The emergence of coronavirus disease 2019 (COVID-19) has significantly affected orthopaedic residency training and education throughout the world1. Elective orthopaedic procedures have been halted to preserve resources including personnel, personal protective equipment (PPE), ventilators and to maximize inpatient capacity for patients who have fallen ill with the virus. Outpatient visits have been replaced with telemedicine to comply with the state and federal recommendations to socially distance and stay at home. In New York City, the current epicenter of the COVID-19 pandemic in the United States, doctors, nurses, and healthcare workers are being repurposed in healthcare systems to meet the inundation of critical cases. Although the orthopaedic resident skill set is multifaceted and versatile, this does not typically include extensive experience in the intensive care unit (ICU) management of intubated patients afflicted with pneumonia and acute respiratory distress syndrome (ARDS). However, there are ways for orthopaedic residents to support their colleagues and make a difference in these unprecedented times. At our institution, orthopaedic residents, under the guidance of attending orthopaedic and critical care faculty, designed a multidisciplinary prone positioning (PP) team to assist with intubated patients. Our purpose is to describe the experience and prone team protocol of one institution in the current epicenter of the COVID-19 outbreak in the United States, with the hope that orthopaedic residencies at other institutions may adopt similar initiatives.
Discussion
As of April 20, 2020, New York State had 247,215 confirmed cases and 18,298 deaths and remains the current epicenter of the COVID-19 pandemic in the United States. In such a unique situation, it is important that orthopaedists think outside the realms of their specialized practice and become an “activated surgeon” to battle this virus2. The orthopaedic patient census at most hospitals has dwindled, and ancillary orthopaedic staff have been reappropriated to COVID-19-specialized units. Some orthopaedic departments are offloading the emergency department by tending to all musculoskeletal complaints so emergency medicine teams can deal directly with COVID-19 patients. Others are establishing and repurposing urgent care centers for all non-COVID-related complaints. At our institution, we elected to actively assist in the care of patients with COVID-19 by forming a voluntary and “prone team” for intubated patients to help alleviate the strain on ICU personnel.
COVID-19 attacks the respiratory system, leading to airway inflammation and progression to ARDS with alarming regularity in the elderly patient and those with preexisting medical comorbidities. These patients often require endotracheal intubation for adequate ventilatory support in an ICU setting. Because the optimal treatments of COVID-19 are still largely unknown, intensivists are using the principles from the treatment of other respiratory diseases and causes of ARDS, such as positive end-expiratory pressure (PEEP) management, to prevent these patients from deteriorating and dying due to this illness. Previous ARDS research has shown that PP can help improve alveolar recruitment in patients who remain hypoxemic despite PEEP optimization3. Positioning the ventilated patient prone has been found to improve perfusion and aeration of dorsal alveoli, enhance recruitment of lung tissue, and prevent ventilator-induced lung injury. One multicenter, randomized controlled trial (Proning Severe ARDS Patients {PROSEVA}) demonstrated a 50% reduction in a 28-day mortality using a PP protocol4. Consistent use of PP requires cooperation from a multidisciplinary team to be safe and effective for the ventilated patient. To that end, it is critical to have experienced and trained medical staff who are familiar with the process of PP to avoid complications such as loss of vascular access points, pressure ulcer formation in dependent regions, and the loss of endotracheal airway access.
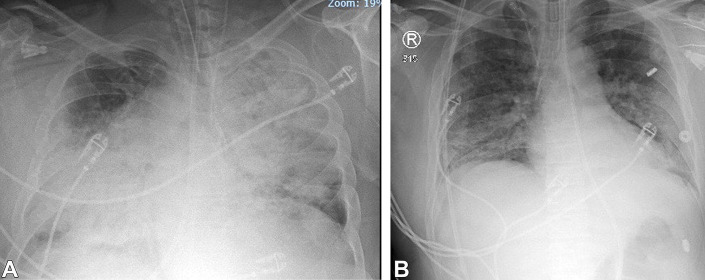
Orthopaedic surgeons are familiar with positioning intubated patients, specifically in the use of PP in spine surgery and lateral decubitus positioning in hip arthroplasty, shoulder arthroscopy, and elbow procedures. Orthopaedic surgeons are comfortable padding pressure-sensitive areas and appropriate head, neck, and arm positioning to prevent iatrogenic nerve palsies. PP, especially with larger body habitus, requires physical strength and endurance in the hospital setting. A dedicated PP team can effectively offload other frontline healthcare professionals, reducing burnout and allowing them to focus on critical care. Along with concurrent intensive care interventions, PP has been used for 16 to 18 hours a day to help improve aeration and perfusion based on interval chest radiographs and overall patient progress (Fig. 1). Because of its early success in treating patients with COVID-19, PP has become a daily routine in the ICU at our institution but requires a trained team of 5 medical personnel for each patient. This is a tall order to accomplish with an ICU functioning at above-maximum patient capacity along with overworked medical staff. To that end, the orthopaedics department has volunteered to provide the staff to the ICU team and has established a PP protocol.
Fig. 1.
Interval posteroanterior (PA) chest radiographs 48 hours apart of an intubated COVID-19+ patient before (Fig. 1-A) and after (Fig. 1-B) prone positioning.
Prone Positioning Protocol
Exposure to patients with COVID-19 is a high-risk endeavor; therefore, access to appropriate PPE is essential. Team members are to wear a surgical hat, one N95 respirator mask, one surgical mask overlying the N95, and one face shield. Once donned, the face area should not be touched until the end of the session. Similar to the operating room protocol, 2 pairs of gloves should be worn by each team member. The first pair of gloves is placed, followed by the disposable gown, followed by the second set of gloves. The gown and top pair of gloves are to be doffed in each patient room and discarded after the turning of the patient. The undergloves should be worn throughout the session and should be cleaned with antimicrobial sanitizer before leaving each room. After exiting the patient's room, the undergloves are immediately discarded and hands are washed thoroughly with soap and warm water.
Outlined in Appendix 1 is the PP protocol that was designed by our Departments of Orthopaedic Surgery and Critical Care Medicine. To increase the efficiency of PP sessions, the necessary materials are gathered before entering the patient room (Table I). This ensures minimal airborne and contact exposure and maximizes PP efficiency. Alternatively, one team member wearing appropriate PPE can enter in advance to the rest of the team and indicate any supplies that are needed. This helps limit the waste of PPE and reduce the number of entrances/exits into the patient room.
TABLE I.
Items Needed Before Prone Positioning
| • Electrocardiography lead pads |
| • 4 Pillows (chest/shoulder, pelvis, knees, feet) |
| • Line caps |
| • Sage Prevalon AirTAP (Stryker). Alternative: chux pads |
| • 5 Team members: intensivist or respiratory therapist at the head of the bed, 2 assistants on each side of the patient. Alternative: 1 assistant can be used on each side depending on body habitus |
This protocol is typically performed in 2 “sessions” per day, with PP of patients in the afternoon and “deproning” or “supining” of the patients in the morning. Before the afternoon sessions, the ICU team determines which intubated patients would benefit from a period of PP and communicates that to the PP team. All patients are then turned by the team according to the protocol. After a period of 16 to 18 hours, any patients who were positioned prone the day before are then repositioned supine the following morning. The protocol for “deproning” patients is very similar, with a few minor adjustments. Pillows are not needed to pad the torso, and the head should be resupported with a pillow when the patient is lying supine. All other steps are readily applicable when turning a patient from prone to supine position.
Post intervention, all disposable PPE should be discarded in each patient's room as outlined. In between sessions, the face shield should be sanitized with a bleach or chlorhexidine germicidal wipe and the N95 should be examined for any deficiencies. The overlying surgical mask should be discarded after each session. If in proper condition, both the face shield and N95 should be kept for future use because of current short supply. Immediately after the entire shift, personal self-decontamination should be performed, including but not limited to thorough hand washing, changing of surgical scrubs, and cleaning of personal items (cell phone, hospital identification card, etc.) with disinfectant wipes. We also recommend body shower immediately after a shift at least once per day at the hospital.
To help mitigate issues with exposure, we have created a shift schedule to limit repeated high exposure levels to the team members. There are 2 teams for the morning and 2 for the afternoon shifts, and participants are limited to a maximum of one shift per day. Diagnostic testing is readily available for our participants. It is also important to stress that participation at our institution remains completely voluntary. The health risks associated with high personal exposure levels and possible transmission of this virus to vulnerable family members and close contacts are not lost on the team members.
Conclusions
Prone positioning is one of many opportunities for orthopaedic surgeons to assist in the COVID-19 pandemic. Although certainly a high risk endeavor, PP is familiar to orthopaedists and can help offload this physical burden from our medical colleagues who are increasingly becoming physically and mentally fatigued. In our experience, this intervention has also helped boost morale and create the sense of a unified front because all healthcare workers move increasingly out of their typical scope of care to assist both patients and colleagues in need.
The COVID-19 pandemic is an unprecedented time for healthcare. It is important for orthopaedic surgeons to take initiative and participate in the frontlines of this pandemic. We recognize that not every institution may possess the resources to institute this protocol. For those that do, this is a model that we have found successful, effective, and quickly deployable. At first glance, a lethal respiratory virus such as COVID-19 may seem like a foe that an orthopaedist is ill-equipped to combat. But in a time of medical crisis, we must view ourselves not as orthopaedic surgeons but as medical doctors who are willing to use any and all of our skills to help those in need.
Appendix
Supporting material provided by the authors is posted with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJSOA/A165).
Acknowledgments
Note: We would like to acknowledge the critical care team at Lenox Hill Hospital including the intensivists, respiratory therapists, ICU nursing staff, and physical therapists for their tireless dedication. We would also like to individually acknowledge our colleagues in the Department of Orthopaedic Surgery for their efforts: Marcel Bas MD, Meghan Bishop MD, Matthew Caid DO, Kristofer Chenard MD, Connor Cole PA, Sameh Elguizaoui MD, Jay Emlen DPM, Gregory Galano MD, Eric Grossman MD, Mikail Koroma MD, Gabrielle Laurenti DPM, Garrett Leonard MD, Frank Mota MD, Brandon Naylor DO, David Nigen MD, Anthony Romeo MD, Andrew Sawires MD, Karen Schneider MD, Bradley Smith MD, Trevor Stubbs MD, Rupesh Tarwala MD, and Michelle Yoon MD.
Footnotes
Investigation performed at Lenox Hill Hospital-Northwell Health, New York, New York
Disclosure: The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A164).
References
- 1.Gray CF, Parvataneni HK, Bozic KJ. Value-based healthcare. Clin Orthop Relat Res. 2020;478(5):954-957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chang Liang Z, Wang W, Murphy D, Po Hui JH. Novel coronavirus and orthopaedic surgery. J Bone Joint Surg. 2020;102(9):745-749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Narendra DK, Hess DR, Sessler CN, Belete HM, Guntupalli KK, Khusid F, Carpati CM, Astiz ME, Raoof S. Update in management of severe hypoxemic respiratory failure. Chest. 2017;152(4):867-879. [DOI] [PubMed] [Google Scholar]
- 4.Guérin C, Reignier J, Richard JC, Beuret P, Gacouin A, Boulain T, Mercier E, Badet M, Mercat A, Baudin O, Clavel M, Chatellier D, Jaber S, Rosselli S, Mancebo J, Sirodot M, Hilbert G, Bengler C, Richecoeur J, Gainnier M, Bayle F, Bourdin G, Leray V, Girard R, Ayzac L, PROSEVA Study Group. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368(23):2159-2168. [DOI] [PubMed] [Google Scholar]