Abstract
Objective: To study the effect of intermittent hypoxia training (IHT) for migraine. Design: A single-blind, randomized controlled trial. All participants were recruited from a rehabilitation department in an acute university-affiliated hospital. Methods: Participants with migraines were randomly assigned to two groups (IHT group and control group). The Migraine Disability Assessment (MIDAS), Visual Analog Scale (VAS), Beck Depression Inventory (BDI), Beck Anxiety Inventory (BAI), Vascular endothelial growth factor (VEGF), calcitonin gene related peptide (CGRP) and cerebrovascular hemodynamic parameters were collected at baseline and end of the 8th week. The attack frequencies of migraines were evaluated at 3 months. Results: Among the 48 subjects, five males and forty-three females, the ages ranged from 19 to 53 years old (mean ± SD = 31.3±7.78). MIDAS, SF-36, VAS, BAI, BDI, VEGF, CGRP and cerebrovascular hemodynamic parameters were improved after IHT intervention. There were significant differences between IHT group and the control group in MIDAS, SF-36, VAS, BAI, BDI, VEGF, CGRP and cerebrovascular hemodynamic parameters at the end of the 8th weeks (P<0.05). Attack frequencies were improved within 3 months after IH training intervention (P<0.01), but not in the control group (P>0.05). No adverse events occurred during the study. Conclusion: IHT could improve migraines after intervention up to three months. IHT could be an effective method for relieving a migraine.
Keywords: Intermittent hypoxia training, migraine
Introduction
A migraine is a common headache disorder characterized by recurrent headaches that are moderate to severe and occur more frequently in women. Typically, the headaches affect one half of the head, are pulsating in nature, and last from 2 to 72 hours [1]. Accompanying symptoms often include nausea, vomiting, and sensitivity to light, sound, or smell, some patients even have agonal feeling with a migraine attack [2]. The pain is generally made worse by physical activity or emotional fluctuation [3]. Up to one-third of people have an aura: typically a short period of visual disturbance that signals that the headache will soon occur [3]. Occasionally, an aura can occur with little or no headache following it [4]. A patient who is experiencing a migraine often suffers from limitations in various common daily activities and is in a dangerous predicament because they can’t control onset time, frequency or emotion.
The underlying mechanisms of a migraine are not fully known. However, it is believed to involve the nerves and blood vessels of the brain. Pain medication (ibuprofen and paracetamol), β1 receptor blocker (metoprolol) and other drugs (valproate) for the treatment of migraines are used to prevent or alleviate the migraine [5,6]. They have failed to completely halt the migraine. Other treatments like acupuncture or physiotherapy have few effects for migraines [7]. It remains a challenge for physicians to remedy, therefore new approaches in treatment are needed.
Intermittent hypoxia training (IHT) is initially recognized by the sports medicine community as a potentially useful strategy to enhance exercise performance in athletes [8]. Living or training under hypoxic conditions may improve exercise performance by promoting cardiopulmonary function without eliciting the detrimental effects of chronic hypoxic exposure. Beyond the enhancement of physical performances [9], and on the basis of some established protective preclinical effects of IH, hypoxic conditioning in healthy subjects has been evaluated as a potentially useful intervention to improve some physiological functions. These include vasomotor function by mediating release of medium in the brain, which may be associated with a migraine [10]. In our previous study, we found that intermittent hypoxia training had an exact effect to dizziness due to its mediating intracranial vessel vasomotor function [11].
To our knowledge, there were minimal studies investigating the effects of IHT for a migraine. The purpose of this study was to investigate migraine improvement under the IHT.
Materials and methods
Study design
This was a prospective, assessor-blinded randomized controlled trial with an 8-week training period, conducted in a rehabilitation department in an acute university-affiliated hospital. The trial was registered with the Chinese Clinical Trial Registry (Study ID ChiCTR1900028242). This study was in accordance with the ethical standards of the responsible committee on human experimentation. All patients were randomly divided into two groups based on the different interventions (IHT group, control group). Randomization was conducted with the method of a computerized sample of convenience after a subject was screened, recruited, and signed an informed consent statement. Assessments were conducted at baseline and the end of the 8th week by a therapist who was blinded to the subjects’ interventions.
Subjects
In this study, of the 66 patients admitted from the acute comprehensive hospital in China from January to December in 2019, 48 patients met the selection criteria. The inclusion criteria for patients were: 1) mentally intact and were able to follow directions; 2) no intracranial lesions by CT or MRI check. Patients were excluded if they had: 1) stroke or transient ischemic attack; 2) headache induced by cervical spondylosis, depression, insomnia, neurasthenia, or intracranial lesions, et al; 3) severe cardiac, liver or kidney dysfunction that caused hospitalization in the last 3 months. All patients provided a written informed consent.
Intermittent hypoxia intervention
Normobaric hypoxia condition was applied by exposing subjects to 5 cycles of 10% O2 for 5 min followed by room air for 5 min. Subjects inspired hypoxic air through an air-cushioned disposable face-mask and then room air directed by a 3-way valve. All subjects practiced intermittent hypoxia 50 minutes per session, 5 times per week for 8 weeks.
Some subjects may be hyper-sensitive to hypoxia (such as an extreme tachycardiac response and/or hyperventilation), although short-duration (5 min) exposures to hypoxia have negligible risk to evoke extreme hyper-reactivity. The orientation session will screen the subjects who cannot tolerate or may have extreme tachycardia and hyperventilation reactions to the face-mask or hypoxic air. Should any subject not get accustomed to the face mask/hypoxic air or have an extreme hyper-reactivity in heart rate, i.e., increases in heart rate more than +30 beats/min, or in ventilation, i.e., breathing frequency more than 24 breaths/min, during hypoxic exposures, we will remove the face-mask immediately and allow the subject direct room air to breathe. The removal of the face mask will eliminate the source of the subject’s distress and result in the subject being released from the whole study. In case of severe reaction, emergency medical services will be made.
Clinical assessments
The baseline information included age, gender and time of onset, et al.
The primary migraine-related scale assessments
The Migraine Disability Assessment (MIDAS), Visual Analog Scale (VAS), Beck Depression Inventory (BDI), and Beck Anxiety Inventory (BAI) were collected at baseline and end of the 8th week. The attack frequencies of migraines were evaluated at 3 months.
The MIDAS is a 5-question tool to quantitatively evaluate the headache-related disability in terms of the number of days in the past 3 months and activity limitations due to the migraines. Scores (0-27), measured the overall level of disability: Grade I (0-5), Grade II (6-10), Grade III (11-20), and Grade IV (above 21). It was found to be both reliable and valid [12].
Pain was measured by means of a VAS with 0 indicating no pain and 10 indicating unbearable pain. The VAS is a valid and reliable measure for pain, and changes of 2 or more were considered as clinically relevant. Reliability for VAS was 0.97 [13].
The BDI is the most commonly used self-rating scale for depression [14]. Participants rated 21 items on a scale from 0 to 3 according to how they felt at the time. Scale 0-9: normal to minimal depression; 10-18: mild to moderate depression; 19-29: moderate to severe depression; 30-63: severe depression. Cronbach coefficient was 0.8.
The BAI is a 21-item self-report measure of anxiety severity, with each item describing a common symptom of anxiety [15]. The respondent is asked to rate how much he or she has been bothered by anxiety symptoms during the previous week on a 4-point scale (0-3). Scale 0-9: normal to minimal anxiety; 10-18: mild to moderate anxiety; 19-29: moderate to severe anxiety; 30-63: severe anxiety. Cronbach coefficient was 0.94.
SF-36 assesses the quality of life in eight areas, including physical functioning, role physical, bodily pain, general health, vitality, social function, emotional role, and mental health. In addition, Physical Component Summary (PCS) encompasses PF, RP, and BP, whereas Mental Component Summary (MCS) includes SF, RE, and MH. Scores ranged from 0-100, with 0 corresponding to low HRQL (Health-Related Quality of Life) and 100 corresponding to high HRQ Scores were recorded from each domain to assess a subject’s quality of life. Reliability for SF-36 was 0.87 [16].
The serum markers and cerebrovascular hemodynamic parameters test vascular endothelial growth factor (VEGF), calcitonin gene related peptide (CGRP) and cerebrovascular hemodynamic parameters were collected at baseline and 8th week.
3 ml venous blood was drawn on baseline and end of the 8th week, the supernatant was taken after centrifugation. VEGF and CGRP were detected by enzyme linked immunosorbent assays. Kits were purchased from Sigma company, and operation steps were implemented strictly according to kit instructions.
For the middle cerebral arteries (MCAs), bilateral flow velocity was simultaneously recorded using a Multi-Dop X/TCD transcranial Doppler instrument (KJ-2V6M, China). Continuous measurements were obtained using two dual 2-MHz transducers fitted on a headband and placed on the temporal bone windows. The optimal signal was obtained at a depth of 50 to 60 mm. For basilar artery (BA) recordings, a probe was placed on the back of the neck and directed toward the foramen magnum. The optimal signal was obtained at a depth of 75 to 85 mm.
Statistical analysis
The data was analyzed using SPSS for Windows version 20.0. Continuous Data was expressed as means and standard deviations. The comparison between baseline and end of the 8th week within each group was performed by the paired t tests for continuous data and McNemar tests for discrete data. The comparisons between groups at baseline and end of 8th week were conducted using one-way analysis of variance for continuous data and X2 tests for discrete data. Significant level was set at P<0.05.
Results
The flow diagram of eligible patients was shown in the study. A total of 66 participants were admitted to the study in the beginning and 18 patients were excluded for several reasons (details are shown in Figure 1). Of these, 48 patients met the inclusion criteria and consented to receive the intervention and follow-up assessment. Eventually, 48 patients completed the study without dropout.
Figure 1.
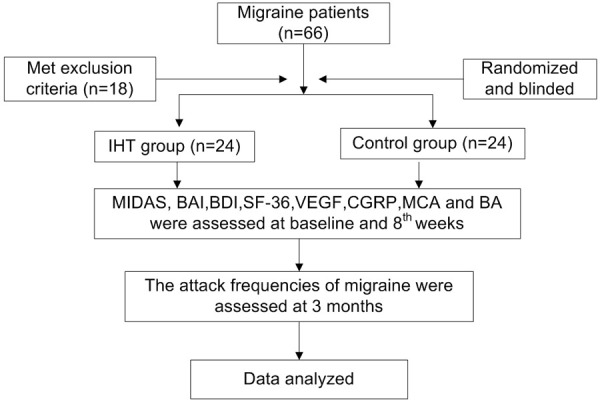
Flow diagram.
Among the 48 subjects, five males and forty-three females, the ages ranged from 19 to 53 years old. (mean ± SD = 31.3±7.78). There was no drop-out during the whole 8-week intervention. Demographic data of the recruited patients were shown in Table 1.
Table 1.
Clinical data
| IHT group | Control group | |
|---|---|---|
| Gender (female) | 21 (87.5%) | 22 (91.7%) |
| Age (years) | 32.1±9.22 | 30.6±5.92 |
| Age since migraine (years) | 22.0±3.39 | 22.3±2.94 |
| Family history | 9 (37.5%) | 11 (45.8%) |
| Other disease | Hyperlipemia (2) | Hyperlipemia (3) |
| Hypertension (1) | Hypertension (0) | |
| Diabetes (1) | Diabetes (0) |
There were clinical data for three groups. Values were presented as mean ± standard deviation; IHT: intermittent hypoxia training.
The comparisons within groups for MIDAS, SF-36, VAS, BAI, BDI, VEGF, CGRP, MCA and BA were shown in Table 2. MIDAS, SF-36, VAS, BAI, BDI scores, VEGF, CGRP, MCA and BA were improved after IHT intervention at the end of 8th week. There were significant differences between IHT group and control group in MIDAS, SF-36, VAS, BAI, BDI scores, VEGF, CGRP, MCA and BA after IHT intervention in the end of 8th weeks (P<0.05).
Table 2.
Comparison of MIDAS, VAS, BAI, BDI, SF-36, MCAs, BA, VEGF and CGRP within groups at 8th week
| IHT Group | Control Group | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||
| Baseline | 8 weeks | P1 value | Baseline | 8 weeks | P1 value | P2 value | P3 value | ||
| MIDAS | 23.4±5.27 | 12.1±3.12 | P<0.05 | 22.6±6.34 | 17.8±5.66 | 0.059 | 0.75 | P<0.05 | |
| SF-36 | PCS | 37.9±5.81 | 50.4±7.57 | P<0.05 | 37.4±3.97 | 40.6±6.51 | 0.16 | 0.79 | P<0.05 |
| MCS | 37.4±6.37 | 48.4±7.61 | P<0.05 | 36.9±5.69 | 41.5±6.06 | 0.06 | 0.85 | P<0.05 | |
| VAS | 6.3±0.92 | 2.3±0.84 | P<0.05 | 6.2±1.06 | 5.4±1.18 | 0.13 | 0.84 | P<0.05 | |
| BAI | 19.3±5.01 | 13.1±3.05 | P<0.05 | 18.9±3.87 | 16.6±3.89 | 0.15 | 0.83 | P<0.05 | |
| BDI | 17.8±3.23 | 12.3±2.91 | P<0.05 | 18.8±2.98 | 17.1±3.42 | 0.19 | 0.43 | P<0.05 | |
| Right MCA | 64.3±7.29 | 51.7±6.76 | P<0.05 | 62.3±6.98 | 58.6±3.72 | 0.18 | 0.56 | P<0.05 | |
| Left MCA | 66.7±7.30 | 53.7±6.26 | P<0.05 | 68.5±4.36 | 64.3±4.45 | 0.058 | 0.53 | P<0.05 | |
| BA | 36.1±4.3 | 26.3±3.38 | P<0.05 | 36.5±4.80 | 34.7±4.42 | 0.41 | 0.85 | P<0.05 | |
| VEGF | 1470.3±132.45 | 1243.6±75.38 | P<0.05 | 1456.7±138.54 | 1421.8±143.90 | 0.69 | 0.87 | P<0.05 | |
| CGRP | 19.0±3.24 | 13.1±2.52 | P<0.05 | 18.4±2.64 | 18.9±2.42 | 0.58 | 0.69 | P<0.05 | |
Values were presented as mean ± standard deviation; P1: comparison between baseline and end of 8th week; P2: comparison between IHT group and control group on baseline; P3: comparison between IH group and control group on end of 8th week. IHT: intermittent hypoxia training; MIDAS: Migraine Disability Assessment; VAS: visual analog scale; BDI: Beck Depression Inventory; BAI: Beck Anxiety Inventory. MCA: Middle Cerebral Artery; BA: Basilar Artery; VEGF: Vascular Endothelial Growth Factor; CGRP: Calcitonin Gene Related Peptide.
The attack frequencies of the migraines within 3 months before and after intervention were showed in Table 3. Attack frequencies were improved within 3 months after IH training intervention (P<0.01), but not in the control group (P>0.05). There was a significant difference between IHT group and control group within 3 months after IHT intervention (P<0.01).
Table 3.
Attack frequency before and after intervention
| Group | Number | Baseline | 3 months | P value |
|---|---|---|---|---|
| IHT Group | 24 | 13.4±4.79 | 7.7±3.95 | <0.01 |
| Control Group | 24 | 15.9±5.50 | 13.6±4.48 | 0.27 |
| P value | 0.23 | <0.01 |
Attack frequency was collected at 3 months before and after intervention. Values were presented as mean ± standard deviation; IHT: intermittent hypoxia training.
Safety outcomes
No adverse events occurred during the study such as chest distress, palpitation, falling, or hyperventilation reactions to the face-mask or hypoxic air.
Discussion
This was the first study to investigate the effects of intermittent hypoxia training in migraine patients. The main new finding of this study was that intermittent hypoxia training significantly relieved the headache, reduced the frequency of migraines and improved the symptom of anxiety and depression induced by a migraine.
The assumptive mechanism of IHT
The mechanism of migraines was complicated. Some studies reported that neuronal mechanisms play a greater role [17], while others believe blood vessels play the key role [18]. Others believe both are likely important. However, the exact mechanism of a migraine remains unknown. Jacobs B [19] reported that migraines were a neurovascular disorder with evidence supporting its mechanisms starting within the brain and then spreading to the blood vessels. Another study reported that migraines maybe associate with increased cerebral blood flow velocities which could be an important factor in migraines [20]. In addition, the effect of hypoxia was to regulate medium release, such as nitric oxide, hypoxia-inducible factor 1 (HIF-1) [21], vascular endothelial growth factor (VEGF) [22,23], or calcitonin gene-related peptide, (CGRP) [24] which could be related to vasodilator or vasculogenesis. In our results, we found that the blood flow velocities of MCAs and BA, VEGF and CGRP were improved after IHT intervention. Hypoxia could regulate the medium release and improve the cerebral blood flow [25,26]. Although the physiological mechanisms underlying vascular adaptations and medium release to hypoxic environment had not yet been elucidated, several studies have indicated that hypoxia is one of the most potent mediators of vessels function [27].
The difference of IHT and chronic hypoxia
The therapeutic application of moderate IHT should not be confused with the intense, episodic intermittent hypoxia associate with sleep apnea. Sleep apnea is a pathological condition which has shorter episodes of hypoxia which are usually more severe and continue throughout sleep for years. This is often accompanied by added stress of partial or complete nocturnal arousal and persistent activation of the sympathetic nervous system. It produced chronic hypertension and had adverse cardiovascular and cerebral effects. In contrast, therapeutic IHT utilized exposures to moderately severe hypoxia produced in hypobaric chambers or by inspiring normobaric atmospheres with O2 content lowered to approximately 10%. Animals, like rats and dogs, subjected to these protocols showed no distress, and humans reported no discomfort. In our previous study, we confirmed that the intermittent hypoxia training was safe for dizziness patients [11]. In other laboratories, human subjects with ischemic heart disease [28,29] and chronic obstructive pulmonary disease [30] had completed similar protocols with no untoward effects. Therefore, IHT is safe and convenient.
In our study, we exposed subjects to 5 cycles of 10% O2 for 5 min followed by room air for 5 min for 8 weeks. We found migraines were improved after intervention and episodes of migraines were reduced. We did not find any adverse events in our study. Although the data is encouraging, some study limitations should be noted. First, we only evaluated the outcomes within three months after intervention, but we did not perform the longer follow up. Therefore, we are not sure from this study how long the effects from each intervention would last after three months. Second, the small sample of subjects might cause insufficient statistical power. This means the results of study may be wrong.
Conclusion
IHT could improve migraines after intervention up to three months. IHT could be an effective method for relieving a migraine.
Acknowledgements
The authors would like to thank all the professors and coworkers for their tireless assistance to this project. We would also thank the individuals who participated in this study as well as all of administrative support staffs for this study. The work presented here is funded by the Science and Technology Planning Project in Shaoguan, China (No. 2018sn022).
Disclosure of conflict of interest
None.
References
- 1.Mayans L. Headache: migraine. FP Essent. 2018;473:11–16. [PubMed] [Google Scholar]
- 2.Cook CL, Shedd GC. Diagnosis and treatment of migraine in the patient with depression. J Am Assoc Nurse Pract. 2018;30:630–637. doi: 10.1097/JXX.0000000000000075. [DOI] [PubMed] [Google Scholar]
- 3.Headache Classification Subcommittee of the International Headache Society. The international classification of headache disorders: 2nd edition. Cephalalgia. 2004;24(Suppl 1):9–160. doi: 10.1111/j.1468-2982.2003.00824.x. [DOI] [PubMed] [Google Scholar]
- 4.Gago-Veiga AB, Pagan J, Henares K, Heredia P, Gonzalez-Garcia N, De Orbe MI, Ayala JL, Sobrado M, Vivancos J. To what extent are patients with migraine able to predict attacks? J Pain Res. 2018;11:2083–2094. doi: 10.2147/JPR.S175602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hebestreit JM, May A. The enigma of site of action of migraine preventives: no effect of metoprolol on trigeminal pain processing in patients and healthy controls. J Headache Pain. 2017;18:116. doi: 10.1186/s10194-017-0827-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dakhale GN, Sharma VS, Thakre MN, Kalikar M. Low-dose sodium valproate versus low-dose propranolol in prophylaxis of common migraine headache: a randomized, prospective, parallel, open-label study. Indian J Pharmacol. 2019;51:255–262. doi: 10.4103/ijp.IJP_457_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhou J, Li J, Yang J, Li J, Wang C. Acupuncture methods for acute migraine attack: a Bayesian network meta-analysis protocol. BMJ Open. 2019;9:e031043. doi: 10.1136/bmjopen-2019-031043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Millet GP, Roels B, Schmitt L, Woorons X, Richalet JP. Combining hypoxic methods for peak performance. Sports Med. 2010;40:1–25. doi: 10.2165/11317920-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 9.Wilber RL. Application of altitude/hypoxic training by elite athletes. Med Sci Sports Exerc. 2007;39:1610–1624. doi: 10.1249/mss.0b013e3180de49e6. [DOI] [PubMed] [Google Scholar]
- 10.Tringali G, Navarra P. Anti-CGRP and anti-CGRP receptor monoclonal antibodies as antimigraine agents. Potential differences in safety profile postulated on a pathophysiological basis. Peptides. 2019;116:16–21. doi: 10.1016/j.peptides.2019.04.012. [DOI] [PubMed] [Google Scholar]
- 11.Bao X, Tan JW, Long Y, Liu H, Liu HY. Effect of intermittent hypoxia training for dizziness: a randomized controlled trial. J Sport Rehabil. 2019;28:540–543. doi: 10.1123/jsr.2017-0341. [DOI] [PubMed] [Google Scholar]
- 12.Stewart WF, Lipton RB, Dowson AJ, Sawyer J. Development and testing of the Migraine Disability Assessment (MIDAS) questionnaire to assess headache-related disability. Neurology. 2001;56:S20–28. doi: 10.1212/wnl.56.suppl_1.s20. [DOI] [PubMed] [Google Scholar]
- 13.Gallagher EJ, Liebman M, Bijur PE. Prospective validation of clinically important changes in pain severity measured on a visual analog scale. Ann Emerg Med. 2001;38:633–638. doi: 10.1067/mem.2001.118863. [DOI] [PubMed] [Google Scholar]
- 14.Sun XY, Li YX, Yu CQ, Li LM. Reliability and validity of depression scales of Chinese version: a systematic review. Zhonghua Liu Xing Bing Xue Za Zhi. 2017;38:110–116. doi: 10.3760/cma.j.issn.0254-6450.2017.01.021. [DOI] [PubMed] [Google Scholar]
- 15.Liang Y, Wang L, Zhu J. Factor structure and psychometric properties of Chinese version of Beck Anxiety Inventory in Chinese doctors. J Health Psychol. 2018;23:657–666. doi: 10.1177/1359105316658971. [DOI] [PubMed] [Google Scholar]
- 16.Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 17.Goadsby PJ. The vascular theory of migraine--a great story wrecked by the facts. Brain. 2009;132:6–7. doi: 10.1093/brain/awn321. [DOI] [PubMed] [Google Scholar]
- 18.Brennan KC, Charles A. An update on the blood vessel in migraine. Curr Opin Neurol. 2010;23:266–274. doi: 10.1097/WCO.0b013e32833821c1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jacobs B, Dussor G. Neurovascular contributions to migraine: moving beyond vasodilation. Neuroscience. 2016;338:130–144. doi: 10.1016/j.neuroscience.2016.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Silvestrini M, Baruffaldi R, Bartolini M, Vernieri F, Lanciotti C, Matteis M, Troisi E, Provinciali L. Basilar and middle cerebral artery reactivity in patients with migraine. Headache. 2004;44:29–34. doi: 10.1111/j.1526-4610.2004.04006.x. [DOI] [PubMed] [Google Scholar]
- 21.Rodriguez-Miguelez P, Lima-Cabello E, Martinez-Florez S, Almar M, Cuevas MJ, Gonzalez-Gallego J. Hypoxia-inducible factor-1 modulates the expression of vascular endothelial growth factor and endothelial nitric oxide synthase induced by eccentric exercise. J Appl Physiol (1985) 2015;118:1075–1083. doi: 10.1152/japplphysiol.00780.2014. [DOI] [PubMed] [Google Scholar]
- 22.Pichiule P, LaManna JC. Angiopoietin-2 and rat brain capillary remodeling during adaptation and deadaptation to prolonged mild hypoxia. J Appl Physiol (1985) 2002;93:1131–1139. doi: 10.1152/japplphysiol.00318.2002. [DOI] [PubMed] [Google Scholar]
- 23.LaManna JC, Chavez JC, Pichiule P. Structural and functional adaptation to hypoxia in the rat brain. J Exp Biol. 2004;207:3163–3169. doi: 10.1242/jeb.00976. [DOI] [PubMed] [Google Scholar]
- 24.Hasbak P, Eskesen K, Schifter S, Edvinsson L. Increased alphaCGRP potency and CGRP-receptor antagonist affinity in isolated hypoxic porcine intramyocardial arteries. Br J Pharmacol. 2005;145:646–655. doi: 10.1038/sj.bjp.0706232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hoiland RL, Bain AR, Rieger MG, Bailey DM, Ainslie PN. Hypoxemia, oxygen content, and the regulation of cerebral blood flow. Am J Physiol Regul Integr Comp Physiol. 2016;310:R398–413. doi: 10.1152/ajpregu.00270.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Manukhina EB, Downey HF, Shi X, Mallet RT. Intermittent hypoxia training protects cerebrovascular function in Alzheimer’s disease. Exp Biol Med (Maywood) 2016;241:1351–1363. doi: 10.1177/1535370216649060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vedam H, Phillips CL, Wang D, Barnes DJ, Hedner JA, Unger G, Grunstein RR. Short-term hypoxia reduces arterial stiffness in healthy men. Eur J Appl Physiol. 2009;105:19–25. doi: 10.1007/s00421-008-0868-6. [DOI] [PubMed] [Google Scholar]
- 28.Burtscher M, Haider T, Domej W, Linser T, Gatterer H, Faulhaber M, Pocecco E, Ehrenburg I, Tkatchuk E, Koch R, Bernardi L. Intermittent hypoxia increases exercise tolerance in patients at risk for or with mild COPD. Respir Physiol Neurobiol. 2009;165:97–103. doi: 10.1016/j.resp.2008.10.012. [DOI] [PubMed] [Google Scholar]
- 29.Kleinman MT, Leaf DA, Kelly E, Caiozzo V, Osann K, O’Niell T. Urban angina in the mountains: effects of carbon monoxide and mild hypoxemia on subjects with chronic stable angina. Arch Environ Health. 1998;53:388–397. doi: 10.1080/00039899809605726. [DOI] [PubMed] [Google Scholar]
- 30.Faulhaber M, Gatterer H, Haider T, Linser T, Netzer N, Burtscher M. Heart rate and blood pressure responses during hypoxic cycles of a 3-week intermittent hypoxia breathing program in patients at risk for or with mild COPD. Int J Chron Obstruct Pulmon Dis. 2015;10:339–345. doi: 10.2147/COPD.S75749. [DOI] [PMC free article] [PubMed] [Google Scholar]


