Abstract
Background
The COVID-19 pandemic has disrupted the provision and use of healthcare services throughout the world. In Slovenia, an epidemic was officially declared between mid-March and mid-May 2020. Although all non-essential health care services were put on hold by government decree, oncological services were listed as an exception. Nevertheless, as cancer control depends also on other health services and additionally major changes in people’s behaviour likely occurred, we aimed to analyse whether cancer diagnosis and management were affected during the COVID-19 epidemic in Slovenia.
Methods
We analysed routine data for the period November 2019 through May 2020 from three sources: (1) from the Slovenian Cancer Registry we analysed data on pathohistological and clinical practice cancer notifications from two major cancer centres in Ljubljana and Maribor; (2) from the e-referral system we analysed data on all referrals in Slovenia issued for oncological services, stratified by type of referral; and (3) from the administrative data of the Institute of Oncology Ljubljana we analysed data on outpatient visits by type as well as on diagnostic imaging performed.
Results
Compared to the November 2019 – February 2020 average, the decrease in April 2020 was about 43% and 29% for pathohistological and clinical cancer notifications; 33%, 46% and 85% for first, control and genetic counselling referrals; 19% (53%), 43% (72%) and 20% (21%) for first (and control) outpatient visits at the radiotherapy, surgery and medical oncology sectors at the Institute of Oncology Ljubljana, and 48%, 76%, and 42% for X-rays, mammograms and ultrasounds performed at the Institute, respectively. The number of CT and MRI scans performed was not affected.
Conclusions
Significant drops in first referrals for oncological services, first visits and imaging studies performed at the Institute, as well as cancer notifications in April 2020 point to a possibility of a delayed cancer diagnosis for some patients during the first surge of SARS-CoV-2 cases in Slovenia. The reasons for the delay cannot be ascertained with certainty and could be linked to health-seeking behaviour of the patients, the beliefs and practices of doctors and/ or the health system management during the epidemic. Drops in control referrals and control visits were expected and are most likely due to the Institute of Oncology Ljubljana postponing non-essential follow-ups through May 2020.
Key words: cancer, COVID, delay in diagnosis, referral
Introduction
Many cancer experts have highlighted the problem of access to and utilisation of cancer care services during and after the COVID-19 pandemic.1, 2, 3 Control measures are effective at containing the spread of disease, and once extensive community transmission of the virus occurs they undoubtedly contribute to preserving cancer services through protecting the health system from collapsing, although they are expected to also have negative effects for cancer control. In Slovenia, a middle European country of approximately two million inhabitants with universal health care, the response to COVID-19 epidemic was swift and included changes in the functioning of the health care system that potentially affected cancer diagnosis and management.
An overview of the COVID-19 epidemic in Slovenia
The first confirmed COVID-19 patient in Slovenia was registered on the 4th of March 2020. The first cases were imported, though soon, secondary, tertiary and quaternary transmissions of the novel virus were detected and on the 12th of March, the Health Minister following the advice of the National Institute of Public Health (NIPH) declared an epidemic, which meant the activation of the Slovenian Pandemic Plan. Control measures implemented thereafter were strict and introduced rapidly with the aim of mitigating the spread of COVID-19. On the 16th of March, all schools and educational institutions were closed, all public transport services stopped and all non-essential services shut. Soon after, all gatherings of people were prohibited, with the exception of members of the same household, working from home was encouraged and restrictions on movement of people were put in place limiting movement to within their municipality (lock-down).
Measures concerning the provision of health care services were enacted through the Ordinance on temporary measures in health care to contain and control the COVID-19 epidemic4 from the 20th of March, which stipulated that all non-essential ambulatory visits (those not referred as needing urgent or very fast management) and elective surgery appointments be put on hold. Oncological services were listed as an exception, though all preventive care activities were also put on hold by decree, meaning all three cancer screening programmes (cervical, breast and colorectal cancer) were temporarily stopped. Screening was stopped also in other countries.5, 6 At the Institute of Oncology Ljubljana, the only tertiary comprehensive cancer centre, COVID-19 preventive measures were being continually introduced and adapted starting on 26th of February. A triage, at first only physical and later also via telephone, was set up to screen patients for COVID-19 symptoms, relative escorts of patients to the hospital and visits of hospitalised patients were not allowed, except for dying patients, while non-essential follow-up visits and surgeries were postponed through May. Despite this, work at the Institute continued almost uninterrupted. Similar measures were taken by oncology departments across Europe7, 8 and many highlighted the need for stricter measures and more testing with the aim of keeping cancer clinics COVID-free given reports of the higher risk COVID-19 poses to people with cancer9 and in order to maintain the provision of oncological services.10, 11
Towards the end of March, the epidemic peaked with daily cases starting to decrease. In the second half of April, easing of control measures in the country started and on the 9th of May, the government lifted restrictions on provision of healthcare services. Following this, on the 15th of May Slovenia declared an end to the epidemic. During this time, the Institute of Oncology Ljubljana continued with normal follow-up and surgeries, also introducing working Saturdays to make up for the delay in these services. Furthermore, cancer screening programmes gradually began sending invitations again and were operating close to or at full capacity in June 2020.
Aim of the study
In light of severe restrictions in movement of individuals, cancellation of non-essential health care services and ensuing behavioural responses among the population, there might be collateral consequences of COVID-19 related measures for cancer control, despite the Institute of Oncology Ljubljana having retained almost normal functioning. In order to gain a quick and timely understanding of how cancer care in Slovenia has been affected by the COVID-19 epidemic, we carried out an analysis on readily available, up-to-date and reliable data sources.
Methods
We carried out an analysis of data from the Slovenian Cancer Registry, the e-referral system of Slovenia, managed by the NIPH, and the administrative hospital data of the Institute of Oncology Ljubljana. Using this data, we evaluated referrals for first and control oncological examination and treatment from all levels of healthcare, as well as cancer diagnosis and treatment at tertiary level only. The observed period was from November 2019 through May 2020.
The Slovenian Cancer Registry is one of the oldest cancer registries in Europe, operating since 1950. In 2018, the transition from passive to active registration started, which allows for up-to-date data on cancer notifications. This is an important feature, considering the need for real-time analysis of data to be able to inform decision-makers regarding the measures for COVID-19 control. From the Cancer Registry, we extracted data on monthly cancer notifications from the two major oncological centres in Slovenia, the Institute of Oncology Ljubljana and the University Medical Centre Maribor which are included in the active registration. The Ljubljana and Maribor oncological centres cover a major part of newly diagnosed cancers in Slovenia. Two types of cancer notifications were evaluated: those from pathohistological departments and those from clinical setting.
The second source was the NIPH e-referral system. We accessed the data from the e-referral system on all monthly referrals issued in Slovenia for selected types of oncological health services as coded in the Codebook of healthcare services, namely the Oncological examination – first, Oncological examination – control and Oncological genetic testing and counselling. As Slovenia has a gate-keeping system in place, where secondary and tertiary care is only possible through referrals, this means the number of referrals is an accurate reflection of demand for specialist oncological care.
Finally, from the administrative data of the Institute of Oncology Ljubljana we analysed data on monthly patient visits, stratified according to first and control outpatient visits, and data on cancer diagnostic imaging, namely the monthly number of X-rays, mammograms, ultrasounds, CT and MRI scans performed.
Results and discussion
Referral for oncological examination and treatment
Figure 1 shows the time trend of monthly referrals during November 2019 – May 2020 where a significant reduction in the number of referrals can be seen in April, with a somewhat smaller reduction in March. The reduction was seen for all types of referrals, though significantly more pronounced for control referrals compared to first referrals, whereas referring for oncological genetic testing and counselling stopped almost completely. Compared to the November – February average, the decrease in April was about 33%, 46% and 85% for first, control and genetic counselling referrals, respectively. In May, the number of all types of referrals started rising again.
Figure 1.

Referrals for oncological services stratified by first referral, control referral and referral for genetic counselling in Slovenian health-care system between November 2019 and May 2020.
The drop in control referrals can most likely be explained as a consequence of the cancer institutes’ policies to defer non-essential control visits. All patients were notified about their deferral and thus there was probably lower demand for control referrals from patients though other reasons could also play a role. Oncological genetic testing and counselling is a preventive service, meaning that doctors were probably less likely to refer patients for this type of care, since the decree on health care stipulated these services are temporarily dis-continued, even though oncological services were clearly listed as an exception. Patients themselves were also less likely to seek services for non-urgent care during lock-down. The reasons behind the drop in first referrals are difficult to determine. It is possible that, compared to pre-epidemic period, during lock-down, people were less likely to seek medical care even if they experienced symptoms of disease. On the other hand, access to primary and secondary level care could have been so disrupted that some patients could not get through to their doctors in order to complain about their issues. Another factor could be that primary level doctors were less likely to refer symptomatic patients for secondary and tertiary diagnostics because these services were not freely available and most of the first symptoms of cancer are rather unspecific. A combination of these factors was likely at play. As a result, we fear that fewer cancers were diagnosed in early stages.
Other countries have reported similar findings. In the UK, a dermatology service found a reduction in referrals for skin cancer of more than 50% in April 2020 compared to April 2019. Additionally, they analysed referrals for other types of cancer in their hospital and found similar reductions for a wide range of cancers, most pronounced for colorectal cancer.12 Also in the UK, others have shown that in the whole country, urgent referrals for cancer from GPs fell by 60% in April.13 In Italy, the referrals for BRCA testing to a genetic laboratory had decreased by about 60%.14
Delay in diagnosis
Figure 2 shows the trend in the number of cancer notifications from pathohistological and clinical departments sent to the Cancer Registry from the two main cancer centres, Institute of Oncology Ljubljana and University Medical Centre Maribor. Again, the same pattern can be observed with the largest decrease observed for April and an upward trend in May. Compared to the November 2019 – February 2020 average, the decrease in April was about 43% and 29% for pathohistological and clinical cancer notifications, respectively.
Figure 2.
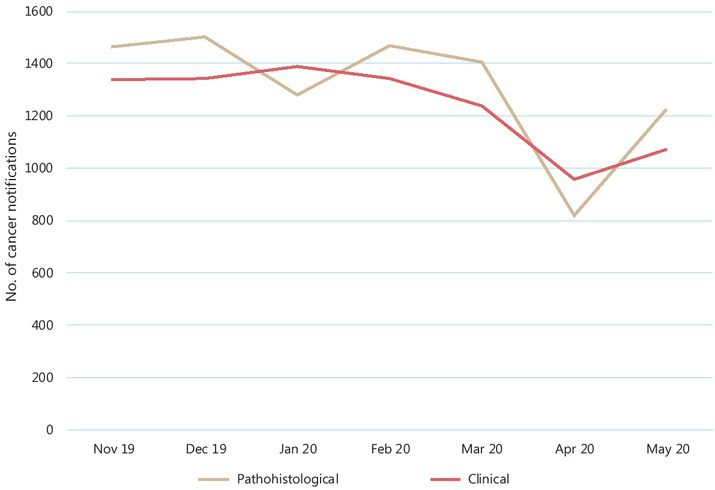
All cancer notifications from pathohistological and clinical departments at the Institute of Oncology Ljubljana and University Medical Centre Maribor between November 2019 and May 2020.
The absolute number of new notifications is not equivalent to the number of newly diagnosed cancers because a cancer case can be reported to the Cancer Registry more than once from different healthcare providers that come into contact with a patient with a cancer, while on the other hand, a small part of notifications turn out not to be malignant cases after additional investigations by the Cancer Registry. Despite this, the relative decline in new notifications can be interpreted as a decrease in newly diagnosed cancers. Roughly, this means in April there were about a third fewer cancers diagnosed in Slovenia compared to the average pre-epidemic period. The reasons for the lower number of cancer notifications are likely related to the drop in referrals. It is not surprising therefore, that the maximum drop in referrals and the maximum drop in newly diagnosed cancers are concurrent. Perhaps the time shift might have been visible if we stratified the data into weeks instead of months, because it takes a week or two for patients who are referred for oncological exam to be diagnosed with cancer. No doubt, another factor for the drop in notifications was the temporary two-month long complete cessation of all three cancer screening programmes, though at the moment it is not possible to quantify what proportion of delayed cancer diagnoses could be attributed to lack of access to cancer screening.
Our results are in line with a study from the Netherlands, where the Netherlands Cancer Registry recorded a decrease in weekly pathological cancer notifications between the end of February and start of April 2020. The decrease was observed for all age groups and all cancer groups but was largest (max. 60%) for skin cancer (excluding basal cell carcinoma), followed by breast cancer (max. 50%). The largest weekly decrease for all cancers excluding skin cancer was approximately a quarter.15 Fewer cancer diagnoses were reported also in Italy. A Pathologic Anatomy Unit in the province of Macerata recorded a decrease in pathohistological diagnoses of cancer during weeks 11-20 (March and April) of 2020 compared to the same period in 2018 and 2019. Unlike in the Netherlands, they did not observe a decrease for malignant melanoma but observed the highest drops for prostate (75%), bladder (66%) and colorectal cancer (62%). Clinically relevant delay was considered only for colorectal cancer. Interestingly, screening for colorectal cancer was disrupted in Italy but was more preserved for breast cancer, which saw a reduction of (only) 25%.16
Diagnostics and treatment
Administrative data from the Institute of Oncology Ljubljana are presented in Figures 3–5. Compared to the November 2019 – February 2020 average, the decrease in first outpatient visits in April 2020 was 19%, 43% and 20% at the radiotherapy, surgery and medical oncology sectors of the Institute, respectively, whereas for control outpatient visits, these numbers were 53%, 72% and 21%.
Figure 3.

First outpatient visits to the Institute of Oncology Ljubljana stratified by type of sector (radiotherapy, surgery, and medical oncology) between November 2019 and May 2020.
Figure 5.
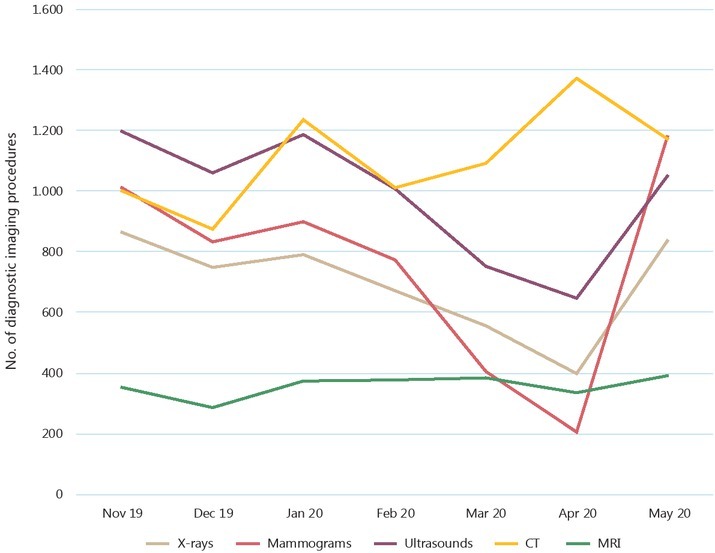
The number of X-rays, mammograms, ultrasounds, CT and MRI scans performed at the Institute of Oncology Ljubljana between November 2019 and May 2020.
Figure 4.

Control outpatient visits to the Institute of Oncology Ljubljana stratified by type of sector (radiotherapy, surgery, and medical oncology) between November 2019 and May 2020.
Visits to the medical oncology department, where patients receive active chemotherapy treatment, were least affected. The largest drop in both first and control visits can be observed for the surgical department. These results are expected, as all truly elective surgeries at the Institute were postponed, though we cannot say if a part of the decrease in the first visits could also to a minor degree reflect less patients having been diagnosed with cancer and planned for surgery as part of their primary treatment. The decline in first visits to radiotherapy and medical oncology departments was small but could also point to fewer (newly diagnosed) patients being treated. In general, reductions in control outpatient visits were expected due to either postponing non-essential follow-up visits or carrying them out as telehealth visits. For radiotherapy, it might be also indicative of the rationalisation in radiotherapy regimes (such as fewer fractions of radiotherapy).
Outpatient visits to oncological centres must have declined across Europe, though we could not find any already published European study which reported on the number of cancer outpatient visits. A report from the US shows that oncology outpatient visits had fallen by as much as 47% in April 2020.17
Regarding diagnostic imaging, in April 2020 compared to the November 2019 – February 2020 average, there were also significant reductions in X-rays (48%), mammograms (76%) and ultrasounds (42%) performed at the Institute. This could again point to fewer patients being in the diagnostic process though there were changes in the functioning of the Institute that could also have contributed to this result. The numbers of CT and MRI scans were not affected. The reduction in diagnostic imaging was thus most pronounced for mammography, which is only in part linked to the suspension of breast cancer screening, as mammograms within the screening programme are tallied separately.
Conclusions
Significant drops in first oncological referrals, first outpatient visits, x-rays, mammograms and ultrasounds as well as cancer notifications from the two major cancer centres all point to a delay in diagnosis and treatment of cancer for some patients during the COVID-19 epidemic in Slovenia. The reasons that lead to this decline cannot be assessed in our study but are presumed to be a combination of COVID-19 related factors on the side of the patients and doctors as well as the health care system and its management during the peak of the crisis. To what extent the pausing of screening programmes influenced cancer diagnosis should be evaluated at least after six months of restarting the programmes. The drop in control referrals and visits is not as relevant clinically and was an expected outcome in light of the decision to postpone non-urgent care. Long-term studies are needed in order to evaluate what the effects of the perceived delay in diagnosis and treatment during the COVID-19 epidemic will be in terms of classical cancer burden indicators, such as poorer survival or a shift toward more advanced stage at diagnosis for specific cancer types. For example, projections for the US show that cumulative excess deaths from colorectal and breast cancers between 2020 and 2030 could be around 1%18, highlighting the need for extreme caution when deciding on what measures to adopt if/when subsequent surges in COVID-19 cases occur so as to not significantly disrupt cancer control services also in the future.
Disclosure
No potential conflicts of interest were disclosed.
References
- 1.Amit M, Tam S, Bader T, Sorkin A, Benov A. Pausing cancer screening during the severe acute respiratory syndrome coronavirus 2 pandemic: should we revisit the recommendations? Eur J Cancer. 2020;134:86–9. doi: 10.1016/j.ejca.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vanni G, Pellicciaro M, Materazzo M, Palombi L, Buonomo OC. Breast cancer diagnosis in coronavirus-era: alert from italy. Frontiers Oncol. 2020;10:938. doi: 10.3389/fonc.2020.00938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vrdoljak E, Sullivan R, Lawler M. Cancer. coronavirus disease. how do we manage cancer optimally through a public health crisis? Eur J Cancer. 2019;132:98–9. doi: 10.1016/j.ejca.2020.04.001. and. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ordinance on interim measures in the field of health activities to contain and control the COVID-19 epidemic.[Slovenian] Uradni list Republike Slovenije. 2020;32(20) https://www.uradni-list.si/glasilo-uradni-list-rs/vsebina/2020-01-0645/odlok-ozacasnih-ukrepih-na-podrocju-zdravstvene-dejavnosti-zaradi-zajezitve-inobvladovanja-epidemije-covid-19 Ljubljana. [cited 2020 Jun 30]. Available at. [Google Scholar]
- 5.Del Vecchio Blanco G, Calabrese E, Biancone L, Monteleone G, Paoluzi OA. The impact of COVID-19 pandemic in the colorectal cancer prevention. Int J Colorectal Dis. 2020. [Ahead of print] 4 Jun 2020. [DOI] [PMC free article] [PubMed]
- 6.World Health Organization. Rapid assessment of service delivery for NCDs during COVID-19 pandemic. Geneva: 2020. [Google Scholar]
- 7.Fong D, Rauch S, Petter C, Haspinger E, Alber M, Mitterer M. Infection rate and clinical management of cancer patients during the COVID-19 pandemic: experience from a tertiary care hospital in northern Italy. ESMO Open. 2020;5:e000810. doi: 10.1136/esmoopen-2020-000810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van de Haar J, Hoes LR, Coles CE, Seamon K, Fröhling S, Jäger D. Caring for patients with cancer in the COVID-19 era. Nat Med. 2020;26:665–71. doi: 10.1038/s41591-020-0874-8. et al. [DOI] [PubMed] [Google Scholar]
- 9.Liang W, Guan W, Chen R, Wang W, Li J, Xu K. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21:335–7. doi: 10.1016/S1470-2045(20)30096-6. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Restivo A, De Luca R, Spolverato G, Delrio P, Lorenzon L, D’Ugo D. The need of COVID19 free hospitals to maintain cancer care. Eur J Surg Oncol. 2020;46:1186–7. doi: 10.1016/j.ejso.2020.04.003. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mahase E. Covid-19: cancer research urges mass testing to enable care to continue during pandemic. BMJ. 2020;369:m1561. doi: 10.1136/bmj.m1561. [DOI] [PubMed] [Google Scholar]
- 12.Earnshaw CH, Hunter HJA, McMullen E, Griffiths CEM, Warren RB. Reduction in skin cancer diagnosis, and overall cancer referrals, during the COVID-19 pandemic. Br J Dermatol. 2020. [Ahead of print] 4 Jun 2020. [DOI] [PMC free article] [PubMed]
- 13.Mahase E. Covid-19: Urgent cancer referrals fall by 60%, showing “brutal” impact of pandemic. BMJ. 2020;369:m2386. doi: 10.1136/bmj.m2386. [DOI] [PubMed] [Google Scholar]
- 14.Minucci A, Scambia G, Santonocito C, Concolino P, Urbani A. BRCA testing in a genomic diagnostics referral center during the COVID-19 pandemic. Mol Biol Rep. 2020;47:4857–60. doi: 10.1007/s11033-020-05479-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dinmohamed AG, Visser O, Verhoeven RHA, Louwman MWJ, van Nederveen FH, Willems SM. Fewer cancer diagnoses during the COVID-19 epidemic in the Netherlands. Lancet Oncol. 2020;21:750–1. doi: 10.1016/S1470-2045(20)30265-5. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.De Vincentiis L, Carr RA, Mariani MP, Ferrara G. Cancer diagnostic rates during the 2020 ‘lockdown’, due to COVID-19 pandemic, compared with the 2018–2019: an audit study from cellular pathology. J Clin Pathol. 2020. [Ahead of print] 19 June 2020. [DOI] [PubMed]
- 17.Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler D. The impact of the COVID-19 pandemic on outpatient visits: a rebound emerges. To the Point (blog), Commonwealth Fund. 2020. https://www.commonwealthfund.org/publications/2020/apr/impact-covid-19-outpatient-visits Published Online First: 19 May 2020. [cited 2020 Jun 30] Available at. [DOI]
- 18.Sharpless NE. COVID-19 and cancer. Science. 2020;368:1290. doi: 10.1126/science.abd3377. [DOI] [PubMed] [Google Scholar]


