Abstract
The absence of a clinically relevant animal model addressing the typical immune characteristics of hepatocellular cancer (HCC) has significantly impeded elucidation of the underlying mechanisms and development of innovative immunotherapeutic strategies. To develop an ideal animal model recapitulating human HCC, immunocompetent male C57BL/6J mice first receive a carbon tetrachloride (CCl4) injection to induce liver fibrosis, then receive histologically-normal oncogenic hepatocytes from young male SV40 T antigen (TAg)-transgenic mice (MTD2) by intrasplenic (ISPL) inoculation. Androgen generated in recipient male mice at puberty initiates TAg expression under control of a liver-specific promoter. As a result, the transferred hepatocytes become cancer cells and form tumor masses in the setting of liver fibrosis/cirrhosis. This novel model mimics human HCC initiation and progression in the context of liver fibrosis/cirrhosis and reflects the most typical features of human HCC including immune dysfunction.
Keywords: hepatocellular cancer, tumor model, mouse, murine model, liver fibrosis, cancer
Introduction
Hepatocellular cancer (HCC) is the most rapidly increasing type of cancer in the United States (US)1,2,3. Every year, approximately 850,000 new cases are diagnosed4,5 and 700,000 patients die from this lethal disease6,7,8,9,10, making it the second-highest cause of cancer-related death worldwide. Management of HCC includes surgical resection, transplantation, ablation, chemoembolization, or systemic therapies, such as sorafenib11. Early diagnosis and management with surgical resection or transplantation have the highest overall survival benefit4. Unfortunately, the majority of patients present at a later stage and require management with ablation, chemoembolization or sorafenib12. Sorafenib, a receptor tyrosine kinase inhibitor (RTKI), was approved by the Food and Drug Administration in 2008 as the only systemic drug therapy available for treating unresectable HCC. Although the drug only provides a modest increase in overall survival, from 7.9 to 10.7 months13, it provided a new therapeutic strategy that could be utilized to manage HCC.
Manipulating the immune system to eliminate established cancers is a rapidly growing field in cancer research14. Immune checkpoint studies have considerably advanced immunotherapeutic drug development in cancer treatment15,16. The FDA approved the use of antibodies (Abs) against cytotoxic T-lymphocyte antigen 4 (CTLA-4), programmed cell death protein 1 (PD-1), and its ligand PD-L1 for the treatment of melanoma, lung cancer, head and neck cancer, and bladder cancer17,18,19,20. Clinical trials of monotherapy or combination therapy using one or multiple antibodies against PD-1, PD-L1, or CTLA-4 for the treatment of advanced HCC are ongoing21,22,23, and some trials have shown favorable results. In 2017, the FDA granted accelerated approval for anti-PD-1 antibody to treat HCC patients, who are resistance to sorafenib, but the overall response rate of this therapy is only 14.3%. Other strategies have not been translated into clinical practice at this time24,25. Overcoming tumor-induced profound immune tolerance to improve immune checkpoint therapy26; predicting efficacy of immune checkpoint therapy; preventing immune-related adverse events; optimizing administration route, dosage, and frequency; and finding effective combinations of therapies27,28,29 all remain extremely challenging tasks.
There are several conventional approaches used to induce HCC in mouse models currently and are utilized depending on the investigator’s particular research question30. Chemically-induced HCC mouse models with genotoxic compounds mimic injury-induced malignancy. Xenograft models through either ectopic or orthotopic implantation of HCC cell lines are suitable for drug screening. A number of genetically modified mice have been engineered to investigate the pathophysiology of HCC. Transgenic mice expressing viral genes, oncogenes and/or growth factors allow the identification of pathways involved in hepatocarcinogenesis. Due to inherent limitations, these models do not recapitulate the typical immune characteristics seen in human HCC, which has significantly impeded elucidation of the underlying mechanisms and development of innovative immunotherapeutic strategies14,15. We recently created a clinically relevant murine model. This novel model not only mimics human HCC initiation and progression but also reflects most typical features of human disease including immune dysfunction. We have characterized its biological and immunological characteristics. Leveraging this novel model, we have explored various immunotherapeutic strategies to treat HCC31,32,33,34,35,36,37. This unique platform allows us to study mechanisms of tumor-induced immunotolerance and to develop proof-of-concept therapeutic strategies for HCC toward eventual clinical translation.
Protocol
NOTE: All the procedure including animal subjects have been approved by the IACUC at the University of Missouri. All mice received humane care according to the criteria outlined in the “Guide for the Care and Use of Laboratory Animals”. The following procedure for cell isolation and inoculation should be performed in a hood. All performers should wear the standard personal protective equipment for handling of the mice and tissue.
1. Induction of Liver Fibrosis and Cirrhosis with IP Injection of Carbon Tetrachloride (CCl4)
NOTE: See Figure 1. (CCl4 is highly hazardous reagent, it should be handled carefully and with wearing chemical-resistant gloves)
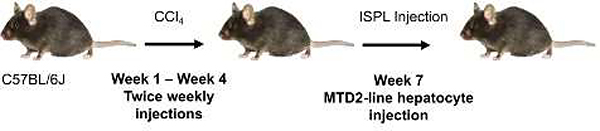
Figure 1: Schematic for preparing mouse model of HCC.
The experimental design for establishing an innovative murine model of HCC. C57BL/6J mice are first treated with IP injection of CCl4 twice weekly for four weeks to induce liver fibrosis. Two weeks following the last IP injection, the CCl4-treated mice receive hepatocytes isolated from young male MTD2 mice via ISPL inoculation. Please click here to view a larger version of this figure.
Obtain male C57BL/6J mice that are six to eight weeks old (see Table of Materials).
Prepare 10% CCl4 (v/v) solution in corn oil in a centrifuge tube. Determine total volume based on number of mice to be injected (see step 1.6).
Use appropriate mice handling technique to select one mouse for injection.
Manually restrain the mouse with its dorsal (abdomen) side up.
Clean the injection site on abdominal wall of the mouse by scrubbing with 70% alcohol.
Inject male C57BL/6J mice with 160 μL of 10% CCl4 solution by intraperitoneal (IP) injection using a 25-gauge disposable needle.
Ensure that the needle penetrates just through the abdominal wall (approximately 4–5 mm) with bevel-side up and slightly angled at 15–20 degrees.
-
Inject mice twice a week for a total of four weeks-each mouse will receive a total of eight injections.
NOTE: Two weeks after the last injection, treated mice are ready for ISPL inoculation of oncogenic hepatocytes from MTD2 mice.
Materials
| Name | Company | Catalog Number | Comments |
|---|---|---|---|
| Anesthesia machine | VETEQUIP | IMPAC6 | anesthesia machine for surgery |
| Butterfly needle | BD | 8122963 | Needle used for liver perfusion |
| C57BL/6 mice | Jackson Lab | 000664 | mice used in prototol |
| Carprofen | CRESCENT CHEMICAL | 20402 | carprofen for pain release |
| Cell Strainer | CORNING | REF 431751 | Cell strainer, 70μm, for hepatocytes isolation |
| Centrifuge | Beckman Coulter | Allegra X-30R | centrifuge for cell isolation |
| Clips | Teleflex Medical | REF 523700 | Titanium Clips for spleen |
| Microscope | Zeiss | Primovert | microscope for cell observation |
| Mtd2 mice | N/A | Gift from Dr. William A Held at roswell Park Cancer Institute in 2002, maintained in our lab | |
| Needle | BD | REF 305109 | BD precisionglide needle, 27G × 1/2 (0.4mm × 13mm) |
| Suture | ETHICON | J303H | coated VICRYL suture |
| SV40 T Ag antibody | Abcam | ab16879 | anti-SV40 T-antigen antibody for IHC |
| Syringe | BD | REF 309626 | 1 mL TB syringe for cell injection |
| Trypan blue | SIGMA | T 8154 | Trypan blue solution for cell viability test |
| Wound clips | Reflex | reflex9, Part. No. 201-1000 | stainless steel wound clips for wound close |
2. Isolating Tag-transgenic Hepatocytes from Line MTD2 mice
NOTE: See Table 1 for solution recipes.
Table 1.
Solution recipes.
| 10x Earle’s Balanced Salt Solution without Ca or Mg (EBSS without Ca or Mg) | 4 g KCl 68 g NaCl 1.4 g NaH2PO4·H2O 10 g dextrose Add water to 1 liter, pH to 4.32 Pass through filter |
| Solution 1 | 20 mL 10x EBSS without Ca or Mg 44 g NaHCO3 1.33 mL 1.5M Hepes 10 mL of 10 mL EGTA Add water to 200 mL |
| Solution 2 | 100 mL 10x EBSS 2.2 g NaHCO3 6.67 mL 1.5 M Hepes Add water to 1 liter |
| 0.75% collagenase solution | 15 mg collagenase type 1 20 mL of solution 2 |
| Complete Medium | 2 RPMI 50 mL FBS 5 mL 100x Penicillin-Streptomycin |
Obtain line MTD2 mice38 to serve as the source of oncogenic hepatocytes.
-
Anesthetize 5-week-old MTD2 mice using 2.5% isoflurane.
NOTE: Proper anesthetization will be checked by toe pinch method. In brief, using two fingers, give the mouse toe/foot a good squeeze. If there is no withdrawal reaction, the animal is judged deep enough to commence surgery.
When adequately sedated, place mice in a supine position and fix the extremities with tape to provide adequate exposure of abdominal surface.
Perform a midline laparotomy incision using scissors along the length of the linea alba large enough to provide an adequate exposure of the liver.
Displace the intestines to the left to provide better exposure of the liver and portal triad.
Dissect above the liver to expose the inferior vena cava (IVC).
Ligate the IVC above the liver using an artery clamp.
Returning to the inferior border of the liver, use a butterfly needle (see materials) to gain IV access to the portal vein. Fix catheter by hand.
Successively perfuse the mouse liver using an injection syringe at 8.9 mL/min with with 15 mL of solution 1, 15 mL of 0.75% collagenase solution 2, and 15 mL of solution 2 via the catheter.
Harvest the perfused liver by cutting and taking the tumor mass from MTD2 mice in a 50 mL conical tube with 10–15 mL of PBS.
Remove PBS and wash an additional time with PBS; do not centrifuge at this step.
Cut the liver into smaller pieces using scissors and then wash again with PBS 2x to remove remaining blood.
Add 5 mL of complete RPMI medium to the conical tube and continuously mince the liver with scissors to small pieces (<3 mm)-tissue should smoothly go through a 5 mL pipette.
Add complete RPMI to a final volume of 30 mL and suspend liver using a 5 mL pipette.
Filter the mixed solution with a 70 μm strainer into a 50 mL conical tube.
Wash the strainer several times with complete RPMI and adjust the final volume to 50 mL by adding additional RPMI medium.
Quickly spin the suspension by centrifuge to a maximum of 500 rpm; once the speed is accelerated to 50 × g, the centrifuge should be stopped.
Decant the supernatant and suspend pellets in 20 mL of PBS.
-
Count cells using Trypan blue exclusion and a hemocytometer, then adjust the cell concentration to 2.5 × 106/mL for the following cell inoculation.
NOTE: The expected yield from 5 grams of tumor tissue is 80 million hepatocytes with viability >95%.
3. Inoculating the hepatocytes from MTD2 mice to the liver of wild type C57BL/6J mice by ISPL injection
The aseptic technique should be used in all the procedures.
Anesthetize the CCl4-treated male C57BL/6J mice with 2.5% isoflurane, the mice should be treated with eye lube to prevent eyes from drying out.
Prepare syringes with 200 μL of hepatocytes for injection.
When adequately sedated, position mice with left side up.
Shave the entire left flank of the mice, then scrub the area, alternating between 70% alcohol and betadine three times.
Make a 1 cm incision on the left flank parallel to the 13th rib from the dorsal extreme beginning just below the spine muscle.
Identify the spleen, then exteriorize it using blunt-pointed forceps.
-
Clip the spleen with two medium-sized titanium clips. Place both clips between the splenic artery and vein, leave room between the clips to cut later after inoculation.
NOTE: The goal is to isolate the inferior pole of the spleen to reduce risk of seeding.
Inject 200 μL (0.5 million) of the prepared hepatocytes into the inferior pole of the spleen using a 27 G needle.
Clip the inferior branch of the pedicle (inferior splenic pole vessels) with one medium-sized clip.
Cut the spleen between the two initially placed clips.
Remove the inferior pole of the spleen that was directly injected with tumor cells.
Use 3–0 polyglactin 910 interrupted suturing to close the inner muscle layer.
-
Use sterilized steel wound clips to close the outer skin layer.
NOTE: Steel clips are preferred over sutures to avoid animals chewing out sutures, leaving a gaping wound.
Administer 5 mg/kg of carprofen subcutaneouly after suture.
Place all recovering animals on a temperature-controlled heating pad and monitor closely until fully recovered from anesthesia.
Give mice free access to water after surgery. If the mouse becomes dehydrated during surgery, administer subcutaneous fluids (<1 mL).
Remove skin clips at 7–10 days post-operatively.
Representative Results
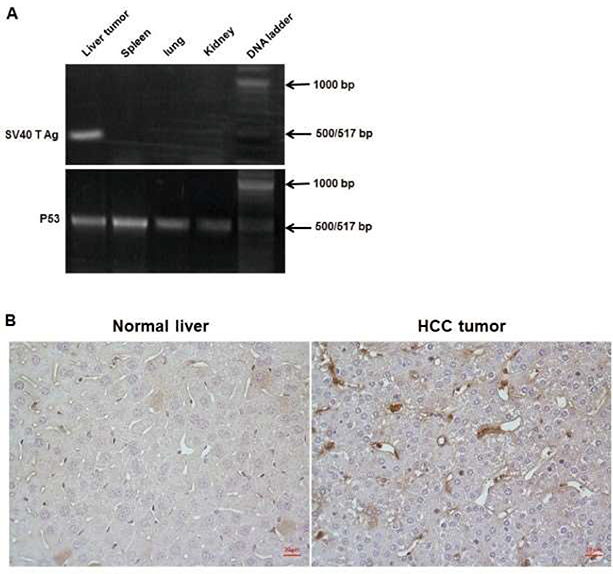
Oncogenic hepatocytes isolated from TAg-transgenic mice (Figure 2) were seeded in the liver of wild type mice by intra-splenic injection (Figure 3). The transplanted hepatocytes successfully and reliably grew orthotopic HCC tumors (Figure 4) with tumor specific antigen SV40 TAg (Figure 5) in the setting of hepatic inflammation and fibrosis (Figure 1).
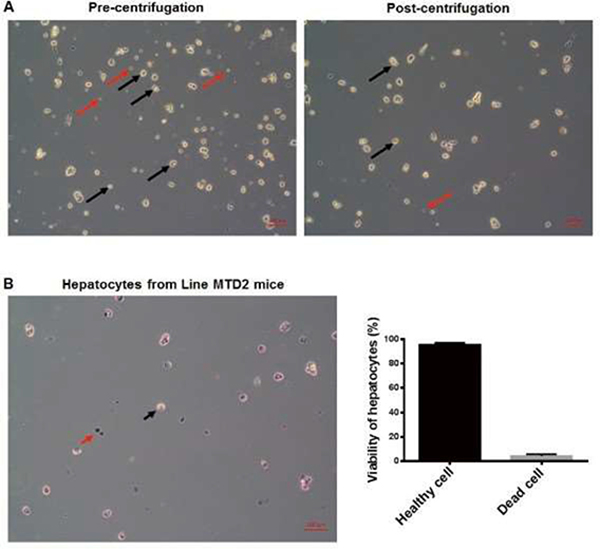
Figure 2: Isolation and purification of hepatocytes from line MTD2 mice.
(A) Hepatocytes isolated from MTD2 mice were prepared according to protocol and stained with trypan blue to detect viability and purity of cell isolation. The left panel shows both hepatocytes (black arrow) and tumor infiltrating lymphocytes (red arrows) that are isolated during the cell extraction. The right panel shows the cell population remaining after low speed centrifugation, including hepatocytes (black arrow) and significantly fewer tumor infiltrating lymphocytes. Magnification = 10x objective, scale bar = 100 μm. (B) Hepatocytes isolated from MTD2 mice are stained with trypan blue solution prior to inoculation of wild type C57BL/6J mice. Cell isolation is determined to be successful if viability is >95%. Dead cells will be stained with the trypan blue (red arrows), while viable cells will not be stained (black arrow). Magnification = 10x objective, scale bar = 100 μm. The graph on the right shows the results of cell isolation with >95% of hepatocytes being viable, statistical data come from 5 different observed field under microscope; error bars represent ±SD. Please click here to view a larger version of this figure.
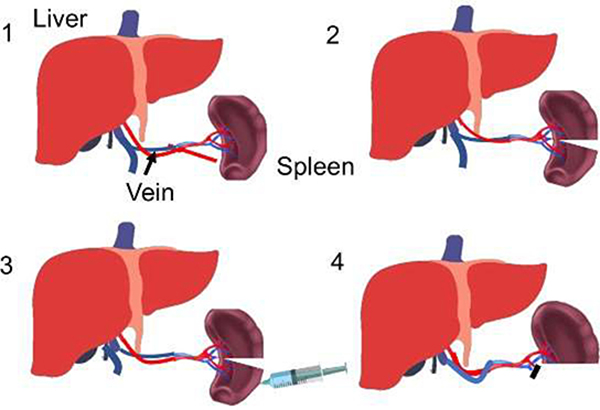
Figure 3: Intrasplenic inoculation of hepatocytes into the liver of wild type C57BL/6J mice.
The experimental design for ISPL inoculation of hepatocytes to induce HCC in C57BL/6J mice. (1) The spleen is identified and exteriorized. (2) The spleen is clipped with two medium-sized titanium clips. (3) Prepared hepatocytes are injected into the inferior pole of the spleen. (4) The inferior branch of the pedicle (inferior splenic pole vessels) is clipped with one medium-sized clip. Please click here to view a larger version of this figure.
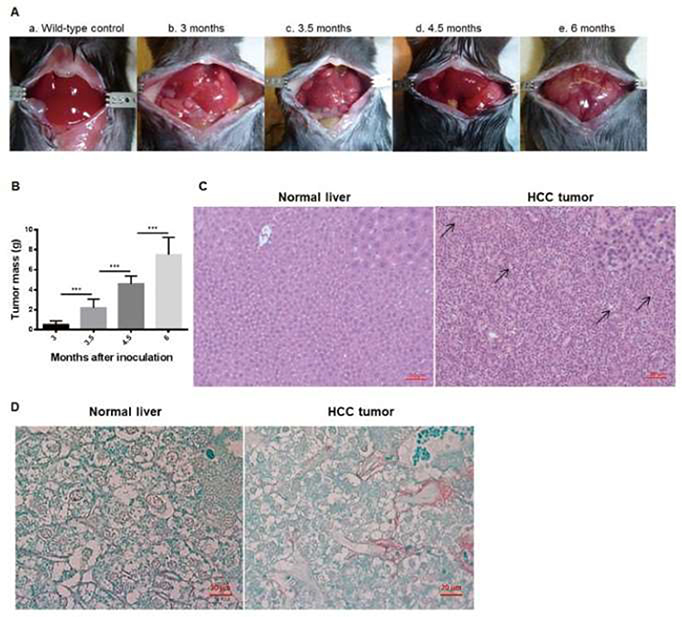
Figure 4: Progressive tumor development in C57BL/6J mice after inoculation with MTD2-hepatocytes.
(A) Hepatocellular carcinoma (HCC) orthotopic tumor model was established according to protocol. Anatomical images were taken before inoculation and at sub-sequential time courses. (a) Shows healthy liver prior to inoculation with MTD2 hepatocytes. (b) Mouse liver 3 months post inoculation with evidence of gross tumor development. (c) 3.5 months after inoculation with increasing tumor burden. (d) 4.5 months after inoculation. (e) 6 months after inoculation with evidence of tumor throughout the liver. (B) Tumor nodules were harvested and weighed at the time points indicated after inoculation with MTD2 hepatocytes. Error bars represent ±SD. ***P < 0.001, statistical analysis was performed by t-tests. (C) Representative images of wildtype and MTD2-inoculated liver sections. Hematoxylin and eosin (H&E) staining depicts pseudogland formation (black arrows). There is nuclear crowding, and tumor cells are eosinophilic with high nucleus-to-cytoplasm ratios (magnified image). Magnification = 20x objective, scale bar = 50 μm. The insets on the upper right are further manually amplified. (D) Sirius red staining indicating abnormal collagen deposition, consistent with liver fibrosis. Magnification: 40x objective, scale bar = 20 μm. Please click here to view a larger version of this figure.
Figure 5: Specific detection of SV40 T antigen gene in tumor.
(A) Tumor tissue and additional tissue samples throughout mice were collected from tumor-established mice. Genomic DNA was isolated from tissue and primers for both SV40 T Ag and P53 (control) were synthesized for conventional PCR. SV40 T antigen gene was detected in tumor tissue but is not present in either the normal tissue or other tissue in the mice. (B) Tumor tissue was collected from tumor-bearing mice and stained with anti-SV40 T antigen antibody. Left panel is a negative control from healthy liver tissue collected from naïve mice. Right panel shows significant SV40 T antigen staining of tumor tissue collected from tumor-bearing mice (brown color). Magnification = 40x objective, scale bar = 20 μm. Please click here to view a larger version of this figure.
Discussion
With this protocol, we have established a reliable and reproducible murine model of HCC that mimics human HCC initiation and progression. Clinically, many risk factors successively induce liver injury, liver fibrosis, cirrhosis and the final stage of HCC. In our protocol, IP injection of CCl4 is used to first produce liver fibrosis in wild type mice, which allows the subsequent oncogenic hepatocytes to form the tumors in the setting of liver fibrosis. We found that tumor formation occurred most successfully in mice that received the hepatocyte inoculation two weeks after CCl4 treatment, compared to mice receiving injections at other time points. In addition, we found liver fibrosis can be detected up to four months after CCl4 injection. This approach results in more than 90% of mice developing HCC tumors compared to the mice without exposure to CCl4. In our model, hepatocytes transferred from line MTD2 mice into C57BL/6J mice, traffic to the liver where they become incorporated as hepatocytes that express TAg as a tissue antigen. Isolation of hepatocytes from MTD2 is a critical step during this protocol. MTD2 mouse livers are perfused thoroughly with the solution 1 and 2 to remove circulating red blood cells within the liver completely. The collagenase solution is used to perfuse the liver at the indicated concentration and speed to generate proper liver digestion to release hepatocytes. The use of lower concentrations of collagenase is insufficient for digestion, resulting in clumps of hepatocytes. In contrast, high concentrations are too harsh on the tissue, resulting in a significant reduction of viable hepatocytes. We also find that brief centrifugation as described in our protocol is required to improve the purity of hepatocytes. The lower spin we used for centrifugation can precipitate hepatocytes and leave leukocytes in the supernatant based on the density difference of these two types of cells.
The next critical step is the route for inoculating hepatocytes into wild type mice. In our pilot studies, we explored various ways to conduct hepatocyte inoculation. The successful orthotopic tumor growth in the liver is seen best in mice receiving intrasplenic inoculation of oncogenic hepatocytes at a dose of half-a-million cells per mouse, compared to the mice receiving cells administered via tail vein and intraperitoneal injection at various doses. These findings suggest that the orthotopic HCC growth is route and dose-dependent. Malignant transformation occurs gradually and is limited to the subpopulation of transplanted hepatocytes rather than the whole liver parenchyma. Continued cell proliferation results in tumor nodules developing throughout the liver.
For HCC or other cancers to progress it must evade the immune system; in fact, avoiding immune destruction is now considered a hallmark of cancer39. However, the lack of tumor-specific antigen is a critical barrier to elucidating the underlying mechanisms. In our model, TAg is expressed in the tumors, not other organs, which acts as a tumor-specific antigen. Also, TAg has numerous well-defined epitopes that can be recognized by CD8 T cells in C57BL/6J mice. Regarding TAg epitope-I, we have generated line 416 mice which transgenically express T cell receptors for this epitope34. Targeting TAg to examine tumor antigen-specific immune response allows us to investigate tumor immune surveillance during tumor initiation and progression, which is not possible using models induced by DEN or genetic manipulation. Elucidating the underlying mechanisms enables us to identify critical cells and molecules mediating tumor-induced immune tolerance. Targeting these key factors can significantly advance our development of innovative immunotherapeutic strategies against HCC. Using this unique HCC model and established tools, we have investigated the mechanisms underlying tumor-induced tolerance25,35 and explored various immune-based antitumor immunotherapies31,32,36,37.
In summary, our established murine model of HCC reflects some typical features of human disease. In our previously published article, we were able to establish this as a clinically relevant tumor model that had typical features of human HCC. We showed that the mice treated with CCl4 and MTD2 hepatocytes developed tumors that expressed HCC-associated antigens, AFP and GPC336. Pathology determined that the lesions in our murine model are similar both macroscopically and pathologically to human HCC. Leveraging this reliable model and the developed tools, we can study this complex human disease including insight into mechanisms of HCC development and clinically available treatment.
Acknowledgments
This work is supported by NIH/NCI R01 CA164335-01A1 (K. F. Staveley-O’Carroll, PI) and NIH/NCI R01CA208396 (Mark Kester, Guangfu Li, Kevin F. Staveley-O’Carroll).
Footnotes
Disclosures
There are none to declare.
Video Link
The video component of this article can be found at https://www.jove.com/video/59368/
References
- 1.O’Connor S, Ward JW Hepatocellular carcinoma – United States, 2001–2006. Morbidity and Mortality Weekly Report. 59, 517–520 (2010). [PubMed] [Google Scholar]
- 2.Petrick J, Kelly S, Altekruse S, McGlynn K, Rosenberg P Future of Hepatocellular Carcinoma Incidence in the United States Forecast Through 2030. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 34, 1787–1794 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Greten T, Lai C, Li G, Staveley-O’Carroll K Targeted and Immune-based Therapies for Hepatocellular Carcinoma. Gastroenterology. 156, 510–524 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Llovet J, Zucman-Rossi J, Pikarsky E, Sangro B, Schwartz M, Sherman M, Gores G Hepatocellular Carcinoma. Nature reviews. Disease primers. 2, 16018 (2016). [DOI] [PubMed] [Google Scholar]
- 5.Ding X, et al. Precision medicine for hepatocellular carcinoma: driver mutations and targeted therapy. Oncotarget. 8, 55715–55730 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Colombo M, Maisonneuve P Controlling liver cancer mortality on a global scale: still a long way to go. Journal of Hepatology. 67, 216–217 (2017). [DOI] [PubMed] [Google Scholar]
- 7.Llovet J, Burroughs A, Bruix J Hepatocellular carcinoma. Lancet. 362 1907–1917 (2003). [DOI] [PubMed] [Google Scholar]
- 8.Parkin D, Bray F, Ferlay J, Pisani P Estimating the world cancer burden: Globocan 2000. International Journal of Cancer. 94, 153–156 (2001). [DOI] [PubMed] [Google Scholar]
- 9.Thomas M, Zhu A Hepocellular carcinoma: the need for progress. Journal of Clinical Oncology. 23, 2892–2899 (2005). [DOI] [PubMed] [Google Scholar]
- 10.Llovet J, Bruix J Molecular targeted therapies in hepatocellular carcinoma. Hepatology. 48, 1312–1327 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bruix J, Sherman M Management of hepatocellular carcinoma: an update. Hepatology. 53, 1020–1022, doi: 10.1002/hep.24199 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pang T, Lam V Surgical management of hepatocellular carcinoma. World Journal of Hepatology. 7, 245–252 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Llovet J, et al. Design and endpoints of clinical trials in hepatocellular carcinoma. Journal of the National Cancer Institution. 100, 698–711 (2008). [DOI] [PubMed] [Google Scholar]
- 14.Mueller K Cancer immunology and immunotherapy. Realizing the promise. Introduction. Science. 348, 54–55 (2015). [DOI] [PubMed] [Google Scholar]
- 15.Gajewski T, Schreiber H, Fu Y Innate and adaptive immune cells in the tumor microenvironment. Nature Immunology. 14, 1014–1022 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ribas A, Wolchok J Combining cancer immunotherapy and targeted therapy. Current Opinion in Immunology. 25, 291–296 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Postow M, Callahan M, Wolchok J Immune checkpoint blockade in cancer therapy. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 33, 1974–1982 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gao J, et al. VISTA is an inhibitory immune checkpoint that is increased in ipilimumab therapy in patients with prostate cancer. Nature Medicine. 23, 551–555 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hahn A, Gill D, Pal S, Agarwal N The future of immune checkpoint cancer therapy after PD-1 and CTLA-4. Immunotherapy. 9, 681–692 (2017). [DOI] [PubMed] [Google Scholar]
- 20.Remon J, Besse B Immune checkpoint inhibitors in first-line therapy of advanced non-small cell lung cancer. Current Opinion in Oncology. 29, 97–104 (2017). [DOI] [PubMed] [Google Scholar]
- 21.Kudo M Immune checkpoint blockade in hepatocellular carcinoma: 2017 update. Liver Cancer. 6, 1–12 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kudo M Immune checkpoint inhibition in hepatocellular carcinoma: Basics and ongoing clinical trials. Oncology. 92, 50–62 (2017). [DOI] [PubMed] [Google Scholar]
- 23.Breous E, Thimme R Potential of immunotherapy for hepatocellular carcinoma. Journal of Hepatology. 54, 830–834 (2011). [DOI] [PubMed] [Google Scholar]
- 24.Sprinzl M, Galle P Facing the dawn of immunotherapy for hepatocellular carcinoma. Journal of Hepatology. 59, 9–10 (2013). [DOI] [PubMed] [Google Scholar]
- 25.Liu D, Staveley-O’Carroll K, Li G Immune-based therapy clinical trials in hepatocellular carcinoma. Journal of Clinical Cell Immunology. 6, 376 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Greten T, Wang X, Korangy F Current concepts of immune based treatments for patients with HCC: from basic science to novel treatment approaches. Gut. 64, 842–848 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Koster B, de Gruijl T, van den Eertwegh A Recent developments and future challenges in immune checkpoint inhibitory cancer treatment. Current Opinion in Oncology. 27, 482–488 (2015). [DOI] [PubMed] [Google Scholar]
- 28.Johnson D, Sullivan R, Menzies A Immune checkpoint inhibitors in challenging populations. Cancer. 123, 1904–1911 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li H, et al. Programmed cell death-1 (PD-1) checkpoint blockade in combination with an mTOR inhibitor restrains hepatocellular carcinoma growth induced by hepatoma cell-intrinsic PD-1. Hepatology. 66, 1920–1933 (2017). [DOI] [PubMed] [Google Scholar]
- 30.Heindryckx F, Colle I, van Vlierberghe H Experimental mouse models for hepatocellular carcinoma research. International Journal of Experimental Pathology. 90, 367–386 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Qi X, et al. Development of inCVAX, in situ cancer vaccine, and its immune response in mice with hepatocellular cancer. Journal of Clinical and Cellular Immunology. 7, 438 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Qi X, et al. Development of a radiofrequency ablation platform in a clinically relevant murine model of hepatocellular cancer. Cancer Biology and Therapy. 16, 1812–1819 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu D, et al. Sunitinib represses regulatory T cells to overcome immunotolerance in a murine model of hepatocellular cancer. Oncoimmunology. 7, e1372079 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Staveley-O’Carroll K, et al. In vivo ligation of CD40 enhances priming against the endogenous tumor antigen and promotes CD8+ T cell effector function in SV40 T antigen transgenic mice. Journal of Immunology. 171, 697–707 (2003). [DOI] [PubMed] [Google Scholar]
- 35.Avella D, et al. Regression of established hepatocellular carcinoma is induced by chemoimmunotherapy in an orthotopic murine model. Hepatology. 55, 141–152 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li G, et al. Successful chemoimmunotherapy against hepatocellular cancer in a novel murine model. Journal of Hepatology. 66, 75–85 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li G, et al. Nanoliposome C6-ceramide increases the anti-tumor immune response and slows growth of liver tumors in ice. Gastroenterology. 154, 1024–1036.e9 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Held W, et al. T antigen expression and tumorigenesis in transgenic mice containing a mouse major urinary protein/SV40 T antigen hybrid gene. EMBO Journal. 8, 183–191 (1989). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hanahan D, Weinber R Hallmarks of cancer: the next generation. Cell. 144, 646–674 (2011). [DOI] [PubMed] [Google Scholar]