Abstract
BACKGROUND:
In the short-stay surgery setting, where patients remain in hospital for a single overnight at most, it is unclear as to whether postoperative length of stay is a good surrogate for assessing rapidity of recovery. We hypothesized that length of stay would be a function of time of surgery and would be a poorer marker of recovery than time of discharge.
METHODS:
A cohort of 891 mastectomy and 538 prostatectomy patients had a planned single overnight stay after surgery at an ambulatory surgical hospital during 2016. The relationship between surgical start time and postoperative length of stay or discharge time was assessed.
RESULTS:
For both mastectomy and prostatectomy patients, 75% of patients were discharged between 10 AM and 12 noon and the median postoperative length of stay was 20 hours. There was a strong association between time of surgery and calculated length of stay. For mastectomies, having a surgery which begins at 6 PM vs 8 AM results in an estimated decrease of 8.8 hours (95% CI, 8.3–9.3) in postoperative length of stay but only 1.2 hours (95% CI, 0.77–1.6) later time of discharge. For prostatectomies, the estimated difference is a decrease of 6.9 hours (95% CI, 6.4–7.4) for postoperative length of stay and 2.5 hours (95% CI, 2.0–3.0) later discharge time.
CONCLUSIONS:
Postoperative length of stay is a poor outcome measure in a short-stay setting. When assessing rapidity of recovery for single overnight stay patients, we advocate the use of discharge time with adjustment for surgery start time. The effect of surgery start time on both postoperative length of stay and discharge time should be investigated to ascertain which is best to assess rapidity of recovery in other ambulatory care settings where recovery involves a single overnight stay. (Anesth Analg 2019;129:1007–13)
Many institutions have established the feasibility and safety of same or next day discharge after increasingly complex surgeries.1–10 Our institution, Memorial Sloan Kettering Cancer Center, has recently opened a freestanding short-stay surgery facility, the Josie Robertson Surgery Center, designed to facilitate the performance of increasingly complex cancer surgeries with a single overnight stay. We developed the concept of the “Ambulatory Extended Recovery” procedure, a procedure with a traditional 2- to 3-day inpatient stay performed with discharge home after a single overnight in the hospital. With careful patient and procedure selection and management on standardized care pathways, we have been successful in performing surgeries such as mastectomy, thyroidectomy, and minimally invasive prostatectomy, nephrectomy, and hysterectomy as Ambulatory Extended Recovery procedures, while maintaining high levels of quality, safety, and patient satisfaction.
Often we wish to investigate variables that are associated with patients’ rapidity of recovery. In the traditional longer stay postsurgery setting, this has typically been assessed as postoperative length of stay, usually measured in days. In our short-stay surgery setting, where the longest length of stay is limited to 1 overnight, it is unclear as to whether length of stay is a good surrogate for postoperative problems or a delay in recovery. This is because patients are not typically discharged between 8 PM and 7 AM the following morning. Consider 2 patients, both of whom require 18 hours to be ready for discharge, but different surgery start times of 10 AM and 2 PM. The former patient would not be discharged at 4 AM, but at 8 AM, the same time as the latter patient, and hence has an apparently longer length of stay. Although this phenomenon has been noticed by other researchers, we have found no literature that proposes alternative measures to assess rapidity of recovery.
We hypothesize that there is an “overnight reset” among our single overnight stay patients, meaning that most patients are ready to be discharged at roughly the same time the following morning regardless of when a patient had surgery the previous day. Patients having surgery later in the day “catch up” in their recovery resulting in artifactually longer postoperative lengths of stay for patients who had earlier surgeries. Issues delaying readiness for discharge would potentially manifest as later discharge that following morning. Therefore, we wished to determine whether postoperative length of stay or discharge time was a better end point for assessing rapidity of recovery.
METHODS
The Josie Robertson Surgery Center is a novel new facility designed to facilitate the performance of more complex cancer surgeries in the ambulatory setting. To this end, care, including patient and procedure selection, education and expectation setting, and intraoperative and postoperative management, is highly protocolized. Approximately 25% of patients eligible to have their surgery at Josie Robertson Surgery Center instead have it performed at our nearby inpatient hospital, Memorial Hospital. The most common reason for this is scheduling convenience for the patient or surgeon, followed by anticipated surgical complexity (ie, suspicion of locally metastatic disease, high probability of needing to open a minimally invasive approach, etc) with consequent higher risk of requiring a longer hospitalization. Less than 5% of surgeries are performed at Memorial Hospital for medical comorbidities. Patients are transferred to Memorial Hospital after surgery at Josie Robertson Surgery Center only if they experience a complication requiring specialty care (cardiology, critical care), transfusion (Josie Robertson Surgery Center is only licensed for emergency transfusion of uncross-matched O-negative blood), or simply are not ready to go home on postoperative day 1 (extremely rare). Finally, by design, Ambulatory Extended Recovery patients are not required to stay overnight but may be discharged when they have met all criteria. If this is achieved late in the evening, they typically stay overnight, but on occasion individual patients opt to go home. For the mastectomy and prostatectomy patients, because both pathways include elements such as physical therapy or late laboratories, this is very uncommon but has occurred.
We focused our analysis on the 2 most common types of surgery conducted in our Ambulatory Extended Recovery setting: mastectomies and prostatectomies. A cohort of 2131 patients underwent 2338 of these surgical procedures at Josie Robertson Surgery Center between January 1, 2016 and December 31, 2016, our first year of operation. We excluded 40 (1.7%) procedures where the patient was transferred to the main hospital and 16 (0.7%) where the patient underwent a reoperation within 24 hours for bleeding. There were 894 and 538 mastectomies and prostatectomies for which the patient stayed overnight, respectively. Three patients had 2 separate unilateral mastectomies; we excluded these patients’ second procedure. Data on patients’ surgery type (mastectomy or prostatectomy), operative time, surgeon, postoperative length of stay, discharge time, age, body mass index, American Society of Anesthesiologists (ASA) score, anesthesia technique, and robotic-assisted surgery status were collected.
We hypothesized that, because the average postoperative recovery time for these procedures is on the order of 12–15 hours, there is an “overnight reset” among patients who remain at the hospital overnight such that most patients achieve readiness for discharge during this overnight period. As a result, regardless of what time a patient had surgery the previous day, all patients having an uncomplicated course should be ready to be discharged at roughly the same time the following morning. Patients are not usually discharged between 8 PM and 7 AM the following morning but have fully recovered during this overnight period. Our analytic framework is that we should disfavor an end point—length of stay versus discharge time—that had an important correlation with the time of day when surgery started. If an end point of interest has a strong association with a variable that is not of interest in the analysis, associations between the outcome and predictors of interest may be obscured. This would raise the potential of confounding if this extraneous variable was also associated with a predictor of interest.
Statistical Analysis
After obtaining institutional review board approval for waiver of consent, we generated scatterplots to visualize the relationship between surgical start time versus discharge time and surgical start time versus postoperative length of stay, defined as time from entry to discharge of the postanesthesia care unit. To assess whether patients with more comorbidities were systematically operated on earlier, and thus potentially biasing the results, we tested for associations among surgery start time and age, body mass index, and ASA classification (I–II versus III–IV) using linear regression separately by surgery type. We modeled the relationship between surgery start time and discharge time and between surgery start time and length of stay using separate univariable linear regressions. We also performed the outlined analysis using surgery end time in place of start time as a sensitivity analysis. P values <.05 were considered significant. All analyses were performed using Stata 15 (StataCorp, College Station, TX). This manuscript adheres to the applicable STrengthening the Reporting of OBservational studies in Epidemiology guidelines.11
RESULTS
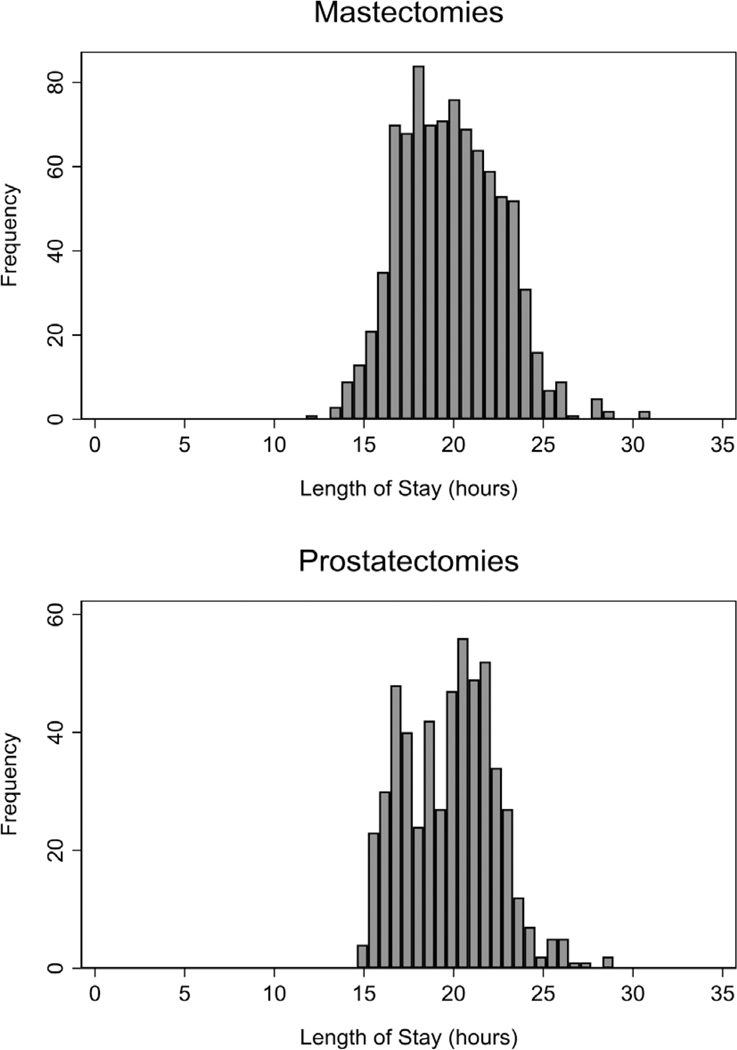
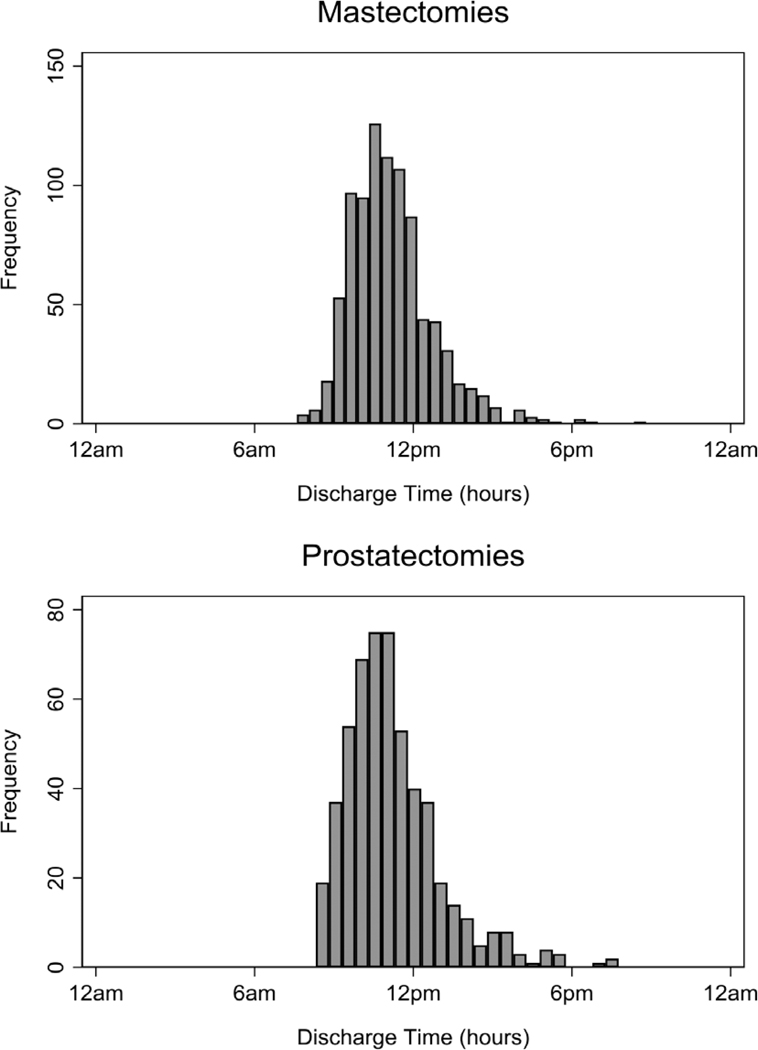
In total, 891 and 538 mastectomy and prostatectomy patients stayed overnight after their surgery at Josie Robertson Surgery Center and were included in this analysis, respectively. Patient characteristics are presented in Table 1. Mastectomies included both unilateral (50%) and bilateral (50%) procedures and could be with (76%) or without (24%) immediate reconstruction with tissue expanders or implants. All prostatectomies were minimally invasive, with most being robotically assisted (83%). The median age at surgery was 51 and 63 years for patients who underwent a mastectomy and prostatectomy, respectively; 17 (1.9%) of mastectomy patients were male; 537 (61%) of mastectomy patients received a peripheral nerve block; 1 (0.2%) prostatectomy patient had an ASA score of 4. The distribution of surgery start time by surgery type is displayed in Supplemental Digital Content, Figure 1, http://links.lww.com/AA/C686. Median postoperative length of stay was 20 hours for both those who underwent a mastectomy (interquartile range, 18–22) and for those who underwent a prostatectomy (interquartile range, 17–22) (Figure 1). Median discharge time was 11 AM (interquartile range, 10–12 AM) for both mastectomy and prostatectomy patients (Figure 2). We did not find sufficient evidence of an association between surgery start time and age or ASA for either surgery type nor for body mass index among those who underwent a mastectomy (all P values ≥ .2). For those who underwent a prostatectomy, higher body mass index was associated with a later start time (coefficient, 0.056; 95% CI, 0–0.112; P = .049); therefore, we have no evidence that patients with more comorbidities were operated on earlier.
Table 1.
Patient Characteristics by Surgery Type
| Characteristic | Mastectomies (N = 891) | Prostatectomies (N = 538) |
|---|---|---|
| Age at surgery | 51 (43–61) | 63 (57–67) |
| Body mass index (N = 1428) | 25 (22–29) | 28 (26–31) |
| Male | 17 (1.9%) | 538 (100%) |
| ASA score | ||
| I | 12 (1.3%) | 12 (2.2%) |
| II | 507 (57%) | 289 (54%) |
| III | 372 (42%) | 236 (44%) |
| IV | 0 (0%) | 1 (0.2%) |
| Robotic-assisted procedure | ||
| No | 891 (100%) | 89 (17%) |
| Yes | 0 (0%) | 449 (83%) |
| Surgery start time | 12:35 PM (10:18 AM to 2:15 PM) | 9:43 AM (8:22 AM to 1:52 PM) |
| Operative time (min) | 160 (127–195) | 245 (220–274) |
| Length of stay (h) | 20 (18–22) | 20 (17–22) |
| Discharge time | 10:57 AM (10:07 AM to 11:56 PM) | 10:53 AM (9:59 AM to 12:06 PM) |
| Breast reconstruction | 674 (76%) | |
| Laterality | ||
| Unilateral | 449 (50%) | … |
| Bilateral | 442 (50%) | … |
| Peripheral nerve block (N = 887) | 537 (61%) | … |
Data are presented as median (interquartile range) or n (%).
Abbreviation: ASA, American Society of Anesthesiologists.
Figure 1.
Histogram of postoperative length of stay (hours) by surgery type.
Figure 2.
Histogram of time of discharge (hours) by surgery type.
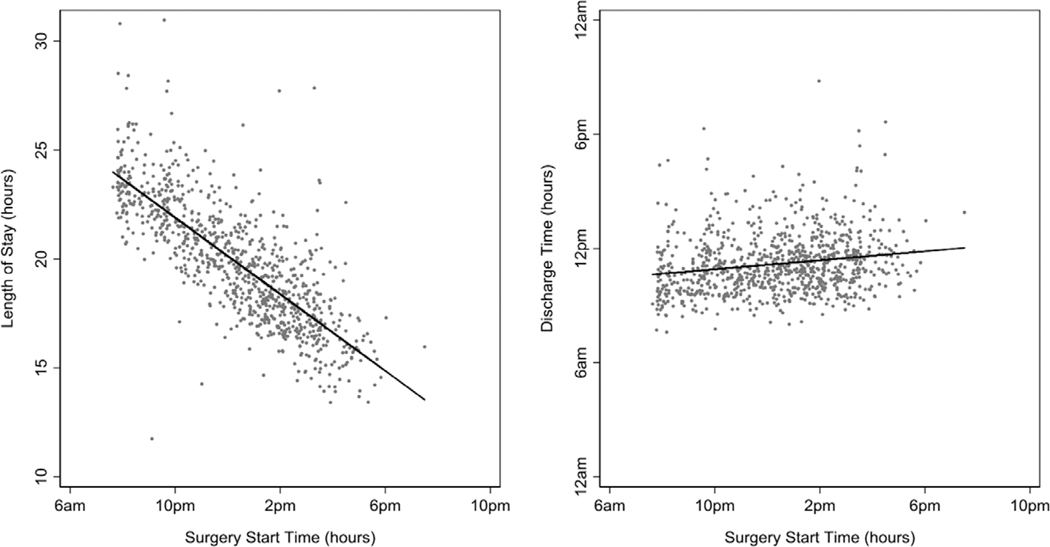
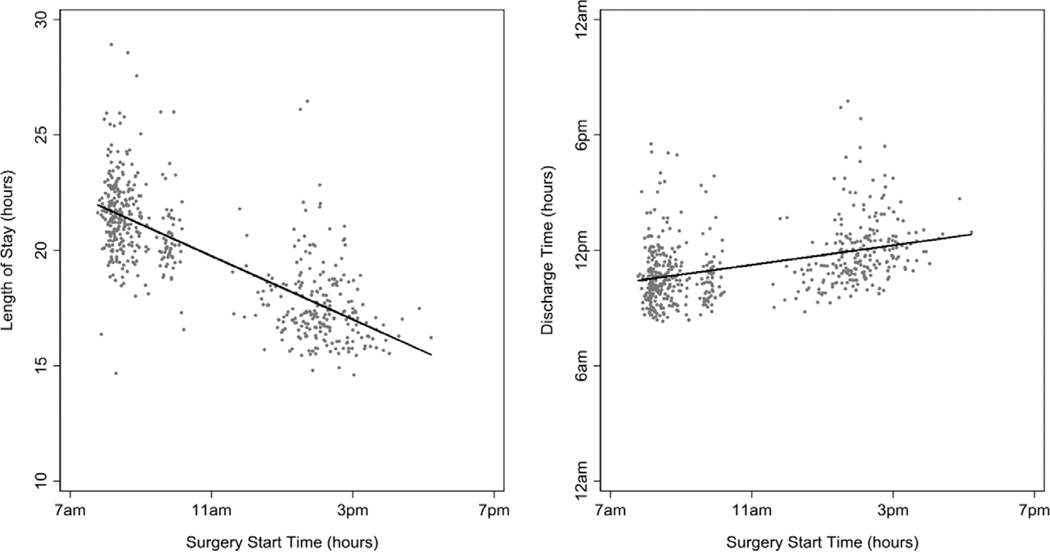
The relationships between surgical start time and postoperative length of stay or discharge time are shown in Figure 3 for mastectomies and Figure 4 for prostatectomies. Although surgery start time was significantly associated with both length of stay and discharge time regardless of surgery type (Table 2; all P values < .0001), the strength of the relationship between surgery start time and length of stay was far greater than that for surgery start time and discharge time. The absolute value of the effect size (coefficient in Table 2) was over 7 times greater for postoperative length of stay compared to discharge time for mastectomies and nearly 3 times greater for prostatectomies. For mastectomies, the estimated increase in postoperative length of stay for a surgery which began at 8 AM vs 10 hours later at 6 PM is 8.8 hours (95% CI, 8.3–9.3), while discharge time the next morning is only 1.2 hours (95% CI, 0.77–1.6) earlier. For prostatectomies, the estimated difference is an increase of 6.9 hours (95% CI, 6.4–7.4) for postoperative length of stay versus a 2.5 hours (95% CI, 2.0–3.1) earlier discharge time. Differences between end points are highly statistically significant (P < .0001). Note that the very narrow CIs and high levels of statistical significance suggest that our convenience sample derived from all eligible patients from our first year of operation has more than adequate statistical power.
Figure 3.
Scatterplots of postoperative length of stay (hours) and discharge time (hours) versus surgery start time (hours) with the univariable predicted lines corresponding to Table 2 overlaid among patients who underwent a mastectomy.
Figure 4.
Scatterplots of postoperative length of stay (hours) and discharge time (hours) versus surgery start time (hours) with the univariable predicted lines corresponding to Table 2 overlaid among patients who underwent a prostatectomy.
Table 2.
Univariable Linear Regression Models for the Associations Between Surgery Start Time and the Outcomes of Interest by Surgery Type
| Mastectomies (n = 891) | Prostatectomies (n = 538) | |||||
|---|---|---|---|---|---|---|
| Outcome | Coefficient | 95% CI | P Value | Coefficient | 95% CI | P Value |
| Length of stay (h) | −0.88 | −0.93 to −0.83 | <.0001 | −0.69 | −0.74 to −0.64 | <.0001 |
| Time of discharge (h) | 0.12 | 0.08–0.16 | <.0001 | 0.25 | 0.20–0.31 | <.0001 |
The coefficient gives the change in the outcome for a 1 h later surgery start time. For instance, length of stay is 0.88 h shorter for breast cancer patients for each hour difference in surgery start time.
Abbreviation: CI, confidence interval.
Results corresponding to the sensitivity analyses investigating the associations with surgery end time were similar. The effect size corresponding to surgery end time was 6 and over 2 times greater for postoperative length of stay compared to discharge time for mastectomies and prostatectomies, respectively (Supplemental Digital Content, Table 1, Figures 2–3, http://links.lww.com/AA/C686).
DISCUSSION
It is important to assess the impact of interventions intended to improve outcomes such as pain and nausea, oral intake, mobility, the ability of patients to participate in postoperative teaching, and ultimately readiness for discharge. For inpatient surgeries with several day hospital stays, improvements are traditionally measured by reductions in hospital length of stay, measured in days: we might be impressed if an intervention reduced length of stay in a specified group of patients from a mean of 5.4–4.8 days.12–15 The same is true for outpatient surgeries with same-day discharge, with delays in patient recovery measured by increases in postoperative or postanesthesia care unit length of stay in hours or minutes.16–18 We recognized potential problems in using postoperative length of stay for short-stay surgeries with a planned single overnight stay, when we observed that our patients were being discharged home the morning after surgery relatively independent of the timing of their surgery. Delays in discharge may be due to logistics of normal discharge activities by staff (standard care elements such as physical therapy or laboratory tests, teaching, administrative paperwork), patient delays (availability of a ride), and patients not medically ready for discharge (persistent pain or nausea, extended observation for bleeding or postsurgical issues, or nonsurgical medical problems). Thus, we examined the relationship between postoperative length of stay, discharge time, and surgical start time for 2 groups of our single overnight stay Ambulatory Extended Recovery patients.
Our results support our “overnight reset” hypothesis; surgery start time was strongly associated with postoperative length of stay while only weakly, albeit significantly, associated with discharge time. Patients who undergo surgery requiring a planned single overnight stay are generally recovered and ready to be discharged when they wake up in the morning. This explains why the discharge times are tightly grouped yet postoperative lengths of stay vary greatly, with variation dependent on surgery start time. Because it is not the hospital’s usual practice to discharge a patient in the middle of the night, the length of stay for patients who had earlier surgeries is extended and, resultantly, postoperative length of stay is strongly dependent on surgery start time.
There remains a significant effect of surgery start time on discharge time, with a magnitude that is about double for prostatectomies compared to mastectomies (Table 2). This effect can be partly explained by different factors in the standardized postoperative care for these patients. Mastectomy patients routinely undergo physical therapy before discharge on the morning after surgery; patients are generally visited by the physical therapist in the order of their surgery start time, thus sequencing discharge to a degree. A patient who is not ready for their physical therapy session because of pain, nausea, or other medical issues, however, will have their discharge time delayed. For patients undergoing prostatectomy, there are generally 2 cases performed in an operating room each day, creating clustering around an early morning start and an early afternoon start. In addition, a 14-hour postoperative laboratory result is required to approve a patient for discharge, obligating those patients with the latest surgery start (and end) times to later discharge times, as illustrated in Figure 4. As a general principle, if the time required for recovery extends beyond the overnight period, then the effect of the “reset” is reduced and eventually lost. To address the relationship between surgery, start time and discharge time identified above, we advocate that differences in surgery start time are accounted for in statistical analyses. For instance, surgery start time could be included as a covariate in a multivariable linear regression model with discharge time as the end point. Discharge time remains an imperfect metric to rapidity of recovery as it is affected by nonmedical factors as discussed above. Furthermore, the degree to which discharge time is sensitive to the incidence of medical issues depends on the time required to resolve these issues; for example, discharge would not be delayed if a patient experiencing severe postoperative nausea was successfully treated in the overnight hours. Patients having earlier surgeries thus have a longer time period during which such issues may be managed without delaying discharge. Nonetheless, compared to postoperative length of stay, discharge time is the superior end point.
We are unaware of any literature that uses discharge time as an indicator for rapidity of recovery or any investigations of shortcomings of using postoperative length of stay in the short-stay setting. Korsholm et al19 identified that surgery start and end time was associated with a decreased probability of a same-day discharge after minimally invasive hysterectomy. Similarly, patients undergoing laparoscopic radical hysterectomy and anterior cervical discectomy were more likely to require overnight admission if the surgery was later in the day.7,20 Thomas et al21 established that patients undergoing prostatectomies later in the day were much more likely to have a hospital stay of ≥2 days than earlier starting cases. These studies were focused on hospital costs and scheduling and did not address the utility of postoperative length of stay as a quality end point, but they nonetheless demonstrate that there is a finite window for discharging more complex ambulatory cases home which, if exceeded, extends the stay to the next day.
A major limitation to our study is that we examined only 2 procedures conducted at Josie Robertson Surgery Center, mastectomies, and minimally invasive prostatectomies. It would be expected that for procedures with a longer recovery time that was not typically complete by morning, then postoperative length of stay might reflect a rapidity of recovery more accurately than discharge time. For example, if the median recovery time was 24 hours (interquartile range, 22–26), one would expect the opposite—postoperative length of stay would be less correlated with surgery start, whereas discharge time would be very strongly correlated with surgery start time. The prostatectomy and mastectomy cases represent a majority of the Ambulatory Extended Recovery surgeries conducted at the Josie Robertson Surgery Center and, at 20 hours, also have the longest recovery period; therefore, discharge time would be favorable in this setting. If researchers are investigating a procedure where expected recovery time is longer than the overnight period, postoperative length of stay may be appropriate.
As more short-stay clinical models such as our Ambulatory Extended Recovery program are implemented, for example, the trend toward ambulatory total joint replacement centers, traditional outcome metrics such as length of stay need to be reevaluated. We have found postoperative length of stay to be a poor outcome measure in this short-stay setting. The effect of surgery start time on such studies, while modest, cannot be ignored and would need to be adjusted for in analyses. When assessing rapidity of recovery in patients who stayed overnight at Josie Robertson Surgery Center, we will use discharge time instead of postoperative length of stay. The effect of surgery start time on both postoperative length of stay and discharge time should be investigated to ascertain which is best to assess rapidity of recovery in other ambulatory care settings where recovery involves a single overnight stay.
Supplementary Material
KEY POINTS.
Question: Is postoperative length of stay a good surrogate for assessing rapidity of recovery in a single overnight stay setting?
Findings: Surgery start time was strongly associated with postoperative length of stay, whereas discharge time was only weakly, albeit significantly, associated.
Meaning: When assessing rapidity of recovery in a single overnight stay setting, we advocate for the use of discharge time, with adjustment for surgery start time, rather than postoperative length of stay.
Acknowledgments
Funding: This work was supported by National Cancer Institute (P50-CA92629 and P30-CA008748), the Sidney Kimmel Center for Prostate and Urologic Cancers, David H. Koch through the Prostate Cancer Foundation, the Richard Capri Foundation, and Ambulatory Cancer Care Electronic Symptom Self-Reporting for Surgical Patients (R-1602-34355 Patient-Centered Outcomes Research Institute).
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (www.anesthesia-analgesia.org).
The authors declare no conflicts of interest
REFERENCES
- 1.Dumestre DO, Webb CE, Temple-Oberle C. Improved recovery experience achieved for women undergoing implant-based breast reconstruction using an enhanced recovery after surgery model. Plast Reconstr Surg. 2017;139:550–559. [DOI] [PubMed] [Google Scholar]
- 2.Gien LT, Kupets R, Covens A. Feasibility of same-day discharge after laparoscopic surgery in gynecologic oncology. Gynecol Oncol. 2011;121:339–343. [DOI] [PubMed] [Google Scholar]
- 3.Lee J, Aphinyanaphongs Y, Curtin JP, Chern JY, Frey MK, Boyd LR. The safety of same-day discharge after laparoscopic hysterectomy for endometrial cancer. Gynecol Oncol. 2016;142:508–513. [DOI] [PubMed] [Google Scholar]
- 4.Lee SJ, Calderon B, Gardner GJ, et al. The feasibility and safety of same-day discharge after robotic-assisted hysterectomy alone or with other procedures for benign and malignant indications. Gynecol Oncol. 2014;133:552–555. [DOI] [PubMed] [Google Scholar]
- 5.Nahas S, Feigenberg T, Park S. Feasibility and safety of same-day discharge after minimally invasive hysterectomy in gynecologic oncology: a systematic review of the literature. Gynecol Oncol. 2016;143:439–442. [DOI] [PubMed] [Google Scholar]
- 6.Penner KR, Fleming ND, Barlavi L, Axtell AE, Lentz SE. Same-day discharge is feasible and safe in patients undergoing minimally invasive staging for gynecologic malignancies. Am J Obstet Gynecol. 2015;212:186.e1–186.e8. [DOI] [PubMed] [Google Scholar]
- 7.Philp L, Covens A, Vicus D, Kupets R, Pulman K, Gien LT. Feasibility and safety of same-day discharge after laparoscopic radical hysterectomy for cervix cancer. Gynecol Oncol. 2017;147:572–576. [DOI] [PubMed] [Google Scholar]
- 8.Richter DL, Diduch DR. Cost comparison of outpatient versus inpatient unicompartmental knee arthroplasty. Orthop J Sports Med. 2017;5:2325967117694352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Segel JM, Duke WS, White JR, Waller JL, Terris DJ. Outpatient thyroid surgery: safety of an optimized protocol in more than 1,000 patients. Surgery. 2016;159:518–523. [DOI] [PubMed] [Google Scholar]
- 10.Sun SX, Leung AN, Dillon PW, Hollenbeak CS. Length of stay and readmissions in mastectomy patients. Breast J. 2015;21:526–532. [DOI] [PubMed] [Google Scholar]
- 11.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–349. [DOI] [PubMed] [Google Scholar]
- 12.Haverkamp MP, de Roos MA, Ong KH. The ERAS protocol reduces the length of stay after laparoscopic colectomies. Surg Endosc. 2012;26:361–367. [DOI] [PubMed] [Google Scholar]
- 13.Gali B, Bakkum-Gamez JN, Plevak DJ, Schroeder D, Wilson TO, Jankowski CJ. Perioperative outcomes of robotic-assisted hysterectomy compared with open hysterectomy. Anesth Analg. 2018;126:127–133. [DOI] [PubMed] [Google Scholar]
- 14.Tang J, Humes DJ, Gemmil E, Welch NT, Parsons SL, Catton JA. Reduction in length of stay for patients undergoing oesophageal and gastric resections with implementation of enhanced recovery packages. Ann R Coll Surg Engl. 2013;95:323–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cakir H, van Stijn MF, Lopes Cardozo AM, et al. Adherence to enhanced recovery after surgery and length of stay after colonic resection. Colorectal Dis. 2013;15:1019–1025. [DOI] [PubMed] [Google Scholar]
- 16.Kumar G, Stendall C, Mistry R, Gurusamy K, Walker D. A comparison of total intravenous anaesthesia using propofol with sevoflurane or desflurane in ambulatory surgery: systematic review and meta-analysis. Anaesthesia. 2014;69: 1138–1150. [DOI] [PubMed] [Google Scholar]
- 17.McKay A, Gottschalk A, Ploppa A, Durieux ME, Groves DS. Systemic lidocaine decreased the perioperative opioid analgesic requirements but failed to reduce discharge time after ambulatory surgery. Anesth Analg. 2009;109:1805–1808. [DOI] [PubMed] [Google Scholar]
- 18.Qiu C, Rinehart J, Nguyen VT, et al. An ambulatory surgery perioperative surgical home in Kaiser Permanente settings: practice and outcomes. Anesth Analg. 2017;124:768–774. [DOI] [PubMed] [Google Scholar]
- 19.Korsholm M, Mogensen O, Jeppesen MM, Lysdal VK, Traen K, Jensen PT. Systematic review of same-day discharge after minimally invasive hysterectomy. Int J Gynaecol Obstet. 2017;136:128–137. [DOI] [PubMed] [Google Scholar]
- 20.Mayo BC, Massel DH, Bohl DD, Long WW, Modi KD, Singh K. Effect of surgery start time on day of discharge in anterior cervical discectomy and fusion patients. Spine (Phila Pa 1976). 2016;41:1939–1944. [DOI] [PubMed] [Google Scholar]
- 21.Thomas AA, Kim B, Derboghossians A, et al. Impact of surgical case order on perioperative outcomes for robotic-assisted radical prostatectomy. Urol Ann. 2014;6:142–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.