Abstract
The objective was to identify facilitators and challenges of implementing diabetes group visits in 5 Midwestern community health center (CHC) settings that care for diverse patient populations. Interview data were collected from July to August 2015. An interview guide was developed to explore health center teams' initial experiences with diabetes group visit implementation. Interviews were conducted with 14 individuals who participated in a training prior to diabetes group visit implementation. Four levels of coding (open, in vivo, categorical, and thematic) were used to identify characteristics of group visit implementation in 5 CHCs. A semi-structured model encouraged interprofessional teamwork across all CHC teams. Self-appointed or chosen team champions were the “pulse” or central driving force of implementation. A designated time in the clinic for patients to receive education and psychosocial support enhanced engagement in diabetes self-management. Early buy-in from upper leadership was critical to securing fiscal and human resources as unexpected needs emerged during group visit implementation. Time commitment of clinic staff and providers for ongoing operations, socioeconomic challenges of patients, staff turnover, and billing were reported as challenges in the initial implementation process. This study acknowledges the influence of administrative and sociocultural factors on successful implementation of diabetes group visits. Future research should further explore how these factors influence successful adoption of diabetes group visits in health centers across the United States and the impact of group visit implementation on staff and patient outcomes.
Keywords: diabetes group visits, community health centers, organizational factors, perceived facilitators and barriers, exploratory case study, formative evaluation research
Introduction
Type 2 diabetes is a common chronic condition that requires multidisciplinary care to meet patients' needs.1,2 Beyond attendance at medical appointments, health care providers recommend patients routinely monitor blood glucose levels, maintain a healthy weight, adopt a healthy diet, engage in physical activity, and take prescribed medications.3,4 Vulnerable populations, such as racial and ethnic minorities and individuals with socioeconomic challenges, are disproportionately affected by type 2 diabetes.5 Community health centers (CHCs) play an important role in providing medical care for these vulnerable individuals, as they often serve a high proportion of medically underserved populations. For patients ages 18–64 years, health care providers working in CHCs diagnose type 2 diabetes in a greater proportion of visits when compared to diagnoses made in physician offices (5.7% vs. 1.6%).6 In addition, CHC patients are burdened with socioeconomic realities that affect their ability to learn and maintain lifestyle practices for successful diabetes self-management. More than 70% of CHC patients have incomes below 100% of the federal poverty level and 57% are people of color.7,8
Coordinated diabetes care offering educational and psychosocial support is an area in which to address gaps in services for vulnerable populations. Diabetes group visits provide a shared space for ongoing patient–provider communication about self-management practices and present opportunities to improve clinical outcomes.9 Group visits are shared patient appointments that include diabetes education in a group setting and individual visits with a primary care provider.10–12 Diabetes group visits vary in structure and participation. Group size can range from 8–20 patients with visits lasting 60–120 minutes.13 In hospital primary care offices, the most objective benefit of diabetes group visits for type 2 diabetes patients is improvement in glycated hemoglobin.14,15 Patients also report improved quality of life15 and cardiovascular benefits (ie, controlled blood pressure, increased aerobic activity) following group visits as well as reduction in their medical costs.16,17
Given the complexity of the disease and the need for multidisciplinary care, group visits are an opportunity to streamline delivery of diabetes care while providing social support and connections. Organizational benefits of diabetes group visits have been documented in hospital primary care offices.18 Facilitators and barriers to early implementation of diabetes group visits in CHCs have not been researched. Hospital primary care and CHCs operate very differently. CHCs have unique challenges related to logistics and patient care. Access to specialty care for CHC patients is often limited.19 In addition, staff turnover can be high and work environments can be stressful because of insufficient resources, high workload, and time pressure.20,21
The purpose of this multisite case study was to identify organizational facilitators and barriers to diabetes group visit implementation for 5 teams from Midwestern CHCs. Focusing on first-time implementation of these diabetes group visits can provide opportunities to understand current infrastructure and resource needs of CHCs that serve medically underserved populations.
Methods
Study participants
Interview data were used to explore lessons learned from health professionals' first-time implementation of diabetes group visits in their respective CHCs. Data included 14 transcripts from individuals reflecting on their experiences 3 months following their completion of a university- and health center network-led diabetes group visit training. These individuals (Table 1) were members of teams from 5 CHCs that were located in Ohio, Nebraska, Michigan, Indiana, and Illinois. All individuals represented CHCs that did not have diabetes group visits and who learned at the training to recruit patients, prepare for group visit sessions, conduct sessions, and evaluate the program.
Table 1.
Group Visit Team Member Characteristics and Experiences with Patient Care and Group Visits (N = 26)
| Characteristic | N(%) or Mean (SD) |
|---|---|
| Age (Mean ± SD) | 44.0 ± 8.5 |
| Female, N (%) | 22 (85%) |
| Race/Ethnicity, N (%) | |
| Non-Hispanic White | 22 (84.6%) |
| Non-Hispanic Black or African American | 2 (7.7%) |
| Non-Hispanic Asian | 1 (3.8%) |
| Hispanic, Latino, or Spanish origin | 1 (3.8%) |
| Current positions at health centers, N (%) | |
| Registered Nurse | 8 (30.8%) |
| Physician | 4 (15.4%) |
| Administrator | 3 (11.5%) |
| Dietitian | 2 (7.7%) |
| Licensed Practical Nurse | 2 (7.7%) |
| Nurse Practitioner/Advanced Practice Nurse | 2 (7.7%) |
| Physician Assistant | 2 (7.7%) |
| Health Educator | 1 (3.8%) |
| Medical Assistant | 1 (3.8%) |
| Social Worker | 1 (3.8%) |
| Years practicing since completing training (Mean ± SD) | 11.9 ± 10.0 |
| Years working at current health center (Mean ± SD) | 6.6 ± 6.4 |
| Percentage with prior training in lifestyle coaching or motivational interviewing techniques, N (%) | 20 (76.9%) |
| Percentage with prior experience conducting group visits, N (%) | 3 (11.5%) |
| Health conditions covered in prior group visits, N (%) | Diabetes, 1 (3.8%) |
| Obesity/Overweight, 1 (3.8%) | |
| Health Literacy, 1 (3.8%) | |
SD, standard deviation.
Development of interview guide
An interview guide was developed by the research team to explore CHC teams' initial experiences with diabetes group visit implementation. Interview questions were based on a literature review focused on chronic disease group visits/shared medical appointments. In addition, 5 domains (intervention characteristics, outer setting, inner setting, characteristics of individuals, and process) of the Consolidated Framework for Implementation Research (CFIR) served as a reference for organizing the interview guide.22 CFIR provides health services researchers a conceptual “lens” through which to examine facilitators and barriers to adoption of new interventions in clinical settings.23 Once the guide was developed, CHC practitioners serving as consultants to the research team provided feedback on the relevancy and clarity of each question. The study protocol was approved by the University of Chicago Institutional Review Board.
Data collection
Trained research staff conducted 1-hour telephone interviews. Fourteen of the 26 individuals trained in the diabetes group visit model participated in the interviews. All interviews were audio recorded and transcribed by the research team. Names of CHCs were removed and each was assigned a number to maintain anonymity of participants without losing the meaning and context of diabetes group visit settings.
Data analysis
All transcripts were entered into Dedoose (SocioCultural Research Consultants, LLC, Manhatten Beach, CA).24 An inductive approach, using 4 levels of coding,25 was used to identify characteristics that promote the implementation of training concepts into the organizational culture of the CHCs. One research team member reviewed and coded all transcripts at the sentence and paragraph levels. In the first phase, open coding was used to segment and organize data into single words or phrases describing group visit implementation in the CHC setting. The second phase involved in vivo coding of words used directly by the respondent to draw additional context and meaning about the respondent's experience with administering and delivering content from the group visit training. In the third phase, categorical coding was used to identify key facilitators and barriers to implementation within and across Midwestern CHCs. In the fourth phase, themes were extrapolated within the context of facilitators and barriers related to diabetes group visit implementation.
At each phase, 3 members of the research team verbally summarized their codes. Unclear codes and concepts were discussed until agreement (<80%) was reached. Through collaborative analysis of the transcripts, the team determined that the interview responses made evident participant roles in implementation, which led the researcher to categorize comments by role - either team leader (champion) or team member. The research team analyzed categories and emerging themes and their connection to all teams and individuals participating, attempting to differentiate if their experiences were common across all CHCs or unique to a particular team.
Results
Analysis of transcripts revealed 4 perceived facilitators and 4 perceived barriers to the implementation of diabetes group visits (Table 2).
Table 2.
Perceived Facilitators and Barriers to Diabetes Group Visit Implementation in Five Midwestern Health Centers
| Health center teams |
||||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | ||
| Perceived Facilitators | 1. A structured, yet flexible group visit model prompts interprofessional teamwork. | x | x | x | x | x |
| 2. Champions were the “pulse” or central driving force of implementation. | x | x | x | x | ||
| 3. Time was allocated for providers, staff, and patients to cultivate positive interpersonal connections and discuss matters related to type 2 diabetes. | x | x | x | |||
| 4. As needs emerged during the implementation process, financial and staff support were provided by administrators. | x | x | x | |||
| Perceived Barriers | 1. Beyond initial planning, it was difficult to designate more time to address patient needs and ongoing operation of diabetes group visits. | x | x | x | x | x |
| 2. Socioeconomic challenges of patients influenced group visit participation. | x | x | x | x | ||
| 3. Staff turnover of core members influenced a team's ability to adapt to organizational change. | x | x | ||||
| 4. Community health centers encountered difficulties billing for diabetes group visits. | x | x | ||||
Facilitator #1: a structured, yet flexible group visit model prompts interprofessional teamwork
A semi-structured model was a major facilitator that enabled all CHC teams to further build the internal capacity needed to engage clinical staff and health care providers in group visit implementation. All practitioners noted that the training materials were helpful in easy start-up and integration in their clinic. Several participants credited the university and the CHC network for providing a proposed model for implementation and educational materials for teams to discuss and consider for use. As stated by one team member:
I was really expecting to get some guidance on how to go about setting up a group visit and kind of what it entailed, like the meat of it, and just really an idea kind of what to expect with doing the visit. They gave us a real lot of ideas for how to kind of tweak things and make it work at our center.
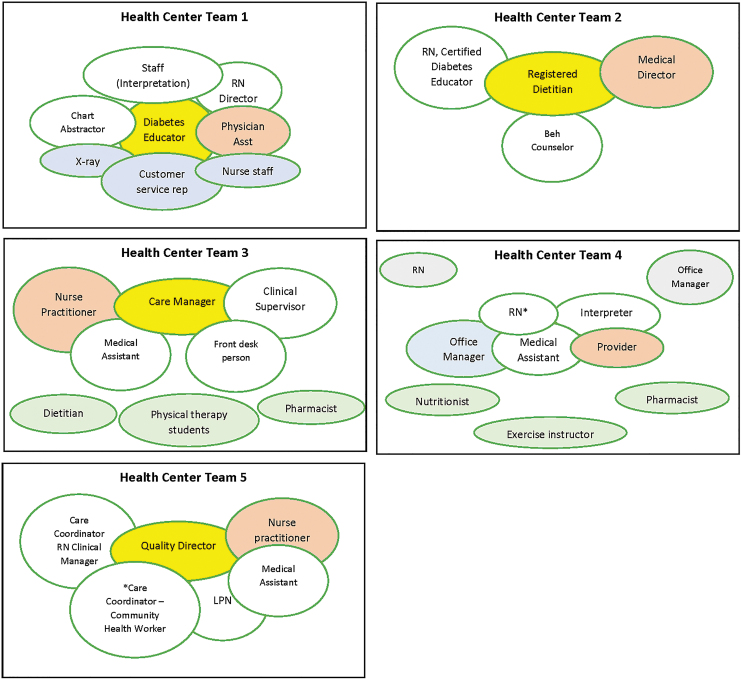
Staff engagement was best captured through the varying composition of CHC teams (Figure 1). All teams were able to maintain a health care provider as a core team member who conducted individual visits with patients. Three CHC teams had nurse practitioners, 2 teams had physicians, and 1 team had a physician assistant. All of the teams also had other clinical staff (eg, nurse, dietitian) involved as team members, ancillary/support staff, or guest speakers to support implementation.
FIG. 1.
Community health center team composition of diabetes group visits (n = 5).
 = group champion/team leader
= group champion/team leader
 = team members (identified before training or attended training)
= team members (identified before training or attended training)
 = guest speakers
= guest speakers
 = team members (recruited after training)
= team members (recruited after training)
 = health care provider
= health care provider
NOTE: One health center did not implement diabetes group visits after participating in the training. Beh, behavioral; LPN, licensed practical nurse; RN, registered nurse.
Three of the 5 teams exceeded the expected number of staff and comprised 5–6 core members. Roles varied by profession and across all teams. For example, a certified diabetes educator (Health Centers 1 and 3) played a major role in delivering education at all the group session. On the other hand, a nutritionist or dietitian served as a peripheral team member (Health Centers 3 and 4) and functioned more as a specialty provider or guest speaker at 1–2 sessions. Common team roles were: patient registration, checking vital signs, diabetes education, and provider one-on-one appointments. Between group visits, teams cooperated on issues such as patient recruitment, program retention, interpreter services, and transportation barriers. Issues were addressed by one team member or as a collective unit.
Although implementing group visits was reported as being quite daunting, all CHC teams stated that it was worthwhile. In fact, their enthusiasm and excitement fueled their efforts. One participant stated, “Everything has been challenging, but it's been a lot of fun too.” Teamwork allowed centers to provide a beneficial service to their patients:
Working with other people who are committed and getting excited about using different learning techniques to encourage the participants to succeed, that has been really fun. I mean this team is pretty awesome, but we all share the same mission and vision and we're going to make it happen and we're going to find a way to do it. The group is very excited. They like watching these people learn and we get really excited after a group visit because we really feel like we've helped these people. There is a kind of an excitement among the group.
Group visits required everyone to share the same vision. Teamwork required different parts of the clinic (from front line to upper management) to contribute at different stages of planning, implementation, and evaluation. As stated by one participant, “we…worked as a team to kind of tweak things and kind of figure things out for everyone.”
Facilitator #2: champions were the “pulse” or central driving force of implementation
Across all CHC teams, the champion was essential to initiating and implementing diabetes group visits. The role of champion was a self-appointed or volunteer leadership role on the team and was not based on position or title of the professional. As illustrated in Figure 1, champions' positions were: a diabetes educator, a dietitian, a care manager, a nurse, and a quality director. Champions self-disclosed or were lauded by their team members for being highly engaged and responsible for facilitating activities related to group visits. One team member described the role of their champion, the diabetes educator, as the lead organizer and the “brains of the operation” for core team members:
Our diabetes educator obviously has been our team lead and my role most of the time has been either brainstorming new directions to go and facilitating the use of other staff members…our diabetes educator in particular, so really just to see him flourish and this program flourish and being successful means that the clinic is being successful as well.
The champion from the same CHC confirmed his active role in moving the team forward with planning activities associated with diabetes group visits:
I am kind of like the project lead and I have been making sure that like we pull everybody together, especially at the beginning we were having meetings about once a week to try to get everything set up…
Group champions underscored the importance of communicating with upper management and clinic staff. Additionally, champions handled administrative aspects of group visits, which included securing meeting locations, distributing meeting reminders, inviting guest speakers, conducting process evaluation of sessions, and creating the agendas.
Facilitator #3: time was allocated for providers, staff, and patients to cultivate positive interpersonal connections and discuss matters related to type 2 diabetes
To the majority of CHC teams, diabetes group visits represented a designated time in the clinic to support patients beyond routine visits. Patient engagement was an initial outcome cited by several team members. Although all teams did not reach the expected number of participants (n = 15), they were pleased with patient engagement as a short-term result. At the time of the interview it was too soon to tell whether elevated blood sugar levels were mitigated through additional education and support provided through group visits. Three of the 5 CHCs reported that interactions occurring among patients in education sessions and with medical providers during one-on-one appointments met their expectations. Team members perceived that patients felt supported and expressed their gratitude to staff for caring about their overall well-being. Overall, diabetes group visits allowed patients to view the clinic from a positive perspective:
[Group visits] have been really a good thing and it is very exciting because the patients are very engaged. They participate, they come back, it has been a real positive thing.
Several participants expressed the benefits of diabetes group visits in affording patients more “aha” moments so they understood the importance of their role in diabetes self-management outside their doctor visits. Seeking mutual benefit was important even if it was not possible to obtain at all times:
…the patient is engaged in their disease process and when they are engaged actively in their disease process they tend to work harder, not in the office but at home on solving issues pertaining to diabetes…the benefit is being able to build rapport with your patients, have that long-term commitment, not only medically but just personally with them where they want to do better.
The small group structure was credited with enhancing opportunities for patients to connect with each other. This dynamic created a sense of camaraderie and gave patients a sense of community. One team member's personal expectation was for the group visits to serve as an extended support group:
I like the way they talk amongst themselves like before we start meeting and even afterwards. They like to ask each other questions and they seem to enjoy each other and they want to know what is going on with each other. We have had several different big things come up health-wise for some of the patients and everybody is kind of taking an interest in everybody else. It is the camaraderie theme, some people are in the same shoes and some people you know have it a whole lot worse.
Facilitator #4: as needs emerged in the implementation process, financial and staff support were provided by administrators
Minimizing resistance to group visit implementation was perceived as a form of organizational support. As stated by a team member: “We are fully supported by our leaders, so what we need we can get. They are going to find a way to make it happen.” CHC leadership also were part of the team, but engaged in the process very differently from the champion and team members. Although they were not typically involved in the daily and weekly planning and execution of activities, they were seen as working “behind the scenes” – similar to a producer providing financial resources to support a production. Leadership engagement often required champions to actively keep them updated on every phase of group implementation. Some CHCs provided examples of tangible support provided by leadership. Examples included: funding to purchase patient incentives for self-management/care (eg, pedometers, foot mirrors) and food/healthy snacks at group visits. A team member who was responsible for education in group visits provided an example of the “behind the scenes” engagement from the leadership in their CHC:
I think they support us but they definitely have a behind-the-scenes type of feel. We don't have much of a budget for this but when we came back from [city's name] the second time, we asked leadership for more of a budget and they were very receptive…they've allowed us to purchase some pedometers and some mirrors for people to do diabetes foot checks and to make certificates, so that was kind of nice to see that they do support us even though they're not actively engaged on a day-to-day basis.
Because of the visible support provided by leadership, teams were empowered to communicate the types of resources required for meeting the needs of their population.
Barrier #1: beyond initial planning, it was difficult to designate more time to address patient needs and ongoing operation of diabetes group visits
Time commitment involved in initiating and implementing diabetes group visits was noted as a concern. Three of the 5 teams shared the challenges of time from 2 perspectives. From one perspective, team members noted that patients had multiple questions for the provider and not enough time was allotted to address them. One team member described, “get[ting] each patient in and out with the physician fairly quickly because some of them, I think, are talkers and they want to spend more time with the physician than maybe a group visit would allow.” From another perspective, time for setup, planning, and follow-through was time consuming. Staff were unable to fully dedicate their time to diabetes group visits only. A part-time or full-time person was needed to address these issues:
…challenges have been just the time, it really almost feels like you need this to be a part-time job for someone and all of us that are participating in this group visit have one or two full-time jobs that we are already doing so it is really challenging to fit it into our workflow.
Overcommitment of staff impacted the successful implementation. Diabetes group visit implementation not only included delivering education sessions and seeing patients in one-on-one appointments, but also extended into the daily operations of the clinic that involved registration/check-in for appointments, billing, chart entry, and data abstraction from charts. Some CHC teams discovered that, if not executed in a timely manner, these additional responsibilities impacted implementation:
…sometimes we overcommit, especially with me being the project lead on this, and I have a lot of commitments elsewhere that made it very challenging trying to keep everybody together, and all of the staff has their specific jobs that they are doing, so just trying to find time where we can pull everybody together…
A note of caution was underscored by 4 of the 5 teams for prospective CHCs considering diabetes group visits. Several team members stated the importance of observing existing diabetes group visits so that CHCs are informed about the time commitment involved with implementation.
Barrier #2: socioeconomic challenges of patients influenced group visit participation
Socioeconomic challenges were cited as barriers to diabetes group visits. Two of the CHC teams dealt with transportation barriers that impacted patients' participation and ongoing attendance. Even when transportation was provided, attendance was affected:
We're dealing with the poorer population who doesn't have transportation even though we let them know we would provide, you know, a way for them to get here…
Also related to challenging sociodemographic barriers were the difficulties of patient recruitment: One team member reported:
…it was very discouraging. I think cold calling our patients is difficult. They are transient in nature, they move around a lot, they switch phone numbers, addresses. These are the challenges we deal with on a daily basis, let alone calling them and trying to get them to come in, so oftentimes people were excluded from being recruited simply because I can't get a hold of them. We've never had good success getting people to participate in groups and I kind of have a, now it's all subjective, but I do feel that there's kind of a culture here of strong, tough independents.
All teams noted diabetes is one of many things that vulnerable populations (eg, the poor, rural residents, the homeless, and the elderly) must contend with on a daily basis. Typically, diabetes self-management was not a priority, or it required the removal of personal housing, financial, or psychosocial challenges that influence whether or not attention to self-care was possible.
Barrier #3: staff turnover of core members influenced a team's ability to adapt to organizational change
A couple of teams encountered issues related to staff turnover, which possibly impacted patient recruitment and connectivity of diabetes group visits to the daily operations of the clinic. Although 6 teams participated in the training, one team experienced a change in leadership because of the resignation of the champion/team lead. This change influenced the team's ability to implement diabetes group visits. Another CHC team also experienced staff turnover with several members of their team because of changes in job responsibilities:
We had a couple of staff changes, so the office manager changed twice during the implementation. Then one of the nurses that was involved changed, so the new nurse who just started is not really a part of it because she is just learning how to do everything.
The ability of the team to adapt when a change in staff occurred was important to maintain program progress and continued implementation.
Barrier #4: CHCs encountered difficulties billing for diabetes group visits
Concern about financial reimbursement varied depending on a team's vision for implementation. Although diabetes group visits were in their infancy and primary focus was given to implementation, one team attempted to identify a financial mechanism to bill for the service. This CHC team noted that there were difficulties in covering provider time, especially when the number of patients attending visits fluctuated:
…the challenge is to just figure how to bill for this, you know, we have to get, to make this efficient or, you know, effective or worthwhile. I know, I hate to say it, but it is about money somewhat, you know, we have to see at least six people at a time at least so, yeah, that because one time I only saw three because I just figured oh, I'll just do it every other month, but we're realizing that that's really not going to be financially doable so, yeah, you have to do at least, see at least six patients…
Discussion
Although studies have demonstrated numerous positive outcomes for diabetes group visits, the experience of health professionals involved in the process of implementation has been understudied, especially in the CHC setting. This study found that a structured, yet flexible model that was easily adaptable to CHC settings prompted interprofessional teamwork and patient engagement. All teams had an “organizational champion” who was actively engaged in the process and was the “pulse” in coordinating logistics and content. Time commitment, socioeconomic challenges (ie, transportation, language) of patients, staff turnover, and billing challenges were noted as major barriers. Understanding these facilitators and barriers is critical to adoption of group visits within the CHC setting.
Engagement was crucial to initial success. In this study, teams were required to identify 3 to 4 core members responsible for executing 6 group sessions. The research team found that all teams maintained at least 3 core members. All teams were dedicated to increasing diabetes education and support and did not ignore the daily contextual challenges that patients face in successfully managing their diabetes. Similar results – that active engagement from staff prompts better adherence in meeting clinical standards – were noted in group visit studies.12,17,18,26 Furthermore, the designation of a team leader or “champion” was instrumental in the initial development and implementation of diabetes group visits. These individuals were either formally appointed by upper management or self-selected by colleagues to facilitate or manage the internal operation of these visits. Champions are individuals who dedicate themselves to supporting, marketing, “driving through,” and overcoming indifference or resistance that the intervention may provoke in an organization. In most cases, these individuals assume this position because it is an extension of their role in the clinic or because implementation of the intervention complements their professional training and expertise. Findings underscore that engagement is not just a step in the process. Thus, these findings suggest that structured, yet flexible diabetes group visit models that align with existing human resources within CHCs may prompt faster adoption. Furthermore, CHCs are ideally positioned to improve care coordination and collaboration by adopting a Patient-Centered Medical Home (PCMH)27 model. This model requires health care settings that promote interprofessional collaboration and patient-centered care. These ideals are vital to increasing staff's satisfaction and the patient's experience and are instrumental to establishing a strong foundation that supports group visit implementation.
This study also captures the perceived social and cultural challenges to diabetes group visits, particularly in recruiting and retaining CHC patients. Social conditions, such as transportation, housing, and insurance coverage, were cited by all CHC teams as major determinants of whether or not patients attended or returned to group visits. Most US CHCs serve patients who have incomes below 100% of the federal poverty level, are uninsured, or are Medicaid and Medicare recipients.8 Given the expenses associated with self-management, diabetes group visits may align better with a value-based payment model as opposed to a traditional fee-for-service model. A value-based model (especially as part of the PCMH model) emphasizes increased coordinated diabetes education and care for patients while rewarding the health care team for promoting overall population health. Thus, implementation of diabetes group visits in this setting must incorporate the social and financial resources that maximize patients' participation. Future studies can explore strategies employed by CHCs implementing diabetes group visits that are sensitive to patients' social and financial needs.
These findings have limited generalizability because of the small-scale nature of this study. The study, however, sets the stage for ongoing exploration of the adoption of diabetes group visit implementation models in CHCs. This is one of the first studies to explore the unique facilitators and challenges of diabetes group visits in CHCs. CHCs are important sources of primary care for underserved, minority, and low-income patients with chronic disease.28 Data from other demonstration projects note that insufficient resources, high workload, and high personnel turnover may influence CHCs in adopting new programs27,29; evaluating the early progression of the implementation process in the CHC setting can assist in identifying assets and deficiencies in adopting this organizational practice into health care systems. Diabetes group visits have the potential to enhance organizational infrastructure of diabetes education and care in CHCs. These visits create pathways for new leadership and interprofessional collaboration. This study found that several administrative and sociocultural factors influenced successful implementation. Considering the complexity of diabetes self-management and the elevated prevalence of diabetes within CHCs, continued examination of health system-related factors is needed. Future research should further examine how these factors influence successful adoption of diabetes group visits in CHCs in different regions of the United States. The impact of group visit implementation on staff outcomes, such as job satisfaction and morale as well as patient's perceptions of group visits, also should be evaluated.
Author Disclosure Statement
The authors declare that there are no conflicts of interest.
Funding Information
This research was supported by the Chicago Center for Diabetes Translation Research (National Institute of Diabetes and Digestive and Kidney Diseases [NIDDK] P30 DK092949). Dr. Baig was supported by a NIDDK Career Development Award (K23 DK087903-01A1).
References
- 1. Centers for Disease Control and Prevention. Team Care Approach for Diabetes Management. https://www.cdc.gov/diabetes/ndep/pdfs/ppod-guide-team-care-approach.pdf Accessed January26, 2019
- 2. National Institutes of Health. Redesigning the health care team: diabetes prevention and lifelong management. NIH publication no. 11-7739 NDEP-37. Bethesda, MD: National Diabetes Education Program, 2011 [Google Scholar]
- 3. Shrivastava SR, Shrivastava PS, Ramasamy J. Role of self-care in management of diabetes mellitus. J Diabetes Metab Disord 2013;12:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Schechter CB, Walker EA. Improving adherence to diabetes self-management recommendations. Diabetes Spectrum 2002;15:170–175 [Google Scholar]
- 5. Centers for Disease Control and Prevention. Addressing Health Disparities in Diabetes. https://www.cdc.gov/diabetes/disparities.html Accessed January26, 2019
- 6. Shi L, Lebrun LA, Tsai J, Zhu J. Characteristics of ambulatory care patients and services: a comparison of community health centers and physicians' offices. J Health Care Poor Underserved 2010;21:1169–1183 [DOI] [PubMed] [Google Scholar]
- 7. Shin P, Sharac J, Rosenbaum S. Community health centers and Medicaid at 50: an enduring relationship essential for health system transformation. Health Aff (Millwood) 2015;34:1096–104 [DOI] [PubMed] [Google Scholar]
- 8. Taylor J. The fundamentals of community health centers. 2004. https://hsrc.himmelfarb.gwu.edu/cgi/viewcontent.cgi?referer=https://scholar.google.com/&httpsredir=1&article=1136&context=sphhs_centers_nhpf Accessed January30, 2019
- 9. Ridge T. Shared medical appointments in diabetes care: a literature review. Diabetes Spectrum 2012;25:72–75 [Google Scholar]
- 10. Burke RE, O'Grady ET. Group visits hold great potential for improving diabetes care and outcomes, but best practices must be developed. Health Aff (Millwood) 2012;31:103–109 [DOI] [PubMed] [Google Scholar]
- 11. Davis A, Sawyer D, Vinci L. The potential of group visits in diabetes care. Clin Diabetes 2008;26:58–61 [Google Scholar]
- 12. Jaber R, Braksmajer A, Trilling J. Group visits for chronic illness care: models, benefits and challenges. Fam Pract Manag 2006;13:37–40 [PubMed] [Google Scholar]
- 13. Kirsh S, Watts S, Pascuzzi K, et al. . Shared medical appointments based on the chronic care model: a quality improvement project to address the challenges of patients with diabetes with high cardiovascular risk. Qual Safe Health Care 2007;16:349–353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Housden L, Wong ST, Dawes M. Effectiveness of group medical visits for improving diabetes care: a systematic review and meta-analysis. CMAJ 2013;185:E635–E644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Edelman D, Gierisch JM, McDuffie JR, Oddone E, Williams JW. Shared medical appointments for patients with diabetes mellitus: a systematic review. J Gen Intern Med 2015;30:99–106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Leung AK, Buckley K, Kurtz J. Sustainability of clinical benefits gained during a multidisciplinary diabetes shared medical appointment after patients return to usual care. Clin Diabetes 2018;36:226–231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Riley SB, Sorensen Marshall E. Group visits in diabetes care: a systematic review. Diabetes Edu 2010;36:936–944 [DOI] [PubMed] [Google Scholar]
- 18. McCuistion MH, Stults CD, Dohan D, Frosch DL, Hung DY, Tai-Seale M. Overcoming challenges to adoption of shared medical appointments. Popul Health Manag 2014;17:100–105 [DOI] [PubMed] [Google Scholar]
- 19. Cook NL, Hicks LS, O'Malley AJ, Keegan T, Guadagnoli E, Landon BE. Access to specialty care and medical services in community health centers. Health Aff (Millwood) 2007;26:1459–1468 [DOI] [PubMed] [Google Scholar]
- 20. Hayashi AS, Selia E, McDonnell K. Stress and provider retention in underserved communities. J Health Care Poor Underserved 2009;20:597–604 [DOI] [PubMed] [Google Scholar]
- 21. Lewis SE, Nocon RS, Tang H, et al. . Patient-centered medical home characteristics and staff morale in safety net clinics. Arch Intern Med 2012;172:23–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Consolidated Framework for Implementation Research. https://cfirguide.org Accessed January26, 2019
- 23. Breimaier HE, Heckemann B, Halfens RJ, Lohrmann C. The Consolidated Framework for Implementation Research (CFIR): a useful theoretical framework for guiding and evaluating a guideline implementation process in a hospital-based nursing practice. BMC Nurs 2015;14:43–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Dedoose. Dedoose Version 8.0.35, web application for managing, analyzing, and presenting qualitative and mixed method research data. Los Angeles: SocioCultural Research Consultants, LLC, 2018. [Google Scholar]
- 25. Saldan∼a J. The coding manual for qualitative researchers. Los Angeles: SAGE Publications; 2013 [Google Scholar]
- 26. Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA 2002;288:1775–1779 [DOI] [PubMed] [Google Scholar]
- 27. Quinn MT, Gunter KE, Nocon RS, et al. . Undergoing transformation to the patient centered medical home in safety net health centers: perspectives from the front lines. Ethn Dis 2013;23:356–362 [PMC free article] [PubMed] [Google Scholar]
- 28. Adashi EY, Geiger HJ, Fine MD. Health care reform and primary care—the growing importance of the community health center. N Engl J Med 2010;362:2047–2050 [DOI] [PubMed] [Google Scholar]
- 29. Chin MH, Cook S, Drum ML, et al. . Improving diabetes care in midwest community health centers with the health disparities collaborative. Diabetes Care 2004;27:2–8 [DOI] [PubMed] [Google Scholar]