Abstract
Background
Electronic health record (EHR)–based disease registries have aided health care professionals and researchers in increasing their understanding of chronic illnesses, including identifying patients with (or at risk of developing) conditions and tracking treatment progress and recovery. Despite excessive alcohol use being a major contributor to the global burden of disease and disability, no registries of alcohol problems exist. EHR-based data in Kaiser Permanente Northern California (KPNC), an integrated health system that conducts systematic alcohol screening, which provides specialty addiction medicine treatment internally and has a membership of over 4 million members that are highly representative of the US population with access to care, provide a unique opportunity to develop such a registry.
Objective
Our objectives were to describe the development and implementation of a protocol for assembling the KPNC Adult Alcohol Registry, which may be useful to other researchers and health systems, and to characterize the registry cohort descriptively, including underlying health conditions.
Methods
Inclusion criteria were adult members with unhealthy alcohol use (using National Institute on Alcohol Abuse and Alcoholism guidelines), an alcohol use disorder (AUD) diagnosis, or an alcohol-related health problem between June 1, 2013, and May 31, 2019. We extracted patients’ longitudinal, multidimensional EHR data from 1 year before their date of eligibility through May 31, 2019, and conducted descriptive analyses.
Results
We identified 723,604 adult patients who met the registry inclusion criteria at any time during the study period: 631,780 with unhealthy alcohol use, 143,690 with an AUD diagnosis, and 18,985 with an alcohol-related health problem. We identified 65,064 patients who met two or more criteria. Of the 4,973,195 adult patients with at least one encounter with the health system during the study period, the prevalence of unhealthy alcohol use was 13% (631,780/4,973,195), the prevalence of AUD diagnoses was 3% (143,690/4,973,195), and the prevalence of alcohol-related health problems was 0.4% (18,985/4,973,195). The registry cohort was 60% male (n=432,847) and 41% non-White (n=295,998) and had a median age of 41 years (IQR=27). About 48% (n=346,408) had a chronic medical condition, 18% (n=130,031) had a mental health condition, and 4% (n=30,429) had a drug use disorder diagnosis.
Conclusions
We demonstrated that EHR-based data collected during clinical care within an integrated health system could be leveraged to develop a registry of patients with alcohol problems that is flexible and can be easily updated. The registry’s comprehensive patient-level data over multiyear periods provides a strong foundation for robust research addressing critical public health questions related to the full course and spectrum of alcohol problems, including recovery, which would complement other methods used in alcohol research (eg, population-based surveys, clinical trials).
Keywords: electronic health records, alcohol, registry, unhealthy alcohol use, alcohol use disorder, recovery, secondary data
Introduction
Electronic health records (EHRs) provide a platform to study many diseases and health-related issues longitudinally in diverse populations, including identification of patients with (or at-risk of developing) conditions, and tracking treatment progress and recovery. The development of EHR-based disease registries has aided health care professionals and researchers in increasing their understanding of chronic illnesses and how to manage them [1]. For example, disease registries can facilitate the coordination of care within a health system [2,3]. However, they can also enable research on treatment effectiveness and patient outcomes, complementing other methods that are costly for repeated data collection in large populations (eg, clinical trials, surveys) [4].
Despite excessive alcohol use being a significant contributor to the global burden of disease and disability [5], to our knowledge, no population-, health system–, or EHR-based registries of individuals with alcohol problems exist. In 2016, excessive alcohol use accounted for 3 million deaths worldwide (5.3% of all deaths), which was higher than that of common conditions, such as diabetes (2.8%), road injuries (2.5%), tuberculosis (2.3%), and hypertension (1.6%) [5]. Alcohol-related death rates in the United States have also increased substantially over the past decade [6], accelerating over recent years [7]. Alcohol use is a known risk factor for serious medical conditions, including pancreatitis [8], stroke [9], and breast cancer [10], and can lead to alcohol use disorder (AUD) and alcoholic liver cirrhosis [11]. Alcohol can also impact the course of disease progression, management, and treatment outcomes for a range of conditions, including diabetes [12], depression [13,14], and anxiety [15]. While the prevalence of excessive alcohol use in the general US population ranges from 6% to 28% (depending on the definition and whether individuals with an AUD diagnosis are included) [16,17], there is evidence that it is increasing [17,18]. Therefore, alcohol problems are a significant public health concern that would benefit from being the primary focus of a disease registry.
The goal of the overall project was to assemble a registry of patients with alcohol problems by leveraging comprehensive EHR-based data within Kaiser Permanente Northern California (KPNC). The registry was developed for research specifically, but with the potential for future clinical or administrative applications such as quality improvement. KPNC is an integrated health care system that provides primary and specialty care internally (including addiction medicine and psychiatry). It has a mature, fully developed Epic EHR system (Epic Systems, Verona, WI), Kaiser Permanente (KP) HealthConnect, that stores data collected throughout the full course of patient care since 2005. Additionally, KPNC has conducted over 12 million alcohol screenings among 4 million adult members since June 2013 as part of a systematic alcohol screening, brief intervention, and referral to treatment initiative in primary care [19], which adds a robust patient-reported element to clinical data recorded in the EHR. Therefore, longitudinal, multidimensional patient-level data can be obtained (including alcohol use, health service utilization, diagnoses, medications, laboratory tests, and responses to health questionnaires), providing a unique opportunity to study the onset and progression of alcohol problems, care provided during all phases (ie, follow-up, management, continuity of care), and measurable outcomes such as changes in drinking. The objective of this paper was to describe the protocol used to develop the registry and to characterize patients who met eligibility criteria, including underlying health conditions. We include our methodological approach and considerations related to the registry, which we hope will be useful to other research teams and health systems with the ability to track unhealthy alcohol use, AUDs, and alcohol-related health problems (ie, conditions that are entirely attributable to alcohol).
Methods
Setting
KPNC serves 4.3 million members, comprising about one-third of the population in Northern California. The membership is diverse and highly representative of the US population with access to care [20]. Membership includes enrollees from Medicaid (12%), Medicare (16%), employer-based plans, and health insurance exchanges. KPNC members have direct access to specialty care clinics, including addiction medicine and psychiatry [21].
In June 2013, KPNC implemented Alcohol as a Vital Sign, a systematic alcohol screening, brief intervention, and referral to treatment initiative, in adult primary care [19]. While the initiative is primary care-based, the EHR screening tools are available for use in outpatient medical departments. KPNC has maintained an average 87% screening rate systemwide in adult primary care. As part of the screening, patients are asked three questions about their alcohol use, including a modified version of the evidence-based National Institute on Alcohol Abuse and Alcoholism (NIAAA) single-item screening question [16] (tailored to the patient’s age and sex)—“How many times in the past three months have you had 5 or more drinks containing alcohol in a day?” (for men aged 18-65 years), or “4 or more drinks” (for all women and for men aged ≥66 years)—and two questions that are used to calculate average drinks consumed per week—“On average, how many days per week do you have an alcoholic drink?” and “On a typical drinking day, how many drinks do you have?” The EHR issues a best practice alert during a primary care visit when screening is required (ie, first visit, annually, or every six months if unhealthy alcohol use was previously reported). The medical assistant may skip these questions for a variety of reasons (eg, late appointment arrivals, forgetting), and patients may decline to respond.
Data Sources
Registry data are leveraged from two existing data sources: Clarity (GridApp Systems, Inc) and the Virtual Data Warehouse (VDW). Clarity is the back-end database of EHR data collected in KP HealthConnect, which we used to extract alcohol screening data. The VDW is a distributed data model developed by the Health Care Systems Research Network (HCSRN) to maintain single extract, transform, and load processes that efficiently create relational tables useful for research [22]. The VDW gathers data from various EHR-based sources, including Clarity, and legacy systems that were used before the implementation of KP HealthConnect in 2005. The VDW data has been developed over many years with standardized data definitions and formats, and rigorous quality assurance.
Objective and Aims
In collaboration with NIAAA, we defined the objective of the registry and target population and formed research aims to frame the registry’s scope. The purpose of the registry is to study the full course of alcohol problems with the flexibility to address many research questions, such as the escalation of unhealthy drinking to development of AUDs and alcohol-related health problems, and the ability to be updated with new data. The target population for the registry is adult patients diagnosed with an alcohol problem and those at risk of developing one.
Protocol
We developed a protocol for building the registry (available upon request), following recommendations from the US Agency for Healthcare Research and Quality [4] and other disease registries [23,24], and received approval by the Institutional Review Board at KPNC. We benchmarked our approach to that of other disease registries at KPNC (eg, HIV [25], diabetes [26], cancer [27], opioid use [28]), to determine feasibility, data storage, and access. We surveyed the literature and involved KPNC physicians in psychiatry and addiction medicine to help select key data elements and clarify data definitions. We established a plan for leveraging available data by characterizing eligibility criteria for inclusion, defining the structure of the registry, and identifying core data elements and variables needed to address the research aims. We developed codebooks to define the scope of the registry (eg, diagnosis codebook of International Classification of Diseases, 9th Revision, Clinical Modification [ICD-9] and 10th Revision, Clinical Modification [ICD-10] codes), which can easily be updated to extend the breadth of data that the registry captures.
Inclusion Criteria
We included adult patients (age ≥18 years) with unhealthy alcohol use, an active AUD diagnosis, or an alcohol-related health problem, from any department or encounter setting within the health system. The initial registry cohort includes patients who met these criteria between June 1, 2013, (when Alcohol as a Vital Sign was implemented) to May 31, 2019. The patient’s index date was the first date in which the patient met eligibility criteria during the study period.
Unhealthy alcohol use was identified using systematic alcohol screening data collected as part of Alcohol as a Vital Sign. Using NIAAA recommended drinking guidelines [16], we defined unhealthy alcohol use as exceeding either the daily (≥5 drinks/day for men aged 18-65 years, or ≥4 drinks/day for women and for men aged ≥66 years) or weekly (>14 drinks/week for men aged 18-65 years, or >7 drinks/week for women and for men aged ≥66 years) drinking limit. To determine which risk threshold to use, we used the patient’s age and EHR-assigned sex, which is directly provided by the purchaser of a health insurance plan during enrollment. For patients with unknown sex (n=270), we used their sex assigned at birth (n=45), if available, which is a patient-reported variable collected along with gender identity in the EHR. Otherwise, we imputed sex based on the patient’s age and which single-item screening question was asked (n=225). If the patient was aged 18-65 years and asked, “How many times in the past three months have you had 5 or more drinks containing alcohol in a day?” sex was imputed as male (n=106), otherwise as female (n=119).
ICD-9 and ICD-10 codes given at any encounter at KPNC or through a claim were used to identify patients with a diagnosis of an active AUD (excluding remission codes) or an alcohol-related health problem (Table 1) [29].
Table 1.
International Classification of Diseases (ICD) codes for identification of active alcohol use disorders and alcohol-related health problems as part of inclusion criteria for the Kaiser Permanente Northern California Adult Alcohol Registry.
| Disorder, ICDa version, and code | Description | ||||
| Alcohol use disorders |
|
||||
|
|
ICD-9 | ||||
|
|
|
291b | Alcohol-induced mental disorders (eg, alcohol withdrawal delirium) | ||
|
|
|
303b, except 303.03 and 303.93c | Alcohol dependence syndrome | ||
|
|
|
305.0b, except 305.03c | Nondependent alcohol abuse | ||
|
|
ICD-10 | ||||
|
|
|
F10.9b | Alcohol use, unspecified (includes alcohol-induced mental disorders) | ||
|
|
|
F10.2b, except F10.21d | Alcohol dependence | ||
|
|
|
F10.1b, except F10.11d | Alcohol abuse | ||
| Alcohol-related health problems |
|
||||
|
|
ICD-9 | ||||
|
|
|
357.5 | Alcoholic polyneuropathy | ||
|
|
|
425.5 | Alcoholic cardiomyopathy | ||
|
|
|
535.3b | Alcoholic gastritis | ||
|
|
|
571.0-571.3 | Alcoholic liver disease | ||
|
|
ICD-10 | ||||
|
|
|
G31.2 | Degeneration of nervous system due to alcohol | ||
|
|
|
G62.1 | Alcoholic polyneuropathy | ||
|
|
|
G72.1 | Alcoholic myopathy | ||
|
|
|
I42.6 | Alcoholic cardiomyopathy | ||
|
|
|
K29.2b | Alcoholic gastritis | ||
|
|
|
K70b | Alcoholic liver disease | ||
|
|
|
K86.0 | Alcohol-induced chronic pancreatitis | ||
aICD: International Classification of Diseases.
bAny (or no) additional digits.
c303.03, 303.93, and 305.03 are ICD-9 remission codes.
dF10.21 and F10.11 are ICD-10 remission codes.
Structure and Data Elements
Like the VDW [22], the registry was designed as a distributed data model where each file contains one main content area, and files can be linked through key variables (eg, person ID, encounter ID; Figure 1). Main content areas include patient eligibility and demographics, alcohol screenings, membership and insurance, geocoded census data, diagnoses, procedures, outpatient pharmacy, prescription diagnoses, laboratory results, patient-reported outcomes, tobacco screenings, health service utilization, mortality, and total KPNC membership. More detailed descriptions of the data elements can be found in Multimedia Appendix 1, and specific diagnoses tracked in the registry in Multimedia Appendix 2. In each file, we retained and created variables necessary to address our research aims and used codebooks to filter the data efficiently (available upon request). We included all data from 1 year prior to the patient’s index date (serving as a time window for identifying co-occurring health conditions [30]) through the end of the study period.
Figure 1.
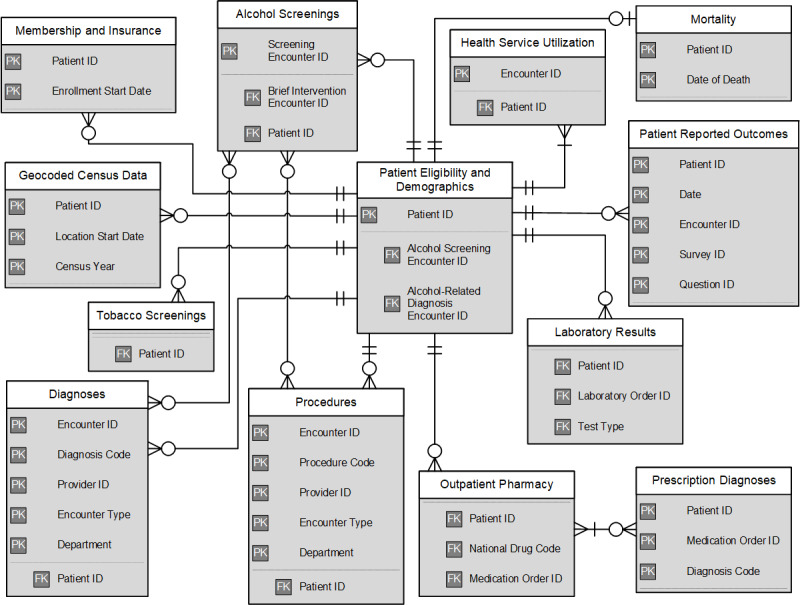
Entity-relationship diagram representing the data structure of core files in the Kaiser Permanente Northern California Adult Alcohol Registry. Primary key variables are unique identifiers that can be used with foreign key variables to link data across files. PK: primary key; FK: foreign key.
Implementation
Implementation of the protocol took about 10 months with 50% programmer time effort. We wrote programs using SAS software, version 9.4 of the SAS System for Unix (SAS Institute), to build the registry, which were designed to minimize user interaction and could be used again to refresh the registry data (eg, using macros and macro variables). We minimized data cleaning to allow future studies to make their own decisions regarding the use of the data. We created a data dictionary to describe the files and variables that comprise the registry. We also developed queries for quality control, such as identifying missing data and characterizing data storage requirements. Last, we created reporting tools to display trends of the registry data over time.
Maintenance
Since the EHR is a constantly changing data environment, refreshing the registry with new data requires programs and documentation to be updated. For example, source variables and tables may be renamed or become deprecated during upgrades of data systems. The amount of time required to refresh the registry depends on the quantity and types of changes needed (eg, adding more ICD codes versus editing SAS programs), but may take anywhere from an hour to several days. Receiving ongoing feedback of the registry as research staff use it for their projects is also critical to ensuring the registry’s validity and usefulness.
Analysis of the Registry Cohort
We calculated the prevalence of alcohol problems among all adult KPNC patients who had at least one encounter with the health system between June 1, 2013, and May 31, 2019. We conducted descriptive analyses to describe demographic, clinical (eg, medical and mental health conditions), and insurance characteristics of the registry cohort. We included only key variables in the current analysis to compare the registry cohort to those in other published studies. All characteristics, such as age, were based on the patient’s index date. We estimated patients’ household income and education using US Census data that has been geocoded to patients’ closest residential addresses in the year prior to and including the month of their index date. If the index date was before January 1, 2017, we used the 2010 US Census data; otherwise, we used 2017 data, since census block boundaries can change over time [31]. We used the median household income of the census block to estimate patients’ household income and categorized patients into groups used in prior epidemiologic studies of the general US population [18,32]. The education level with the highest proportion of households in the census block was used to estimate patients’ education. To identify smoking status, we used the closest screening in the year prior to and including the month of the index date. We calculated the Charlson comorbidity score, which estimates the 1-year mortality risk based on a weighted score of 17 medical conditions [33], and identified chronic medical and mental health conditions and substance use disorder diagnoses in the year prior to the index date. All analyses were conducted using SAS software version 9.4.
Results
We identified 723,604 adult patients eligible for inclusion in the registry between June 1, 2013, to May 31, 2019: 631,780 with unhealthy alcohol use, 143,690 with an AUD diagnosis, and 18,985 with an alcohol-related health problem, anytime during the study period. Counts are not independent, as 65,064 patients met two or more eligibility criteria. Of 4,973,195 adult KPNC patients with at least one encounter with the health system during the study period, the prevalence of unhealthy alcohol use was 13% (631,780/4,973,195), the prevalence of AUD diagnoses was 3% (143,690/4,973,195), and the prevalence of alcohol-related health problems was 0.4% (18,985/4,973,195).
The registry cohort was about 60% (n=432,847) male and 40% (n=290,755) female, and there were 2 patients with other/unknown sex. In regard to gender, 0.1% (n=688) of the cohort were gender minorities (transgender, nonbinary, or other gender). The median age was 41 years (IQR=27; Table 2). The cohort was 19% (n=138,925) Latino/Hispanic, 11% (n=76,197) Asian, Native Hawaiian or Pacific Islander, and 7% (n=50,601) Black. Based on geocoded US Census data, 57% (n=409,004) of the cohort had higher household incomes (≥$70,000) and 72% (n=517,624) had some college or higher education. Most of the cohort had commercial insurance (87%, n=561,620), although 3% (n=19,834) had Medicaid. Patients had a median of 21 months (IQR=39) of follow-up data and up to 15 alcohol screenings after entering the registry (Table 2). About 48% (n=346,408) of the cohort had a chronic medical condition, 18% (n=130,031) had a mental health condition, and 4% (n=30,429) had a drug use disorder diagnosis (Table 3). The most common conditions were hypertension (21%, n=152,928), hyperlipidemia (19%, n=134,705), nicotine use disorder (12%, n=86,540), mood disorder (11%, n=82,059), anxiety disorder (11%, n=76,444), and gastroesophageal reflux (10%, n=71,159).
Table 2.
Characteristics of patients meeting eligibility criteria for the Kaiser Permanente Northern California Adult Alcohol Registry between 6/1/2013 and 5/31/2019 (N=723,604).
| Characteristic | Value | ||
| Sex, n (%)a |
|
||
|
|
Male | 432,847 (59.8) | |
|
|
Female | 290,755 (40.2) | |
|
|
Other/Unknown | 2 (<0.1) | |
| Gender, n (%)a |
|
||
|
|
Male | 432,614 (59.8) | |
|
|
Female | 290,302 (40.1) | |
|
|
Transgender male | 217 (<0.1) | |
|
|
Transgender female | 241 (<0.1) | |
|
|
Non-binary | 229 (<0.1) | |
|
|
Other/Unknown | 1 (<0.1) | |
| Age in years, median (IQR) | 41.0 (27.0) | ||
| Age group (years), n (%)a |
|
||
|
|
18-34 | 279,276 (38.6) | |
|
|
35-49 | 187,072 (25.9) | |
|
|
50-64 | 156,250 (21.6) | |
|
|
≥65 | 101,006 (14.0) | |
| Race/ethnicity, n (%)a |
|
||
|
|
White | 427,606 (59.1) | |
|
|
Asian/Native Hawaiian/Pacific Islander | 76,197 (10.5) | |
|
|
Black | 50,601 (7.0) | |
|
|
Latino/Hispanic | 138,925 (19.2) | |
|
|
Native American | 7,015 (1.0) | |
|
|
Other/Unknown | 23,260 (3.2) | |
| Household income (US$)b, n (%)a |
|
||
|
|
0-19,999 | 5,694 (0.8) | |
|
|
20,000-34,999 | 38,534 (5.3) | |
|
|
35,000-69,999 | 264,638 (36.6) | |
|
|
≥70,000 | 409,004 (56.5) | |
|
|
Unknown | 5,734 (0.8) | |
| Educationc, n (%)a |
|
||
|
|
Less than high school | 32,446 (4.5) | |
|
|
High school graduate | 171,132 (23.6) | |
|
|
Some college or higher | 517,624 (71.5) | |
|
|
Unknown | 2,402 (0.3) | |
| Smoking status, n (%)a |
|
||
|
|
Never or former | 552,618 (76.4) | |
|
|
Current | 115,557 (16.0) | |
|
|
Unknown | 55,429 (7.7) | |
| Charlson comorbidity score, n (%)a |
|
||
|
|
0 | 614,422 (84.9) | |
|
|
1 | 64,420 (8.9) | |
|
|
≥2 | 44,762 (6.2) | |
| Type of insurance, n (%)a |
|
||
|
|
None | 30,033 (4.2) | |
|
|
Medicaid | 19,834 (2.7) | |
|
|
Medicare | 105,393 (14.6) | |
|
|
Commercial | 561,620 (77.6) | |
|
|
Other | 6,724 (0.9) | |
| Enrolled via California Affordable Care Act exchange, n (%)a | 44,110 (6.1) | ||
| Months of follow-up data in the registry, median (IQR) | 21.0 (39.0) | ||
| Number of alcohol screenings, minimum-maximum | 0-15 | ||
aPercentages may not add up to 100% due to rounding error.
bMedian household income from geocoded census blocks to patients’ residential addresses was used as a proxy of individual-level data.
cThe proportion of individuals within a census block with a level of education was used to estimate each patient’s education level.
Table 3.
Diagnosesa of patients in the Kaiser Permanente Northern California Adult Alcohol Registry (N=723,604).
| Condition | Value, n (%) | |||
| Chronic medical conditions | ||||
|
|
Any chronic medical condition | 346,408 (47.9) | ||
|
|
Arthritis and other rheumatic conditions | 70,371 (9.7) | ||
|
|
Asthma | 65,073 (9.0) | ||
|
|
Atherosclerosis | 12,751 (1.8) | ||
|
|
Atrial fibrillation | 49,141 (6.8) | ||
|
|
Cerebrovascular disease | 14,920 (2.1) | ||
|
|
Chronic kidney disease | 23,253 (3.2) | ||
|
|
Chronic liver disease | 21,363 (3.0) | ||
|
|
Chronic obstructive pulmonary disease | 21,953 (3.0) | ||
|
|
Chronic pain | 41,089 (5.7) | ||
|
|
Coronary disease | 20,644 (2.9) | ||
|
|
Dementia | 2,143 (0.3) | ||
|
|
Diabetes | 45,988 (6.4) | ||
|
|
Epilepsy | 5,050 (0.7) | ||
|
|
Gastroesophageal reflux | 71,159 (9.8) | ||
|
|
Heart failure | 8,342 (1.2) | ||
|
|
HIV | 2,424 (0.3) | ||
|
|
Hyperlipidemia | 134,705 (18.6) | ||
|
|
Hypertension | 152,928 (21.1) | ||
|
|
Migraine | 23,600 (3.3) | ||
|
|
Osteoarthritis | 66,800 (9.2) | ||
|
|
Osteoporosis and osteopenia | 18,626 (2.6) | ||
|
|
Parkinson’s disease | 713 (0.1) | ||
|
|
Peptic ulcer | 3,074 (0.4) | ||
|
|
Rheumatoid arthritis | 3,179 (0.4) | ||
| Mental health conditions |
|
|||
|
|
Any mental health condition | 130,031 (18.0) | ||
|
|
Anxiety disorder | 76,444 (10.6) | ||
|
|
|
Obsessive-compulsive disorder | 1,700 (0.2) | |
|
|
|
Panic disorder | 7,823 (1.1) | |
|
|
|
Posttraumatic stress disorder | 5,312 (0.7) | |
|
|
Eating disorder | 924 (0.1) | ||
|
|
|
Anorexia nervosa | 276 (<0.1) | |
|
|
|
Bulimia nervosa | 699 (0.1) | |
|
|
Mood disorder | 82,059 (11.3) | ||
|
|
|
Bipolar disorder | 9,162 (1.3) | |
|
|
|
Depression | 75,445 (10.4) | |
|
|
|
Other mood disorder | 842 (0.1) | |
|
|
Pervasive developmental disorder | 221 (<0.1) | ||
|
|
Psychoses | 6,016 (0.8) | ||
|
|
|
Schizoaffective disorder | 1,427 (0.2) | |
|
|
|
Schizophrenia | 1,534 (0.2) | |
|
|
|
Other psychoses | 4,555 (0.6) | |
|
|
Trauma- and stressor-related disorders | 12,158 (1.7) | ||
| Substance use disorder |
|
|||
|
|
Nicotine use disorder | 86,540 (12.0) | ||
|
|
Any drug use disorder | 30,429 (4.2) | ||
|
|
|
Cannabis | 15,175 (2.1) | |
|
|
|
Cocaine | 4,980 (0.7) | |
|
|
|
Opioid | 5,934 (0.8) | |
|
|
|
Other drugs | 10,418 (1.4) | |
|
|
|
Stimulants | 7,293 (1.0) | |
aDiagnoses were identified using ICD codes given at encounters in the year before the patient’s eligibility date for the registry (ie, index date).
Discussion
In an integrated health system, we identified a large, population-based cohort of adult patients with unhealthy alcohol use, an AUD, or an alcohol-related health problem that had about 2 years of follow-up time. The KPNC Adult Alcohol Registry can evaluate the full course of alcohol problems, longitudinally and comprehensively, including early identification, initiation and engagement in treatment (including psychiatry, addiction medicine, and pharmacotherapy), and long-term outcomes (eg, drinking, physical and mental well-being), which are critical to understanding recovery. The prevalence of unhealthy alcohol use was 13%, which falls within the range reported by prior studies of the general US population (6%-28%) [16,17]. However, the prevalence of AUD diagnoses in our population (3%) was lower than the 2012-2013 prevalence of Diagnostic and Statistical Manual of Mental Disorders-5 (DSM-5) AUD (13.9% [32]) and DSM-IV AUD (12.6%, [18]) estimated from surveys of the general US population, which might be because diagnoses in health systems depend on clinician assessment and diagnosis during utilization of health care services. Only about 7.6% of individuals with AUD in the general US population seek treatment [34] Additionally, these were crude estimates of prevalence over 6 years and not standardized rates, which a future study could evaluate.
Similar to other studies using population-based survey data that indicated a higher prevalence of unhealthy drinking and AUDs in younger males [18,32], our cohort included more males than females, and younger patients (18-34 years) compared to other age groups. The registry cohort was ethnically diverse, but less representative of lower socioeconomic statuses than samples based on the general US population [18,35]. The cohort included patients with a range of mental health conditions and other substance use disorders, enabling future studies to evaluate the treatment and long-term measurable outcomes in these clinically relevant subgroups.
This EHR-based registry provides a strong foundation for robust research examining the development of alcohol problems and recovery from them. In contrast to national population-based surveys such as the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) [36] and clinical trials such as Project MATCH [37] and COMBINE [38] that collect data from participants at study visits (ie, primary data), the registry takes advantage of data that is collected during health care delivery (ie, secondary data). Primary data collection can be costly for both researchers and participants, especially in large populations, while the use of secondary data can be a cost-effective way to achieve similar research goals. Costs of an EHR-based registry include the initial investment to build it and those related to maintaining it over time, which are less than what a primary research study with equivalent sample size and time points would cost. In many ways, EHR data in KPNC are similar to that in the Veterans Health Administration (VA), the nation’s most extensive integrated health care system, which implemented alcohol screening in 2004 [39]; however, our registry cohort of KPNC members is more generalizable to the insured US population since the VA samples are predominantly male, white, and older [40,41].
Additionally, our registry data are longitudinal, spanning over 6 years as of May 31, 2019, and the registry can be continually refreshed with new data extracted from the EHR, including adding new cases and more time points for existing cases. Some current alcohol research studies utilize longitudinal data (eg, NESARC, Project MATCH), but many are repeated cross-sectional studies with different samples (eg, National Health and Nutrition Examination Survey [42], National Health Interview Survey). The registry data are also comprehensive, capturing not only a variety of diagnoses and lab tests that can be used to measure physical functioning, but also health service utilization, insurance factors, and patient-reported outcomes, including alcohol use levels.
We included gender minorities in our registry, given recent research demonstrating a high prevalence of unhealthy drinking in this population [43]. Additionally, the NIAAA has recognized that transgender communities are relevant subpopulations to consider for addressing health disparities [44]. However, there are no general guidelines for how gender minorities should be screened and which risk thresholds to use. For purposes of this registry, we used the patient’s EHR-assigned sex, and when applicable, their response to sex assigned at birth to determine unhealthy alcohol use. We present this approach to be transparent in how sex and gender were operationalized in our registry with the hope of strengthening future research in this area [43].
Limitations
EHR-based registries enable observational studies of “real-world” settings (eg, comparative effectiveness research), an alternative to randomized controlled trials, which may not be feasible; however, using secondary data for research has limitations, including the omission of essential variables and potential for bias (eg, selection bias, information bias, confounding). For example, clinicians in addiction medicine and psychiatry assess AUD symptoms based on the DSM-5, but detailed data are not entered in the EHR. Instead, clinicians record ICD codes to indicate AUD diagnoses, which we use in the registry. While ICD codes for AUDs are not given lightly in other departments, they do occur, and it is not clear what guidelines are used. Therefore, a future validation study of alcohol screening results and the use of these ICD codes is warranted. We also do not have direct measures of individual socioeconomic status (eg, income, education), which are important factors associated with unhealthy alcohol use [18], or social functioning (eg, the Psychosocial Functioning Inventory [45]), an important recovery outcome [46]. Though not only an issue with secondary data analysis, missing data can create bias in a study if it is not missing completely at random; therefore, future studies utilizing the registry data should check for missingness and apply proper statistical methods to address issues as needed [47]. Reliance on accurate reporting of alcohol use and other measures is also a concern; however, it is not a unique problem of EHR data and shared by other studies that collect self-report data. While novel statistical methodologies can be applied to deal with issues of confounding [48] (eg, the counterfactual framework [49]), temporality may remain an issue. Measures of alcohol use and diagnoses are recorded in the EHR when patients seek care rather than when alcohol-related issues emerge, similar to other disease-based registries that rely on data collected during care (eg, diagnostic tests for cancer) and survey-based studies that gather data on past-year or lifetime alcohol problems without specific dates.
Sex and gender variables in the EHR can change and are not collected longitudinally, so their values in the registry reflect what was present at the time of the data extraction rather than historical values, for example, at the time of alcohol screening. We are also not certain which variables are used to determine the appropriate screening questions and risk thresholds (especially for gender minorities), which a future study could evaluate. Therefore, some alcohol screening results may have been misclassified in the registry, affecting eligibility; however, we expect this to have a minimal impact on future studies.
Future Directions
While we included only core data elements that were necessary to address our research aims, the registry could be extended to include other types of data, including provider information, family members of patients with alcohol problems, and medications prescribed off-label to treat AUD (eg, gabapentin [50]). Other health systems in the HCSRN with harmonized VDW data [22] may also want to create their own registry of alcohol problems, enabling the potential for multi-site studies [51-53]. The registry’s utility may also extend beyond research to clinical or administrative purposes, for example, to manage care or evaluate performance, which would require additional support from KPNC organizational stakeholders and institutional review boards to protect patient privacy and confidentiality.
Conclusions
We demonstrate that EHR-based data collected during routine clinical care within an integrated health care system can be leveraged to develop a registry of patients with alcohol problems that is flexible and can be easily refreshed and extended. The registry can be used to address critical public health questions related to the full spectrum and course of alcohol problems, which will complement other methods used in alcohol research. Future analyses will aim to provide insight on how to strengthen efforts in the prevention of alcohol-related disability and mortality and improve patient-centered health care delivery. We hope that other researchers and health systems interested in assembling a similar registry can take advantage of the time we invested in developing this protocol.
Acknowledgments
This project was funded by contracts (#HHSN275201800625P and #75N94019P00907) and a grant (R01AA025902) from the National Institute on Alcohol Abuse and Alcoholism (NIAAA). We gratefully acknowledge Dr Raye Litten and Dr Daniel Falk at the NIAAA for their expertise in alcohol research, and Yun Lu at the Kaiser Permanente Northern California Division of Research for assistance in extracting data used in this project.
Abbreviations
- AUD
alcohol use disorder
- EHR
electronic health record
- HCSRN
Health Care Systems Research Network
- ICD
International Classification of Diseases
- ICD-9
International Classification of Diseases, 9th Revision, Clinical Modification
- ICD-10
International Classification of Diseases, 10th Revision, Clinical Modification
- KP
Kaiser Permanente
- KPNC
Kaiser Permanente Northern California
- NESARC
National Epidemiologic Survey on Alcohol and Related Conditions
- NIAAA
National Institute on Alcohol Abuse and Alcoholism
- VDW
Virtual Data Warehouse
Appendix
Detailed descriptions of data elements in the Kaiser Permanente Northern California Adult Alcohol Registry.
Additional diagnoses tracked among patients in the Kaiser Permanente Northern California Adult Alcohol Registry.
Footnotes
Conflicts of Interest: None declared.
References
- 1.Schmittdiel J, Bodenheimer T, Solomon NA, Gillies RR, Shortell SM. Brief report: The prevalence and use of chronic disease registries in physician organizations. A national survey. J Gen Intern Med. 2005 Sep;20(9):855–8. doi: 10.1111/j.1525-1497.2005.0171.x. https://onlinelibrary.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=0884-8734&date=2005&volume=20&issue=9&spage=855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McEvoy P, Laxade S. Patient registries: a central component of the chronic care model. Br J Community Nurs. 2008 Mar;13(3):127–8, 130. doi: 10.12968/bjcn.2008.13.3.28677. [DOI] [PubMed] [Google Scholar]
- 3.Feller DJ, Lor M, Zucker J, Yin MT, Olender S, Ferris DC, Elhadad N, Mamykina L. An investigation of the information technology needs associated with delivering chronic disease care to large clinical populations. Int J Med Inform. 2020 Feb 13;137:104099. doi: 10.1016/j.ijmedinf.2020.104099. [DOI] [PubMed] [Google Scholar]
- 4.Gliklich RE, Dreyer NA, Leavy MB, editors. Registries for Evaluating Patient Outcomes: A User's Guide. 3rd ed. Rockville, MD: Agency for Healthcare Research and Quality (US); 2014. Apr, Section I. Creating Registries. [PubMed] [Google Scholar]
- 5.Global status report on alcohol and health 2018. Geneva: World Health Organization; 2018. [2019-09-10]. https://apps.who.int/iris/bitstream/handle/10665/274603/9789241565639-eng.pdf?ua=1. [Google Scholar]
- 6.White AM, Castle IP, Hingson RW, Powell PA. Using Death Certificates to Explore Changes in Alcohol-Related Mortality in the United States, 1999 to 2017. Alcohol Clin Exp Res. 2020 Jan;44(1):178–187. doi: 10.1111/acer.14239. [DOI] [PubMed] [Google Scholar]
- 7.Spillane S, Shiels MS, Best AF, Haozous EA, Withrow DR, Chen Y, Berrington de González A, Freedman ND. Trends in Alcohol-Induced Deaths in the United States, 2000-2016. JAMA Netw Open. 2020 Feb 05;3(2):e1921451. doi: 10.1001/jamanetworkopen.2019.21451. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2019.21451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Samokhvalov AV, Rehm J, Roerecke M. Alcohol Consumption as a Risk Factor for Acute and Chronic Pancreatitis: A Systematic Review and a Series of Meta-analyses. EBioMedicine. 2015 Dec;2(12):1996–2002. doi: 10.1016/j.ebiom.2015.11.023. https://linkinghub.elsevier.com/retrieve/pii/S2352-3964(15)30208-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ricci C, Wood A, Muller D, Gunter MJ, Agudo A, Boeing H, van der Schouw YT, Warnakula S, Saieva C, Spijkerman A, Sluijs I, Tjønneland A, Kyrø C, Weiderpass E, Kühn T, Kaaks R, Sánchez M, Panico S, Agnoli C, Palli D, Tumino R, Engström G, Melander O, Bonnet F, Boer JMA, Key TJ, Travis RC, Overvad K, Verschuren WMM, Quirós JR, Trichopoulou A, Papatesta E, Peppa E, Iribas CM, Gavrila D, Forslund A, Jansson J, Matullo G, Arriola L, Freisling H, Lassale C, Tzoulaki I, Sharp SJ, Forouhi NG, Langenberg C, Saracci R, Sweeting M, Brennan P, Butterworth AS, Riboli E, Wareham NJ, Danesh J, Ferrari P. Alcohol intake in relation to non-fatal and fatal coronary heart disease and stroke: EPIC-CVD case-cohort study. BMJ. 2018 May 29;361:k934. doi: 10.1136/bmj.k934. http://www.bmj.com/cgi/pmidlookup?view=long&pmid=29844013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shield KD, Soerjomataram I, Rehm J. Alcohol Use and Breast Cancer: A Critical Review. Alcohol Clin Exp Res. 2016 Jun;40(6):1166–81. doi: 10.1111/acer.13071. [DOI] [PubMed] [Google Scholar]
- 11.Shield KD, Parry C, Rehm J. Chronic diseases and conditions related to alcohol use. Alcohol Res. 2013;35(2):155–73. http://europepmc.org/abstract/MED/24881324. [PMC free article] [PubMed] [Google Scholar]
- 12.Thomas RM, Francis Gerstel PA, Williams EC, Sun H, Bryson CL, Au DH, Bradley KA. Association between alcohol screening scores and diabetic self-care behaviors. Fam Med. 2012 Sep;44(8):555–63. http://www.stfm.org/fmhub/fm2012/September/Rachel555.pdf. [PubMed] [Google Scholar]
- 13.Worthington J, Fava M, Agustin C, Alpert J, Nierenberg AA, Pava JA, Rosenbaum JF. Consumption of alcohol, nicotine, and caffeine among depressed outpatients. Relationship with response to treatment. Psychosomatics. 1996;37(6):518–22. doi: 10.1016/S0033-3182(96)71515-3. [DOI] [PubMed] [Google Scholar]
- 14.Sullivan LE, Fiellin DA, O'Connor PG. The prevalence and impact of alcohol problems in major depression: a systematic review. Am J Med. 2005 Apr;118(4):330–41. doi: 10.1016/j.amjmed.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 15.Bahorik AL, Leibowitz A, Sterling SA, Travis A, Weisner C, Satre DD. The role of hazardous drinking reductions in predicting depression and anxiety symptom improvement among psychiatry patients: A longitudinal study. J Affect Disord. 2016 Dec;206:169–173. doi: 10.1016/j.jad.2016.07.039. http://europepmc.org/abstract/MED/27475887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Helping patients who drink too much: a clinician's guide. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2005. [2018-03-13]. https://pubs.niaaa.nih.gov/publications/practitioner/cliniciansguide2005/guide.pdf. [Google Scholar]
- 17.Azagba S, Shan L, Latham K, Manzione L. Trends in Binge and Heavy Drinking among Adults in the United States, 2011-2017. Subst Use Misuse. 2020 Jan 30;:1–8. doi: 10.1080/10826084.2020.1717538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grant BF, Chou SP, Saha TD, Pickering RP, Kerridge BT, Ruan WJ, Huang B, Jung J, Zhang H, Fan A, Hasin DS. Prevalence of 12-Month Alcohol Use, High-Risk Drinking, and DSM-IV Alcohol Use Disorder in the United States, 2001-2002 to 2012-2013: Results From the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry. 2017 Sep 01;74(9):911–923. doi: 10.1001/jamapsychiatry.2017.2161. http://europepmc.org/abstract/MED/28793133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mertens JR, Chi FW, Weisner CM, Satre DD, Ross TB, Allen S, Pating D, Campbell CI, Lu YW, Sterling SA. Physician versus non-physician delivery of alcohol screening, brief intervention and referral to treatment in adult primary care: the ADVISe cluster randomized controlled implementation trial. Addict Sci Clin Pract. 2015 Nov 19;10:26. doi: 10.1186/s13722-015-0047-0. https://ascpjournal.biomedcentral.com/articles/10.1186/s13722-015-0047-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gordon N. Similarity of the adult Kaiser Permanente membership in Northern California to the insured and general population in Northern Californiatatistics from the 2011 California Health Interview Survey. 2015. [2019-03-15]. https://divisionofresearch.kaiserpermanente.org/projects/memberhealthsurvey/SiteCollectionDocuments/chis_non_kp_2011.pdf.
- 21.Chi FW, Satre DD, Weisner C. Chemical dependency patients with cooccurring psychiatric diagnoses: service patterns and 1-year outcomes. Alcohol Clin Exp Res. 2006 May;30(5):851–9. doi: 10.1111/j.1530-0277.2006.00100.x. [DOI] [PubMed] [Google Scholar]
- 22.Ross TR, Ng D, Brown JS, Pardee R, Hornbrook MC, Hart G, Steiner JF. The HMO Research Network Virtual Data Warehouse: A Public Data Model to Support Collaboration. EGEMS (Wash DC) 2014;2(1):1049. doi: 10.13063/2327-9214.1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Viviani L, Zolin A, Mehta A, Olesen HV. The European Cystic Fibrosis Society Patient Registry: valuable lessons learned on how to sustain a disease registry. Orphanet J Rare Dis. 2014 Jun 07;9:81. doi: 10.1186/1750-1172-9-81. https://ojrd.biomedcentral.com/articles/10.1186/1750-1172-9-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gitt AK, Bueno H, Danchin N, Fox K, Hochadel M, Kearney P, Maggioni AP, Opolski G, Seabra-Gomes R, Weidinger F. The role of cardiac registries in evidence-based medicine. Eur Heart J. 2010 Mar;31(5):525–9. doi: 10.1093/eurheartj/ehp596. [DOI] [PubMed] [Google Scholar]
- 25.Silverberg MJ, Chao C, Leyden WA, Xu L, Horberg MA, Klein D, Towner WJ, Dubrow R, Quesenberry CP, Neugebauer RS, Abrams DI. HIV infection, immunodeficiency, viral replication, and the risk of cancer. Cancer Epidemiol Biomarkers Prev. 2011 Dec;20(12):2551–9. doi: 10.1158/1055-9965.EPI-11-0777. http://cebp.aacrjournals.org/cgi/pmidlookup?view=long&pmid=22109347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Karter AJ, Ackerson LM, Darbinian JA, D'Agostino RB, Ferrara A, Liu J, Selby JV. Self-monitoring of blood glucose levels and glycemic control: the Northern California Kaiser Permanente Diabetes registry. Am J Med. 2001 Jul;111(1):1–9. doi: 10.1016/s0002-9343(01)00742-2. [DOI] [PubMed] [Google Scholar]
- 27.Oehrli M, Quesenberry C, Leyden W. Annual report on trends, incidence, and outcomes: Northern California Cancer Registry at the Division of Research. Oakland, CA: Kaiser Permanente Northern California; 2018. [Google Scholar]
- 28.Ray GT, Bahorik AL, VanVeldhuisen PC, Weisner CM, Rubinstein AL, Campbell CI. Prescription opioid registry protocol in an integrated health system. Am J Manag Care. 2017 May 01;23(5):e146–e155. https://www.ajmc.com/pubMed.php?pii=87063. [PMC free article] [PubMed] [Google Scholar]
- 29.Alcohol-related ICD codes. Atlanta, GA: Centers for Disease Control and Prevention; 2019. [2019-01-12]. Alcohol and Public Health: Alcohol-Related Disease Impact. https://nccd.cdc.gov/DPH_ARDI/Info/ICDCodes.aspx. [Google Scholar]
- 30.Weisner C, Campbell CI, Altschuler A, Yarborough BJH, Lapham GT, Binswanger IA, Hechter RC, Ahmedani BK, Haller IV, Sterling SA, McCarty D, Satre DD, Kline-Simon AH. Factors associated with Healthcare Effectiveness Data and Information Set (HEDIS) alcohol and other drug measure performance in 2014-2015. Subst Abus. 2019;40(3):318–327. doi: 10.1080/08897077.2018.1545728. http://europepmc.org/abstract/MED/30676915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rossiter K. What are census blocks? United States Census Bureau; 2011. [2020-03-23]. https://www.census.gov/newsroom/blogs/random-samplings/2011/07/what-are-census-blocks.html. [Google Scholar]
- 32.Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, Pickering RP, Ruan WJ, Smith SM, Huang B, Hasin DS. Epidemiology of DSM-5 Alcohol Use Disorder: Results From the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015 Aug;72(8):757–66. doi: 10.1001/jamapsychiatry.2015.0584. http://europepmc.org/abstract/MED/26039070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992 Jun;45(6):613–9. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 34.Olfson M, Blanco C, Wall MM, Liu S, Grant BF. Treatment of Common Mental Disorders in the United States: Results From the National Epidemiologic Survey on Alcohol and Related Conditions-III. J Clin Psychiatry. 2019 May 28;80(3) doi: 10.4088/JCP.18m12532. http://www.psychiatrist.com/JCP/article/Pages/2019/v80/18m12532.aspx. [DOI] [PubMed] [Google Scholar]
- 35.Chavez LJ, Bradley K, Tefft N, Liu C, Hebert P, Devine B. Preference weights for the spectrum of alcohol use in the U.S. Population. Drug Alcohol Depend. 2016 Apr 01;161:206–13. doi: 10.1016/j.drugalcdep.2016.02.004. [DOI] [PubMed] [Google Scholar]
- 36.National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III) Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2015. [2019-09-27]. https://www.niaaa.nih.gov/research/nesarc-iii. [Google Scholar]
- 37.Project MATCH Research Group Project MATCH (Matching Alcoholism Treatment to Client Heterogeneity): rationale and methods for a multisite clinical trial matching patients to alcoholism treatment. Alcohol Clin Exp Res. 1993 Dec;17(6):1130–45. doi: 10.1111/j.1530-0277.1993.tb05219.x. [DOI] [PubMed] [Google Scholar]
- 38.COMBINE Study Research Group Testing combined pharmacotherapies and behavioral interventions in alcohol dependence: rationale and methods. Alcohol Clin Exp Res. 2003 Jul;27(7):1107–22. doi: 10.1097/00000374-200307000-00011. [DOI] [PubMed] [Google Scholar]
- 39.Bradley KA, Williams EC, Achtmeyer CE, Volpp B, Collins BJ, Kivlahan DR. Implementation of evidence-based alcohol screening in the Veterans Health Administration. Am J Manag Care. 2006 Oct;12(10):597–606. https://www.ajmc.com/pubMed.php?pii=3204. [PubMed] [Google Scholar]
- 40.Chavez LJ, Williams EC, Lapham GT, Rubinsky AD, Kivlahan DR, Bradley KA. Changes in Patient-Reported Alcohol-Related Advice Following Veterans Health Administration Implementation of Brief Alcohol Interventions. J Stud Alcohol Drugs. 2016 May;77(3):500–8. doi: 10.15288/jsad.2016.77.500. http://europepmc.org/abstract/MED/27172583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kalpakci A, Sofuoglu M, Petrakis I, Rosenheck RA. Gender differences among Veterans with alcohol use disorder nationally in the Veterans Health Administration. J Addict Dis. 2018;37(3-4):185–194. doi: 10.1080/10550887.2019.1653739. [DOI] [PubMed] [Google Scholar]
- 42.National Center for Health Statistics. Atlanta, GA: Centers for Disease Control and Prevention; 2019. [2019-09-26]. National Health and Nutrition Examination Survey. https://www.cdc.gov/nchs/nhanes/index.htm. [Google Scholar]
- 43.Gilbert PA, Pass LE, Keuroghlian AS, Greenfield TK, Reisner SL. Alcohol research with transgender populations: A systematic review and recommendations to strengthen future studies. Drug Alcohol Depend. 2018 May 01;186:138–146. doi: 10.1016/j.drugalcdep.2018.01.016. http://europepmc.org/abstract/MED/29571076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.National Institute on Alcohol Abuse and Alcoholism Strategic Plan 2017-2021. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2017. [2019-09-25]. https://www.niaaa.nih.gov/sites/default/files/StrategicPlan_NIAAA_optimized_2017-2020.pdf. [Google Scholar]
- 45.Feragne MA, Longabaugh R, Stevenson JF. The psychosocial functioning inventory. Eval Health Prof. 1983 Mar;6(1):25–48. doi: 10.1177/016327878300600102. [DOI] [PubMed] [Google Scholar]
- 46.Witkiewitz K, Kirouac M, Roos CR, Wilson AD, Hallgren KA, Bravo AJ, Montes KS, Maisto SA. Abstinence and low risk drinking during treatment: Association with psychosocial functioning, alcohol use, and alcohol problems 3 years following treatment. Psychol Addict Behav. 2018 Sep;32(6):639–646. doi: 10.1037/adb0000381. http://europepmc.org/abstract/MED/30160499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rubin DB. Inference and Missing Data. Biometrika. 1976 Dec;63(3):581. doi: 10.2307/2335739. [DOI] [Google Scholar]
- 48.Grimes DA, Schulz KF. Bias and causal associations in observational research. Lancet. 2002 Jan 19;359(9302):248–52. doi: 10.1016/S0140-6736(02)07451-2. [DOI] [PubMed] [Google Scholar]
- 49.Bours MJL. A nontechnical explanation of the counterfactual definition of confounding. J Clin Epidemiol. 2020 Feb 14;121:91–100. doi: 10.1016/j.jclinepi.2020.01.021. [DOI] [PubMed] [Google Scholar]
- 50.Anton RF, Latham P, Voronin K, Book S, Hoffman M, Prisciandaro J, Bristol E. Efficacy of Gabapentin for the Treatment of Alcohol Use Disorder in Patients With Alcohol Withdrawal Symptoms: A Randomized Clinical Trial. JAMA Intern Med. 2020 Mar 09; doi: 10.1001/jamainternmed.2020.0249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Binswanger IA, Carroll NM, Ahmedani BK, Campbell CI, Haller IV, Hechter RC, McNeely J, Yarborough BJH, Kline-Simon AH, Satre DD, Weisner C, Lapham GT. The association between medical comorbidity and Healthcare Effectiveness Data and Information Set (HEDIS) measures of treatment initiation and engagement for alcohol and other drug use disorders. Subst Abus. 2019;40(3):292–301. doi: 10.1080/08897077.2018.1545726. http://europepmc.org/abstract/MED/30676892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Health Care Systems Research Network The Virtual Data Warehouse (VDW) and how to use it. http://www.hcsrn.org/en/Resources/VDW/VDWScientists/The+VDW+and+How+to+Use+It.pdf.
- 53.Yarborough BJH, Ahmedani BK, Boggs JM, Beck A, Coleman KJ, Sterling S, Schoenbaum M, Goldstein-Grumet J, Simon GE. Challenges of Population-based Measurement of Suicide Prevention Activities Across Multiple Health Systems. EGEMS (Wash DC) 2019 Apr 12;7(1):13. doi: 10.5334/egems.277. http://europepmc.org/abstract/MED/30993146. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Detailed descriptions of data elements in the Kaiser Permanente Northern California Adult Alcohol Registry.
Additional diagnoses tracked among patients in the Kaiser Permanente Northern California Adult Alcohol Registry.


