Abstract
Purpose
To determine the clinical and genetic characteristics of patients with GUCY2D-associated retinal disorder (GUCY2D-RD).
Methods
Fifteen patients from 12 families with inherited retinal disorder (IRD) and harboring GUCY2D variants were ascertained from 730 Japanese families with IRD. Comprehensive ophthalmological examinations, including visual acuity (VA) measurement, retinal imaging, and electrophysiological assessment were performed to classify patients into three phenotype subgroups; macular dystrophy (MD), cone-rod dystrophy (CORD), and Leber congenital amaurosis (LCA). In silico analysis was performed for the detected variants, and the molecularly confirmed inheritance pattern was determined (autosomal dominant/recessive [AD/AR]).
Results
The median age of onset/examination was 22.0/38.0 years (ranges, 0-55 and 1-73) with a median VA of 0.80/0.70 LogMAR units (ranges, 0.00-1.52 and 0.10-1.52) in the right/left eye, respectively. Macular atrophy was identified in seven patients (46.7%), and two had diffuse fundus disturbance (13.3%), and six had an essentially normal fundus (40.0%). There were 11 patients with generalized cone-rod dysfunction (78.6%), two with entire functional loss (14.3%), and one with confined macular dysfunction (7.1%). There were nine families with ADCORD, one with ARCORD, one with ADMD, and one with ARLCA. Ten GUCY2D variants were identified, including four novel variants (p.Val56GlyfsTer262, p.Met246Ile, p.Arg761Trp, p.Glu874Lys).
Conclusions
This large cohort study delineates the disease spectrum of GUCY2D-RD. Diverse clinical presentations with various severities of ADCORD and the early-onset severe phenotype of ARLCA are illustrated. A relatively lower prevalence of GUCY2D-RD for ADCORD and ARLCA in the Japanese population was revealed.
Translational Relevance
The obtained data help to monitor and counsel patients, especially in East Asia, as well as to design future therapeutic approaches.
Keywords: macular dystrophy, cone rod dystrophy, GUCY2D, autosomal dominant, Leber congenital amaurosis
Introduction
Inherited retinal disorder (IRD) is a leading cause of blindness,1 and includes disorders such as retinitis pigmentosa (RP), cone/cone-rod dystrophy (CORD), macular dystrophy (MD), Stargardt disease (STGD), Leber congenital amaurosis (LCA) and others.1–6 IRD is characterized by heterogeneity both in the clinical and genetic aspects, with different inheritance patterns, including autosomal dominant (AD), autosomal recessive (AR), X-linked, and mitochondrial inheritance.7–9 Significant clinical and genetic overlap is well-known in the spectrum of IRD, and diverse clinical phenotypes, including CORD, MD, STGD, RP, and LCA, can manifest as a result of pathogenic variants in a single gene (e.g., ABCA4, BEST1, PRPH2, RPGR, CRX, GUCY2D, RS1, POC1B, PROM1, CNGA3, CNGB3).2,3,7,8,10–18
GUCY2D, denoted as guanylate cyclase 2D (OMIM: 600179), is located on 17p13.1 and contains 20 exons and encodes one of the two retinal membrane guanylyl cyclase isozymes expressed in photoreceptors.19,20 Retinal membrane guanylyl cyclase isozymes synthesize the intracellular messenger of photoreceptor excitation, cyclic guanosine monophosphate, which is regulated by the intracellular Ca2+-sensor proteins of guanylate cyclase-activating proteins.19–26 RetGCs and guanylate cyclase-activating proteins are responsible for the Ca2+ -sensitive restoration of cyclic guanosine monophosphate levels after the light activation of the phototransduction cascade.26
A locus and gene for LCA was first mapped and identified as GUCY2D (LCA1) in 1995 and 1996.19,27 Since then, more than 200 variants in the GUCY2D gene have been associated with a wide range of different phenotypes of IRDs.9,19,20,28–39 Sharon et al. reported that 88% of GUCY2D-associated retinal disorder (GUCY2D-RD) is AR-LCA, whereas pathogenic heterozygous missense GUCY2D variants cause AD-CORD.20 In that, pathogenic GUCY2D variants are one of the major causes of LCA, as well as a major cause of AD-CORD.20 Recently, Stunkel et al. identified five patients with AR congenital night blindness caused by biallelic GUCY2D variants, which may slowly progress to mild retinitis pigmentosa.40 Thus, AR-LCA, AD-CORD, and AR congenital night blindness are the main clinical presentations of GUCY2D-RD.
Studies of GUCY2D-RD have been conducted separately for each phenotype, such as CORD or RP/LCA; thus, it has been hard to comprehensively understand the disorder with diverse clinical manifestations and different modes of inheritance. To grasp the whole picture of GUCY2D-RD, large cohort studies with standardized clinical and genetic investigations for IRD in total are required.
The purpose of this study was to characterize the clinical and molecular genetic features of GUCY2D-RD in a large nationwide cohort of Japanese subjects diagnosed with IRD.
Methods
The protocol of this study followed the tenets of the Declaration of Helsinki. Informed consent was obtained from all affected subjects and unaffected subjects after explanation of the nature and possible consequences of the study. This research was approved by the Institutional Review Board of the National Institute of Sensory Organs, National Hospital Organization Tokyo Medical Center (Reference R18-029).
Participants from the Japan Eye Genetics Consortium Study
Participants with a clinical diagnosis of IRD and available genetic data by whole-exome sequencing (WES) were studies between 2008 and 2018 as part of the Japan Eye Genetics Consortium Study (JEGC studies; http://www.jegc.org/) conducted in collaboration of 38 institutes all over Japan.41 A total of 1294 subjects from 730 families were reviewed, including 30 families with AD-CORD/MD/STGD (defined as families with clear AD family history) and 41 families with AR or sporadic LCA.
Clinical Examinations
A detailed history was obtained in all affected subjects and unaffected family members (where available). The onset of disease was defined as the age when any visual symptom was first noted by patients or parents or when the subject was first diagnosed. The duration of disease was defined as the time between the onset of disease and the latest examination.
Comprehensive ophthalmological investigations were performed, including measurements of the best-corrected decimal visual acuity (BCVA) converted to the logarithm of the minimum angle of resolution (LogMAR) units, ophthalmoscopy, fundus photography, fundus autofluorescence (FAF) imaging, spectral-domain optical coherence tomography (SD-OCT), visual field testing, and electrophysiological assessments mainly according to the international standards of the International Society for Clinical Electrophysiology of Vision.42–45
Phenotype Subgroup
For the purpose of this study, the phenotype subgroup was defined based on clinical findings such as disease onset, symptoms, natural course, affected part on retinal imaging, the pattern of retinal dysfunction, and the history and phenotype of affected family members, partially according to the previous report13: LCA (including early-onset RP), a severe retinal dystrophy with early onset (<10 years) and complete loss of retinal function; RP (including rod-cone dystrophy), a progressive retinal dystrophy initially often affecting the peripheral retina with generalized rod dysfunction; CORD, a progressive retinal dystrophy initially often affecting the macula with generalized cone dysfunction; MD, a progressive retinal dystrophy presenting macular atrophy with confined macular dysfunction despite no abnormal generalized retinal function; and SNB, a stationary night blindness presenting congenital or early-onset night blindness, often affecting generalized rod function despite essentially normal visual acuity (VA) and no atrophy.
GUCY2D Variant Detection
Genomic DNA was extracted from affected subjects and unaffected family members (where available for cosegregation analysis). WES with target analysis of 301 retinal disease-associated genes (RetNET) was performed based on the previously published method and through the Phenopolis platform.41,46 The identified variants were filtered with the allele frequency (less than 1%) of the Human Genetic Variation Database (HGVD), which provides the allele frequency of the general Japanese population. Depth and coverage for the target exons were examined with the integrative Genomics Viewer.
Disease-causing variants were determined from the detected variants in the 301 retinal-disease-associated genes, considering the clinical findings of the affected subjects, the pattern of inheritance in the pedigree, and the results of cosegregation analysis.
In Silico Molecular Genetic Analysis
Sequence variant nomenclature was performed according to the guidelines of the Human Genome Variation Society (HGVS). The allele frequency of all detected GUCY2D variants in the HGVD, Integrative Japanese Genome Variation (iJGVD 2k), the 1000 Genomes Project, and the genome Aggregation Database (gnomAD) was established according to the previous method.41
All detected GUCY2D variants were analyzed with the following prediction programs; MutationTaster, FATHMM, SIFT, PROVEAN, and PolyPhen-2. Evolutional conservation scores were calculated for all detected GUCY2D variants by the UCSC database. Pathogenicity classification of all detected GUCY2D variants was performed based on the guidelines of the American College of Medical Genetics and Genomics.47
Results
Participants
Fifteen affected subjects from 12 families with a clinical diagnosis of IRD and harboring GUCY2D variants were ascertained. The detailed demographic features and summarized genetic results are provided in Table 1, and the pedigrees of 12 families are shown in Figure 1.
Table 1.
Demographic Features of 15 Japanese Patients from 12 Families with GUCY2D-Associated Retinal Disorder (GUCY2D-RD)
| Refraction | LogMAR VA | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Family No. | Patient No. | Inheritance | Sex | Age (at Latest Examination) | Onset | Chief Complaint | Other ocular symptoms | RE | LE | RE | LE | Phenotype Subgroup | Inheritance Suggested by Molecular genetic diagnosis | Genotype |
| 1 (MU01) | 1-II:2 (Patient 1) | Sporadic | F | 1 | 0 | Reduced visual acuity/poor visual acuity | Nystagmus | NA | NA | NA | NA | LCA | AR | c.167_168delTG, p.Val56GlyfsTer262; c.738G>C, p.Met246Ile |
| 2 (TMC01) | 2-II:2 (Patient 2) | Sporadic | M | 12 | 3 | Reduced visual acuity/ poor visual acuity | Night blindness | −1 | −1 | 0.22 | 0.22 | CORD (moderate) | AR | c.238_252del, p.Ala80_Leu84del; c.2620G>A, p.Glu874Lys |
| 3 (NU01) | 3-II:7 (Patient 3) | Sporadic | M | 73 | NA | Night blindness | NA | +1.5 | +3.5 | 1 | 1.52 | CORD (severe) | AD | c.2281C>T, p.Arg761Trp |
| 4 (KDU01) | 4-III:1 (Patient 4) | AD | M | 30 | 23 | Reduced visual acuity/ poor visual acuity | NA | −2.5 | 2.5 | 0.82 | 0.82 | CORD (moderate) | AD | c.2512C>T, p.Arg838Cys |
| 4 (KDU01) | 4-II:2 (Patient 5) | AD | F | 61 | 21 | Reduced visual acuity/ poor visual acuity | Photophobia | −1.5 | −1.5 | 1.05 | 1.05 | CORD (moderate) | AD | c.2512C>T, p.Arg838Cys |
| 5 (GU01) | 5-III:5 (Patient 6) | AD | F | 31 | 18 | Reduced visual acuity/ poor visual acuity | Photophobia | −7 | −7 | 0 | 0.1 | CORD (mild) | AD | c.2513G>A, p.Arg838His |
| 6 (TMC02) | 6-III:1 (Patient 7) | AD | M | 38 | 7 | Reduced visual acuity/ poor visual acuity | Photophobia | −5 | −5 | 1.52 | 1.52 | CORD (severe) | AD | c.2513G>A, p.Arg838His |
| 7 (JU01) | 7-II:5 (Patient 8) | AD | F | 36 | 35 | Reduced visual acuity/ poor visual acuity | NA | −6 | −6.5 | 0.22 | 0.52 | CORD (mild) | AD | c.2513G>A, p.Arg838His |
| 7 (JU01) | 7-II:3 (Patient 9) | AD | F | 43 | 30 | Reduced visual acuity/ poor visual acuity | NA | −6 | −6.5 | 0.7 | 0.7 | CORD (moderate) | AD | c.2513G>A, p.Arg838His |
| 7 (JU01) | 7-I:2 (Patient 10) | AD | M | 68 | NA | NA | NA | +1 | −2 | 0.82 | 1 | CORD (NA) | AD | c.2513G>A, p.Arg838His |
| 8 (JU02) | 8-II:2 (Patient 11) | Sporadic | M | 23 | 23 | Photophobia | Color vision abnormality | −11.5 | −11.5 | 0.15 | 0.15 | CORD (mild) | AD (de novo) | c.2513G>A, p.Arg838His |
| 9 (KDU02) | 9-III:3 (Patient 12) | Sporadic | M | 64 | 41 | Reduced visual acuity/ poor visual acuity | NA | NA | NA | NA | NA | CORD (NA) | AD | c.2521G>A, p.Glu841Lys |
| 10 (TMC03) | 10-II:2 (Patient 13) | Sporadic | M | 10 | 0 | Reduced visual acuity/ poor visual acuity | Photophobia | +1.5 | +1.5 | 1 | 1 | CORD (moderate) | AD (de novo) | c.2704G>T, p.Val902Leu |
| 11 (NU02) | 11-II:2 (Patient 14) | Sporadic | M | 43 | NA | Reduced visual acuity/ poor visual acuity | Central visual field loss | −10 | −12 | 0.8 | 0.6 | CORD (moderate) | AD | c.2747T>C, p.Ile916Thr |
| 12 (MU02) | 12-II:5 (Patient 15) | Sporadic | F | 71 | 55 | Reduced visual acuity/ poor visual acuity | Photophobia | 0 | 0 | 0.52 | 0.52 | MD | AD | c.2747T>C, p.Ile916Thr |
AD, autosomal dominant; AR, autosomal recessive; CORD, cone rod dystrophy; F, female; LCA, Leber congenital amaurosis; LE, left eye; M, male; NA, not available; RE, right eye; LogMAR VA, best corrected logarithm of the minimum angle of resolution visual acuity; MD, macular dystrophy.
Autosomal dominant family history (at least having two affected subjects in two consecutive generations) was clearly reported in four families. Age described in the column was defined as the age when the latest examination was performed. The age of onset was defined as either the age at which visual loss was first noted by the patient or, in the “asymptomatic” patients, when an abnormal retinal finding was first detected. Patients 10 and 14 had cataract.
The phenotype subgroup was defined based on clinical findings, such as disease onset, symptoms, natural course, affected part on retinal imaging, the pattern of retinal dysfunction, and the history and phenotype of affected family members, partially according to the previous report: LCA (including early-onset RP), a severe retinal dystrophy with early-onset (<10 years) and complete loss of retinal function; RP (including rod-cone dystrophy), a progressive retinal dystrophy initially often affecting the peripheral retina with generalized rod dysfunction; CORD, a progressive retinal dystrophy initially often affecting the macula with generalized cone dysfunction; MD, a progressive retinal dystrophy presenting macular atrophy with confined macular dysfunction despite no abnormal generalized retinal function; and SNB, a stationary night blindness presenting congenital or early-onset night blindness often affecting generalized rod function despite essentially normal visual acuity and no atrophy.
There were two severe CORD subjects with poor VA and severe retinal dysfunction (patients 3, 7), six moderate CORD subjects with intermediate severity of VA or retinal function (patients 2, 4, 5, 9, 13, 14), and three mild CORD subjects with relatively favorable VA and relatively preserved generalized rod function (patients 6, 8, 11). Two subjects with CORD were unavailable for severity assessment due to unavailable VA or electrophysiological data.
Sequence variant nomenclature was performed according to the guidelines of the Human Genome Variation Society.
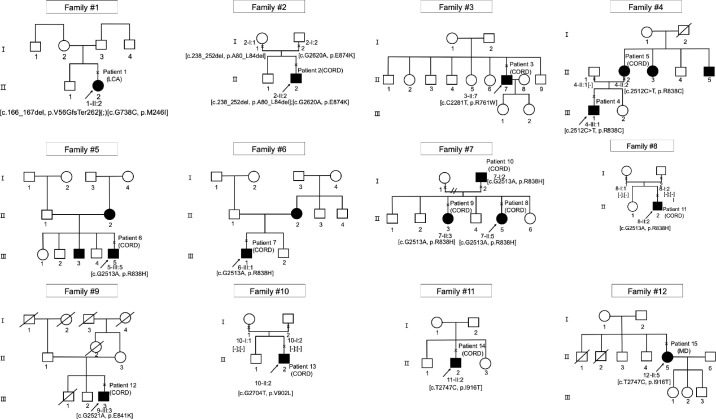
Figure 1.
Pedigrees of 12 Japanese families with inherited retinal disorder harboring GUCY2D variants. The solid squares and circles (men and women, respectively) represent the affected subjects and the white icons represent the unaffected family members. The slash symbol indicates deceased individuals. The generation number is noted on the left. The proband is marked by an arrow; the clinically investigated individuals are indicated by a cross.
All affected and unaffected subjects were Japanese, and any mixture with other ethnicity was not reported. There were four families with clear AD family history (4/12, 33.3%; families 4–7), and eight sporadic families with no affected family members than the proband (8/12, 66.7%; families 1–3, 8–12). There were four families with unknown familial information (families 3, 9, 11, 12). Consanguineous marriage was not reported in any of the 12 families.
There were five affected females (5/15, 33.3%) and 10 affected males (10/15, 66.7%). The median age at the latest examination of the 15 affected subjects was 38.0 years (range, 1–73).
Onset, Chief Complaint, and Visual Acuity
The median age of onset and duration of disease of the 12 affected subjects with available records was 22.0 years (range, 0–55), and 11.5 years (range, 1–40), respectively.
Four subjects had childhood-onset of 15 years or earlier (4/12, 33.3%; patients 1, 2, 7, 13). Later onset of disease (45 years or later) was reported in one subject (1/12, 8.3%; patient 15).
Reduced visual acuity/poor visual acuity was reported as a chief complaint at the initial visit in 12 of 14 affected subjects with available records (12/14, 85.7%; patients 1, 2, 4–9, 12–14,15), one with photophobia (1/14, 7.1%; patient 11), and one with night blindness (1/14, 7.1%; patient 3).
The median BCVA in the right and left eyes of the 12 affected subjects with available records was 0.80 (range, 0.00–1.52) and 0.70 (range, 0.10–1.52) LogMAR units, respectively. One of the two subjects with unavailable LogMAR VA testing had nystagmus (patient 1). Four subjects of 13 with available records had relatively favorable VA (4/13, 30.8%, patients 2, 6, 8, 11; 0.22 or better LogMAR units in the better eye), five subjects had intermediate VA (5/13, 38.5%, patients 4, 9, 10, 14, 15; between 0.22 and 1.0 LogMAR units in the better eye), and four subjects had poor VA (4/13, 30.8%; patients 3, 5, 7, 13; 1.0 or worse LogMAR units in the better eye).
Retinal Imaging and Morphological Findings
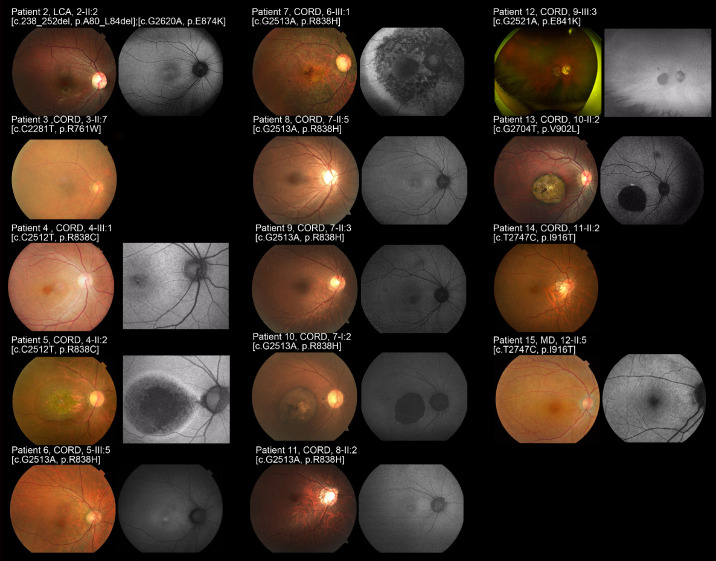
Fundus photographs were obtained in 14 affected subjects (patients 2–15), and FAF images were available in 12 affected subjects (patients 2, 4–13, 15). A description of funduscopy was available in one subject (patient 1). The representative images are presented in Figure 2, and the detailed findings are described in Table 2.
Figure 2.
Fundus photographs and fundus autofluorescence images of 14 patients with GUCY2D-associated retinal disorder (GUCY2D-RD; patients 2–15). Fundus photographs and fundus autofluorescence (FAF) images of the right eyes demonstrated macular atrophy in seven affected subjects (patients 4, 5, 7, 9, 10, 12, 13) with intrachoroidal cavitation in three subjects (patients 5, left; 10, left; 13) and slight fine dots at the macula in two subjects (patients 4, 9). Atrophic change at the posterior pole extending to the periphery was observed in patient 7 and subtle diffuse disturbance at the posterior pole with vessel attenuation was found in patient 7. Normal fundus appearance was noted in five subjects (patients 1, 2, 6, 8, 14). Patient 11 had essentially normal retinal appearance except for optic disk cupping. The atrophic changes were more evident on FAF images. A loss of AF signal at the macula was identified in five subjects (patients 5, 7, 10, 12, 13). Increased AF signal at the macula was observed in five subjects (patients 2, 4, 6, 8, 11). A patchy area of decreased AF signal at the posterior pole extending to the periphery surrounded by a ring of increased AF signal was found in patient 7.
Table 2.
Retinal Imaging and Morphological Findings of 15 Patients with GUCY2D-RD
| Fundus | FAF | SD-OCT | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient No. | Phenotype Subgroup | Macular Atrophy | Atrophy Along the Arcade | Peripheral Atrophy | Vessel Attenuation | Pigmentation | Comments | Area of Decreased Density at the Central Retina | Area of Increased Density at the Macula | Ring of Increased Density | Areas of Abnormal Density Along the Arcade | Areas of Abnormal Density Areas in the Periphery | Foveal Sparing Surrounded by Decreased Density at the Parafovea | Comments | Outer Retinal Disruption at the Fovea | Outer Retinal Disruption at the Parafovea | Increased Signal of the Choroid | EZ Preservation at the fovea (RE) | EZ Preservation at the fovea (LE) | Comments |
| 1 (MU01-01) | LCA | No | No | No | No | No | Funduscopy, normal | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | ||
| 2 (TMC01-01) | CORD | No | No | No | No | No | Normal | No | Yes | No | No | No | No | Slightly increased AF at the fovea | No | No | No | Yes | Yes | Loss of IZ at the macula |
| 3 (NU01-01) | CORD | No | No | No | Yes | No | Subtle diffuse disturbance at the posterior pole | NA | NA | NA | NA | NA | NA | No | Yes | No | Yes | Yes | Loss of IZ at the macula with ERM in the right eye | |
| 4 (KDU01-01) | CORD | Yes | No | No | No | No | Subtle fine dots at the macula | No | Yes | No | No | No | No | No | No | No | No | No | Loss of EZ/IZ at the fovea | |
| 5 (KDU01-02) | CORD | Yes | Yes | No | No | No | Intrachoroidal cavitaion in the left eye | Yes | No | Yes | No | No | No | Yes | Yes | Yes | No | No | Thinned sensory retina and loss of EZ/IZ at the macla; Intrachoroidal cavitaion at the left macula | |
| 6 (GU01-01) | CORD | No | No | No | No | No | Normal | No | Yes | No | No | No | No | Slightly increased AF at the fovea | No | No | No | Yes | Yes | Loss of IZ at the macula |
| 7 (TMC02-01) | CORD | Yes | Yes | Yes | Yes | Yes | Atrophic changes with at the posterior pole extended to the periphery | Yes | No | Yes | Yes | Yes | No | Yes | Yes | Yes | No | No | ||
| 8 (JU01-01) | CORD | No | No | No | No | No | Normal | No | Yes | Yes | No | No | No | Slightly increased AF at the fovea of the right eye | No | No | No | Yes | Yes | Loss of IZ at the macula |
| 9 (JU01-02) | CORD | Yes | No | No | No | No | Subtle fine dots at the macula | No | No | No | No | No | No | Slightly abnormal background | Yes | No | No | No | No | |
| 10 (JU01-03) | CORD | Yes | No | No | No | Yes | Pigmentation at the macula in both eyes, intrachoroidal cavitation in the left eye | Yes | No | No | No | No | No | Loss of AF signal at the macula | Yes | Yes | Yes | No | No | Intrachoroidal cavitation at the left macula. |
| 11 (JU02-01) | CORD | No | No | No | No | No | Essential normal except for optic disc cupping | No | Yes | No | No | No | Yes | No | No | No | Yes | Yes | Loss of IZ at the macula | |
| 12 (KDU02-01) | CORD | Yes | No | No | No | Yes | Yes | No | No | No | No | No | Artifact due to the medial condition | Yes | Yes | Yes | No | No | Thinned sensory retina and loss of EZ/IZ at the macula | |
| 13 (TMC03-01) | CORD | Yes | Yes | No | No | No | Intrachoroidal cavitation | Yes | No | No | No | No | No | Loss of AF signal at the macula | Yes | Yes | Yes | No | No | Thinned sensory retina/intrachoroidal cavitation at the macula |
| 14 (NU02-01) | CORD | No | No | No | No | No | Normal | NA | NA | NA | NA | NA | NA | No | No | No | No | No | Loss of EZ/IZ at the macula | |
| 15 (MU02-01) | MD | No | No | No | No | No | Subtle diffuse disturbance at the posterior pole | No | No | No | No | No | No | Slightly abnormal background | No | No | No | Yes | Yes | Loss of IZ at the macula |
BE, both eyes; EZ, ellipsoid zone; FAF, fundus autofluorescence; FS, foveal sparing; LE, left eye; M male; NA not available; RE, right eye; SD-OCT, spectral domain optical coherence tomography.
Foveal sparing was defined as remaining foveal AF signal surrounded by the area of decreased AF.
Macular atrophy was identified in seven affected subjects (7/15, 46.7%; patients 4, 5, 7, 9, 10, 12, 13), with intrachoroidal cavitation in three subjects (patients 5, 10, 13) and slight fine dots at the macula in two subjects (patients 4, 9). Atrophic change at the posterior pole extending to the periphery was observed in one subject (1/15, 6.7%; patient 7). Subtle diffuse disturbance at the posterior pole with vessel attenuation was found in two subjects (2/15, 13.3%; patients 3, 15). Normal fundus appearance was noted in five subjects (5/15, 33.3%; patients 1, 2, 6, 8, 14). One subject had a normal retinal appearance except for optic disk cupping (1/15, 6.7%, patient 11).
The retinal atrophy at the macula was more evident on FAF images, and the loss of AF signal at the macula was identified in five subjects (5/12, 41.7%, patients 5, 7, 10, 12, 13). Increased AF signal at the macula was observed in five subjects (5/12, 41.7%; patients 2, 4, 6, 8, 11), one of whom showed subtle fine dots at the macula and the other four subjects had no abnormal findings at the macula on fundus photography. One subject showed patchy areas of decreased AF signal at the posterior pole extending to the periphery (1/12, 8.3%; patient 7).
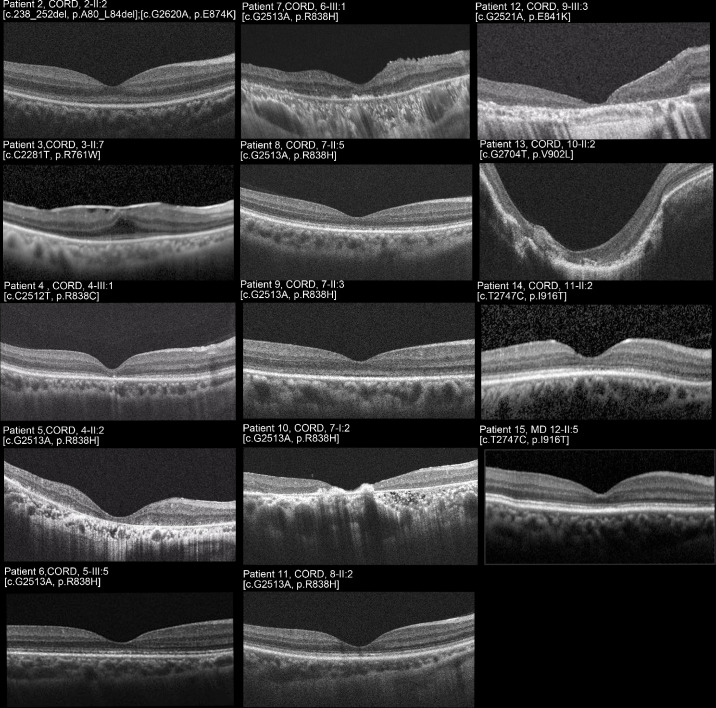
SD-OCT images were obtained in 14 affected subjects (patients 2–15), and the representative images are presented in Figure 3. One subject had an epiretinal membrane (patient 3, right). Outer retinal disruption at the fovea and/or parafovea was identified in six subjects (6/14, 42.9%; patients 5, 7, 9, 10, 12, 13), three of whom showed intrachoroidal cavitation (patients 5, left; 10, left; 13). A relatively preserved photoreceptor ellipsoid zone (EZ) line at the fovea was found in six subjects (6/14, 42.9%; patients 2, 3, 6, 8, 11, 15), one of whom showed outer retinal disruption at the parafovea (patient 3).
Figure 3.
Spectral-domain optical coherence tomographic images of 11 patients with GUCY2D-RD (patients 2, 3, 6–11, 13–15). Spectral-domain optical coherence tomography of the right eye demonstrated outer retinal disruption at the fovea in six subjects (patients 5, 7, 9, 10, 12, 13) and at the parafovea in six subjects (patients 3, 5, 7, 10, 12, 13) with intrachoroidal cavitation in one subject (patient 13, right). A relatively preserved photoreceptor ellipsoid zone (EZ) line at the fovea was found in six subjects (patients 2, 3, 6, 8, 11, 15), one of whom showed outer retinal disruption at the parafovea (patient 3). One subject had an epiretinal membrane (patient 3).
Visual Fields and Electrophysiological Findings
The detailed findings of visual fields and electrophysiological assessments are described in Table 3. Visual field testing was performed in nine affected subjects (patients 2, 4–9, 12, 13), with Goldmann perimetry (seven subjects) and Humphrey visual field analyzer (four subjects). Central scotoma was detected in eight subjects (8/9, 88.9%; patients 4–9, 12, 13) and paracentral scotoma was observed in all nine subjects (9/9; 100%). Peripheral visual loss was found in four subjects (4/9, 44.4%; patients 2, 5–7).
Table 3.
Visual fields, and Electrophysiological Assessments of 15 Patients with GUCY2D-RD
| Visual Fields | Electrophysiological Assessment | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Patient No. | Phenotype Subgroup | Method | Central Scotoma | Paracentral Scotoma | Peripheral Visual Field Loss | Comments | Responses in Dark-adapted Condition | Responses in Light-adapted Condition | Lower b to a Ratio in Dark-adapted Bright Flash Responses | Comments |
| 1 (MU01-01) | LCA | NA | NA | NA | NA | Undetectable | Undetectable | No | Skin electrodes | |
| 2 (TMC01-01) | CORD | GP | No | Yes | Yes | Paracentral relative scotoma | Severely decreased | Undetectable | No | |
| 3 (NU01-01) | CORD | NA | NA | NA | NA | Undetectable | Undetectable | No | Recorded in the right eye | |
| 4 (KDU01-01) | CORD | GP/HFA | Yes | Yes | No | WNL | Mildly decreased | NA | Reduced central responses in mfERGs | |
| 5 (KDU01-02) | CORD | GP/HFA | Yes | Yes | Yes | Mildly decreased | Undetectable | Yes | ||
| 6 (GU01-01) | CORD | HFA | Yes | Yes | Yes | Central and paracentral relative scotoma | Mildly decreased | Severely decreased | No | Reduced central responses in mfERGs |
| 7 (TMC02-01) | CORD | GP | Yes | Yes | Yes | Severely decreased | Undetectable | No | ||
| 8 (JU01-01) | CORD | GP | Yes | Yes | No | Mildly decreased | Severely decreased | No | ||
| 9 (JU01-02) | CORD | GP/HFA | Yes | Yes | No | Mildly decreased | Moderately decreased | No | ||
| 10 (JU01-03) | CORD | NA | NA | NA | NA | NA | NA | NA | ||
| 11 (JU02-01) | CORD | NA | NA | NA | NA | Mildly decreased | Undetectable | Yes | Reduced central responses in mfERGs | |
| 12 (KDU02-01) | CORD | GP | Yes | Yes | Yes | Moderately decreased | Severely decreased | No | ||
| 13 (TMC03-01) | CORD | GP | Yes | Yes | No | Moderately decreased | Undetectable | No | ||
| 14 (NU02-01) | CORD | NA | NA | NA | NA | Mildly decreased | Severely decreased | Yes | ||
| 15 (MU02-01) | MD | NA | NA | NA | NA | WNL | WNL | No | Reduced central responses in FMERG | |
FMERG, focal macular electroretinogram; GP, Goldmann kinetic perimetry; HFA, Humphry field analyzer; mfERG, multifocal electroretinogram; WNL, within normal limit.
Lower b to a ratio in dark-adapted bright flash responses was defined as less than 0.9.
Severity of electrophysiological responses were defined as follows; undetectable, more than 90% amplitude reduction compared to the normal reference; severely decreased response, between 90% and 75% amplitude reduction; moderately decreased response, between 75% and 50% amplitude reduction; mildly decreased responses, less than 50% amplitude reduction.
Full-field electroretinograms were recorded in 14 affected subjects (patients 2–9, 11–15). Multifocal ERGs (mfERGs) were recorded in three subjects (patients 4, 6, 11), and focal macular ERGs (FMERGs) were obtained in one subject (patient 15).
Undetectable light-adapted (LA) responses were demonstrated in seven subjects (7/14, 50.0%; patients 1–3, 5, 7, 11, 13), with undetectable dark-adapted (DA) responses in two subjects (patients 1, 3), severely decreased DA responses in two subjects (patients 2, 7), moderately decreased DA responses in one subject (patient 13), and mildly decreased DA responses in two subjects (patients 5, 11). Severely decreased LA responses were identified in four subjects (4/14, 28.6%; patients 6, 8, 12, 14), with moderately decreased DA responses in one subject (patient 12) and mildly decreased DA responses in three subjects (patients 6, 8, 14). Moderately decreased LA responses with mildly decreased DA responses were shown in one subject (1/14, 7.1%; patient 9). Mildly decreased LA responses with normal DA responses were found in one subject (1/14, 7.1%; patient 4). Normal responses both in LA and DA conditions were noted in one subject (1/14, 7.1%; patient 15). A lower b-to-a ratio (ratio of b wave to a wave for dark-adapted bright flash responses was less than 0.9) was observed in three subjects (3/14, 21.4%; patients 5, 11, 14). Reduced central responses were detected by mfERG in three subjects (patients 4, 6, 11), and reduced central focal responses were demonstrated by FMERGs in one subject (patient 15).
Generalized entire loss of function was identified in two subjects (2/14, 14.3%; patients 1, 3), generalized cone rod dysfunction was found in 11 subjects (11/14, 78.6%; patients 2, 4, 5–9, 11–14), and confined macular dysfunction was noted in one subject (1/14, 7.1%; patient 15).
Phenotype Subgroups
Phenotype subgroup classification was performed in all 15 affected subjects. There were 13 subjects with CORD (13/15, 86.7%; patients 2–14), one with MD (1/15, 6.7%; patient 15), and one with LCA (1/15, 6.7%; patient 1). There were no subjects with RP or SNB.
The mean age of onset of the 13 subjects with CORD/one with MD/one with LCA was 20.0 (range, 0-41)/55/0 years, with the mean duration of disease of 14.7 (range,0-40)/1.0/16.0 years, respectively. The mean VA for eyes with CORD/MD was 0.73 (range, 0.00-1.52)/0.52 in LogMAR units.
There were two severe CORD subjects with poor VA and severe retinal dysfunction (patients 3, 7), six moderate CORD subjects with intermediate severity of VA or retinal function (patients 2, 4, 5, 9, 13, 14), and three mild CORD subjects with relatively favorable VA and relatively preserved generalized rod function (patients 6, 8, 11). Two subjects with CORD were unavailable for severity assessment because of unavailable VA or electrophysiological data.
GUCY2D Variants
The variant data of 15 affected and seven unaffected subjects from 12 families are summarized in Table 4. Ten GUCY2D variants were identified in the heterozygous state: c.167_168delTG, p.Val56GlyfsTer262; c.238_252del, p.Ala80_Leu84del; c.738G>C, p.Met246Ile; c.2281C>T, p.Arg761Trp; c.2513G>A, p.Arg838His; c.2512C>T, p.Arg838Cys; c.2521G>A, p.Glu841Lys; c.2620G>A, p.Glu874Lys; c.2704G>T, p.Val902Leu; and c.2747T>C, p.Ile916Thr (NM_000180.3).
Table 4.
Summary of Detected Variants of 15 Affected and 7 Unaffected Subjects from 12 Families with GUCY2D-RD
| Family ID | Subject ID | Affected/Unaffected | Exon | Nucleotide and Amino Acid Changes | State |
|---|---|---|---|---|---|
| 1 (MU01) | 1-II:2 (patient 1) | Affected | 2 | c.167_168delTG, p.Val56GlyfsTer262 | Heterozygous |
| 3 | c.738G>C, p.Met246Ile | Heterozygous | |||
| 2 (TMC01) | 2-II:2 (patient 2) | Affected | 2 | c.238_252del, p.Ala80_Leu84del | Compound heterozygous |
| 14 | c.2620G>A, p.Glu874Lys | ||||
| 2-I:1 | Unaffected | 14 | c.2620G>A, p.Glu874Lys | Heterozygous | |
| 2-I:2 | Unaffected | 2 | c.226_240del, p.Ala76_Ala80del | Heterozygous | |
| 3 (NU01) | 3-II:7 (patient 3) | Affected | 12 | c.2281C>T, p.Arg761Trp | Heterozygous |
| 4 (KDU01) | 4-III:1 (patient 4) | Affected | 13 | c.2512C>T, p.Arg838Cys | Heterozygous |
| 4-II:2 (patient 5) | Affected | 13 | c.2512C>T, p.Arg838Cys | Heterozygous | |
| 4-II:1 | Unaffected | 13 | c.2512C>T, p.Arg838Cys | ND | |
| 5 (GU01) | 5-III:5 (patient 6) | Affected | 13 | c.2513G>A, p.Arg838His | Heterozygous |
| 6 (TMC02) | 6-III:1 (patient 7) | Affected | 13 | c.2513G>A, p.Arg838His | Heterozygous |
| 7 (JU01) | 7-II:5 (patient 8) | Affected | 13 | c.2513G>A, p.Arg838His | Heterozygous |
| 7-II:3 (patient 9) | Affected | 13 | c.2513G>A, p.Arg838His | Heterozygous | |
| 7-I:2 (patient 10) | Affected | 13 | c.2513G>A, p.Arg838His | Heterozygous | |
| 8 (JU02) | 8-II:2 (patient 11) | Affected | 13 | c.2513G>A, p.Arg838His | Heterozygous (de novo) |
| 8-I:2 | Unaffected | 13 | c.2513G>A, p.Arg838His | ND | |
| 8-I:1 | Unaffected | 13 | c.2513G>A, p.Arg838His | ND | |
| 9 (KDU02) | 9-III:3 (patient 12) | Affected | 13 | c.2521G>A, p.Glu841Lys | Heterozygous |
| 10 (TMC03) | 10-II:2 (patient 13) | Affected | 14 | c.2704G>T, p.Val902Leu | Heterozygous (de novo) |
| 10-I:2 | Unaffected | 14 | c.2704G>T, p.Val902Leu | ND | |
| 10-I:1 | Unaffected | 14 | c.2704G>T, p.Val902Leu | ND | |
| 11 (NU02) | 11-II:2 (patient 14) | Affected | 14 | c.2747T>C, p.Ile916Thr | Heterozygous |
| 12 (MU02) | 12-II:5 (patient 15) | Affected | 14 | c.2747T>C, p.Ile916Thr | Heterozygous |
GUCY2D transcript ID: NM_000180.3
ND, not detected
Novel variants are shown in italic.
Whole-exome sequencing with targeted analysis for retinal disease-causing genes on RetNET (https://sph.uth.edu/retnet/) was performed in 15 affected and 7 unaffected subjects from 12 families.
There were eight missense variants, one with a 2-bp deletion leading to a frame shift, and one with an in-frame deletion. Three variants were identified in multiple families: p.Arg838Cys (families 4, 5), p.Arg838His (families 6–8), and p.Ile916Thr (families 11, 12). Intrafamiliar cosegregation analysis was performed in five families (families 2, 4, 7, 8, 10), and the de novo (patient 11, p.Arg838His; patient 10, p.Val902Leu), compound heterozygous (patient 2; p.Ala80_Leu84del, p.Glu874Lys), and heterozygous (patient 4, p.Arg838Cys; patient 8, p.Arg838His; patient 11, p.Arg838His) states were confirmed.
GUCY2D-RD caused by six detected variants has been reported before: CORD for p.Ala80_Leu84del9; ADCORD for p.Arg838His;34,38 ADCORD for p.Arg838Cys,29,34 ADCORD for p.Glu841Lys,30 ADCORD for p.Val902Leu,31 ADCORD for p.Ile916Thr.32 Four variants have never been reported; p.Val56GlyfsTer262, p.Met246Ile, p.Arg761Trp, and p.Glu874Lys.
In Silico Molecular Genetic Analysis
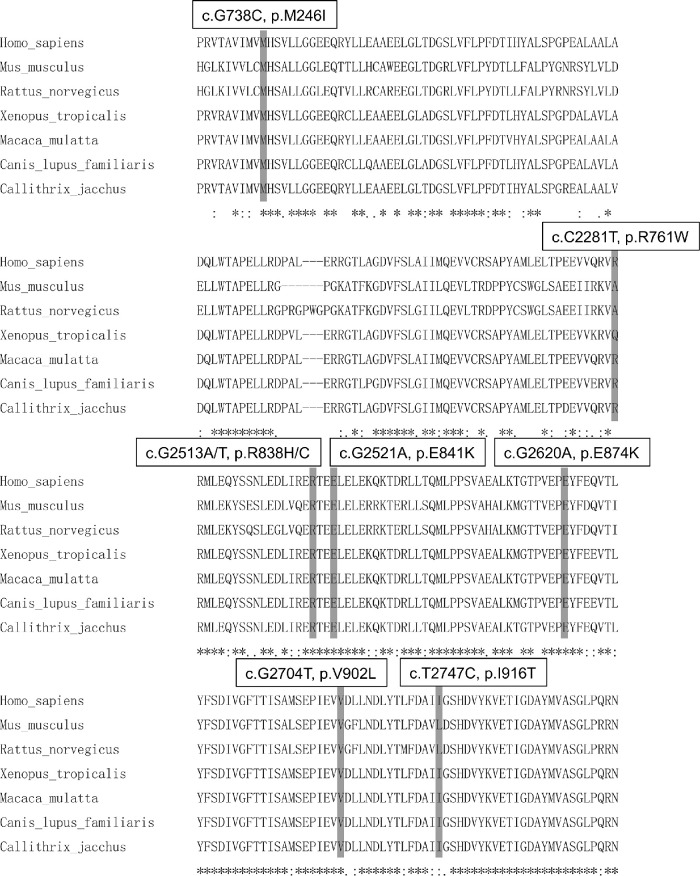
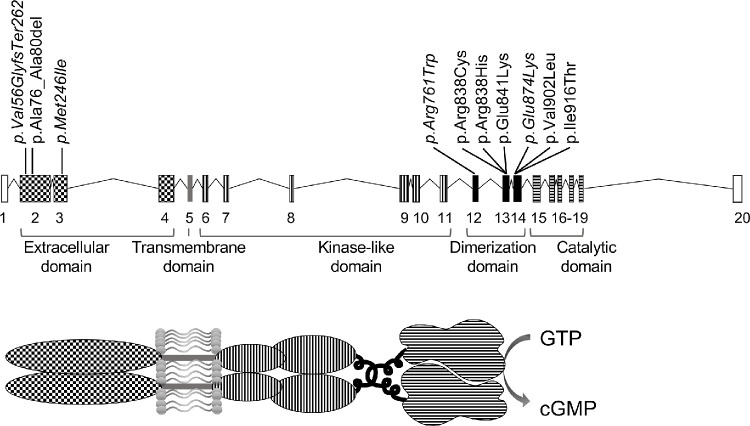
The detailed results of in silico molecular genetic analyses for the 10 detected GUCY2D variants are presented in Supplementary Tables S1 and S2. A schematic genetic and protein structure of GUCY2D and multiple alignments of eight species of GUCY2D are shown in Figures 4 and 5.
Figure 4.
Multiple alignment of eight species of GUCY2D. The alignment was performed with the Clustal Omega program (https://www.ebi.ac.uk/Tools/msa/clustalo/) and the amino-acid-sequence alignment was numbered in accordance with the Homo sapiens GUCY2D sequence (ENST00000254854.4). *Complete conservation across the eight species. The positions of eight missense variant residues are highlighted with gray background: p.Met246Ile, p.Arg761Trp, p.Arg838His, p.Arg838Cys, p.Glu841Lys, p.Glu874Lys, p.Val902Leu, and p.Ile916.
Figure 5.
A schematic genetic and protein structure of GUCY2D and the location of the detected variants. The GUCY2D gene (ENST00000254854.4) contains 20 exons that encode a protein containing an extracellular domain, transmembrane domain, kinase-like domain, dimerization domain, catalytic domain, and others (Lazar et al., 2014). The 10 variants detected in this study are presented. The four novel variants are shown: p.Val56GlyfsTer262, p.Met246Ile, p.Arg761Trp, and p.Glu874Lys.
Seven variants are located in exons 12-14 (p.Arg761Trp, p.Arg838His, p.Arg838Cys, p.Glu841Lys, p.Glu874Lys, p.Val902Leu, p.Ile916Thr), which are presumably associated with the dimerization domain in the GUCY2D protein, and the other missense variant was in exon 3, which is associated with the extracellular domain (Fig. 4). Complete evolutionary conservation was confirmed in six missense variants (p.Met246Ile, p.Arg838His, p.Arg838Cys, p.Glu841Lys, p.Glu874Lys, p.Val902Leu) and relatively high conservation was found in two variants (p.Arg761Trp, p.Ile916Thr) (Fig. 5).
The allele frequency available for three GUCY2D variants (p.Ala80_Leu84del, p.Arg761Trp, and p.Arg838Cys) in the East Asian/South Asian/African/European (non-Finnish) general population was 0.0%/0.000055%/0.00085%/0.0%, 0.0%/0.0%/0.0%/0.000045%, and 0.0%/0.0%/0.0%/0.0%, respectively. All detected GUCY2D variants were not found in the general Japanese population according to the HGVD and iJGVD databases.
General prediction, functional prediction, and conservation were assessed for the 10 GUCY2D variants, and the pathogenicity classification according to the American College of Medical Genetics and Genomics guidelines was pathogenic for the four missense variants (p.Arg838His, p.Arg838Cys, p.Glu841Lys, p.Val902Leu); likely pathogenic for the truncating variant, the in-frame deletion variant, and the missense variant (p.Val56GlyfsTer262, p.Ala80_Leu84del, p.Ile916Thr, respectively); and uncertain significance for the three missense variants (p.Met246Ile, p.Arg761Trp, p.Glu874Lys).
Overall, 10 disease-causing variants in the GUCY2D gene were ascertained in nine families with ADCORD, one family with ARCORD, one family with MD, and one family with ARLCA. Together with the clinical features of the affected subjects and the models of inheritance in the pedigree, 10 disease-causing variants in the GUCY2D gene were determined.
Discussion
The detailed clinical and genetic characteristics of a cohort of 15 affected subjects from 12 families with GUCY2D-RD are illustrated in a nationwide cohort with IRD in Japan. Different clinical presentations were identified with different inheritance patterns, including ADCORD with various severities, severe ARLCA, severe ARCORD, and mild ADMD.
To our knowledge, this large cohort of GUCY2D-RD patients includes the highest number of ADCORD patients to date. Four of 30 families (13.3%) with AD-CORD/MD/STGD in the JEGC IRD cohort were associated with ADGUCY2D-CORD. The proportion of GUCY2D-RD in molecularly confirmed AD-CORD/MD/STGD in the JEGC cohort was 27.2% (6/22 families). In a previous report of a Chinese cohort, Jiang et al. reported nine unrelated probands with GUCY2D-RD ascertained from 74 probands with CORD (9/74, 12.2%) and seven of 15 ADCORD families had GUCY2D-RD (7/15, 46.7%).37 The proportion of GUCY2D-RD in molecularly confirmed ADCORD was 34.6% in a UK cohort and 29.4% in a French cohort.5,48 Given these results, the prevalence of GUCY2D-RD for CORD in Japan was not as high as that in other populations in Asia or Europe; however, GUCY2D-RD is a major cause of the ADCORD.
One family with ARLCA was ascertained from 41 families with AR or sporadic LCA in the JEGC cohort (1/41 families, 2.4%). The proportion of GUCY2D-RD for molecularly confirmed LCA in the JEGC cohort was 5.3% (1/19 families). Hosono et al. reported two families with ARLCA in 34 Japanese families with LCA (2/34, 5.9%).36 In previous reports of Chinese cohorts, Wang et al. reported the prevalence of GUCY2D-RD as 10.7% (14/131 LCA families), and Xu et al. reported the prevalence as 10.7% (17/159 LCA families).49,50 In European cohorts, GUCY2D-RD accounts for approximately 10% to 20% of LCA.4 These findings imply the low prevalence of ARLCA in the Japanese population, although data from a larger cohort of ARGUCY2D-LCA patients are still to draw conclusions.
In the present study of Japanese GUCY2D-RD, there were no patients with SNB. There was one 12-year-old subject with night blindness, favorable VA, normal fundus, and compound heterozygous GUCY2D variants (patient 2). These findings were consistent with the spectrum of SNB; however, this subject demonstrated undetectable generalized cone function with severely decreased rod function, which is not compatible with the striking ERG features of SNB (undetectable rod responses with identical traces for a single cone and DA bright flash ERGs).40
Thirteen affected subjects from nine families with molecularly confirmed GUCY2D-associated ADCORD demonstrated various findings, in terms of onset (0-41 years), the duration of disease (0-40 years), VA (0.0-1.52) in LogMAR units, fundus appearance (normal to extended atrophy, without/with intrachoroidal cavitation), and morphological finding (EZ preservation at the fovea to outer retinal disruption at the macula and paramacula); however, ocular symptoms such as reduced VA/poor VA, photophobia, and the pattern of dysfunction in electrophysiology with early involvement of generalized cone function were commonly shared.
Several reports have described patients with COD/CORD showing a coloboma-like macular atrophy caused by pathogenic variants in several genes, such as NMNAT1,51,52 ADAM9,53 GUCA1A,54 and GUCY2D.55 In the present study, an intrachoroidal cavitation resembling coloboma-like macular atrophy was presented in three subjects bilaterally or unilaterally. Poor visual acuity was observed in the eyes with intrachoroidal cavitation; thus, this striking finding implies severe central visual loss. The mechanism that causes the coloboma-like macular atrophy/intrachoroidal cavitation remains uncertain.
All eight subjects with normal or subtle changes demonstrated generalized retinal dysfunction (patients 2–4, 6, 8, 9, 11, 14), which is crucial to make a clinical diagnosis of GUCY2D-RD. Interestingly, a lower b-to-a ratio in dark-adapted bright flash responses was identified in three subjects (3/14, 21.4%). This electronegative finding is also observed in the early stage of other CORD and may not be specific for GUCY2D-RD.11–13,16,56 These findings are consistent with previous reports of ADGUCY2D-CORD.20,34,37,38 Therefore, comprehensive clinical investigations, including electrophysiological assessments, are essential for the diagnosis and monitoring of GUCY2D-RD.
Ten GUCY2D variants were identified in our cohort, including six previously reported and four novel variants. Six pathogenic and three likely pathogenic variants have been previously reported, and the phenotype subgroups determined in our cohort were compatible with those of the previous reports, whereas the phenotype subgroup for p.Ile916Thr in our cohort was MD, and the phenotype subgroup for this variant in the previous report was CORD. Two variants (p.Arg838His, p.Val902Leu) were found in the de novo state in our cohort (patients 11, 13), and these variants were also identified as de novo in the previous report.31,39 Because haplotype analysis around these variants was not performed, the possibility of the nonpaternity cannot be formally excluded in these families (families 8, 10). Therefore, it is more precise to describe these variants not found in parents as “most likely de novo.” A different inheritance pattern of ADCORD was described for p.Ala80_Leu84del in the previous report9; however, the detailed information of the parents of the proband was not shown. Thus, the disease causation by this variant, in our case with AR inheritance (patient 2), is still unclear.
Four novel GUCY2D variants were found in our cohort: one variant with likely pathogenic frameshift (p.Val56GlyfsTer262) and three variants of uncertain significance (p.Met246Ile, p.Arg761Trp, p.Glu874Lys). Two variants in the compound heterozygous state (p.Val56GlyfsTer262, p.Met246Ile) were found in a subject with ARLCA (Patient 1). Because there are no candidate variants for the other ARLCA-associated genes, the putative causation of these two GUCY2D variants is predicted. One missense variant (p.Arg761Trp) was found in a subject with night blindness, normal fundus, relatively preserved foveal structure, and a loss of generalized retinal function. Although there were no candidate variants causative for ARRP, ARCORD, and ARLCA, further detailed analyses with more samples/information of the other family members are required to decide the conclusive genetic diagnosis. Another missense variant (p.Glu874Lys) was identified with the aforementioned in-frame deletion variant (p.Ala80_Leu84del) in a subject with ARCORD (patient 2). Given the clinically examined unaffected mother harboring this variant (p.Glu874Lys), the possibility that the disease was caused by this variant in an AR manner cannot be excluded.
This study has several limitations. The selection bias related to disease severity is inherent because it is uncommon for genetically affected subjects with good vision to visit clinics or hospitals. The resources of clinical information or genomic DNA from unaffected family members are limited in our cohort, and it was hard to conclusively determine the inheritance pattern in most families. Further information on clinical and genetic assessment both in affected and unaffected subjects could improve the accuracy of clinical inheritance, as well as molecularly confirmed inheritance.
The data of the current study were obtained from the JEGC IRD database. The clinical data from patients registered from multiple institutions were uploaded into the database and shared among the JEGC study group. However, the examination devices used at the different institutions could have been different because the diagnostic criteria and monitoring methods were shared. It is of note that the information was collected retrospectively, and that some of the interpatient variability may be due to differences in methods of testing patients in different institutions. Therefore, a detailed quantitative analysis could not be performed.
WES with targeted analysis applied in the current study could miss the disease-causing variants in the genes outside of the target (301 retinal disease-associated genes) and structural variants, including large deletions in the target region. More comprehensive gene screening and analysis by methods such as long-read whole-genome sequencing could help to determine the genetic aberrations, including structural and noncoding variants, in our cohort. The molecular mechanisms of some AD missense, AR missense, and AR in-frame deletion variants have not yet been clarified, and further functional investigation for each variant is required to draw concludes on the disease causation.
In conclusion, this nationwide large cohort study delineates the clinical and genetic characteristics of GUCY2D-RD, including nine ADCORD families, one ARCORD family, one MD family, and one ARLCA family. Diverse clinical presentations with various severities were demonstrated in ADCORD, and an early-onset severe phenotype was shown in ARLCA. A relatively low prevalence of GUCY2D-RD for ADCORD and ARLCA in the Japanese population was identified compared to the other populations. This information helps to monitor and counsel patients, especially in East Asia, as well as to design future therapeutic approaches.
Supplementary Material
Acknowledgments
We thank Kazuki Yamazawa and Satomi Inoue, National Institute of Sensory Organs, National Tokyo Medical Center, Japan, for their help in the clinical genetic data analysis.
The laboratory of Visual Physiology, Division for Vision Research, National Institute of Sensory Organs, National Hospital Organization, Tokyo Medical Center, Tokyo, Japan is supported by grants from Astellas Pharma Inc. (NCT03281005), outside the submitted work. Supported by grants from Grant-in-Aid for Young Scientists (A) of the Ministry of Education, Culture, Sports, Science and Technology, Japan (16H06269); grants from Grant-in-Aid for Scientists to support international collaborative studies of the Ministry of Education, Culture, Sports, Science and Technology, Japan (16KK01930002); grants from the National Hospital Organization Network Research Fund (H30-NHO-Sensory Organs-03); grants from FOUNDATION FIGHTING BLINDNESS ALAN LATIES CAREER DEVELOPMENT PROGRAM (CF-CL-0416-0696-UCL); grants from Health Labour Sciences Research Grant, the Ministry of Health, Labour and Welfare (201711107A); and grants from the Great Britain Sasakawa Foundation Butterfield Awards (KF). Supported by grants from Grant-in-Aid for Young Scientists of the Ministry of Education, Culture, Sports, Science and Technology, Japan (18K16943) (YF-Y). Supported by a Fight for Sight (UK) early career investigator award, NIHR-BRC at Moorfields Eye Hospital and the UCL Institute of Ophthalmology, NIHR-BRC at Great Ormond Street Hospital and UCL Institute of Child Health, and Great Britain Sasakawa Foundation Butterfield Award, UK (GA). Funded by the NIHR-BRC at Moorfields Eye Hospital and the UCL Institute of Ophthalmology (NP). Supported by Tsubota Laboratory, Inc, Fuji Xerox Co., Ltd, Kirin Company, Ltd, Kowa Company, Ltd, Novartis Pharmaceuticals, Santen Pharmaceutical Co. Ltd, and ROHTO Pharmaceutical Co.,Ltd. (TK). Supported by the Japan Agency for Medical Research and Development (AMED) (18ek0109282h0002) (TI). Supported by AMED; the Ministry of Health, Labor and Welfare, Japan (18ek0109282h0002); Grants-in-Aid for Scientific Research, Japan Society for the Promotion of Science, Japan (H26-26462674); grants from the National Hospital Organization Network Research Fund, Japan (H30-NHO-Sensory Organs-03) and Novartis Research Grant (2018) (KT). The funding sources had no role in the design and conduct of the study; the collection, management, analysis, and interpretation of the data; the preparation, review, and approval of the manuscript; or the decision to submit the manuscript for publication.
Kaoru Fujinami has full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Research design: Xiao Liu, Kaoru Fujinami, Lizhu Yang, Yu Fujinami-Yokokawa, Kazushige Tsunoda. Data acquisition and/or research execution: All authors. Data analysis and/or interpretation: All authors. Manuscript preparation: Xiao Liu, Kaoru Fujinami, Lizhu Yang, Yu Fujinami-Yokokawa, Gavin Arno, Nikolas Pontikos, Kazushige Tsunoda.
Disclosure: X. Liu, None; K. Fujinami, Astellas Pharma Inc. (C, F), Kubota Pharmaceutical Holdings Co. Ltd (C, F), Acucela Inc. (C, F), Novartis AG (C), Janssen Pharmaceutical K.K. (C), NightStar (C, F), SANTEN Company Limited (F), Foundation Fighting Blindness (F), Foundation Fighting Blindness Clinical Research Institute (F), Japanese Ophthalmology Society (F), Japan Retinitis Pigmentosa Society (F); K. Kuniyoshi, None; M. Kondo, None; S. Ueno, None; T. Hayashi, None; K. Mochizuki, None; S. Kameya, None; L. Yang, None; Y. Fujinami-Yokokawa, None; G. Arno, None; N. Pontikos, None; H. Sakuramoto, None; T. Kominami, None; H. Terasaki, None; S. Katagiri, None; K. Mizobuchi, None; N. Nakamura, None; K. Yoshitake, None; Y. Miyake, None; S. Li, None; T. Kurihara, Tsubota Laboratory, Inc. (F), Fuji Xerox Co., Ltd. (F), Kirin Company, Ltd. (F), Kowa Company, Ltd. (F), Novartis Pharmaceuticals (F), Santen Pharmaceutical Co., Ltd. (F), ROHTO Pharmaceutical Co., Ltd. (F); K. Tsubota, None; T. Iwata, None; K. Tsunoda, None
References
- 1. Liew G, Michaelides M, Bunce C. A comparison of the causes of blindness certifications in England and Wales in working age adults (16-64 years), 1999-2000 with 2009-2010. BMJ Open. 2014; 4: e004015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tee JJ, Smith AJ, Hardcastle AJ, Michaelides M. RPGR-associated retinopathy: clinical features, molecular genetics, animal models and therapeutic options. Br J Ophthalmol. 2016; 100: 1022–1027. [DOI] [PubMed] [Google Scholar]
- 3. Hirji N, Aboshiha J, Georgiou M, Bainbridge J, Michaelides M. Achromatopsia: clinical features, molecular genetics, animal models and therapeutic options. Ophthalmic Genet. 2018; 39: 149–157. [DOI] [PubMed] [Google Scholar]
- 4. Kumaran N, Pennesi ME, Yang P, et al.. Leber congenital amaurosis/early-onset severe retinal dystrophy overview. In: Adam MP Ardinger HH Pagon RA, et al. (eds), GeneReviews((R)). Seattle (WA); 2018. [Google Scholar]
- 5. Gill JS, Georgiou M, Kalitzeos A, Moore AT, Michaelides M. Progressive cone and cone-rod dystrophies: clinical features, molecular genetics and prospects for therapy. Br J Ophthalmol. 2019; 103: 711–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tanna P, Strauss RW, Fujinami K, Michaelides M. Stargardt disease: clinical features, molecular genetics, animal models and therapeutic options. Br J Ophthalmol. 2017; 101: 25–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Neveling K, Collin RW, Gilissen C, et al.. Next-generation genetic testing for retinitis pigmentosa. Hum Mutat. 2012; 33: 963–972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Stone EM, Andorf JL, Whitmore SS, et al.. Clinically focused molecular investigation of 1000 consecutive families with inherited retinal disease. Ophthalmology. 2017; 124: 1314–1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Carss KJ, Arno G, Erwood M, et al.. Comprehensive rare variant analysis via whole-genome sequencing to determine the molecular pathology of inherited retinal disease. Am J Hum Genet. 2017; 100: 75–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Michaelides M, Hardcastle AJ, Hunt DM, Moore AT. Progressive cone and cone-rod dystrophies: phenotypes and underlying molecular genetic basis. Surv Ophthalmol. 2006; 51: 232–258. [DOI] [PubMed] [Google Scholar]
- 11. Fujinami K, Lois N, Davidson AE, et al.. A longitudinal study of Stargardt disease: clinical and electrophysiologic assessment, progression, and genotype correlations. Am J Ophthalmol. 2013; 155: 1075–1088 e1013. [DOI] [PubMed] [Google Scholar]
- 12. Fujinami K, Sergouniotis PI, Davidson AE, et al.. The clinical effect of homozygous ABCA4 alleles in 18 patients. Ophthalmology. 2013; 120: 2324–2331. [DOI] [PubMed] [Google Scholar]
- 13. Hull S, Arno G, Plagnol V, et al.. The phenotypic variability of retinal dystrophies associated with mutations in CRX, with report of a novel macular dystrophy phenotype. Invest Ophthalmol Vis Sci. 2014; 55: 6934–6944. [DOI] [PubMed] [Google Scholar]
- 14. Oishi M, Oishi A, Gotoh N, et al.. Comprehensive molecular diagnosis of a large cohort of Japanese retinitis pigmentosa and Usher syndrome patients by next-generation sequencing. Invest Ophthalmol Vis Sci. 2014; 55: 7369–7375. [DOI] [PubMed] [Google Scholar]
- 15. Arai Y, Maeda A, Hirami Y, et al.. Retinitis pigmentosa with EYS mutations is the most prevalent inherited retinal dystrophy in Japanese populations. J Ophthalmol. 2015; 2015: 819760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fujinami K, Zernant J, Chana RK, et al.. Clinical and molecular characteristics of childhood-onset Stargardt disease. Ophthalmology. 2015; 122: 326–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Nakanishi A, Ueno S, Hayashi T, et al.. Clinical and genetic findings of autosomal recessive bestrophinopathy in Japanese cohort. Am J Ophthalmol. 2016; 168: 86–94. [DOI] [PubMed] [Google Scholar]
- 18. Oishi M, Oishi A, Gotoh N, et al.. Next-generation sequencing-based comprehensive molecular analysis of 43 Japanese patients with cone and cone-rod dystrophies. Mol Vis. 2016; 22: 150–160. [PMC free article] [PubMed] [Google Scholar]
- 19. Perrault I, Rozet JM, Calvas P, et al.. Retinal-specific guanylate cyclase gene mutations in Leber's congenital amaurosis. Nat Genet. 1996; 14: 461–464. [DOI] [PubMed] [Google Scholar]
- 20. Sharon D, Wimberg H, Kinarty Y, Koch KW. Genotype-functional-phenotype correlations in photoreceptor guanylate cyclase (GC-E) encoded by GUCY2D. Prog Retin Eye Res. 2018; 63: 69–91. [DOI] [PubMed] [Google Scholar]
- 21. Goraczniak RM, Duda T, Sitaramayya A, Sharma RK. Structural and functional characterization of the rod outer segment membrane guanylate cyclase. Biochem J. 1994; 302(Pt 2): 455–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yang RB, Foster DC, Garbers DL, Fulle HJ. Two membrane forms of guanylyl cyclase found in the eye. Proc Natl Acad Sci USA. 1995; 92: 602–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Goraczniak R, Duda T, Sharma RK. Structural and functional characterization of a second subfamily member of the calcium-modulated bovine rod outer segment membrane guanylate cyclase, ROS-GC2. Biochem Biophys Res Commun. 1997; 234: 666–670. [DOI] [PubMed] [Google Scholar]
- 24. Pugh EN Jr. Duda T, Sitaramayya A, Sharma RK. Photoreceptor guanylate cyclases: a review. Biosci Rep. 1997; 17: 429–473. [DOI] [PubMed] [Google Scholar]
- 25. Dizhoor AM, Hurley JB. Regulation of photoreceptor membrane guanylyl cyclases by guanylyl cyclase activator proteins. Methods. 1999; 19: 521–531. [DOI] [PubMed] [Google Scholar]
- 26. Hunt DM, Buch P, Michaelides M. Guanylate cyclases and associated activator proteins in retinal disease. Mol Cell Biochem. 2010; 334: 157–168. [DOI] [PubMed] [Google Scholar]
- 27. Camuzat A, Dollfus H, Rozet JM, et al.. A gene for Leber's congenital amaurosis maps to chromosome 17p. Hum Mol Genet. 1995; 4: 1447–1452. [DOI] [PubMed] [Google Scholar]
- 28. Downes SM, Payne AM, Kelsell RE, et al.. Autosomal dominant cone-rod dystrophy with mutations in the guanylate cyclase 2D gene encoding retinal guanylate cyclase-1. Arch Ophthalmol. 2001; 119: 1667–1673. [DOI] [PubMed] [Google Scholar]
- 29. Kelsell RE, Gregory-Evans K, Payne AM, et al.. Mutations in the retinal guanylate cyclase (RETGC-1) gene in dominant cone-rod dystrophy. Hum Mol Genet. 1998; 7: 1179–1184. [DOI] [PubMed] [Google Scholar]
- 30. Lazar CH, Mutsuddi M, Kimchi A, et al.. Whole exome sequencing reveals GUCY2D as a major gene associated with cone and cone-rod dystrophy in Israel. Invest Ophthalmol Vis Sci. 2014; 56: 420–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wimberg H, Lev D, Yosovich K, et al.. Photoreceptor guanylate cyclase (GUCY2D) mutations cause retinal dystrophies by severe malfunction of Ca(2+)-dependent cyclic GMP synthesis. Front Mol Neurosci. 2018; 11: 348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. de Castro-Miro M, Pomares E, Lores-Motta L, et al.. Combined genetic and high-throughput strategies for molecular diagnosis of inherited retinal dystrophies. PLoS One. 2014; 9: e88410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ito S, Nakamura M, Nuno Y, Ohnishi Y, Nishida T, Miyake Y. Novel complex GUCY2D mutation in Japanese family with cone-rod dystrophy. Invest Ophthalmol Vis Sci. 2004; 45: 1480–1485. [DOI] [PubMed] [Google Scholar]
- 34. Ito S, Nakamura M, Ohnishi Y, Miyake Y. Autosomal dominant cone-rod dystrophy with R838H and R838C mutations in the GUCY2D gene in Japanese patients. Jpn J Ophthalmol. 2004; 48: 228–235. [DOI] [PubMed] [Google Scholar]
- 35. Hosono K, Harada Y, Kurata K, et al.. Novel GUCY2D gene mutations in Japanese male twins with Leber congenital amaurosis. J Ophthalmol. 2015; 2015: 693468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hosono K, Nishina S, Yokoi T, et al.. Molecular diagnosis of 34 Japanese families with Leber congenital amaurosis using targeted next generation sequencing. Sci Rep. 2018; 8: 8279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Jiang F, Xu K, Zhang X, Xie Y, Bai F, Li Y. GUCY2D mutations in a Chinese cohort with autosomal dominant cone or cone-rod dystrophies. Doc Ophthalmol. 2015; 131: 105–114. [DOI] [PubMed] [Google Scholar]
- 38. Payne AM, Morris AG, Downes SM, et al.. Clustering and frequency of mutations in the retinal guanylate cyclase (GUCY2D) gene in patients with dominant cone-rod dystrophies. J Med Genet. 2001; 38: 611–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Mukherjee R, Robson AG, Holder GE, et al.. A detailed phenotypic description of autosomal dominant cone dystrophy due to a de novo mutation in the GUCY2D gene. Eye (Lond). 2014; 28: 481–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Stunkel ML, Brodie SE, Cideciyan AV, et al.. Expanded retinal disease spectrum associated with autosomal recessive mutations in GUCY2D. Am J Ophthalmol. 2018; 190: 58–68. [DOI] [PubMed] [Google Scholar]
- 41. Fujinami K, Kameya S, Kikuchi S, et al.. Novel RP1L1 variants and genotype-photoreceptor microstructural phenotype associations in cohort of Japanese patients with occult macular dystrophy. Invest Ophthalmol Vis Sci. 2016; 57: 4837–4846. [DOI] [PubMed] [Google Scholar]
- 42. Hood DC, Bach M, Brigell M, et al.. ISCEV standard for clinical multifocal electroretinography (mfERG) (2011 edition). Doc Ophthalmol. 2012; 124: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. McCulloch DL, Marmor MF, Brigell MG, et al.. Erratum to: ISCEV Standard for full-field clinical electroretinography (2015 update). Doc Ophthalmol. 2015; 131: 81–83. [DOI] [PubMed] [Google Scholar]
- 44. McCulloch DL, Marmor MF, Brigell MG, et al.. ISCEV Standard for full-field clinical electroretinography (2015 update). Doc Ophthalmol. 2015; 130: 1–12. [DOI] [PubMed] [Google Scholar]
- 45. Terasaki H, Miyake Y, Nomura R, et al.. Focal macular ERGs in eyes after removal of macular ILM during macular hole surgery. Invest Ophthalmol Vis Sci. 2001; 42: 229–234. [PubMed] [Google Scholar]
- 46. Pontikos N, Yu J, Moghul I, et al.. Phenopolis: an open platform for harmonization and analysis of genetic and phenotypic data. Bioinformatics. 2017; 33: 2421–2423. [DOI] [PubMed] [Google Scholar]
- 47. Richards S, Aziz N, Bale S, et al.. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015; 17: 405–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Boulanger-Scemama E, El Shamieh S, Demontant V, et al.. Next-generation sequencing applied to a large French cone and cone-rod dystrophy cohort: mutation spectrum and new genotype-phenotype correlation. Orphanet J Rare Dis. 2015; 10: 85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Wang H, Wang X, Zou X, et al.. Comprehensive molecular diagnosis of a large Chinese Leber congenital amaurosis cohort. Invest Ophthalmol Vis Sci. 2015; 56: 3642–3655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Xu Y, Xiao X, Li S, et al.. Molecular genetics of Leber congenital amaurosis in Chinese: new data from 66 probands and mutation overview of 159 probands. Exp Eye Res. 2016; 149: 93–99. [DOI] [PubMed] [Google Scholar]
- 51. Falk MJ, Zhang Q, Nakamaru-Ogiso E, et al.. NMNAT1 mutations cause Leber congenital amaurosis. Nat Genet. 2012; 44: 1040–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Nash BM, Symes R, Goel H, et al.. NMNAT1 variants cause cone and cone-rod dystrophy. Eur J Hum Genet. 2018; 26: 428–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. El-Haig WM, Jakobsson C, Favez T, Schorderet DF, Abouzeid H. Novel ADAM9 homozygous mutation in a consanguineous Egyptian family with severe cone-rod dystrophy and cataract. Br J Ophthalmol. 2014; 98: 1718–1723. [DOI] [PubMed] [Google Scholar]
- 54. Kamenarova K, Corton M, Garcia-Sandoval B, et al.. Novel GUCA1A mutations suggesting possible mechanisms of pathogenesis in cone, cone-rod, and macular dystrophy patients. Biomed Res Int. 2013; 2013: 517570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Xu F, Dong F, Li H, Li X, Jiang R, Sui R. Phenotypic characterization of a Chinese family with autosomal dominant cone-rod dystrophy related to GUCY2D. Doc Ophthalmol. 2013; 126: 233–240. [DOI] [PubMed] [Google Scholar]
- 56. Khan KN, Kasilian M, Mahroo OAR, et al.. Early patterns of macular degeneration in ABCA4-associated retinopathy. Ophthalmology. 2018; 125: 735–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.