within the community (Balkhy et al., 2010). On the other hand, the SEM showed that AD would have a significant effect on PE (β:0.679; p = 0.001). The SEM indicated that a healthy lifestyle of people would help to achieve PE by increasing their immunity to avoid the transmission of the disease. Finally, the results imply that a healthy lifestyle, social distancing, face mask, proper hygiene, and lockdown would enhance the perceived effectiveness of COVID-19 preventive measures.
Surprisingly, the Understanding of COVID-19 had a significant indirect effect on perceived effectiveness (β:0.567; p = 0.001). Educating the community, particularly concerning the transmission period, the incubation period, the symptoms, the protocol if they have the symptoms, and the hospital that can treat COVID-19 would significantly lead to the perceived effectiveness of the prevention measures. Our results proved that the government and other stakeholders really need to educate the community about COVID-19, including the prevention measures.
In the Philippines, there are different quarantine levels that Inter-Agency Task Force for the Management of Emerging Infectious Diseases (IATF-EID) recommended; these are Enhanced Community Quarantine (ECQ), Modified Enhanced Community Quarantine (MECQ) for high-risk areas, and General Community Quarantine (GCQ) for moderate risk areas (Ranada, 2020). Cities such as Metro Manila, Laguna, and Cebu City were placed under MECQ from May 16 until May 31, 2020. MECQ, as defined by the IATF-EID, is the transition phase between ECQ and GCQ. During this phase, residents are still required to follow the government's implemented protocol, especially staying at home for people who are considered vulnerable and transmitters. Currently, some regions (e.g., Region II, Region III, Region IV, NCR) and provinces (e.g., Albay and Pangasinan) in Luzon are placed under GCQ, which has more relaxed measures compared to MECQ (GOVPH, 2020). The difference between GCQ and MECQ is that during the GCQ, transportation, excluding the jeepneys and buses, is now allowed but not at full capacity in compliance with strict social distancing. All industries and businesses are allowed to operate up to 75% and must follow strict protocols. Although our study was conducted during ECQ, our results are still valid during MECQ, and GCQ since the implemented preventive measures of the government are still in effect.
Despite the clear and substantial contributions, the authors would like to acknowledge several limitations of this study. First, the current study was mainly focused on perceived effectiveness rather than measuring the effectiveness of prevention measures themselves. A future study to correlate the perceived effectiveness and the number of cases would be a very promising topic. Second, our sample was collected through an online questionnaire. Future research to collect more samples in the community after ECQ would lead to more comprehensive results. Last but not least, we did not correlate the power of the media to the understanding of COVID-19. Future studies should also incorporate people's trust in information and outcome expectations as one of the essential predictors of behavioral intention to follow.
Conclusion
The COVID-19 pandemic is a global crisis in 2020. It has grown extensively to infect 10,185,374 people worldwide, with 503,862 deaths as of June 30, 2020 (WHO, 2020a, WHO, 2020b). In the Philippines, there have been 36,438 confirmed cases of the infection and 1255 deaths as of June 29, 2020, leading the government to enact several preventive measures such as ECQ in Luzon. The current study integrated Protection Motivation Theory (PMT) and extended Theory of Planned Behavior (TPB) to evaluate factors affecting the perceived effectiveness of COVID-19 prevention measures among Filipinos during Enhanced Community Quarantine (ECQ) in Luzon, Philippines. A total of 649 Filipinos answered the online questionnaire, which contained 63 questions. The results of Structural Equation Modeling (SEM) indicated that understanding of COVID-19 had significant direct effects on perceived vulnerability and perceived severity. In addition, perceived vulnerability and perceived severity had significant indirect effects on intention to follow. Intention to follow had significant direct effects on actual behavior and adapted behavior, which subsequently leads to perceived effectiveness.
Interestingly, an understanding of COVID-19 was found to have a significant indirect effect on perceived effectiveness. The current study is one of the first studies that analyzed factors affecting the perceived effectiveness of COVID-19 prevention measures during the global pandemic. Finally, the integrated PMT and extended TPB of this study can be applied and extended to evaluate the perceived effectiveness of COVID-19 measures in other countries that currently dealing with COVID-19 pandemic.
Conflict of interest
None declared.
Authors’ contributions
YTP, as the first and the corresponding author, was responsible for the paper's conceptualization as well as securing the funding from Mapúa University DRIVE, running SEM in AMOS, and finalizing the manuscript. AMC, LJS, JAS, and JAS designed the framework, collected data, and prepared the manuscript. All authors significantly contributed to the revisions of the manuscript.
Funding
The authors would like to thank Mapúa University Directed Research for Innovation and Value Enhancement (DRIVE) for funding this study.
Ethical approval
Approval was not required.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.ijid.2020.07.074.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- Abebe T.B., Bhagavathula A.S., Tefera Y.G., Ahmad A., Khan M.U., Belachew S.A. Healthcare professionals’ awareness, knowledge, attitudes, perceptions and beliefs about Ebola at Gondar University Hospital, Northwest Ethiopia: a cross-sectional study. J Public Health Afr. 2016;7(2) doi: 10.4081/jphia.2016.570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adam D. 2020. The Effects of Physical Isolation on the Pandemic Quantified.https://www.the-scientist.com/news-opinion/the-effects-of-physical-isolation-on-the-pandemic-quantified-67407 April, Retrieved from. [Google Scholar]
- Adnan Shereen M., Khan S., Kazmi A., Bashir N., Siddique R. COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. J Adv Res. 2020 doi: 10.1016/j.jare.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. doi: 10.1016/0749-5978(91)90020-t. [DOI] [Google Scholar]
- Ajzen I. McGraw-Hill/Open University Press; Maidenhead, England: 2011. Attitudes, Personality and Behavior. [Google Scholar]
- Armitage C.J., Conner M. Efficacy of the theory of planned behaviour: a meta-analytic review. Br J Social Psychol. 2001;40(4):471–499. doi: 10.1348/014466601164939. [DOI] [PubMed] [Google Scholar]
- Aronson E., Wilson T.D., Akert R.M. Pearson; New Jersey: 2020. Social Psychology. [Google Scholar]
- Balkhy H.H., Abolfotouh M.A., Al-Hathlool R.H., Al-Jumah M.A. Awareness, attitudes, and practices related to the swine influenza pandemic among the Saudi public. BMC Infect Dis. 2010;10(1) doi: 10.1186/1471-2334-10-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. doi: 10.1037/0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Adv Behav Res Ther. 1978;1(4):139–161. doi: 10.1016/0146-6402(78)90002-4. [DOI] [PubMed] [Google Scholar]
- Barati M., Bashirian S., Jenabi E., Khazaei S., Karimi-Shahanjarini A., Zareian S. Factors associated with preventive behaviours of COVID-19 among hospital staff in Iran in 2020: an application of the Protection Motivation Theory. J Hosp Infect. 2020 doi: 10.1016/j.jhin.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basheti I.A., Nassar R., Barakat M., Alqudah R., Abufarha R., Mukattash T.L. Pharmacists’ readiness to deal with the coronavirus pandemic: assessing awareness and perception of roles. Res Social Administrative Pharm. 2020 doi: 10.1016/j.sapharm.2020.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentler P.M., Speckart G. Models of attitude-behavior relations. Psychol Rev. 1979;86(5):452–464. doi: 10.1037/0033-295x.86.5.452. [DOI] [Google Scholar]
- Berkman N.D., Sheridan S.L., Donahue K.E., Halpern D.J., Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Inter Med. 2011;155(2):97. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- Biglan A., Taylor T.K. Why have we been more successful in reducing tobacco use than violent crime? Am J Community Psychol. 2000;28(3):269–302. doi: 10.1023/a:1005155903801. [DOI] [PubMed] [Google Scholar]
- Bulgurcu Burcu, Cavusoglu Hasan, Benbasat Izak. Information security policy compliance: an empirical study of rationality-based beliefs and information security awareness. MIS Q. 2010;34(3):523. doi: 10.2307/25750690. [DOI] [Google Scholar]
- Burgelt Petra Topaz, Paton D., Johnston D.M. GNS Science; Lower Hutt, N.Z: 2009. Factors and Processes Influencing Individual and Community Preparedness for a Pandemic Outbreak in New Zealand. [Google Scholar]
- Cameron K.A., Ross E.L., Clayman M.L., Bergeron A.R., Federman A.D., Bailey S.C. Measuring patients’ self-efficacy in understanding and using prescription medication. Patient Educ Couns. 2010;80(3):372–376. doi: 10.1016/j.pec.2010.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cássaro F.A., Pires L.F. Can we predict the occurrence of COVID-19 cases? Considerations using a simple model of growth. Sci Total Environ. 2020;728:138834. doi: 10.1016/j.scitotenv.2020.138834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2020). Retrieved from https://www.cdc.gov/healthywater/hygiene/etiquette/coughing_sneezing.html.
- Chan M., Woon I., Kankanhalli A. Perceptions of information security in the workplace: linking information security climate to compliant behavior. J Inf Privacy Secur. 2005;1(3):18–41. doi: 10.1080/15536548.2005.10855772. [DOI] [Google Scholar]
- Chin J., Jiang B., Mufidah I., Persada S., Noer B. The Investigation of consumers’ behavior intention in using green skincare products: a pro-environmental behavior model approach. Sustainability. 2018;10(11):3922. doi: 10.3390/su10113922. [DOI] [Google Scholar]
- Coccia M. Factors determining the diffusion of COVID-19 and suggested strategy to prevent future accelerated viral infectivity similar to COVID. Sci Total Environ. 2020;729:138474. doi: 10.1016/j.scitotenv.2020.138474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conner K. 2020. Face Masks in Cars, Stores, Outside: Places You’re Expected to Wear a Covering.https://www.cnet.com/health/face-masks-in-cars-stores-outside-places-youre-expected-to-wear-a-covering/ Retrieved from. [Google Scholar]
- CSIS (2020). Retrieved from https://www.csis.org/programs/southeast-asia-program/southeast-asia-covid-19-tracker-0.
- D’Amours K. 2020. Stop the Spread of COVID-19 by Wearing Your Face Mask Properly.https://www.wwlp.com/news/health/coronavirus-local-impact/combat-covid-19-spread-by-wearing-your-face-mask-properly/ Retrieved from. [Google Scholar]
- Dariya B., Nagaraju G.P. Understanding novel COVID-19: its impact on organ failure and risk assessment for diabetic and cancer patients. Cytokine Growth Factor Rev. 2020 doi: 10.1016/j.cytogfr.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis T.C., Wolf M.S., Bass P.F., Thompson J.A., Tilson H.H., Neuberger M. Literacy and misunderstanding prescription drug labels. Ann Inter Med. 2006;145(12):887. doi: 10.7326/0003-4819-145-12-200612190-00144. [DOI] [PubMed] [Google Scholar]
- Díaz A., Soriano J.F., Beleña Á. Perceived vulnerability to disease questionnaire: factor structure, psychometric properties and gender differences. Pers Individ Differ. 2016;101:42–49. doi: 10.1016/j.paid.2016.05.036. [DOI] [Google Scholar]
- Duddu P. 2020. Coronavirus in Philippines: How the COVID-19 Affects Philippines.https://www.airport-technology.com/features/coronavirus-affected-countries-philippines-measures-impact-tourism-economy/ Retrieved from. [Google Scholar]
- Ellen P.S., Wiener J.L., Cobb-Walgren C. The role of perceived consumer effectiveness in motivating environmentally conscious behaviors. J Public Policy Mark. 1991;10(2):102–117. doi: 10.1177/074391569101000206. [DOI] [Google Scholar]
- Fan J., Liu X., Shao G., Qi J., Li Y., Pan W. The epidemiology of reverse transmission of COVID-19 in Gansu Province, China. Travel Med Infect Dis. 2020:101741. doi: 10.1016/j.tmaid.2020.101741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FAO . 2020. Maintaining a Healthy Diet During the COVID-19 Pandemic. Rome. [Google Scholar]
- Feng S., Shen C., Xia N., Song W., Fan M., Cowling B.J. Rational use of face masks in the COVID-19 pandemic. Lancet Respir Med. 2020;8(5):434–436. doi: 10.1016/s2213-2600(20)30134-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feuer W. 2020. Drinking Alcohol Can Make The Coronavirus Worse, The WHO Says In Recommending Restricting Access.https://www.cnbc.com/2020/04/15/drinking-alcohol-can-make-the-coronavirus-worse-the-who-says-in-recommending-restricting-access.html Retrieved from. [Google Scholar]
- Gabriel E.H., Hoch M.C., Cramer R.J. Health Belief Model Scale and Theory of Planned Behavior Scale to assess attitudes and perceptions of injury prevention program participation: an exploratory factor analysis. J Sci Med Sport. 2019;22(5):544–549. doi: 10.1016/j.jsams.2018.11.004. [DOI] [PubMed] [Google Scholar]
- Gefen D., Straub D., Boudreau M. Structural equation modeling and regression: guidelines for research practice. Commun Assoc Inf Syst. 2000:4. doi: 10.17705/1cais.00407. [DOI] [Google Scholar]
- Geggel L. 2020. Can Wearing A Face Mask Protect You From The New Coronavirus?https://www.livescience.com/face-mask-new-coronavirus.html Retrieved from. [Google Scholar]
- Gorbalenya The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nature Microbiol. 2020 doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorbalenya A.E., Baker S.C., Baric R.S. The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020:536–544. doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorlick A. 2020. The Productivity Pitfalls of Working From Home In The Age of COVID-19.https://news.stanford.edu/2020/03/30/productivity-pitfalls-working-home-age-covid-19/ Retrieved from. [Google Scholar]
- GOVPH . 2020. ECQ and GCQ Guidelines.http://www.covid19.gov.ph/ecq-gcq-guidelines/ Retrieved July 18, 2020, from. [Google Scholar]
- Grimes M., Marquardson J. Quality matters: evoking subjective norms and coping appraisals by system design to increase security intentions. Decis Support Syst. 2019;119:23–34. doi: 10.1016/j.dss.2019.02.010. [DOI] [Google Scholar]
- Grover S., Dua D., Sahoo S., Mehra A., Nehra R., Chakrabarti S. Why all COVID-19 hospitals should have mental health professionals: the importance of mental health in a worldwide crisis! Asian J Psychiatry. 2020:102147. doi: 10.1016/j.ajp.2020.102147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagger M.S., Chan D.K., Protogerou C., Chatzisarantis N.L. Using meta-analytic path analysis to test theoretical predictions in health behavior: an illustration based on meta-analyses of the theory of planned behavior. Preventive Med. 2016;89:154–161. doi: 10.1016/j.ypmed.2016.05.020. [DOI] [PubMed] [Google Scholar]
- Hair J.F. Pearson; Upper Saddle River: 2010. Multivariate Data Analysis: A Global Perspective. [Google Scholar]
- Herath T., Rao H.R. Protection motivation and deterrence: a framework for security policy compliance in organisations. Eur J Inf Syst. 2009;18(2):106–125. doi: 10.1057/ejis.2009.6. [DOI] [Google Scholar]
- Hill R.J., Fishbein M., Ajzen I. Belief, attitude, intention and behavior: an introduction to theory and research. Contemp Sociol. 1977;6(2):244. doi: 10.2307/2065853. [DOI] [Google Scholar]
- Hinkle S., Fox-Cardamone L., Haseleu J.A., Brown R., Irwin L.M. Grassroots political action as an intergroup phenomenon. J Social Issues. 1996;52(1):39e51. doi: 10.1111/j.1540-4560.1996.tb01360.x. [DOI] [Google Scholar]
- Ho S.M., Ocasio-Velázquez M., Booth C. Trust or consequences? Causal effects of perceived risk and subjective norms on cloud technology adoption. Comput Secur. 2017;70:581–595. doi: 10.1016/j.cose.2017.08.004. [DOI] [Google Scholar]
- Hu L., Bentler P.M. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equation Model: A Multidiscip J. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Huang X., Dai S., Xu H. Predicting tourists’ health risk preventative behaviour and travelling satisfaction in Tibet: combining the theory of planned behaviour and health belief model. Tour Manag Perspect. 2020;33:100589. doi: 10.1016/j.tmp.2019.100589. [DOI] [Google Scholar]
- Hung W.-S., Hu S.C., Hsu Y.-C., Chen K.-L., Chen K.-H., Yu M.-C. Factors affecting the use of anti-malaria preventive measures among Taiwan immigrants returning to malaria-endemic regions. Travel Med Infect Dis. 2014;12(4):370–377. doi: 10.1016/j.tmaid.2013.07.001. [DOI] [PubMed] [Google Scholar]
- Ilesanmi Olayinka, Alele Faith Osaretin. Knowledge, attitude and perception of ebola virus disease among secondary school students in Ondo State, Nigeria, october 2014. PLoS Curr. 2016 doi: 10.1371/currents.outbreaks.c04b88cd5cd03cccb99e125657eecd76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janmaimool P. Application of Protection Motivation Theory to investigate sustainable waste management behaviors. Sustainability. 2017;9(7):1079. doi: 10.3390/su9071079. [DOI] [Google Scholar]
- Johnson E.J., Hariharan S. Public health awareness: knowledge, attitude and behaviour of the general public on health risks during the H1N1 influenza pandemic. J Public Health. 2017;25(3):333–337. doi: 10.1007/s10389-017-0790-7. [DOI] [Google Scholar]
- Kam J.A., Matsunaga M., Hecht M.L., Ndiaye K. Extending the theory of planned behavior to predict alcohol, tobacco, and marijuana use among youth of mexican heritage. Prev Sci. 2008;10(1):41–53. doi: 10.1007/s11121-008-0110-0. [DOI] [PubMed] [Google Scholar]
- Khosravi M. Perceived risk of COVID-19 pandemic: the role of public worry and trust. Electron J Gen Med. 2020;17(4) doi: 10.29333/ejgm/7856. [DOI] [Google Scholar]
- Lau J.T., Griffiths S., Choi K.C., Tsui H.Y. Widespread public misconception in the early phase of the H1N1 influenza epidemic. J Infect. 2009;59(2):122–127. doi: 10.1016/j.jinf.2009.06.004. [DOI] [PubMed] [Google Scholar]
- Lau J.T., Yeung N.C., Choi K., Cheng M.Y., Tsui H., Griffiths S. Factors in association with acceptability of A/H1N1 vaccination during the influenza A/H1N1 pandemic phase in the Hong Kong general population. Vaccine. 2010;28(29):4632–4637. doi: 10.1016/j.vaccine.2010.04.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H., Park S.J., Lee G.R., Kim J.E., Lee J.H., Jung Y. The relationship between trends in COVID-19 prevalence and traffic levels in South Korea. Int J Infect Dis. 2020;96:399–407. doi: 10.1016/j.ijid.2020.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., Xu S., Yu M., Wang K., Tao Y., Zhou Y. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol. 2020 doi: 10.1016/j.jaci.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin S., Nadlifatin R., Amna A., Persada S., Razif M. Investigating Citizen behavior intention on mandatory and voluntary pro-environmental programs through a pro-environmental planned behavior model. Sustainability. 2017;9(7):1289. doi: 10.3390/su9071289. [DOI] [Google Scholar]
- Lin C., Prasetyo Y., Widyaningrum R. Eye movement parameters for performance evaluation in projection-based stereoscopic display. J Eye Mov Res. 2018;11(6) doi: 10.16910/jemr.11.6.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin C.J., Prasetyo Y.T., Siswanto N.D., Jiang B.C. Optimization of color design for military camouflage in CIELAB color space. Color Res Appl. 2019;44(3):367–380. doi: 10.1002/col.22352. [DOI] [Google Scholar]
- Lin C.J., Prasetyo Y.T., Widyaningrum R. Eye movement measures for predicting eye gaze accuracy and symptoms in 2D and 3D displays. Displays. 2019;60:1–8. doi: 10.1016/j.displa.2019.08.002. [DOI] [Google Scholar]
- Liu L. Emerging study on the transmission of the Novel Coronavirus (COVID-19) from urban perspective: evidence from China. Cities. 2020;103:102759. doi: 10.1016/j.cities.2020.102759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo Y., Yao L., Zhou L., Yuan F., Zhong X. Factors influencing health behaviours during the covid-19 outbreak in China: an extended IMB model. Public Health. 2020 doi: 10.1016/j.puhe.2020.06.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahardika H., Thomas D., Ewing M.T., Japutra A. Comparing the temporal stability of behavioural expectation and behavioural intention in the prediction of consumers pro-environmental behaviour. J Retail Consum Serv. 2020;54:101943. doi: 10.1016/j.jretconser.2019.101943. [DOI] [Google Scholar]
- Martinez J.E.F., Prasetyo Y.T., Robielos R.A.C., Panopio M.M., Urlanda A.A.C., Topacio-Manalaysay K.A.C. The Usability of Metropolitan Manila Development Authority (MMDA) mobile traffic navigator as perceived by users in Quezon City and Mandaluyong City, Philippines. Proceedings of the 2019 5th International Conference on Industrial and Business Engineering - ICIBE 2019. 2019 doi: 10.1145/3364335.3364391. [DOI] [Google Scholar]
- Matrajt L., Leung T. Evaluating the effectiveness of social distancing interventions to delay or flatten the epidemic curve of coronavirus disease. Emerging Infect Dis. 2020;26(8) doi: 10.3201/eid2608.201093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcmillan B., Conner M. Using the theory of planned behaviour to understand alcohol and tobacco use in students. Psychol Health Med. 2003;8(3):317–328. doi: 10.1080/1354850031000135759. [DOI] [Google Scholar]
- Medalie L. 2020. Why Sleep Is So Important During The Coronavirus Outbreak.https://www.uchicagomedicine.org/forefront/coronavirus-disease-covid-19/advice-for-sleeping-well-during-the-covid-19-outbreak Retrieved from. [Google Scholar]
- Mi Y.-n., Huang T.-t., Zhang J.-x., Qin Q., Gong Y.-x., Liu S.-y. Estimating instant case fatality rate of COVID-19 in China. Int J Infect Dis. 2020 doi: 10.1016/j.ijid.2020.04.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miraja B.A., Persada S.F., Prasetyo Y.T., Belgiawan P.F., Redi A.P. Applying Protection Motivation Theory to understand generation z students intention to comply with educational software anti piracy law. Int J Emerging Technol Learn (iJET) 2019;14(18):39. doi: 10.3991/ijet.v14i18.10973. [DOI] [Google Scholar]
- Mishra P., Bhadauria U.S., Dasar P.L., Kumar S., Lalani A., Sarkar P. Knowledge, attitude and anxiety towards pandemic flu a potential bio weapon among health professionals in Indore City. Przegl Epidemiol. 2016;70 41-5, 125. [PubMed] [Google Scholar]
- Myyry L., Siponen M., Pahnila S., Vartiainen T., Vance A. What levels of moral reasoning and values explain adherence to information security rules? An empirical study. Eur J Inf Syst. 2009;18(2):126–139. doi: 10.1057/ejis.2009.10. [DOI] [Google Scholar]
- Nadlifatin R., Lin S., Rachmaniati Y., Persada S., Razif M. A pro-environmental reasoned action model for measuring citizens’ intentions regarding ecolabel product usage. Sustainability. 2016;8(11):1165. doi: 10.3390/su8111165. [DOI] [Google Scholar]
- 2020. New Zealand Government.https://covid19.govt.nz/covid-19/how-were-uniting/wash-your-hands/?fbclid=IwAR0yhEkNrjR29H9LCHcPViSAHzHRWXk0EjKhnXloPudBg0k-37I0f-imgPQ Retrieved from. [Google Scholar]
- Ng B.-Y., Kankanhalli A., Xu Y.C. Studying users computer security behavior: a health belief perspective. Decis Support Syst. 2009;46(4):815–825. doi: 10.1016/j.dss.2008.11.010. [DOI] [Google Scholar]
- Nicola M., Oneill N., Sohrabi C., Khan M., Agha M., Agha R. Evidence based management guideline for the COVID-19 pandemic-Review article. Int J Surg. 2020;77:206–216. doi: 10.1016/j.ijsu.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens S. ‘Engaging the public’: information and deliberation in environmental policy. Environ Plann A: Economy Space. 2000;32(7):1141–1148. doi: 10.1068/a3330. [DOI] [Google Scholar]
- Oyeniran O.I., Chia T. Novel Coronavirus disease 2019 (COVID-19) outbreak in Nigeria: how effective are government interventions? Ethics Med Public Health. 2020:100515. doi: 10.1016/j.jemep.2020.100515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pahnila S., Siponen M., Mahmood A. Employees behavior towards IS security policy compliance. 2007 40th Annual Hawaii International Conference on System Sciences (HICSS07) 2007 doi: 10.1109/hicss.2007.206. [DOI] [Google Scholar]
- Paital B., Das K., Parida S.K. Inter nation social lockdown versus medical care against COVID-19, a mild environmental insight with special reference to India. Sci Total Environ. 2020:138914. doi: 10.1016/j.scitotenv.2020.138914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perlman S. Another decade, another coronavirus. N Engl J Med. 2020 doi: 10.1056/nejme2001126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pradhan D., Biswasroy P., Naik P.K., Ghosh G., Rath G. A review of current interventions for COVID-19 prevention. Arch Med Res. 2020 doi: 10.1016/j.arcmed.2020.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prokop P., Kubiatko M. Perceived vulnerability to disease predicts environmental attitudes. EURASIA J Math Sci Technol Educ. 2014;10(1) doi: 10.12973/eurasia.2014.1017a. [DOI] [Google Scholar]
- 2020. Public Health of England.https://www.gov.uk/government/publications/guidance-to-employers-and-businesses-about-covid-19/guidance-for-employers-and-businesses-on-coronavirus-covid-19?fbclid=IwAR3TWkbEiw8kGHpduJ6B8TFRRKFN2IZ7l2yni7R5S5qHNglwHeOYdavnWdY Retrieved from. [Google Scholar]
- Ranada P. 2020. Metro Manila, Cebu City, Laguna Under ‘Modified’ ECQ Until May 31.https://rappler.com/nation/metro-manila-cebu-city-laguna-to-remain-under-modified-ecq Retrieved July 18, 2020, from. [Google Scholar]
- Reuben R.C., Danladi M.M., Saleh D.A., Ejembi P.E. Knowledge, attitudes and practices towards COVID-19: an epidemiological survey in North-Central Nigeria. J Community Health. 2020 doi: 10.1007/s10900-020-00881-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy D., Tripathy S., Kar S.K., Sharma N., Verma S.K., Kaushal V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J Psychiatry. 2020;51:102083. doi: 10.1016/j.ajp.2020.102083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubio-Romero J.C., Pardo-Ferreira M.D., García J.A., Calero-Castro S. Disposable masks: disinfection and sterilization for reuse, and non-certified manufacturing, in the face of shortages during the COVID-19 pandemic. Saf Sci. 2020:104830. doi: 10.1016/j.ssci.2020.104830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rula H. 2020. Keeping Your Immune System Healthy During the Coronavirus Pandemic.https://www.ironwoodcrc.com/keeping-your-immune-system-healthy-during-the-coronavirus-pandemic/ Retrieved from. [Google Scholar]
- Sarkodie S.A., Owusu P.A. Investigating the cases of novel coronavirus disease (COVID-19) in China using dynamic statistical techniques. SSRN Electron J. 2020 doi: 10.2139/ssrn.3559456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sasikumar R. 2020. Coronavirus Pandemic: An Early Lockdown Is Not Always the Best Strategy.https://science.thewire.in/the-sciences/coronavirus-lockdown-herd-immunity-economic-human-costs/ Retrieved from. [Google Scholar]
- Sasse, M., Brostoff, S., Weirich, D. Transforming the Weakest Link-a Human-Computer Interaction Approach to Usable and Effective security. Internet and Wireless Security, (n.d.) 243–262. doi: 10.1049/pbbt004e_ch15. [DOI]
- Sato Ana. What is the importance of vaccine hesitancy in the drop of vaccination coverage in Brazil? Revista saude publica. 2018;52:96. doi: 10.11606/S1518-8787.2018052001199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schepers J., Wetzels M. A meta-analysis of the technology acceptance model: investigating subjective norm and moderation effects. Inf Manage. 2007;44(1):90–103. doi: 10.1016/j.im.2006.10.007. [DOI] [Google Scholar]
- Seale H., Heywood A.E., Leask J., Steel M., Thomas S., Durrheim D.N. COVID-19 is rapidly changing: examining public perceptions and behaviors in response to this evolving pandemic. PLoS One. 2020 doi: 10.1101/2020.05.04.20091298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sen-Crowe B., Mckenney M., Elkbuli A. Social distancing during the COVID-19 pandemic: staying home save lives. Am J Emergency Med. 2020 doi: 10.1016/j.ajem.2020.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shader R.I. COVID-19 and depression. Clin Ther. 2020 doi: 10.1016/j.clinthera.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw R., Kim Y.-K., Hua J. Governance, technology and citizen behavior in pandemic: lessons from COVID-19 in East Asia. Prog Disaster Sci. 2020;6:100090. doi: 10.1016/j.pdisas.2020.100090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen Kaining, Yang Yonghong, Wang Tianyou, Zhao Dongchi, Jiang Y.i., Zheng Yuejie. Diagnosis, treatment, and prevention of 2019 novel coronavirus infection in children: experts’ consensus statement. World J Pediatr. 2020 doi: 10.1007/s12519-020-00343-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shim E., Tariq A., Choi W., Lee Y., Chowell G. Transmission potential of COVID-19 in South Korea. Int J Infect Dis. 2020 doi: 10.1101/2020.02.27.20028829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steiger J.H. Understanding the limitations of global fit assessment in structural equation modeling. Pers Individ Differ. 2007;42(5):893–898. doi: 10.1016/j.paid.2006.09.017. [DOI] [Google Scholar]
- Taghizadeh-Hesary F., Akbari H. The powerful immune system against powerful COVID-19: a hypothesis. Med Hypotheses. 2020 doi: 10.20944/preprints202004.0101.v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanoue Y., Nomura S., Yoneoka D., Kawashima T., Eguchi A., Shi S. Mental health of family, friends, and co-workers of COVID-19 patients in Japan. Psychiatry Res. 2020:113067. doi: 10.1016/j.psychres.2020.113067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torres M.E.S., Prasetyo Y.T., Robielos R.A.C., Domingo C.V.Y., Morada M.C. The effect of nutrition labelling on purchasing decisions. Proceedings of the 2019 5th International Conference on Industrial and Business Engineering - ICIBE 2019. 2019 doi: 10.1145/3364335.3364374. [DOI] [Google Scholar]
- UNICEF. (2020). Retrieved from https://www.unicef.org/coronavirus/everything-you-need-know-about-washing-your-hands-protect-against-coronavirus-covid-19.
- University of Michigan School of Public Health. (2020) Retrieved from https://sph.umich.edu/news/2020posts/mass-cancellations-slowing-the-spread-and-flattening-the-curve.html.
- USA Food & Drug Administration (2020). Retrieved from https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-continues-ensure-availability-alcohol-based-hand-sanitizer-during.
- Veldhuijzen Judy, Kenemans J.L., Bruin C.M., Olivier B., Volkerts Edmund. Pain and attention: attentional disruption or distraction? J Pain. 2006 doi: 10.1016/j.jpain.2005.06.003. [DOI] [PubMed] [Google Scholar]
- Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi: 10.1016/s0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2020. Advice For Public.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public Retrieved from. [Google Scholar]
- WHO . 2020. Advice For Public.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public Retrieved from. [Google Scholar]
- Workman M., Bommer W.H., Straub D. Security lapses and the omission of information security measures: a threat control model and empirical test. Comput Hum Behav. 2008;24(6):2799–2816. doi: 10.1016/j.chb.2008.04.005. [DOI] [Google Scholar]
- World Health Organization (2020). Retrieved from https://covid19.who.int/.
- World Health Organization . World Health Organization; 2020. Updated WHO Recommendations For International Traffic In Relation To COVID-19 Outbreak.https://www.who.int/news-room/articles-detail/updated-who-recommendations-for-international-traffic-in-relation-to-covid-19-outbreak [Google Scholar]
- Wu Z., Mcgoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China. JAMA. 2020;323(13):1239. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- Yancey-Bragg N., Bravo V. 2020. Can I Still Go For A Walk, Run Under Stay At Home Orders? Should I Wear A Mask?https://www.usatoday.com/in-depth/news/health/2020/04/15/coronavirus-masks-how-safely-go-outside-during-stay-home-order/2970072001/ Retrieved from. [Google Scholar]
- Zhou P., Yang X.-L., Wang X.-G., Hu B., Zhang L., Zhang W. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020 doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Perlman.S., Geleris J., Doremalen Nvan, Cao B., China Novel Coronavirus Investigating and Research Team, & NHC Key Laboratory A novel coronavirus from patients with pneumonia in China, 2019. NEJM. 2020;(February) https://www.nejm.org/doi/full/10.1056/NEJMoa2001017 Retrieved from. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.