Abstract
Pertrochanteric hip fractures are among the most common and the use of short cephalomedullary nails as the treatment of choice is increasing.
A systematic review regarding distal locking options for short cephalomedullary nails was undertaken using Medline/PubMed®, Embase® and Cochrane Library® in order to evaluate current indications, associated complications and to provide treatment recommendations.
The results seem to support the use of distal static locking for unstable fractures, dynamic locking for length stable/rotational unstable fractures and no locking for stable fractures.
Complications associated with distal locking include iatrogenic fractures, thigh pain, delayed union and nonunion, implant failure, screw loosening and breaking, drill bit breaking, soft tissue irritation, femoral artery branch injury, intramuscular haematoma and compartment syndrome. It is also associated with longer operative time and radiation exposure.
In unlocked constructs, dorsomedial comminution and nail/medullary canal mismatch contribute to peri-implant fractures. Anterior cortical impingement is associated with cut-out and nonunion.
Most studies comparing distally locked and unlocked nails report a short follow-up.
Distal locking mode should be based on the fracture’s stability.
Cite this article: EFORT Open Rev 2020;5:421-429. DOI: 10.1302/2058-5241.5.190045
Keywords: distal, locked, nail, pertrochanteric, short, trochanteric, unlocked
Introduction
Hip fractures are among the most common fractures in orthopaedics, and are associated with a high social burden and mortality, estimated at approximately 22% at one year.1 The worldwide incidence of hip fractures is estimated at 1.5 million people per year, rising to 2.6 million in 2025 and 6.25 million in 2050, because of the aging population and an increased incidence of osteoporosis.2 Hip fractures (proximal femoral fractures) are classified in accordance with the Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) classification into trochanteric (31A), femoral neck (31B) and femoral head (31C) fractures. Trochanteric fractures are defined as fractures occurring from the extracapsular basilar femoral neck to the region along the lesser trochanter, proximal to the medullary canal, and represent approximately 50% of proximal femoral fractures.3 Trochanteric fractures are further classified into simple pertrochanteric, two-part fractures (31A1), multi-fragmentary pertrochanteric fractures (31A2) and intertrochanteric fractures with a horizontal (reverse oblique) line (31A3) (Table 1).4 A stable fracture, once reduced and fixed is compressed and minimally displaced by weight-bearing. A1 and A2 fractures demonstrate generally stable patterns. Unstable fracture patterns include dorsomedial comminution, basicervical patterns, reverse obliquity patterns and fractures with an incompetent lateral wall and are associated with collapse on axial loading.5,6
Table 1.
Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) classification for trochanteric fractures4
| AO/OTA classification | Description | Distribution2 |
|---|---|---|
| 31A1 (Fig. 1) | Simple pertrochanteric fracture (two part). Considered stable after reduction. | 29% |
| 31A2 (Fig. 2) | Multi-fragmentary pertrochanteric. If lateral wall incompetent ( ≤ 20.5 mm) or if there is dorsomedial comminution, the fracture is considered unstable. | 49% |
| 31A3 (Fig. 3) | Intertrochanteric (reverse obliquity) fracture. The fracture line extends medially from above the lesser trochanter to laterally below the crest of the vastus lateralis. Considered unstable. | 22% |
Fig. 1.
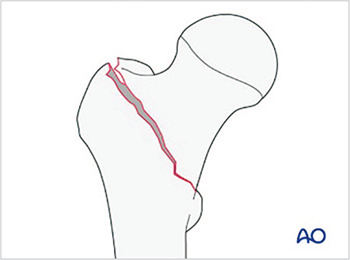
Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) 31A1 pertrochanteric fracture illustration.
Source. AO Surgery Reference, www.aosurgery.org. Copyright by AO Foundation, Switzerland. Used with permission.
Fig. 2.
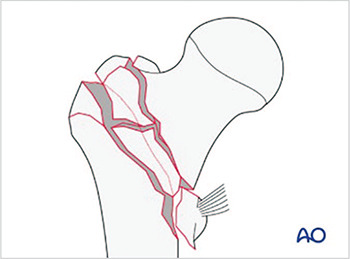
Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) 31A2 pertrochanteric fracture illustration.
Source. AO Surgery Reference, www.aosurgery.org. Copyright by AO Foundation, Switzerland. Used with permission.
Fig. 3.
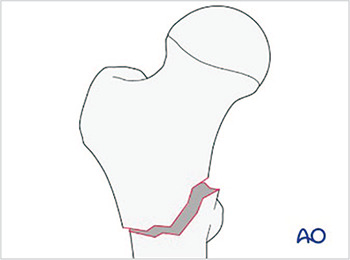
Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) 31A3 intertrochanteric fracture illustration.
Source. AO Surgery Reference, www.aosurgery.org. Copyright by AO Foundation, Switzerland. Used with permission.
The treatment of trochanteric fractures is mainly surgical, with non-operative treatment being reserved for non-ambulatory, severely demented patients with controllable pain or patients with terminal disease.6,7
Several surgical devices are employed for the treatment of trochanteric fractures, including extramedullary devices, of which the dynamic hip screw is the most used; and, more recently, intramedullary devices, namely short and long nails. For unstable trochanteric fractures, intramedullary nailing appears to provide better results compared with extramedullary devices.8–11 As for stable intertrochanteric fractures, there is still debate about the superiority of intramedullary nails compared with dynamic hip screws,3,12,13,14 although intramedullary nails are rising in popularity, going from 3% of usage in 1999 to 67% in 2006.15,16 Intramedullary nails are load-sharing implants that allow early weight-bearing. Short nails are typically used for trochanteric fractures, while long nails are used for subtrochanteric fractures and for some trochanteric fractures with subtrochanteric extent or when protection of the femoral shaft is needed (severe osteoporosis, morbid obesity, metastatic lesions, or suspected femoral pathology).17–21 Different nails have been manufactured, although in a recent review no superiority was found for any model.22,23
Distal locking provides length and rotational stability and restrains the movement of the distal tip of the nail in broad medullary canals. The original Gamma nail (Stryker Ltd, 1980), allows distal locking through two static screws transfixing the nail in two separate holes.22,24 Most recent nails present an oblong hole at the distal tip that can accommodate two screws: a proximal screw for static locking and a distal screw for dynamic locking. Static locking provides a rigid, length stable construct suited for preventing shortening of the limb and displacement of the fracture while dynamic locking allows some compression of the fracture with weight-bearing.12,22,24,25 Initially, a distally locked construct bears most of the load which is gradually transferred to the distal cortex as the fracture heals. With good cortical apposition, most of the compressive load is supported by the bone cortices. Without cortical contact, all of the load is transferred to the distal screw though the nail until the fracture heals or fatigue failure occurs; hence the importance of a stable reduction of the fracture.17,26–28 Furthermore, in stable fractures, rotational stability is provided by lag screws going through the intact lateral femoral cortex.10
The aim of this review is to evaluate the indications and complications of distal locking of short cephalomedullary nails for trochanteric femur fractures and to provide a rational decision-making algorithm.
Methods
A systematic review was undertaken using Medline/PubMed®, Embase ® and Cochrane Library® in the English language, from database inception to June 2019, using the following string of words: (proximal femoral OR trochanteric OR pertrochanteric OR intertrochanteric) AND nail AND (dynamic OR static OR unlocked) AND distal, with no limits specified. A total of 205 records were screened (Medline/PubMed® n = 88, Embase® n = 101, and Cochrane Library® reviews n = 16). After duplicate removal, 149 records remained. Screening for articles referring to the treatment of pertrochanteric fractures in adult human specimens with short nails or associated complications yielded a total of 50 records. Abstracts of articles written in languages other than English were excluded. After full-text assessment, 25 articles were included in the qualitative analysis, (clinical studies n = 17, review articles n = 4, biomechanical studies n = 2, meta-analysis = 1, case-study n = 1).
For the current study, we used the AO/OTA classification of trochanteric fractures as it is the most commonly adopted for research purposes (Table 1).
Results
Biomechanical evidence
Two biomechanical studies have been identified. In order to investigate the origin of fractures at the distal locking site of the original Gamma nail, Lacroix et al subjected 10 human cadaver femora to torsional load until fracture occurred and reported that. with an additional distal screw, the mean failure load in torsion decreased by 35.7%, arguing that ‘additional drill holes should be avoided because they act as stress raisers’.29
Rosenblum et al studied the strain distribution in the proximal femur in 10 human femora loaded under 1800 N with or without distal locking and noticed no change in the pattern of proximal femoral strain with distal locking, suggesting that ‘distal locking screws may not be necessary for stable intertrochanteric fractures’.30
Clinical evidence
Evidence suggests that stress concentration occurs at the nail tip and manifests radiographically by cortical hypertrophy (Fig. 4), in approximately 20% of patients, which is thought to predispose to thigh pain, fractures around the distal tip of the nail and implant breakage.31
Fig. 4.

Radiographic image of distal cortical hypertrophy around the distal medial nail tip.
For stable fracture patterns, less cortical hypertrophy has been reported with dynamically locked nails compared to statically locked, with other outcomes being equal.32,33
Recent reports suggest that stable trochanteric fractures can be treated using distally unlocked nails with good clinical results, as shown in Table 2.10,33–37 The first meta-analysis of this issue, comparing distally locked versus unlocked trochanteric nails in stable fractures, reports significant differences in operation time (standard mean difference (SMD) 0.77, 95% confidence interval (CI) 0.36–1.17), fluoroscopy exposure time (SMD 1.02, 95% CI 0.52–1.52), blood loss (SMD 0.80, 95% CI 0.62–0.99), thigh pain (relative risk (RR) 4.71, 95% CI 2.40–9.21) and total incision length (SMD 1.16, 95% CI 0.86–1.47), with no difference in hip pain, distal tip fracture, lag screw cut-out, nonunion, deep vein thrombosis, wound infection, Harris Hip Score and walking ability.32
Table 2.
Characteristics, results and conclusions of studies published in the last five years comparing distally locked versus unlocked nails in stable pertrochanteric fractures
| Study | Type | N | Follow-up | Locking | Operation time (min) |
Length of incision (cm) | Fluoroscopy time (s) |
Blood loss (mL/Hb) |
Other results | Conclusions | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LG | UG | LG | UG | LG | UG | LG | UG | |||||||
| Yan et al, 202032 | Meta-analysis | 480–800 | 10–18 months | Locked/ Unlocked | – | SMD 0.77 (CI 0.36–1.17) |
– | SMD 1.16 (CI 0.86–1.47) |
– | SMD 1.44 (CI 0.46–2.41) |
– | SMD 0.80 (CI 0.62–0.99) |
– | Locked nails should not be recommended for stable fractures |
| Ciaffa et al, 201833 | RCT | 240 | 12 months | Static/ Dynamic/Unlocked | DG 39.4 ± 4.7 SG 40.1 ± 3.7 |
33.8 ± 6.3 | DG 13.5 ± 2.3 SG 13.8 ± 3.0 |
11.4 ± 2.2 | DG 56.3 ± 7.0 SG 54.2 ± 8.0 |
48.4 ± 3.3 | DG 172.4 ± 38.0 SG 174.2 ± 3.4 |
152.6 ± 43.0 | – | Short nails do not need to be locked |
| Lanzetti et al, 201834 | Cohort study | 143 | 12–19 months | Dynamic/Unlocked | 47.16 ± 13.26 | 31.87 ± 18.26 | – | – | 31.59 | 25.40 | 11.61 ± 1.65 * |
11.08 ± 1.41 * |
– | In stable fractures, the absence of locking does not compromise bone healing and prevents complications |
| Caiaffa et al, 201610 | RCT | 266 | 12 months | Locked/ Unlocked | 41.3 ± 9.5 | 36.6 ± 8.1 | 11.2 ± 1.8 | 8.5 ± 2.1 | 52.0 ± 4.2 | 43.0 ± 3.5 | 185.3 ± 44.6 | 137.6 ± 57.6 | DL associated with greater thigh pain (26.9% LG vs. 5% UG) | Stable fractures can be treated successfully with unlocked nails |
| Li et al, 201535 | RCT | 70 | 12 months | Static/ Unlocked | 48.5 ± 9.0 | 39.2 ± 7.6 | 13.1 ± 2.1 | 10.9 ± 1.7 | 57.8 ± 4.3 | 53.7 ± 3.9 | 194.3 ± 61.6 | 158.6 ± 63.6 | – | Unlocked nails may be an acceptable option for stable fractures |
| López-Vega et al, 201536 | RCT | 177 | 10 months | Dynamic/Unlocked | 41.07 ± 16.42 | 40.06 ± 19.46 | – | – | 31.59 ± 30.34 | 25.40 ± 21.44 | 2.06 ± 0.81** | 2.09 ± 0.92** | More complications in LG: medical (36 vs. 23) biomechanical (5 vs. 14) fracture collapse (5.41 ± 4.51 vs. 3.78 ± 3.39) |
The use of distal locking screw in the Gamma 3 nails should be restricted to unstable fractures |
Note. N, number of cases; LG, locked group; UG, unlocked group; DG, dynamic group; SG, static group; Hb, hemoglobin g/dL; CI, confidence interval (95%); RCT, randomized controlled study; SMD, standardized mean difference.
*postoperative; **variation pre/postoperative.
All the patients presented with AO A1 or A2 fracture patterns.
Complications
The complication rate associated with distal locking has been reported to be as high as 15% with older nails, with the incidence being lower with newer designs.38
Iatrogenic fractures: Peri-implant fractures generally occur around the distal tip of the nail, in approximately 1.1–2.6% of cases. One of the mechanisms suggested to predispose patients to peri-implant fractures is weakening of the cortical bone through excessive distal drilling, which may be caused by a malfunctioning targeting device or incorrect technique.3,39
Thigh pain has been associated with distal locking and is presumably caused by cortical hypertrophy secondary to stress concentration at the distal screw. The reported incidence varies between 1.08% and 12.7%, and is higher with older nail models, if two distal screws are used, if there is a mismatch between the femoral canal and the nail, if there is a mismatch between the nail and the femoral canal, in osteoporotic patients, and if insufficient reaming was performed.40
Vascular injury: Internal rotation and adduction of the leg during trochanteric nailing approximates the femoral artery to the femur ( < 10 mm), predisposing patients to iatrogenic vascular injury.10 Pseudoaneurysms of the femoral artery branches were reported in 0.2% of cases, caused by overpenetration of the drill bit or irritation of the protruding distal locking screw.41,42
Delayed union and nonunion are relatively rare (1–2%) as a result of an excellent blood supply and abundant cancellous bone.43
Other complications have been reported with distally locked constructs, including implant failure (0.2%), screw loosening and breaking, drill bit breaking (0.4%), soft tissue irritation, intramuscular haematoma and compartment syndrome.10,40,44,45,46 Higher radiation exposure for the surgical team is also a factor to consider in distally locked nails.45
Distally unlocked constructs in stable trochanteric fractures are not devoid of complications:
Peri-implant fractures: It has been suggested that distal screws act as stress risers, predisposing patients to fractures around the screw.35,36,46 This notion has been recently challenged in two articles. Skála-Rosenbaum et al conducted an 849-patient prospective study which reported an 85.7% higher risk of peri-implant fracture after unlocked distal nailing of AO 31A1 and A2 fractures relative to locked nailing in dynamic mode. The authors described two fracture patterns related to the distal locking technique, all of which occurred as a low-energy trauma after a fall. Type I fractures occur in the proximal part of the femur, above the tip of the nail during the first postoperative weeks, before fracture healing has occurred. The authors suggest that the cause of instability is a large dorsomedial fragment whose size or comminution may not have been fully appreciated through radiography or secondary fracture lines that occurred during nail insertion. Type II fractures occur at the tip of the nail after bone consolidation has taken place. In 4/6 cases, the nails did not fill the intramedullary cavity completely (Fig. 5). It has been proposed that micromovements at the tip of the unlocked nail weaken the femoral shaft cortex, which predisposes patients to peri-implant fracture.47 Lindvall et al reported similar findings in a study with 171 patients treated using short nails. They reported eight refractures (9.0% at five years), seven of which were in the distally unlocked group, occurring at or distal to the nail tip. The eighth refracture was supracondylar.48 Both studies were observational in nature. To the best of our knowledge, there are no randomized controlled studies comparing the long-term ( > 5 years) refracture rate of distally locked versus unlocked nails.
Anterior cortical impingement of the nail (Fig. 6) is defined as contact between the nail tip and the anterior femoral cortex. Mori et al evaluated 169 stable trochanteric fractures treated using an unlocked intramedullary nail and concluded that the occurrence of cut-out and nonunion appears to be correlated with the presence of anterior cortical impingement, which can be caused by an excessive anterior femoral bow or an incorrect entry point.49 Anterior impingement has also been described in locked nails and although theoretically may be associated with nonunion and peri-implant fractures, it has not yet been proven.50,51,52
Fig. 5.

Radiographic image of a nail/femoral canal mismatch. This nail has been distally locked.
Fig. 6.

Radiographic image of anterior cortical notching of the nail tip.
Discussion
Expert recommendations
Expert opinion is divergent in terms of locking mode. Some authors prefer locking all the nails, regardless of the fracture configuration,17 in static53 or dynamic mode6 while others consider placement of locking screws as optional.40,54,55
Baumgaertner and Fishler describe a distal locking technique that involves evaluating the fracture for length and rotational stability. If the pattern is length stable, then traction is released prior to distal locking and rotational stability is assessed by securing the distal extremity and gently rotating the insertional jig. If the fracture moves as a unit, then distal locking is optional, and if there are doubts about the motion then a single dynamic screw is used. If the pattern is length unstable, two distal screws are placed.56
Recommendations for prevention and management of complications associated with distal locking include:
Iatrogenic fractures: Replacing or repairing the targeting device each 30–40 surgical acts.57 Incorrect incision of the fascia may force the targeting device off the distal locking hole. If the first drilling attempt is unsuccessful, it is recommended to drill the second hole.25 Excessive reaming, excessive tightening of the screw and eccentric screw insertion may also predispose patients to fracture.41
Thigh pain: The pain usually resolves with dynamization of the nail or removal of the implant.40
Vascular injury: To prevent this complication, the drill must not be pushed further once the second cortex is breached.40 Release of the traction and return of the limb to a neutral position is recommended after inserting the lag screw.3
Delayed union and nonunion: Locking a nail in distraction of the two main fragments should be avoided as it predisposes the patient to impaired healing and fatigue break of the nail.38
Recommendations for prevention and management of complications associated with unlocked constructs include:
Anterior cortical impingement of the nail: A method of preventing this complication is by avoiding posterior starting points.50
Algorithm
Given the lack of consensus regarding distal locking options and after reviewing the available literature, the authors present the following decision algorithm regarding distal locking of short trochanteric nails.
The algorithm is based on the Baumgaertner and Fishler technique published in 2013,56 with the main differences being:
The recommendation for insertion of a single static screw instead of two, to prevent stress concentration, cortical weakening and thigh pain.32,57
The recommendation to distally lock the nails in patients with a wide intramedullary canal, intraoperative fractures and large dorsomedial comminution to avoid secondary fractures, even in stable fracture patterns.47
Acknowledgement of the recent articles reporting good clinical results with distally unlocked nails, in fractures with confirmed stability and none of the risk factors presented above.10,33–37
Graphical representation of the algorithm (Fig. 7).
Fig. 7.
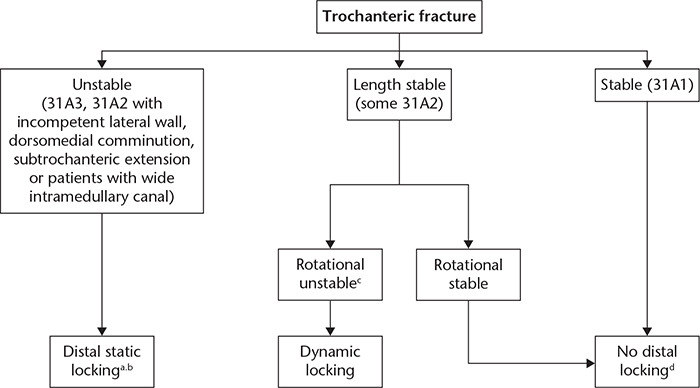
Distal locking algorithm for treatment of pertrochanteric fractures with short cephalomedullary nails.
- a) A long nail may be considered in case of subtrochanteric extension or for protection of the femoral shaft (in case of severe osteoporosis, metastatic lesions, or suspected femoral pathology).
- b) Consider using a single static screw instead of two static screws as it may prevent stress concentration and thigh pain.
- c) A method of detecting rotational instability is by gently rotating the insertional jig after inserting the lag screw. If the fragments move as a unit, the fracture is treated as stable.
- d) Consider an extramedullary device as a viable alternative in stable fractures.
Unstable fractures (31A3 and some 31A2)
In fractures with a 31A3 pattern, the diaphyseal fragment may rotate if the nail is unlocked, causing malrotation of the limb.38 Additional unstable fracture patterns that benefit from locked nailing include fractures with an incompetent lateral wall, severe dorsomedial comminution, subtrochanteric extension and a wide intramedullary canal.6,52,54
Little evidence is available comparing static and dynamic locking modes in unstable fracture patterns. Some authors advocate static mode to prevent fracture displacement and leg shortening,3,36,41,43,51 while others prefer distal locking in dynamic mode arguing that it reduces distal cortical hypertrophy, thigh pain, and fracture risk and allows compression of the fracture with load-bearing.6,32,34,35,38,46,47
Some authors argue that long cephalomedullary nails should be considered in fractures with subtrochanteric extension or for protection of the femoral shaft (in case of severe osteoporosis, metastatic lesions, or suspected femoral pathology).6,43
Length stable fractures (some 31A2)
According to the Baumgaertner and Fishler technique, presented above, in length stable fractures, after reduction and placement of the lag screw, if the fragments move as a unit by rotating the insertional jig, locking is optional, otherwise a distal screw is placed in dynamic mode.55
Testing the rotational stability of the construct may help to differentiate between stable and unstable 31A2 fractures and avoid Type I fractures described by Skála-Rosenbaum et al.47
In the presented algorithm, if a 31A2 fracture is length stable after reduction and rotational stability is confirmed, the fracture is treated as stable.
Most authors do not differentiate length from rotational instability when making recommendations relative to the distal locking mode. As such, we see no reason to deviate from Baumgaertner and Fishler’s recommendation to statically lock length unstable fractures and dynamically lock rotational unstable fractures.
Stable fractures (31A1)
Biomechanical29,30 and clinical evidence10,33–37 supports the use of unlocked constructs in stable pertrochanteric fractures. Yan et al conducted the first meta-analysis on the issue and recommended against the use of distally locked intramedullary nails as a routine choice in stable trochanteric fractures.33
It should be noted that not all patients with stable fracture patterns are eligible for distally unlocked nails. Patients with large intramedullary canals, iatrogenic intraoperative fractures or large dorsomedial fragments or comminution should be treated using locked intramedullary nails regardless of the fracture pattern to avoid secondary fractures.47 Further studies are needed to evaluate the long-term results of distally unlocked nails.
Anterior cortical impingement of the nail tip should be avoided.50
Extramedullary devices, namely dynamic hip screws, can also be considered as a viable alternative for stable trochanteric fracture fixation.3,12,13
Conclusions
The current review presents an instructional decision-making algorithm based on current literature. Distal locking should be used in unstable fractures, static locking is typically used in length unstable fractures, dynamic locking in rotationally unstable fractures and, according to recent evidence, no locking is needed for stable pertrochanteric fractures. Further studies are needed to evaluate clinical results, additional risk factors for implant failure and long-term patient recovery. The present algorithm should be used as a general guideline. The decision on distal locking mode should be based on the surgeon’s best judgment and tailored to each individual. This algorithm may become outdated as new evidence emerges.
Footnotes
ICMJE Conflict of interest statement: The authors declare no conflict of interest relevant to this work.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Downey C, Kelly M, Quinlan JF. Changing trends in the mortality rate at 1-year post hip fracture: a systematic review. World J Orthop 2019;10:166–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mattisson L, Bojan A, Enocson A. Epidemiology, treatment and mortality of trochanteric and subtrochanteric hip fractures: data from the Swedish fracture register. BMC Musculoskelet Disord 2018;19:369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mavrogenis AF, Panagopoulos GN, Megaloikonomos PD, et al. Complications after hip nailing for fractures. Orthopedics 2016;39:e108–e116. [DOI] [PubMed] [Google Scholar]
- 4. Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF. Fracture and dislocation classification compendium-2018. J Orthop Trauma 2018;32:S1–S170. [DOI] [PubMed] [Google Scholar]
- 5. Socci AR, Casemyr NE, Leslie MP, Baumgaertner MR. Implant options for the treatment of intertrochanteric fractures of the hip: rationale, evidence, and recommendations. Bone Joint J 2017;99-B:128–133. [DOI] [PubMed] [Google Scholar]
- 6. Russell TA. Intertrochanteric fractures of the hip. In: Court-Brown CM, ed. Rockwood and Green’s fractures in adults. Eighth ed Philadelphia: Wolters Kluwer Health, 2015:2076–2129. [Google Scholar]
- 7. Kawaji H, Uematsu T, Oba R, Takai S. Conservative treatment for fracture of the proximal femur with complications. J Nippon Med Sch 2016;83:2–5. [DOI] [PubMed] [Google Scholar]
- 8. Zhu Q, Xu X, Yang X, et al. Intramedullary nails versus sliding hip screws for AO/OTA 31-A2 trochanteric fractures in adults: a meta-analysis. Int J Surg 2017;43:67–74. [DOI] [PubMed] [Google Scholar]
- 9. Kregor PJ, Obremskey WT, Kreder HJ, Swiontkowski MF. Unstable pertrochanteric femoral fractures. J Orthop Trauma 2014;28:S25–S28. [DOI] [PubMed] [Google Scholar]
- 10. Caiaffa V, Vicenti G, Mori C, et al. Is distal locking with short intramedullary nails necessary in stable pertrochanteric fractures? A prospective, multicentre, randomised study. Injury 2016;47:S98–S106. [DOI] [PubMed] [Google Scholar]
- 11. Yu X, Wang H, Duan X, Liu M, Xiang Z. Intramedullary versus extramedullary internal fixation for unstable intertrochanteric fracture, a meta-analysis. Acta Orthop Traumatol Turc 2018;52:299–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Parker MJ, Handoll HH. Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures in adults. Cochrane Database Syst Rev 2010;9:CD000093. [DOI] [PubMed] [Google Scholar]
- 13. National Institute for Health and Care Excellence. Hip fracture: management, 2017. https://www.nice.org.uk/guidance/cg124/chapter/Recommendations (date last accessed 24 June 2019). [PubMed]
- 14. Ramos PL, Seral B, Beano A, et al. Fractures of the proximal femur: the Gamma nail versus plate. Osteosynth Trauma Care 2005;13:18–25 [Google Scholar]
- 15. Anglen JO, Weinstein JN; American Board of Orthopaedic Surgery Research Committee. Nail or plate fixation of intertrochanteric hip fractures: changing pattern of practice. A review of the American Board of Orthopaedic Surgery Database. J Bone Joint Surg Am 2008;90:700–707. [DOI] [PubMed] [Google Scholar]
- 16. Niu E, Yang A, Harris AHS, Bishop J. Which fixation device is preferred for surgical treatment of intertrochanteric hip fractures in the united states? A survey of orthopaedic surgeons. Clin Orthop Relat Res 2015;473:3647–3655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Maniar HH, Tawari AA, Mookerjee G, Horwitz DS, Mookerjee, Gaurav BA, Horwitz DS. Short or long, locked or unlocked nails for intertrochanteric fractures. Tech Orthop 2015;30:87–96. [Google Scholar]
- 18. Joglekar SB, Lindvall EM, Martirosian A. Contemporary management of subtrochanteric fractures. Orthop Clin North Am 2015;46:21–35. [DOI] [PubMed] [Google Scholar]
- 19. Konstantinidis L, Helwig P, Hirschmüller A, Langenmair E, Südkamp NP, Augat P. When is the stability of a fracture fixation limited by osteoporotic bone? Injury 2016;47:S27–S32. [DOI] [PubMed] [Google Scholar]
- 20. Adam P. Treatment of recent trochanteric fracture in adults. Orthop Traumatol Surg Res 2014;100:S75–S83. [DOI] [PubMed] [Google Scholar]
- 21. Roberts KC, Brox WT, Jevsevar DS, Sevarino K. Management of hip fractures in the elderly. J Am Acad Orthop Surg 2015;23:131–137. [DOI] [PubMed] [Google Scholar]
- 22. Queally JM, Harris E, Handoll HH, Parker MJ. Intramedullary nails for extracapsular hip fractures in adults. [Review]. Cochrane Database Syst Rev 2014;9:CD004961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nyholm AM, Palm H, Malchau H, Troelsen A, Gromov K. Lacking evidence for performance of implants used for proximal femoral fractures: a systematic review. Injury 2016;47:586–594. [DOI] [PubMed] [Google Scholar]
- 24. Hardy DC, Descamps PY, Krallis P, et al. Use of an intramedullary hip-screw compared with a compression hip-screw with a plate for intertrochanteric femoral fractures: a prospective, randomized study of one hundred patients. J Bone Joint Surg Am 1998;80:618–630. [DOI] [PubMed] [Google Scholar]
- 25. Skála-Rosenbaum J, Bartonícek J, Bartoška R. Is distal locking with IMHN necessary in every pertrochanteric fracture? Int Orthop 2010;34:1041–1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Carr JB. The anterior and medial reduction of intertrochanteric fractures: a simple method to obtain a stable reduction. J Orthop Trauma 2007;21:485–489. [DOI] [PubMed] [Google Scholar]
- 27. Guerado E, Bertrand ML. Malalignment in intramedullary nailing: how to achieve and to maintain correct reduction? Injury 2017;48:S30–S34. [DOI] [PubMed] [Google Scholar]
- 28. Koyuncu Ş, Altay T, Kayalı C, Ozan F, Yamak K. Mechanical failures after fixation with proximal femoral nail and risk factors. Clin Interv Aging 2015;10:1959–1965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lacroix H, Arwert H, Snijders CJ, Fontijne WP. Prevention of fracture at the distal locking site of the Gamma nail: a biomechanical study. J Bone Joint Surg Br 1995;77:274–276. [PubMed] [Google Scholar]
- 30. Rosenblum SF, Zuckerman JD, Kummer FJ, Tam BS. A biomechanical evaluation of the Gamma nail. J Bone Joint Surg Br 1992;74:352–357. [DOI] [PubMed] [Google Scholar]
- 31. Lanzetti RM, Caraffa A, Lupariello D, et al. Comparison between locked and unlocked intramedullary nails in intertrochanteric fractures. Eur J Orthop Surg Traumatol 2018;28:649–658. [DOI] [PubMed] [Google Scholar]
- 32. Hardy DC, Drossos K. Slotted intramedullary hip screw nails reduce proximal mechanical unloading. Clin Orthop Relat Res 2003;406:176–184. [DOI] [PubMed] [Google Scholar]
- 33. Yan WS, Cao WL, Sun M, Ma DY, Zhang P. Distal locked or unlocked nailing for stable intertrochanteric fractures? A meta-analysis. ANZ J Surg 2020;90:27-33. Epub 2019. May 13 (date last accessed 24 June 2019). [DOI] [PubMed] [Google Scholar]
- 34. Ciaffa V, Vicenti G, Mori CM, et al. Unlocked versus dynamic and static distal locked femoral nails in stable and unstable intertrochanteric fractures: a prospective study. Injury 2018;49:S19–S25. [DOI] [PubMed] [Google Scholar]
- 35. Lanzetti RM, Caraffa A, Lupariello D, et al. Comparison between locked and unlocked intramedullary nails in intertrochanteric fractures. Eur J Orthop Surg Traumatol 2018;28:649–658. [DOI] [PubMed] [Google Scholar]
- 36. Li X, Zhang L, Hou Z, et al. Distal locked and unlocked nailing for perthrochanteric fractures: a prospective comparative randomized study. Int Orthop 2015;39:1645–1652. [DOI] [PubMed] [Google Scholar]
- 37. López-Vega M, Gil-Monzó ER, Rodrigo-Pérez JL, et al. [Randomized prospective study on the influence distal block and Gamma 3 nail on the treatment of intertrochanteric fractures of femur]. Rev Esp Cir Ortop Traumatol 2015;59:26–35. [DOI] [PubMed] [Google Scholar]
- 38. Bartoníček J. Musculoskeletal key 2016: complications of trochanteric fractures. https://musculoskeletalkey.com/complications-of-trochanteric-fractures/ (date last accessed 24 June 2019).
- 39. Norris R, Bhattacharjee D, Parker MJ. Occurrence of secondary fracture around intramedullary nails used for trochanteric hip fractures: a systematic review of 13,568 patients. Injury 2012;43:706–711. [DOI] [PubMed] [Google Scholar]
- 40. Shen WY. Complications with the Gamma nail and long Gamma nail, and their prevention. Osteosynth Trauma Care 2005;13:34–41. [Google Scholar]
- 41. Gong J, Liu P, Cai M. Imaging evaluation of the safe region for distal locking screw of proximal femoral nail anti-rotation in patients with proximal femoral fracture. Med Sci Monit 2017;23:719–724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Segal D, Yaacobi E, Marom N, et al. The incidence of life threatening iatrogenic vessel injury following closed or open reduction and internal fixation of intertrochanteric femoral factures. Int Orthop 2017;41:1845–1850. [DOI] [PubMed] [Google Scholar]
- 43. Kanakaris NK, Tosounidis TH, Giannoudis PV. Nailing intertrochanteric hip fractures: short versus long; locked versus nonlocked. J Orthop Trauma 2015;29:S10–S16. [DOI] [PubMed] [Google Scholar]
- 44. Kukla C, Heinz T, Gaebler C, Heinze G, Vécsei V. The standard Gamma nail: a critical analysis of 1,000 cases. J Trauma 2001;51:77–83. [DOI] [PubMed] [Google Scholar]
- 45. Rashid MS, Aziz S, Haydar S, Fleming SS, Datta A. Intra-operative fluoroscopic radiation exposure in orthopaedic trauma theatre. Eur J Orthop Surg Traumatol 2018;28:9–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ozkan K, Unay K, Demircay C, Cakir M, Eceviz E. Distal unlocked proximal femoral intramedullary nailing for intertrochanteric femur fractures. Int Orthop 2009;33:1397–1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Skála-Rosenbaum J, Džupa V, Bartoška R, Douša P, Waldauf P, Krbec M. Distal locking in short hip nails: cause or prevention of peri-implant fractures? Injury 2016;47:887–892. [DOI] [PubMed] [Google Scholar]
- 48. Lindvall E, Ghaffar S, Martirosian A, Husak L. Short versus long intramedullary nails in the treatment of pertrochanteric hip fractures: incidence of ipsilateral fractures and costs associated with each implant. J Orthop Trauma 2016;30:119–124. [DOI] [PubMed] [Google Scholar]
- 49. Mori CM, Vicenti G, Carrozzo M, et al. The fake unlocked femoral nail: a configuration to avoid in stable pertrochanteric femur fractures. Injury 2018;49:S32–S36. [DOI] [PubMed] [Google Scholar]
- 50. Roberts JW, Libet LA, Wolinsky PR. Who is in danger? Impingement and penetration of the anterior cortex of the distal femur during intramedullary nailing of proximal femur fractures: preoperatively measurable risk factors. J Trauma Acute Care Surg 2012;73:249–254. [DOI] [PubMed] [Google Scholar]
- 51. Peña OR, Gómez Gélvez A, Espinosa KA. Clinical implications of impingement of the anterior femoral cortex after cephalomedullary nailing. Injury 2016;47:2300–2306. [DOI] [PubMed] [Google Scholar]
- 52. Maniscalco P, Rivera F, D’Ascola J, Del Vecchio EO. Failure of intertrochanteric nailing due to distal nail jamming. J Orthop Traumatol 2013;14:71–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Simmermacher RKJ. Femur and periprosthetic fractures. In: Buckley RE, ed. AO principles of fracture management. Third ed New York: Thieme, 2017:773–814. [Google Scholar]
- 54. Weinlein JC. Fractures and dislocations of the hip. In: Azar FM, ed. Campbell’s operative orthopaedics. Thirteenth ed Philadelphia: Elsevier, 2017:2817–2864. [Google Scholar]
- 55. Hak DJ, Mauffrey C. Femoral and hip injuries. In: Miller MD, ed. Miller’s review of orthopaedics. Seventh ed Philadelphia: Elsevier, 2016:807–813. [Google Scholar]
- 56. Baumgaertner MR, Fishler T. Intertrochanteric hip fractures: intramedullary hip screws. In: Morrey BF, ed. Master techniques in orthopaedic surgery – fractures. Third ed Philadelphia: Wolters Kluwer Health, 2013:686–714. [Google Scholar]
- 57. Pascarella R, Fantasia R, Maresca A, et al. How evolution of the nailing system improves results and reduces orthopedic complications: more than 2000 cases of trochanteric fractures treated with the Gamma Nail System. Musculoskelet Surg 2016;100:1–8. [DOI] [PubMed] [Google Scholar]


