Abstract
Background: The bicuspid aortic valve (BAV) is the most common cardiac congenital disease and is associated with an increased risk of developing ascending aorta dilation; which can have fatal consequences. Currently; no established risk biomarkers exist to facilitate the diagnosis and prognosis of BAV. Methods: Using an untargeted metabolomic approach; we identified the levels of metabolites in plasma samples and compared them depending on the bicuspid or tricuspid morphology of the aortic valve. Including those patients with ascending aortic dilation and/or aortic stenosis (n = 212), we analyzed the role possibly played by alpha-Tocopherol in BAV disease; considering its association with the pathophysiological characteristics of BAV and biomarkers related to inflammation, oxidative stress and endothelial damage, as well as characteristics related to alpha-Tocopherol functionality and metabolism. Results: We found that BAV patients; especially those with ascending aortic dilation; presented lower antioxidant capacity; as determined by decreased plasma levels of alpha-Tocopherol; paraoxonase 1 and high-density lipoprotein (HDL), as well as increased levels of C-reactive protein (CRP; a biomarker of inflammation) and endothelial microparticles (EMPs; an endothelial damage biomarker). By applying random forest analyses; we evaluated the significant screening capacity of alpha-Tocopherol; CRP and EMPs to classify patients depending on the morphology of the aortic valve. Discussion: Our findings support the role of decreased antioxidant capacity; increased inflammation and endothelial damage in the pathogenesis of BAV and the progression of aortic dilation. Moreover; determining the plasma levels of alpha-Tocopherol; CRP and EMPs could improve BAV diagnosis in large populations.
Keywords: bicuspid aortic valve, ascending aortic dilation, metabolomics, alpha-Tocopherol, antioxidant, inflammation
1. Introduction
Bicuspid aortic valve (BAV) is the most common cardiac congenital malformation, affecting 1–2% of the population and occurring when two of the three leaflets (or cups) of the aortic valve did not separate during fetal development (or less frequently, when congenitally only two leaflets are presents), leading to a bicuspid configuration, rather than the normal three (tricuspid aortic valve; TAV) [1].
As such, BAV patients present a high prevalence of aortic dilation (greater than 50%) which, if untreated, can lead to fatal consequences, such as aortic dissection and/or rupture [2,3]. Bicuspid morphology of the aortic valves causes turbulent blood flow and abnormal hemodynamical patterns in the proximal ascending aorta [4], generating shear stress that impacts the endothelial cells that line the inner surface and leading to dysfunctional aortic endothelium [5,6].
In clinical practice, early detection of BAV is difficult because most of the patients are asymptomatic for a long time and echocardiography is the technique most frequently used to achieve a conclusive diagnosis. Currently, no effective strategies exist to prevent the progression of BAV disease and its related disorders; therefore, the development of new and efficient approaches require a more detailed understanding of the molecular mechanisms for BAV pathogenesis [7]. Echocardiographic measurement of the ascending aortic diameter is the most current method used to monitor aortopathy in BAV patients. Therefore, development of new screening methods and identification of non-invasive biomarkers that could be examined in a high-throughput format could facilitate and improve the prompt diagnosis of BAV.
Untargeted metabolomic profiling is considered a powerful analytic tool for the identification of disease-related biomarkers and pathways that can be used to develop new diagnostic and treatment methods [8]. Considering our previous publications that describe an association between BAV and the circulating levels of biologically active molecules, including microparticles and microRNAs [9,10,11], in this study, we hypothesized that the complex etiology of the BAV valvulopathy and aortopathy could be associated with a differential circulating profile of metabolites, which could supply an improvement in the diagnostic methods and could also elucidate the molecular mechanisms and functional implications underlying BAV.
2. Methods
2.1. Study Participants
In this study, we included patients belonging to a cohort of TAV controls and BAV patients prospectively included and followed-up in our facilities. The participants were informed and provided written consent. BAV was diagnosed when two aortic leaflets were visualized, with or without a raphe, in the parasternal short-axis view of a transthoracic or transesophageal echocardiogram [12] or on a cardiac magnetic resonance image [13]. Explorations were performed or supervised by the same observer (JM.A.). This study was conducted according to the principles of the Declaration of Helsinki and was approved by the Institutional Review Board and Ethics Committee (03-06-19/6proj4 and 114/2020) of our institutions, the Hospital Universitari de Sant Joan and the Institut d’Investigació Sanitària Pere Virgili.
The design of this study included two evaluations of four independent cohorts of age 18–78 years, including TAV individuals (TAV), BAV patients with no aortic dilation (BAV), patients with BAV and ascending aorta dilation at the time of diagnosis (BAVdil) and patients with TAV and ascending aorta dilation (TAVdil) (n = 212). The patient characteristics are described in Table 1. First, we determined the influence of the aortic valve morphology on the plasma metabolome by comparing the circulating metabolite profile between TAV and BAV patients. For this purpose and to exclude the effects of possible confounding factors, we included only those TAV (n = 33) and BAV patients (n = 62) with no aortic dilation (i.e., patients with a diameter of the ascending aorta less than 37 mm) and with no aortic stenosis (defined as patients with a mean transaortic pressure gradient less than 20 mmHg). However, in the second evaluation and to gain insight into the molecular mechanisms underlying the complexity of BAV pathology and the predictive value of the identified metabolites, we included patients with both morphologies (tricuspid or bicuspid) and aortic dilation (TAVdil; n = 35 and BAVdil; n = 82), as well as patients with aortic stenosis independent of the morphology of the aortic valve.
Table 1.
Clinical and echocardiographic characteristics of patients included in this study.
| TAV | BAV | TAVdil | BAVdil | p-Value | |
|---|---|---|---|---|---|
| n | 33 | 62 | 35 | 82 | |
| Age (years) | 47 ± 2 | 41 ± 2 | 63 ± 2 | 52 ± 2 | 3.9 × 10−11 **, b,c,d |
| Sex (male/female) | (25/8) | (45/17) | (22/13) | (58/24) | 0.670 |
| Body weight (kg) | 71.32 ± 2.4 | 71.00 ± 2.0 | 80.50 ± 11.5 | 76.52 ± 1.8 | 0.183 |
| Severe aortic stenosis (mean gradient ≥ 40 mm Hg) | 0 (0%) | 3 (5%) | 0 (0%) | 19 (23%) | 2.1 × 10−5 ** |
| Aortic valve gradient (mean, mm Hg) | 3.57 ± 1.0 | 12.04 ± 1.8 | 2.85 ± 0.8 | 24.75 ± 2.6 | 5.5 × 10−12 **, b,d |
| Left ventricle diastolic diameter (mm) | 50.22 ± 0.9 | 52.20 ± 0.8 | 53.48 ± 1.0 | 53.79 ± 1.0 | 0.100 |
| Left ventricle systolic diameter (mm) | 30.35 ± 1.2 | 32.56 ± 0.8 | 30.01 ± 0.9 | 33.36 ± 0.9 | 0.175 |
| Left ventricular ejection fraction (%) | 71.92 ± 1.9 | 70.72 ± 1.2 | 70.86 ± 1.8 | 69.18 ± 1.1 | 0.568 |
| Aortic root diameter (mm) | 33.06 ± 0.8 | 33.93 ± 0.8 | 41.94 ± 1.2 | 39.32 ± 0.6 | 2.4 × 10−13 **, b,c |
| Ascending aorta diameter (mm) | 30.81 ± 0.6 | 32.56 ± 0.4 | 44.88 ± 0.7 | 44.36 ± 0.6 | 5.5 × 10−47 **, b,c |
TAV tricuspid aortic valve; BAV bicuspid aortic valve patients; BAVdil patients with bicuspid aortic valve and aortic dilation * Significant values (Overall p < 0.01); a, p < 0.05 TAV vs. BAV; b, p < 0.05 BAV vs. BAVdil; c, p < 0.05 TAV vs. TAVdil; d, p < 0.05 BAVdil vs. TAVdil. ** p-value < 0.01.
Patients diagnosed with Marfan syndrome or diabetes mellitus, or those receiving pharmacologic treatment (including statins, ACE/ARBs and/or β-blockers), were excluded.
2.2. Blood Sampling and Analyses
Blood samples were collected under overnight fasting conditions and were processed within 90 min of collection. The samples were centrifuged at 1500× g for 15 min to obtain plasma, which was further centrifuged at 4000× g for 10 min to obtain platelet-poor plasma. The plasma was stored at −80 °C in our biological samples bank (Biobanc IISPV–HUSJR) until needed.
Total cholesterol, triglycerides, low-density lipoprotein (LDL) cholesterol, direct high-density lipoprotein (HDL) cholesterol, high-sensitivity C-reactive protein (CRP), lipoprotein (a) (Lpa), apolipoprotein B100 and apolipoprotein A1 were measured using standardized enzymatic and immunoturbidimetric assays (Spinreact and Horiba ABX Montpellier) adapted to a Cobas Mira Plus autoanalyzer (Roche Diagnostics).
The levels of circulating endothelial microparticles (EMPs) were determined as previously described [9]. Briefly, EMPs were measured using flow cytometry (EPICS-XL; Beckman Coulter) at a low rate and 30 s stop time. The Nano Fluorescent Particle Size Standard Kit (Spherotech) and Flow Count fluorospheres (Beckman Coulter) were used in instrument standardization and as an internal calibrator for microparticle amount calculation, respectively.
Plasma EMPs were defined as particles > 0.1 and <1 μm in size and their endothelial origin was identified based on their affinity to specific cell surface antigens, CD31 and CD42b. Possible contamination with leukocyte-derived microparticles was discarded by measuring <4.5% of microparticles co-expressing CD31+CD45+. EMPs were measured by trained technicians who were blind to the clinical status of the patients as well as to the results.
2.3. Metabolomics Profiling
A biphasic extraction with methanol in 0.1% formic acid and dichloromethane was used to extract metabolites. Methanol in 0.1% formic acid was added to plasma samples followed by vortexing and 3 volumes of dichloromethane and 1 volume of water were added. After a 30-min incubation at 4 °C, samples were centrifuged (15,000 rpm, 15 min at 4 °C) and the organic phase was collected for drying under nitrogen. Pellets were resuspended in methanol:toluene (9:1) for LC/MS analysis.
Untargeted liquid chromatography/mass spectrometry (LC/MS) analyses were performed using an ultrahigh-performance liquid chromatography (UHPLC) system (1290 Agilent) coupled to a 6550 ESI-QTOF MS (Agilent Technologies) instrument operating in positive (ESI+) electrospray ionization mode. Metabolites were separated by reverse-phase chromatography with an Acquity UPLC C18-RP instrument (ACQUITY UPLC BEH C18 1.7 µM, Waters). Mobile phase A was acetonitrile/water (60:40) (10 mM ammonium formate) and mobile phase B was isopropanol/acetonitrile (90:10) (10 mM ammonium formate). Solvent modifiers were used to enhance ionization and to improve the LC resolution in positive ionization modes. The separation was conducted under the following gradient—0 in 15% of B; 0–2 min 30% of B; 2–2.5 min 48% of B; 2.5–11 min 82% of B; 11–11.5 min 99% of B; 11.5–12 min 99% of B; 12–12.1 min 15% of B; and 12.1–15 min 15% of B. The ESI conditions were applied as follows—gas temperature = 150 °C; drying gas = 13 L min−1; nebulizer = 35 psig; fragmentor = 150 V; and skimmer = 65 V. The instrument was set to work over an m/z range of 50–1200 with an acquisition rate of 3 spectra/sec. For compound identification, tandem mass Spectrometry (MS/MS) analyses were performed in targeted mode with a default iso-width (width at half-maximum of the quadrupole mass bandpass used during MS/MS precursor isolation) of 4 m/z. The collision energy was fixed at 20 and 40 V.
LC/MS data were processed using XCMS [14] software (version 1.34.0) to detect and align mzRT features. XCMS analysis of these data produced a matrix containing the retention time, m/z value and integrated peak area of each feature for each sample. We constrained the initial number of features via the following criteria. Only features above an intensity threshold of 5.000 were retained for further statistical analysis. Quality control samples (QCs) consisting of pooled samples from each condition were injected at the beginning and periodically throughout the worklist. The performance of the LC/MS platform for each mzRT feature detected in the samples was assessed by calculating the relative standard deviation of these features on pooled samples (CVQC) [15]. Statistical analyses were performed using the specmine package [16] in R Bioconductor.
2.4. Random Forest Model Construction and Validation
A model was constructed to estimate the capacity to predict or classify patients based on the morphology of the aortic valve. Therefore, the selection of the variables that make the largest contributions to classification was conducted using association based on Spearman’s correlation and linear regression analysis and random forest variable importance measures. The analyses were performed using the randomForest package [17] in R (Bioconductor). We build a model to discriminate patients depending on the morphology of their aortic valve. This model was evaluated including patients with no aortic dilation (BAV and TAV, n = 95) or including the four previously described groups (TAV, TAVdil, BAV and BAVdil, n = 212). Patients were randomly divided into two subsets—63% of the individuals were used to train the model and 37% of the individuals were used to test the developed models. The training data set was evaluated with a 10-fold cross-validation fold procedure. The statistical parameters for assessing the predictive performance of the random forest classifier were based on the accuracy, sensitivity and specificity.
2.5. Statistical Analysis
Data are expressed as the mean ± standard error mean (SEM). Continuous variables were compared between groups using the Wilcoxon test. Correlations were evaluated using Spearman’s Rho. Statistical analyses were performed using SPSS software (IBM SPSS Statistics, United States, version 22.0) and R (Bioconductor). P-values < 0.05 were considered to be significant.
3. Results
3.1. Circulating Profile of Metabolites Depends on the Morphology of the Aortic Valve
To analyze whether BAV valvulopathy could be related to a differential profile of circulating metabolites, we compared the circulating metabolome of patients with bicuspid or tricuspid morphology of the aortic valve using an untargeted metabolomics approach. In this analysis, we selected patients with homogeneous characteristics, no aortic dilation and with no aortic stenosis to exclude the effects of possible confounding factors.
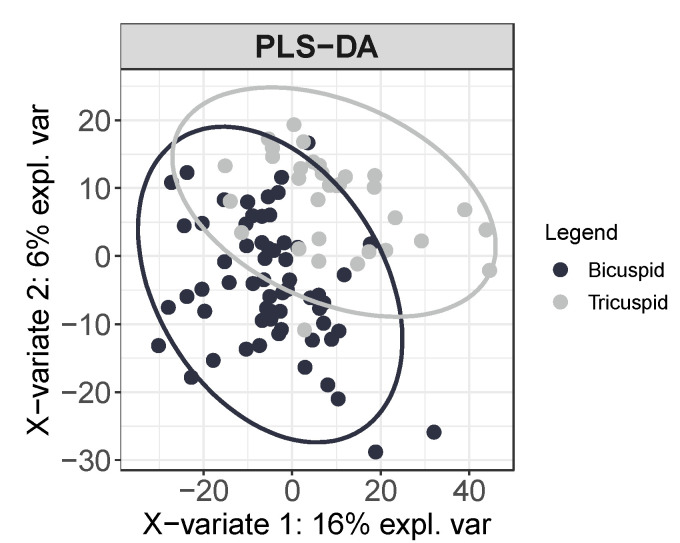
Using this high-throughput approach, we detected 2289 distinct metabolite features in plasma samples. As an exploratory analysis, using unsupervised principal component analysis (PCA), we firstly corroborated the absence of outliers, trends, patterns or clusters in the data prior to statistical analysis. Moreover, using a supervised partial-least-squares discrimination analysis (PLS-DA), we determined that by measuring the metabolomic plasma profile, patients can be classified depending on the bicuspid or tricuspid morphology of their aortic valves (Figure 1). Thus, from the 2289 metabolite features measured, 2 unique metabolites were significantly different between TAV and BAV, namely, alpha-Tocopherol (fdr = 2.17 × 10−3) and choline (fdr = 8.44 × 10−3) and both metabolites presented lower abundance in the plasma of BAV patients than in that of TAV patients.
Figure 1.
Plasma metabolome differs depending on the morphology of the aortic valve. Multivariate supervised partial-least-squares discrimination analysis PLS-DA of the 2289 total metabolite features detected in plasma classifies between tricuspid aortic valve (TAV) and bicuspid aortic valve (BAV), patients (95% confidence interval ellipses are shown for the TAV and BAV groups). (n = 95).
3.2. Functional Implication of the Identified Metabolites
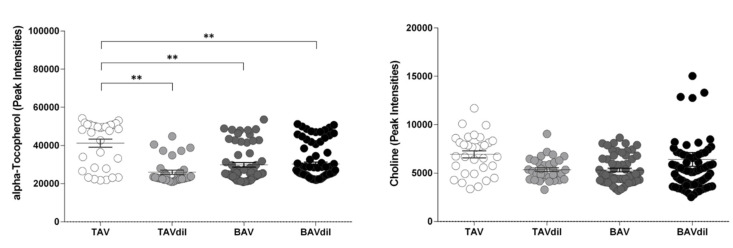
Dilation of the ascending aorta and aortic stenosis are the two most common comorbidities associated with BAV; therefore, to improve the translational character and the clinical applicability of the obtained results, we analyzed whether the circulating levels of alpha-Tocopherol and choline remained significantly different between TAV and BAV patients when we consider those patients with an ascending aortic dilation (TAVdil and BAVdil) and also include those patients with aortic stenosis in the corresponding groups (Figure 2).
Figure 2.
Peak intensities measured for the alpha-Tocopherol and choline levels in TAV and BAV patients. n = 202. ** p-value < 0.01.
We observed that although the levels of alpha-Tocopherol were higher in TAV individuals than in patients with BAV, BAVdil and TAVdil, no significant changes were observed in the circulating levels of choline. We performed a 3-way ANOVA including the valve morphology, ascending aortic dilation and aortic stenosis as independent variables and alpha-Tocopherol or choline as dependent variables and we found that only the interaction between the valve morphology (BAV vs TAV) and dilation resulted significative (p-value = 0.042) for the alpha-Tocopherol levels and no main effects nor interactions resulted significative for the choline levels.
To analyze the relationship between alpha-Tocopherol plasma levels and BAV disease and whether it might play a role in the progression of the disease, we analyzed the association of the circulating levels of alpha-Tocopherol with the pathophysiological characteristics of BAV disease, including echocardiographic and other confounding clinical variables. Using multivariate linear regression analysis (Table 2), we observed that the diameter of the ascending aorta was the only variable independently and negatively associated with the plasma levels of alpha-Tocopherol.
Table 2.
Multivariate linear analysis of variables related to the plasma levels of alpha-Tocopherol.
| Coefficient | Std-Coefficient | p-Value | |
|---|---|---|---|
| alpha-Tocopherol | |||
| Age (years) | −47.99 (−157.20 to 61.31) | −0.75 | 0.388 |
| Aortic root (mm) | 120.60 (−207.20 to 448.39) | 0.75 | 0.469 |
| Ascending aorta (mm) | −370.60 (−643.81 to −97.39) | −2.68 | 8.13 × 10−3 ** |
| Mean transaortic pressure gradient (mm Hg) | 25.91 (−58.78 to 110.61) | 0.046 | 0.547 |
| Left ventricle diastolic diameter (mm) | 29.72 (−316.57 to 376.01) | 0.021 | 0.169 |
| Left ventricle systolic diameter (mm) | 133.85 (−418.85 to 686.54) | 0.071 | 0.633 |
| Left ventricular ejection fraction (%) | 165.13 (−76.42 to 406.68) | 0.157 | 0.179 |
** p-value < 0.01.
Using this approach to elucidate the biological implication and the functionality of alpha-Tocopherol in BAV disease, we considered both the cellular and molecular mechanisms that have been associated with BAV, including inflammation, oxidative stress and endothelial damage [6]. Furthermore, we also considered characteristics related to alpha-Tocopherol function and metabolism, including its role as the most important lipid-soluble antioxidant carried by lipoproteins in plasma. Therefore, we first analyzed the effect of aortic valve morphology and ascending aortic dilation on the plasma levels of parameters associated with lipid and lipoproteins, inflammation, oxidative stress and endothelial damage.
We determined that the bicuspid morphology of the aortic valve and dilation of the ascending aorta were related to higher levels of endothelial microparticles (EMPs) and C-reactive protein (CRP), which are biomarkers related to endothelial damage and inflammation, respectively but these patients also had lower levels of apolipoprotein A1 (ApoA1), the major HDL protein (Table 3).
Table 3.
Effect of aortic valve morphology and ascending aortic dilation on the plasma levels of parameters associated with lipid metabolism, inflammation, oxidative stress and endothelial damage.
| TAV | BAV | TAVdil | BAVdil | p-Value | |
|---|---|---|---|---|---|
| Total cholesterol (mmol/L) | 5.61 ± 0.3 (5.04–6.18) |
4.77 ± 0.2 (4.43–5.01) |
5.20 ± 0.3 (4.60–5.79) |
5.07 ± 0.1 (4.79–5.33) |
0.171 |
| Triglycerides (mmol/L) | 1.36 ± 0.2 (0.96–1.76) |
0.97 ± 0.7 (0.82–1.11) |
1.48 ± 0.2 (1.13–1.84) |
1.33 ± 0.1 (1.06–1.60) |
0.139 |
| LDL (mmol/L) | 3.45 ± 0.2 (3.00–3.90) |
2.87 ± 0.1 (2.58–3.15) |
3.26 ± 0.2 (2.80–3.72) |
2.97 ± 0.1 (2.74–3.20) |
0.172 |
| HDL (mmol/L) | 1.55 ± 0.1 (1.32–1.77) |
1.47 ± 0.5 (1.37–1.57) |
1.26 ± 0.1 (1.14–1.39) |
1.49 ± 0.5 (1.39–1.59) |
0.049 * |
| ApoA1 (mg/dL) | 160.67 ± 7.3 (144.67–176.66) |
133.47 ± 4.4 (124.60–142.35) |
139.53 ± 4.5 (130.02–149.03) |
140.61 ± 3.7 (133.22–148.00) |
0.007 ** a, e |
| ApoB100 (mg/dL) | 118.50 ± 6.9 (103.27–133.73) |
88.67 ± 4.1 (80.38–96.95) |
112.88 ± 6.2 (99.65–126.12) |
99.22 ± 3.7 (91.79–106.64) |
0.005 ** a, c |
| C-reactive protein (mg/dL) | 1.06 ± 0.3 (0.38–1.72) |
1.71 ± 0.3 (1.14–2.29) |
1.84 ± 0.5 (0.86–2.82) |
2.42 ± 0.4 (1.70–3.13) |
0.046 * e |
| Paraoxonase 1 (ng/mL) | 85.23 ± 6.5 (70.94–99.94) |
94.61 ± 8.8 (76.67–112.55) |
78.12 ± 8.0 (61.25–94.99) |
87.12 ± 7.1 (72.86–101.37) |
0.647 |
| Endothelial microparticles (log part/μL) | 2.49 ± 0.4 (1.55–3.43) |
3.68 ± 0.3 (3.05–4.27) |
3.24 ± 0.3 (2.55–3.92) |
3.78 ± 0.2 (3.35–4.20) |
0.020 * e |
| Albumin (g/dL) | 4.64 ± 0.3 (4.55–4.73) |
4.53 ± 0.1 (4.53–4.65) |
4.39 ± 0.1 (4.27–4.52) |
4.52 ± 0.1 (4.46–4.58) |
0.010 * c |
* Significant values (Overall p < 0.05), ** Significant values (Overall p < 0.01), a, p < 0.05 TAV vs. BAV; b, p < 0.05 BAV vs. BAVdil; c, p < 0.05 TAV vs. TAVdil; d, p < 0.05 BAVdil vs. TAVdil; e, p < 0.05 TAV vs. BAVdil.
Using an analysis of covariance (ANCOVA) we found that the levels of alpha-Tocopherol remained significantly different between groups (p-value < 0.01) while considering the effect of ApoA1 (p-value = 0.423) or HDL (p-value = 0.773).
Furthermore, using Spearman’s correlation coefficient, we found that plasma levels of alpha-Tocopherol were negatively associated with the diameter of the ascending aorta, the aortic root and the age. The plasma levels of alpha-Tocopherol were also associated with circulating concentrations of ApoA1 and albumin, the two carriers of alpha-Tocopherol in plasma and paraoxonase 1, an enzyme with antioxidant properties transported in HDL (Table 4).
Table 4.
Linear relationship between the plasma levels of the identified metabolites and the parameters associated with lipid metabolism, inflammation, oxidative stress and endothelial damage.
| Alpha-Tocopherol | ||
|---|---|---|
| R | p-Value | |
| Aortic root (mm) | −0.172 | 0.012 * |
| Ascending aorta (mm) | −0.271 | 7.20 × 10−5 ** |
| Mean transaortic pressure gradient (mm Hg) | −0.083 | 0.230 |
| Age (y) | −0.179 | 0.009 ** |
| Lipid Metabolism | ||
| Total cholesterol (mmol/L) | 0.052 | 0.514 |
| Triglycerides (mmol/L) | 0.023 | 0.770 |
| ApoA1 (mg/dL) | 0.209 | 0.008 ** |
| ApoB100 (mg/dL) | 0.082 | 0.305 |
| Inflammation | ||
| C-reactive protein (mg/dL) | 0.042 | 0.607 |
| Oxidative stress | ||
| Paraoxonase 1 | 0.195 | 0.030 * |
| Endothelial damage | ||
| Endothelial microparticles (log part/μL) | 0.097 | 0.263 |
| Liver damage | ||
| Albumin (g/dL) | 0.248 | 0.002 ** |
* p-value < 0.05; ** p-value < 0.01.
3.3. Prediction of the Morphology of the Aortic Valve or the Dilation of the Ascending Aorta in BAV Patients
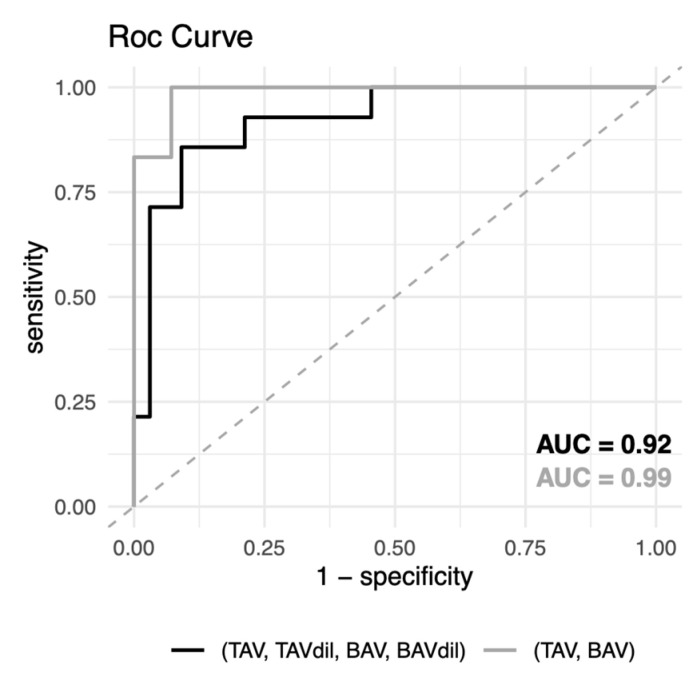
The results obtained in the previous analyses enable us to consider the role of plasma biomarkers based on its functional implication in aortic valve dysfunction and also as predictive circulating signatures of aortic valve morphology. Thus, we evaluated the predictive capacity of the differential metabolomic signature in plasma together with the variables that make the largest contributions to classification. To this end, we used the random forest algorithm to construct a model able to discriminate patients depending on the morphology of the aortic valve (Table 5 and Figure 3). The model was constructed using two approaches, one including all patients independent of the morphology of the aortic valve and the dilation of the ascending aorta and the other excluding those patients with ascending aortic dilation.
Table 5.
Evaluation of multivariable biomarker models including alpha-Tocopherol, endothelial microparticles (EMPs) and C-reactive protein (CRP) for the prediction of aortic valve morphology.
| p-Value | OOB Error | Accuracy (95% CI) |
Sensitivity | Specificity | AUC |
|---|---|---|---|---|---|
| TAV + TAVdil + BAV + BAVdil | |||||
| 3.9 × 10−3 ** | 21.7% | 0.89 (0.77–0.96) |
0.91 | 0.86 | 0.92 |
| TAV + BAV | |||||
| 7.6 × 10−3 ** | 17.5% | 0.95 (0.75–0.99) |
0.93 | 1.00 | 0.99 |
** p-value < 0.01.
Figure 3.
ROC curves of cross-validated random forest classification of test data.
We determined that the alpha-Tocopherol, EMPs and CRP circulating levels were variables able to discriminate patients based on their valve morphologies. Thus, the model constructed using these variables presented an accuracy of 0.89, a test sensitivity of 0.91, a specificity of 0.86 and a p-value (accuracy > no information rate) = 3.9 × 10− when we do not exclude patients depending on aortic diameter. However, in the case in which only TAV and BAV patients with no ascending aortic dilation were included in the model construction, the test sensitivity and specificity values were 0.95 and 1.00, respectively and the p-value (accuracy > no information rate) = 7.6 × 10−3.
4. Discussion
Using an untargeted metabolomics approach, we have identified significant associations between the plasma levels of alpha-Tocopherol and the morphology of the aortic valve and diameter of the ascending aorta. Moreover, we have determined that BAV patients, especially those with ascending aortic dilation, are characterized by increased levels of circulating biomarkers of inflammation, such as CRP, endothelial damage by measuring EMPs and decreased antioxidant capacity due to the lower circulating levels of alpha-Tocopherol, as well as its main carrier in plasma, the HDL lipoprotein, measured as ApoA1. Finally, we have evaluated how the circulating levels of alpha-Tocopherol, together with CRP and EMPs, are significant predictors of the aortic valve morphology, thereby identifying alpha-Tocopherol as the most important classification variable.
The pathogenesis of ascending aortic dilation in BAV is not completely understood. Two main non-mutually exclusive theories exist associating BAV aortopathy with genetic or hemodynamic causes. Focusing on hemodynamic causes, the bicuspid morphology of the aortic valve causes an abnormal biochemical environment, a consequence mainly of the non-physiological hemodynamic impact on the ascending aorta. This morphology-associated helical flow alteration that propagates flow eccentricity leads to increased wall shear stress on the endothelium and progressive dilation of the ascending aorta [18,19]. Although BAV disease is asymptomatic initially, the lack of an early diagnosis can lead to identifying the case in advanced stages or after an event. Therefore, in clinical practice, the existing approaches to achieving a conclusive diagnosis and to monitoring aortopathy in BAV patients are based on images obtained by transthoracic echocardiography [20]. A clear need exists for novel diagnostic and molecular tools to improve BAV screening, disease stratification and monitoring response to therapeutic interventions [21].
Untargeted metabolomics is a powerful tool that can supply a high-resolution snapshot of the complete set of metabolites, leading to the identification of specific metabolic signatures that can determine any perturbation of single or multiple metabolites and the related biochemical pathways [22], thereby offering new insights into the molecular mechanisms underlying complex diseases. Therefore, despite our untargeted metabolomics approach that identified the alpha-Tocopherol and the choline, only alpha-Tocopherol levels remained significantly different when we included patients with dilated ascending aorta and aortic stenosis, the two common complications related to BAV progression, in the analysis. Alpha-Tocopherol, as the primary form of the vitamin E, is a fat-soluble antioxidant with the capacity to neutralize endogenous free radicals and is carried in the blood primarily through HDL lipoproteins [23] but would also be bound to albumin [24]. Supporting this observation, we found a significant positive correlation between plasma levels of alpha-Tocopherol and ApoA1, albumin and paraoxonase 1, an enzyme transported by HDL with antioxidant and anti-atherogenic properties [25]. Interestingly, in addition to its antioxidant capacity, alpha-Tocopherol also acts as a regulator of the expression of genes involved in lipid metabolism and inflammation [26]. The plasma levels of alpha-Tocopherol have not been previously related to BAV pathology but nevertheless, a previous study Wang et al. [27] identified choline as one of the different metabolites in the serum of BAV patients before aortic valve replacement surgery compared with healthy individuals. However, the patients included in that study presented severe conditions (aortic valve dysfunction and/or aortic dilatation) leading to surgery indication; thus, those conditions together with BAV could affect the circulating metabolome profile. Choline is an essential nutrient for human health, being the liver the central organ responsible for its metabolization. Choline is involved in several physiological functions, phosphorylated, choline acts as the substrate for the synthesis of phosphatidylcholine, a key component of eukaryotic cellular membranes when its oxidized, choline participates as a methyl-donor in the methylation processes and in the case to be acetylated, choline generates acetylcholine, an important neurotransmitter [28,29]. Further, choline also participates in the solubilization of bile salts and is required for the generation of VLDL lipoproteins [30]. Choline has cardioprotective effects by downregulating inflammation, restoring endothelium structure and by inhibiting the generation of reactive oxygen species [28,31].
The results presented in this study showed that circulating levels of alpha-Tocopherol were higher in TAV individuals than in patients with BAV but also in those patients with dilated ascending aorta, that is, including TAVdil and BAVdil patients. Therefore, we speculated that the decrease in the measured levels of alpha-Tocopherol could occur because of cellular and molecular events related to pathogenesis of BAV and vascular wall remodeling associated with dilation of the ascending aorta, rather than as a consequence of the bicuspid morphology of the aortic valve itself. BAV patients normally present increased, even not clinically significant, diameters of the ascending aorta than healthy TAV ones (32.56 ± 0.4 and 30.81 ± 0.6 p = 0.003, respectively; Table 1) and according to reported in [32]. However, histological differences exist in the dilated ascending aorta between BAV and TAV patients and several studies have determined that the inherent defects of the aortas in BAV patients lead to altered wall mechanical properties, which might contribute to the progressive dilation of the ascending aorta [33,34].
Using the alpha-Tocopherol levels together with the variables associated with the bicuspid morphology of the aortic valve, that is, the levels of EMPs and CRP, we constructed a model that significantly classified individuals depending on the morphology of the aortic valve. Interestingly, alpha-Tocopherol was identified as the most important variable. Therefore, measuring the levels of alpha-Tocopherol together with the parameters associated with inflammation and endothelial damage might be useful as a more feasible alternative for BAV screening and could be complementary to echocardiogram examination in large populations, as well as being useful in risk stratification of patients susceptible to developing ascending aortic dilation.
However, considering that the alpha-Tocopherol is functionally related to lipid and lipoprotein metabolism, we must consider whether the endothelial damage and pro-inflammatory state observed in BAV patients, especially in BAV patients with ascending aorta dilation, could be a consequence not only of hemodynamic forces and shear stress due to the bicuspid morphology of the aortic valve but also of an alteration to lipid and lipoprotein metabolism. In support of this hypothesis, selected authors have suggested that several molecular mechanisms that promote atherosclerosis are also present in BAV and that these alterations could underlie the progression of aortic stenosis and dilation [35]. The results reported in this study supported the hypothesis that BAV and dilation of the ascending aorta are associated with increased endothelial damage and inflammation. However, although the results presented in this study support the hypothesis that the lipid and lipoprotein metabolism might play an important role in BAV disease, we cannot establish causality.
Accordingly, additional studies are necessary to further evaluate whether different lipoproteins profiles in plasma affect the endothelium in BAV patients depending on susceptibility to developing ascending aorta dilation. Additionally, further research is warranted to determine whether alpha-Tocopherol administration might influence the progression of BAV pathology.
Abbreviations
| Tricuspid aortic valve | TAV |
| Tricuspid aortic valve with ascending aortic dilation | TAVdil |
| Bicuspid aortic valve | BAV |
| Bicuspid aortic valve with ascending aortic dilation | BAVdil |
| endothelial microparticles | EMPs |
| C-reactive protein | CRP |
| apolipoprotein A1 | ApoA1 |
| apolipoprotein B100 | ApoB100 |
Limitations
We excluded from the analysis patients with diabetes mellitus and those receiving certain pharmacological treatments such as statins, ACE inhibitors/ARBs and beta-blockers, to minimize the possibility that the excluded variables could influence the identification of related metabolites with the BAV. Subsequent studies carried out in a large population including the excluded variables should validate the generalization of our results.
Author Contributions
Conceptualization, N.M.-M. and J.M.A.; Data curation, C.L., A.J. and O.Y.; Formal analysis, N.M.-M.; Validation, B.A.-G.; Funding acquisition, JM.A.; Investigation, N.M.-M. and J.M.A.; Methodology, A.J., O.Y. and N.M.-M.; Supervision, JM.A.; Writing—original draft, B.A.-G., N.M.-M. and J.M.A.; Writing—review & editing, N.M.-M. and J.M.A. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by funds from the Sociedad Española de Cardiología (SEC).
Conflicts of Interest
The authors have declared that no competing interest exists.
References
- 1.Hoffman J.I.E., Kaplan S. The incidence of congenital heart disease. J. Am. Coll. Cardiol. 2002;39:1890–1900. doi: 10.1016/S0735-1097(02)01886-7. [DOI] [PubMed] [Google Scholar]
- 2.Cecconi M., Nistri S., Quarti A., Manfrin M., Colonna P.L., Molini E., Perna G.P. Aortic dilatation in patients with bicuspid aortic valve. J. Cardiovasc. Med. 2006;7:11–20. doi: 10.2459/01.JCM.0000199777.85343.ec. [DOI] [PubMed] [Google Scholar]
- 3.Evangelista A., Gallego P., Calvo-Iglesias F., Bermejo J., Robledo-Carmona J., Sánchez V., Saura D., Arnold R., Carro A., Maldonado G., et al. Anatomical and clinical predictors of valve dysfunction and aortic dilation in bicuspid aortic valve disease. Heart. 2018;104:566–573. doi: 10.1136/heartjnl-2017-311560. [DOI] [PubMed] [Google Scholar]
- 4.Rodríguez-Palomares J.F., Dux-Santoy L., Guala A., Kale R., Maldonado G., Teixidó-Turà G., Galian L., Huguet M., Valente F., Gutiérrez L., et al. Aortic flow patterns and wall shear stress maps by 4D-flow cardiovascular magnetic resonance in the assessment of aortic dilatation in bicuspid aortic valve disease. J. Cardiovasc. Magn. Reson. 2018;20:28. doi: 10.1186/s12968-018-0451-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van de Pol V., Kurakula K., DeRuiter M.C., Goumans M.J. Thoracic aortic aneurysm development in patients with bicuspid aortic valve: What is the role of endothelial cells? Front. Physiol. 2017;8:938. doi: 10.3389/fphys.2017.00938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ali O.A., Chapman M., Nguyen T.H., Chirkov Y.Y., Heresztyn T., Mundisugih J., Horowitz J.D. Interactions between inflammatory activation and endothelial dysfunction selectively modulate valve disease progression in patients with bicuspid aortic valve. Heart. 2014;100:800–805. doi: 10.1136/heartjnl-2014-305509. [DOI] [PubMed] [Google Scholar]
- 7.Girdauskas E., Kaemmerer H., von Kodolitsch Y. Unravelling the Pathogenetic Mechanisms in Congenital Aortopathies: Need for an Integrative Translational Approach. J. Clin. Med. 2020;9:204. doi: 10.3390/jcm9010204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheng M.-L., Wang C.-H., Shiao M.-S., Liu M.-H., Huang Y.-Y., Huang C.-Y., Mao C.-T., Lin J.-F., Ho H.-Y., Yang N.-I. Metabolic Disturbances Identified in Plasma Are Associated With Outcomes in Patients With Heart Failure. J. Am. Coll. Cardiol. 2015;65:1509–1520. doi: 10.1016/j.jacc.2015.02.018. [DOI] [PubMed] [Google Scholar]
- 9.Alegret J.M., Martínez-Micaelo N., Aragonès G., Beltrán-Debón R. Circulating endothelial microparticles are elevated in bicuspid aortic valve disease and related to aortic dilation. Int. J. Cardiol. 2016;217:35–41. doi: 10.1016/j.ijcard.2016.04.184. [DOI] [PubMed] [Google Scholar]
- 10.Martínez-Micaelo N., Beltrán-Debón R., Baiges I., Faiges M., Alegret J.M. Specific circulating microRNA signature of bicuspid aortic valve disease. J. Transl. Med. 2017;15:76. doi: 10.1186/s12967-017-1176-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martínez-Micaelo N., Beltrán-Debón R., Aragonés G., Faiges M., Alegret J.M. MicroRNAs Clustered within the 14q32 Locus Are Associated with Endothelial Damage and Microparticle Secretion in Bicuspid Aortic Valve Disease. Front. Physiol. 2017;8:648. doi: 10.3389/fphys.2017.00648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alegret J.M., Palazón O., Duran I., Vernis J.M. Aortic valve morphology definition with transthoracic combined with transesophageal echocardiography in a population with high prevalence of bicuspid aortic valve. Int. J. Cardiovasc. Imaging. 2005;21:213–217. doi: 10.1007/s10554-004-3901-9. [DOI] [PubMed] [Google Scholar]
- 13.Gleeson T.G., Mwangi I., Horgan S.J., Cradock A., Fitzpatrick P., Murray J.G. Steady-state free-precession (SSFP) cine MRI in distinguishing normal and bicuspid aortic valves. J. Magn. Reson. Imaging. 2008;28:873–878. doi: 10.1002/jmri.21547. [DOI] [PubMed] [Google Scholar]
- 14.Smith C.A., Want E.J., O’Maille G., Abagyan R., Siuzdak G. XCMS: Processing Mass Spectrometry Data for Metabolite Profiling Using Nonlinear Peak Alignment, Matching, and Identification. Anal. Chem. 2006;78:779–787. doi: 10.1021/ac051437y. [DOI] [PubMed] [Google Scholar]
- 15.Vinaixa M., Samino S., Saez I., Duran J., Guinovart J.J., Yanes O. A Guideline to Univariate Statistical Analysis for LC/MS-Based Untargeted Metabolomics-Derived Data. Metabolites. 2012;2:775–795. doi: 10.3390/metabo2040775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Costa C., Maraschin M., Rocha M. An R package for the integrated analysis of metabolomics and spectral data. Comput. Methods Programs Biomed. 2016;129:117–124. doi: 10.1016/j.cmpb.2016.01.008. [DOI] [PubMed] [Google Scholar]
- 17.Wiener AL and, M. Classification and Regression by randomForest. R News 2. [(accessed on 2 July 2020)];2003 Available online: http://www.stat.berkeley.edu/
- 18.Sophocleous F., Milano E.G., Pontecorboli G., Chivasso P., Caputo M., Rajakaruna C., Bucciarelli-Ducci C., Emanueli C., Biglino G. Enlightening the Association between Bicuspid Aortic Valve and Aortopathy. J. Cardiovasc. Dev. Dis. 2018;5:21. doi: 10.3390/jcdd5020021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Braverman A.C., Güven H., Beardslee M.A., Makan M., Kates A.M., Moon M.R. The bicuspid aortic valve. Curr. Probl. Cardiol. 2005;30:470–522. doi: 10.1016/j.cpcardiol.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 20.Liu T., Xie M., Lv Q., Li Y., Fang L., Zhang L., Deng W., Wang J. (2019) Bicuspid aortic valve: An update in morphology, genetics, biomarker, complications, imaging diagnosis and treatment. Front. Physiol. 2019;9:1921. doi: 10.3389/fphys.2018.01921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Della Corte A., Michelena H.I., Citarella A., Votta E., Piatti F., Lo Presti F., Ashurov R., Cipollaro M., Forte A. Risk Stratification in Bicuspid Aortic Valve Aortopathy: Emerging Evidence and Future Perspectives. Curr. Probl. Cardiol. 2019 doi: 10.1016/j.cpcardiol.2019.06.002. [DOI] [PubMed] [Google Scholar]
- 22.Gertsman I., Barshop B.A. Promises and pitfalls of untargeted metabolomics. J. Inherit. Metab. Dis. 2018;41:355–366. doi: 10.1007/s10545-017-0130-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Behrens W.A., Thompson J.N., Madère R. Distribution of α-tocopherol in human plasma lipoproteins. Am. J. Clin. Nutr. 1982;35:691–696. doi: 10.1093/ajcn/35.4.691. [DOI] [PubMed] [Google Scholar]
- 24.Fanali G., Fasano M., Ascenzi P., Zingg J.M., Azzi A. α-Tocopherol binding to human serum albumin. BioFactors. 2013;39:294–303. doi: 10.1002/biof.1070. [DOI] [PubMed] [Google Scholar]
- 25.Efrat M., Aviram M. Paraoxonase 1 interactions with HDL, antioxidants and macrophages regulate atherogenesis—A protective role for HDL phospholipids. Adv. Exp. Med. Biol. 2010;660:153–166. doi: 10.1007/978-1-60761-350-3_14. [DOI] [PubMed] [Google Scholar]
- 26.Wallert M., Schmölz L., Galli F., Birringer M., Lorkowski S. Regulatory metabolites of vitamin E and their putative relevance for atherogenesis. Redox Biol. 2014;2:495–503. doi: 10.1016/j.redox.2014.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang W., Maimaiti A., Zhao Y., Zhang L., Tao H., Nian H., Xia L., Kong B., Wang C., Liu M., et al. Analysis of Serum Metabolites to Diagnose Bicuspid Aortic Valve. Sci. Rep. 2016;6:37023. doi: 10.1038/srep37023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhu J., Wu Y., Tang Q., Leng Y., Cai W. The effects of choline on hepatic lipid metabolism, mitochondrial function and antioxidative status in human hepatic C3A cells exposed to excessive energy substrates. Nutrients. 2014;6:2552–2571. doi: 10.3390/nu6072552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zeisel S. Choline, Other Methyl-Donors and Epigenetics. Nutrients. 2017;9:445. doi: 10.3390/nu9050445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Corbin K.D., Zeisel S.H. Choline metabolism provides novel insights into nonalcoholic fatty liver disease and its progression. Curr. Opin. Gastroenterol. 2012;28:159–166. doi: 10.1097/MOG.0b013e32834e7b4b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu L., Lu Y., Bi X., Xu M., Yu X., Xue R. Choline ameliorates cardiovascular damage by improving vagal activity and inhibiting the inflammatory response in spontaneously hypertensive rats. Sci. Rep. 2017;7:1–13. doi: 10.1038/srep42553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Keane M.G., Wiegers S.E., Plappert T., Pochettino A., Bavaria J.E., St John Sutton M.G. Bicuspid aortic valves are associated with aortic dilatation out of proportion to coexistent valvular lesions. Circulation. 2000;102:Iii-35–Iii-39. doi: 10.1161/01.CIR.102.suppl_3.III-35. [DOI] [PubMed] [Google Scholar]
- 33.Meierhofer C., Schneider E.P., Lyko C., Hutter A., Martinoff S., Markl M., Hager A., Hess J., Stern H., Fratz S. Wall shear stress and flow patterns in the ascending aorta in patients with bicuspid aortic valves differ significantly from tricuspid aortic valves: A prospective study. Eur. Heart J. Cardiovasc. Imaging. 2013;14:797–804. doi: 10.1093/ehjci/jes273. [DOI] [PubMed] [Google Scholar]
- 34.Pasta S., Rinaudo A., Luca A., Pilato M., Scardulla C., Gleason T.G., Vorp D.A. Difference in hemodynamic and wall stress of ascending thoracic aortic aneurysms with bicuspid and tricuspid aortic valve. J. Biomech. 2013;46:1729–1738. doi: 10.1016/j.jbiomech.2013.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Magni P. Bicuspid aortic valve, atherosclerosis and changes of lipid metabolism: Are there pathological molecular links? J. Mol. Cell. Cardiol. 2019;129:231–235. doi: 10.1016/j.yjmcc.2019.03.004. [DOI] [PubMed] [Google Scholar]