Abstract
Background
Breaking bad news (BBN) may be associated with increasing risk of burnout in practising physicians. However, there is little research on the association between the way bad news is broken and burnout. We investigated the association between physicians’ self-efficacy regarding communication to patients and risk of burnout.
Methods
We performed a cross-sectional study by proposing an ad-hoc survey exploring attitudes and practice regarding BBN and the Maslach Burnout Inventory - Human Service Survey to 379 physicians from two University Hospitals in Italy. Associations were assessed by multivariable logistic regression models.
Results
Two-hundred twenty-six (60%) physicians returned the questionnaires. 76% of physicians acquired communication skills by observing mentors or colleagues, 64% considered BBN as discussing a poor prognosis, 56% reported discussing prognosis as the most difficult task, 38 and 37% did not plan a BBN encounter and considered it stressful. The overall burnout rate was 59%. Considering BBN a stressful task was independently associated with high risk of burnout (OR 3.01; p = 0.013). Planning the encounter (OR = 0.43, p = 0.037), mastering communication skills (OR = 0.19, p = 0.034) and the self-evaluation as good or very good at BBN (OR 0.32; 0.15 to 0.71; p = 0.0) were associated with low risk of burnout.
Conclusions
Our findings suggest that some physicians’ BBN attitudes and knowledge of conceptual frameworks may influence the risk of burnout and support the notion that increasing knowledge about communication skills may protect clinicians from burnout. Further research is needed in this area.
Keywords: Breaking serious news, Attitudes, Burnout, Communication skills
Background
Burnout is a psychological work-related syndrome typically affecting the helping professions, characterised by 3 core dimensions: physical and emotional exhaustion (PEE), cynicism and depersonalization (CD), and low personal accomplishment (PA) [1, 2]. Recent studies have reported that more than 50% of medical doctors suffer from burnout. Such an epidemic negatively affects patient care, professionalism, physicians’ health and safety, and the viability of health-care systems. Numerous individual and work-related factors contribute to develop the burnout of clinicians [3]. One of the most frequently advocated stressor is breaking bad news (BBN) [2, 3].
BBN, such as discussing diagnosis, disclosing a poor prognosis or discussing the transition to palliative care with patients and their families, is a core communication task in medicine [4]. The ability of physicians to deliver bad news has been studied with surveys exploring mainly their self-efficacy, intended as the beliefs in their capacity to execute such a task and their expectation of being able to successfully perform that behaviour according to experiences and/or training [5–7]. The way BBN is conveyed may seriously affect patients and families [8]. However, BBN have consequences also for physicians, who may experience strong emotions and distress. By harnessing simulation methodologies and measuring physiological indices, such as heart rate and sweating indices, several studies have empirically demonstrated that BBN may provoke fear, anxiety, discomfort and burden of responsibility in physicians. All these causes of distress may ultimately lead to burnout, with detrimental consequences on clinical effectiveness [9–11]. Nonetheless, the association between the way serious news are broken and burnout has not yet been explored [12].
We have sought to examine the association between the frameworks and professional development opportunities physicians utilise regarding healthcare communication (HC) and how that relates to a metric linked with burnout.
Methods
Characteristics of the study
The study is a cross-sectional survey study enrolling physicians working in two tertiary care hospitals (AOU-Policlinico di Modena and AOU-Ospedale Civile di Baggiovara) in Modena, Italy. The study was approved by the local Ethical Committee (CE protocol n° 244/16). An informed consent was obtained from physicians participating in the study. Participation was voluntary, anonymous and no incentive was offered. The survey was delivered by e-mail or directly to the ward, according to the number of physicians we knew working in that specific ward, and it was returned with the same procedures.
Study population
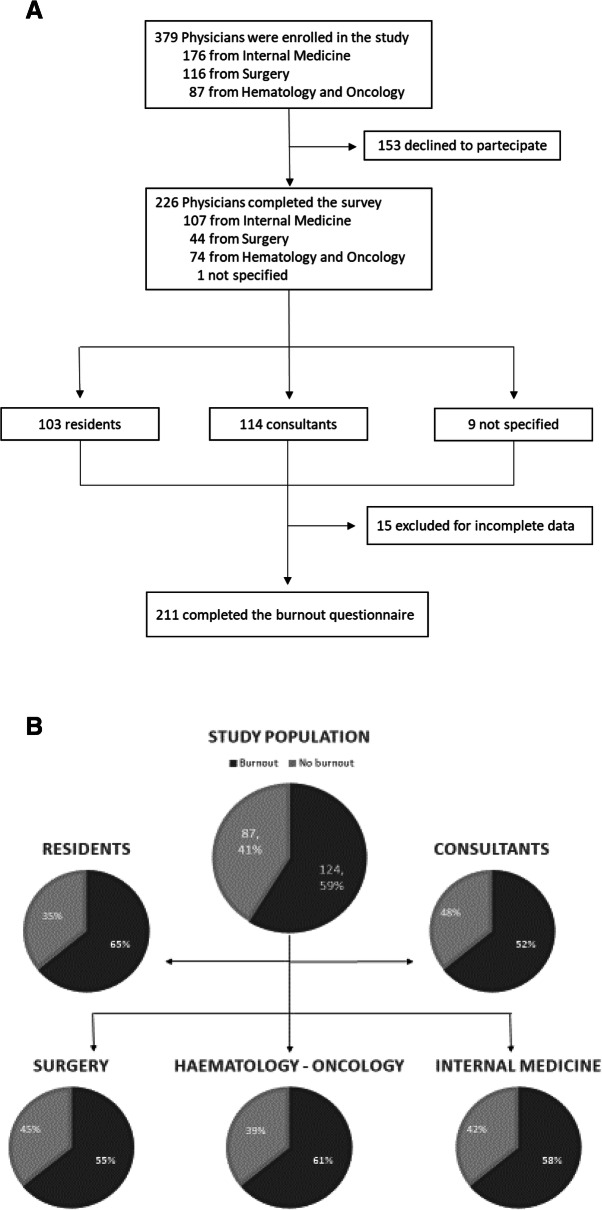
Three-hundreds-seventy-nine physicians were enrolled into the study. Of them, 226 (60%) completed the survey (Fig. 1a). A complete description of the sample is provided in Table 1. As the survey was anonymous, we were unable to evaluate the characteristics of physicians who did not return the questionnaire. The clustering of the years from graduation into 4 levels was aimed to group together physicians with supposed similar levels expertise in and development opportunities and acquisition of communication skills.
Fig. 1.
a,b. Study design flowchart and burnout analysis. a. The flowchart shows physicians’ characteristics and responses at the questionnaires. b. Burnout rates in consultants and residents and according to their branch of medical practice. Dark grey segments represent physicians with burnout in at least one dominion. Light grey segments represent physicians without burnout
Table 1.
Characteristics of Physicians
| (N/%) | |
|---|---|
| Physicians enrolled | 379 |
| Physicians returning the questionnaire | 226(60) |
| Specialty | |
| Internal Medicine area | 107(47) |
| Haematology/Oncology area | 74(33) |
| Surgical area | 44(20) |
| Unspecified | 1 |
| Gender | |
| Male | 100(44) |
| Female | 116(51) |
| Unknown | 10(5) |
| Professional Role | |
| Resident | 103(46) |
| Consultant | 114(50) |
| Not specified | 9(4) |
| Years from graduation | |
| ≤ 3 | 55(24) |
| > 3 and ≤ 6 | 45(20) |
| > 6 and ≤ 16 | 60(26) |
| > 16 | 62(28) |
| Not specified | 4(2) |
Internal medicine area includes Internal Medicine, Pneumology, Infectivology, Emergency Medicine, Nefrology, Gastroenterology and Endocrinology; Haematology/Oncology area includes Haematology and Oncology; Surgical Area includes Otorhinolaryngology, Plastic Surgery, General Surgery, Thoracic Surgery and Orthopaedics
Survey instruments
Clinician-perceived communication skills questionnaire
No validated instruments for measuring clinicians’ communication skills have been developed. An ad-hoc survey was developed by the authors, including a psychiatrist specialized in burnout and assisting cancer and terminal-ill patients and physicians specialized in providing specific supportive care with an advanced training in communication skills. In particular, one of them underwent a faculty development course of VitalTalk (www.vitaltalk.org) and all the other underwent communication skills training according to the same model. The Oncotalk/VitalTalk teaching model is based on evidence-based principles and includes brief didactic sessions to provide specific communication skills, demonstration of those skills by faculties, intensive skill practice with simulated patients during which group and faculties give feedbacks to the trainee focusing on trainee’s needs and attending to trainee’s attitudes and emotions [13]. The survey was based on previously published researches exploring physician communication of bad news through self-administered questionnaires, investigating the attitudes and problems in disclosure BBN, perceived confidence and outcome of physicians’ own communication skills, knowledge and self-efficacy about BBN, the usual practice, frequencies and format of communication with patients and/or family members [4, 14–20].
The tool is composed by a 23-item questionnaire for assessing physicians’ perceptions of their communication skills (CS) knowledge and self-rating of HC. The questionnaire was strictly confidential and anonymous. The following steps and key aspects of a clinician-patient encounter were investigated: 1) plan the encounter, 2) BBN, 3) discussing prognosis, 4) shared decision making process, 5) tracking and responding to emotions, 6) communication skill training (CST), 7) self-evaluation about communication skills. 16 out of 23 items allowed multiple answers and 7 had only one possible answer.
Burnout questionnaire
Burnout was measured using the validated Italian version of the Maslach Burnout Inventory - Human Services Survey (MBI-HSS), 22-items [1, 21]. The standard scoring for health care workers was used. Burnout syndrome was considered present if at least one of the three dimensions was severely abnormal, according to criteria proposed by Grunfeld et al. [21].
Statistical analysis
Descriptive statistics of the study sample were calculated; mean and standard deviation were used for continuous variables, whereas absolute and percentage frequencies were used for categorical variables. Results were expressed in terms of odds ratios (OR) with 95% confidence interval (95% CI) and associated p-values, comparing each modality with the reference modality. Association between our observed covariates and the presence of burnout was assessed by means of logistic regression models. First, a single-item analysis was performed, where the dependent variable was a positive score for burnout and the independent variables were the items of the communication skills questionnaire. The single-item analysis was carried out for all the 23 items of the questionnaire. Finally, a multivariable analysis was also performed, by considering a positive score for burnout as the dependent variable, while 8 items of the communication skills questionnaire as well as being a resident or a consultant as the independent variables. The 8 items, for a total of 25 covariates, were the following: 1, 4, 7, 9, 16, 19, 20, 22. These items were chosen because they resulted statistically significant in the single-item analysis. Only 2 items associated with measures of burnout in the single-item analysis, namely n 11 and n 23, were excluded, due to high rate of missing data, to maintain the ratio between subjects with burnout/evaluated covariates greater than five and to avoid the risk of multicollinearity in the covariates. Goodness-of-fit of our multivariable model was measured by means of the c-statistic (i.e. area under the ROC curve). Data were analysed by means of the R 3.4.3 software (The R Foundation for Statistical Computing, Wien).
Results
Communication skills questionnaire
A full report of the results is included in Table 2.
Table 2.
Physicians’ communication preferences
| IMAa | HOAb | SAc | TOT | IMA % | HOA% | SA % | TOT % | |
|---|---|---|---|---|---|---|---|---|
| Planning the encounter | ||||||||
| 1. How do you prepare for breaking bad news encounters? | ||||||||
| Have a consistent plan or strategy | 40 | 32 | 14 | 86 | 37% | 43% | 32% | 38% |
| No consistent approach to task | 42 | 30 | 15 | 87 | 39% | 41% | 34% | 39% |
| Use my experience | 19 | 5 | 3 | 27 | 18% | 7% | 7% | 12% |
| Follow my emotions | 7 | 6 | 7 | 20 | 7% | 8% | 16% | 9% |
| Plan to provide all relevant information at once then respond to questions | 22 | 17 | 13 | 52 | 21% | 23% | 30% | 23% |
| 2. In your opinion, would a strategy or approach to breaking bad news be important? | ||||||||
| Yes | 67 | 47 | 25 | 139 | 63% | 64% | 57% | 62% |
| No | 10 | 1 | 4 | 15 | 9% | 1% | 9% | 7% |
| Maybe | 28 | 20 | 13 | 61 | 26% | 27% | 30% | 27% |
| Don’t know | 2 | 6 | 2 | 10 | 2% | 8% | 5% | 4% |
| 3. In your opinion, why physicians do not use a strategy or approach to breaking bad news? | ||||||||
| Lack of time | 32 | 27 | 17 | 76 | 30% | 36% | 39% | 34% |
| Not necessary | 26 | 22 | 10 | 58 | 24% | 30% | 23% | 26% |
| Can’t say | 20 | 13 | 9 | 42 | 19% | 18% | 20% | 19% |
| Not to put distance between themselves and the patient | 23 | 15 | 7 | 45 | 21% | 20% | 16% | 20% |
| Don’t consider breaking bad news a clinical skill | 19 | 9 | 4 | 32 | 18% | 12% | 9% | 14% |
| Breaking bad news | ||||||||
| 4. What does breaking bad news mean for you? | ||||||||
| Discussing diagnosis | 22 | 17 | 5 | 44 | 21% | 23% | 11% | 20% |
| Telling patient he/she is terminally ill | 45 | 29 | 11 | 85 | 42% | 39% | 25% | 38% |
| Discussing a poor prognosis | 71 | 47 | 27 | 145 | 66% | 64% | 61% | 64% |
| Talking about end of active treatment | 57 | 47 | 16 | 120 | 53% | 64% | 36% | 53% |
| Discussing diagnosis of cancer | 35 | 25 | 5 | 65 | 33% | 34% | 11% | 29% |
| 5. In an average month, how often do you have to break bad news to a patient/family? | ||||||||
| Never | 6 | 0 | 10 | 16 | 6% | 0% | 23% | 7% |
| 1 to 5 times | 69 | 33 | 21 | 123 | 64% | 45% | 48% | 55% |
| 5 to 10 times | 26 | 21 | 7 | 54 | 24% | 28% | 16% | 24% |
| More than 10 times | 6 | 20 | 6 | 32 | 6% | 27% | 14% | 14% |
| 6. Which one do you think is the most difficult task of breaking bad news? | ||||||||
| Discussing prognosis | 60 | 45 | 20 | 125 | 56% | 61% | 45% | 56% |
| Telling patient about recurrence | 19 | 26 | 15 | 60 | 18% | 35% | 34% | 27% |
| Discussing transition to palliative care | 30 | 42 | 15 | 87 | 28% | 57% | 34% | 39% |
| Encouraging and dealing with family involvement | 15 | 10 | 5 | 30 | 14% | 14% | 11% | 13% |
| Discussing diagnosis | 22 | 11 | 6 | 39 | 21% | 15% | 14% | 17% |
| 7. How would you describe the part of your job in which you break bad news? | ||||||||
| Stimulating | 4 | 5 | 2 | 11 | 4% | 7% | 5% | 5% |
| Stressful | 36 | 33 | 14 | 83 | 34% | 45% | 32% | 37% |
| Emotionally engaging | 78 | 60 | 30 | 168 | 73% | 81% | 68% | 75% |
| Worrisome | 6 | 4 | 2 | 12 | 6% | 5% | 5% | 5% |
| Depressing | 9 | 5 | 3 | 17 | 8% | 7% | 7% | 8% |
| 8. What do you feel is the most difficult part of breaking bad news? | ||||||||
| Being honest but not taking away hope | 75 | 55 | 32 | 162 | 70% | 74% | 73% | 72% |
| Dealing with the patient’s emotions | 27 | 26 | 6 | 59 | 25% | 35% | 14% | 26% |
| Spending the right amount of time | 8 | 15 | 9 | 32 | 7% | 20% | 20% | 14% |
| Involving friends and family of the patient | 3 | 3 | 0 | 6 | 3% | 4% | 0% | 3% |
| Involving patient or family in decision making | 13 | 5 | 5 | 23 | 12% | 7% | 11% | 10% |
| Discussing prognosis | ||||||||
| 9. What does discussing prognosis mean for you? | ||||||||
| Information about illness trajectory and outcome | 56 | 42 | 19 | 117 | 52% | 57% | 43% | 52% |
| Success/failure rates of treatment options | 61 | 49 | 24 | 134 | 57% | 66% | 55% | 60% |
| Mean survival time for patients affected by the same disease and undergoing the same treatment | 20 | 14 | 6 | 40 | 19% | 19% | 14% | 18% |
| Chances of cure | 27 | 13 | 5 | 45 | 25% | 18% | 11% | 20% |
| Success rates of treatment options | 37 | 32 | 11 | 80 | 35% | 43% | 25% | 36% |
| 10. Would you inform patient and family about prognosis? | ||||||||
| Yes, certainly | 67 | 44 | 28 | 139 | 63% | 59% | 64% | 62% |
| No | 3 | 1 | 2 | 6 | 3% | 1% | 5% | 3% |
| Patient no, family yes | 13 | 11 | 5 | 29 | 12% | 15% | 11% | 13% |
| Family no, patient yes | 5 | 1 | 2 | 8 | 5% | 1% | 5% | 4% |
| Only if patient/family asks about it | 12 | 20 | 5 | 37 | 11% | 27% | 11% | 16% |
| Only under certain circumstances | 3 | 1 | 1 | 5 | 3% | 1% | 2% | 2% |
| 11. If yes, for which reason? | ||||||||
| Ethical reasons | 14 | 10 | 6 | 30 | 13% | 14% | 14% | 13% |
| Foster therapeutic compliance | 21 | 13 | 6 | 40 | 20% | 18% | 14% | 18% |
| Improve patient’s awareness of treatment plan | 23 | 22 | 17 | 62 | 21% | 30% | 39% | 28% |
| Make patient aware of illness trajectory, therapeutic choices and optimize adjustment to new conditions | 65 | 42 | 20 | 127 | 61% | 57% | 45% | 56% |
| 12. If not, for which reason? | ||||||||
| Physicians are not updated about diseases prognosis | 2 | 0 | 0 | 2 | 3% | 0% | 0% | 1% |
| Physicians do not know how to discuss prognosis | 1 | 2 | 1 | 4 | 2% | 3% | 5% | 3% |
| Lack of time | 0 | 1 | 0 | 1 | 0% | 2% | 0% | 1% |
| Not to take away hope | 10 | 13 | 5 | 28 | 16% | 22% | 24% | 20% |
| Not to scare patients | 4 | 7 | 0 | 11 | 7% | 12% | 0% | 8% |
| Patients might not be ready | 12 | 13 | 6 | 31 | 20% | 22% | 29% | 22% |
| Patients might not be able to handle emotions | 16 | 13 | 6 | 35 | 26% | 22% | 29% | 25% |
| Physicians cannot know every single patient’s prognosis | 12 | 5 | 1 | 18 | 20% | 8% | 5% | 13% |
| Physicians do not ask how patients want to discuss prognosis | 5 | 5 | 2 | 12 | 8% | 8% | 10% | 9% |
| Sharing decision making | ||||||||
| 13. Do you usually ask patients how much they want to know before breaking bad news? | ||||||||
| Yes | 23 | 25 | 11 | 59 | 21% | 33% | 25% | 26% |
| No | 84 | 50 | 33 | 167 | 79% | 67% | 75% | 74% |
| 14. In your opinion, why do not physicians ask patients how much they want to know? | ||||||||
| They can understand it all by themselves | 23 | 19 | 5 | 47 | 21% | 26% | 11% | 21% |
| Physicians always tell what they consider necessary | 30 | 27 | 16 | 73 | 28% | 36% | 36% | 32% |
| Patients might get scared by that question | 45 | 27 | 12 | 84 | 42% | 36% | 27% | 37% |
| Patients are always informed by physicians | 28 | 17 | 19 | 64 | 26% | 23% | 43% | 28% |
| 15. In an average month, how often do you talk to patients who do not want to receive information about their disease? | ||||||||
| Less than 5 times | 100 | 54 | 42 | 196 | 93% | 74% | 95% | 87% |
| 5 to 10 times | 4 | 17 | 1 | 22 | 4% | 23% | 2% | 10% |
| 10 to 20 times | 2 | 1 | 1 | 4 | 2% | 1% | 2% | 2% |
| More than 20 times | 1 | 1 | 0 | 2 | 1% | 1% | 0% | 1% |
| 16. What do you offer when discussing treatment options? | ||||||||
| The best treatment for the patient, to the best of my knowledge and belief | 72 | 52 | 33 | 157 | 67% | 70% | 75% | 70% |
| To choose between all the available treatment options | 17 | 5 | 8 | 30 | 16% | 7% | 18% | 13% |
| To share decision with me | 45 | 36 | 8 | 89 | 42% | 49% | 18% | 40% |
| To trust my opinion | 0 | 0 | 1 | 1 | 0% | 0% | 2% | 0% |
| The most innovative treatment option | 1 | 0 | 0 | 1 | 1% | 0% | 0% | 0% |
| 17. At the end of a visit, how often do you check for patient understanding? | ||||||||
| Every time | 43 | 22 | 16 | 81 | 40% | 30% | 36% | 36% |
| Never | 2 | 1 | 1 | 4 | 2% | 1% | 2% | 2% |
| Every time I think patient is not understanding | 61 | 50 | 24 | 135 | 57% | 68% | 55% | 60% |
| Every time I notice patient has limited health literacy | 12 | 5 | 2 | 19 | 11% | 7% | 5% | 8% |
| When patient asks me weird questions | 13 | 9 | 4 | 26 | 12% | 12% | 9% | 12% |
| Tracking and responding to emotions | ||||||||
| 18. Which of the following emotions do patients show you more often? | ||||||||
| Fear | 76 | 58 | 30 | 164 | 71% | 78% | 68% | 73% |
| Anger | 14 | 24 | 3 | 41 | 13% | 32% | 7% | 18% |
| Sadness | 34 | 31 | 16 | 81 | 32% | 42% | 36% | 36% |
| Disgust | 0 | 1 | 1 | 2 | 0% | 1% | 2% | 1% |
| Happiness | 6 | 5 | 0 | 11 | 6% | 7% | 0% | 5% |
| Disappointment | 13 | 15 | 5 | 33 | 12% | 20% | 11% | 15% |
| 19. What do you do when patients show you their feelings? | ||||||||
| Talk about the benefits of therapy | 12 | 6 | 8 | 26 | 11% | 8% | 18% | 12% |
| Remain silent waiting for the end | 15 | 15 | 4 | 34 | 14% | 20% | 9% | 15% |
| Address patients’ emotions with empathic responses | 74 | 49 | 22 | 145 | 69% | 66% | 50% | 64% |
| Highlight what is positive | 41 | 27 | 18 | 86 | 38% | 36% | 41% | 38% |
| Interrupt the visit then start again when patients are more relaxed | 1 | 1 | 0 | 2 | 1% | 1% | 0% | 1% |
| Communication skills training | ||||||||
| 20. How did you develop your communication skills? | ||||||||
| Observing mentors and older colleagues | 78 | 61 | 31 | 170 | 73% | 82% | 70% | 76% |
| Experience | 58 | 41 | 17 | 116 | 54% | 55% | 39% | 52% |
| Communication skills training courses | 8 | 7 | 0 | 15 | 7% | 9% | 0% | 7% |
| Textbooks and scientific literature | 6 | 4 | 4 | 14 | 6% | 5% | 9% | 6% |
| Medical school | 3 | 6 | 5 | 14 | 3% | 8% | 11% | 6% |
| 21. Would a strategy or approach to breaking serious news be helpful in your practice? | ||||||||
| Yes, certainly | 76 | 60 | 34 | 170 | 70% | 81% | 77% | 75% |
| No | 3 | 0 | 0 | 3 | 3% | 0% | 0% | 1% |
| It is not possible to determine in advance a way to do it regardless of the situation and the individual needs. | 29 | 14 | 10 | 53 | 27% | 19% | 23% | 24% |
| Self-evaluation | ||||||||
| 22. How do you feel about your own ability to break serious news? | ||||||||
| Very good | 2 | 0 | 2 | 4 | 2% | 0% | 5% | 2% |
| Good | 32 | 26 | 16 | 74 | 30% | 35% | 36% | 33% |
| Fair | 57 | 32 | 21 | 110 | 53% | 43% | 48% | 49% |
| Poor | 8 | 9 | 2 | 19 | 7% | 12% | 5% | 8% |
| Very poor | 9 | 7 | 3 | 19 | 8% | 9% | 7% | 8% |
| 23. In a qualitative study on patient-physician relationship, patients have been asked to “classify” their physicians basing on the attitudes and skills physicians showed them during treatments.[26] Which kind of physicians do you think you are? | ||||||||
| Unskilled | 25 | 14 | 6 | 45 | 24% | 21% | 14% | 21% |
| Emotionally overwhelmed | 4 | 2 | 1 | 7 | 4% | 3% | 2% | 3% |
| Tough but skillful | 6 | 4 | 6 | 16 | 6% | 6% | 14% | 8% |
| Insensitive but skillful | 4 | 1 | 2 | 7 | 4% | 1% | 5% | 3% |
| Detached | 6 | 1 | 1 | 8 | 6% | 1% | 2% | 4% |
| Empathic and professional | 59 | 45 | 26 | 130 | 57% | 67% | 62% | 61% |
Abbreviations: IMA Internal Medicine Area, HOA Haematology/Oncology Area, SA Surgical Area
Among the most notable answers, there were the following: in the “plan the encounter” section, 139 physicians (62%) considered important to have a plan before BBN encounter. However, only 86 (38%) admitted preparing one, while 87 (39%) reported not to have a plan for the encounter, providing lack of time (N = 76, 34%) and the idea that planning may not be necessary (N = 58, 26%) as the main causes.
When asked about “definition of BBN”, 145 (64%) and 120 (53%) physicians answered that BBN means discussing a poor prognosis or talking about the end of disease-modifying treatment, respectively. Discussing prognosis and transition to palliative care were considered to be the most difficult tasks of BBN by 125 (56%) and 87 (39%) physicians. 168 (75%) of interviewees described BBN as emotionally engaging and 83 (37%) stressful. The most difficult part of BBN was balancing hope with honesty for 162 (75%) physician. 59 (26%) reported this was dealing with patients’ emotions.
As to “discussing prognosis”, 139 (62%) physicians would be in favour of informing both patients and families about prognosis, mainly because they believe it promotes patients’ coping skills and empowerment. Nevertheless, 125 (56%) physicians acknowledged that they disclose prognosis only by talking about the rates for cure and response of treatment options.
When asked about “sharing decision making”, 167 physicians (74%) revealed they do not usually ask patients how much information they want to know before BBN, mainly because they think that it is already felt by patients as worrisome, and patients may get scared simply by such question [84 (37%)]. As to discussing treatment options, 157 (70%) physicians just recommended the best treatment, in their opinion for the patients, while 89 (40%) attempted to share the decision making. Only 81 (36%) declared to check the patients understanding at the end of every visit.
Regarding to “tracking and responding to emotions”, 164 (73%) physicians thought fear to be the most common emotion showed by patients. Overall, 145 (64%) reported to address patients’ emotions with empathic responses.
The vast majority of respondent (170, 76%) based their HC professional development by observing colleagues and/or relied on experience. Only 15 (7%) and 14 (6%) physicians, respectively, reported attended CS training courses or receiving this training in Medical Schools. 14 (6%) relied on learning CS from textbooks or the scientific literature.
188 (84%) physicians considered themselves to be at least fair at BBN and 130 (61%) to be empathic and professional, while 45 (21%) acknowledged themselves to be unskilled for the task. Three quarters of the sample admitted not having an evidence based approach and that a strategy to BBN would be helpful in their clinical practice.
Burnout
211 (93%) out of 226 questionnaires were fully evaluable for analysis. 124 (59%), physicians reached clinical significance of burnout in at least one of the 3 dimensions. In details, 66 (53%) out of 124 in 1 dimension; 46 (37%) in 2 dimensions and 12 (10%) in all 3 dimensions. Burnout levels of junior doctor, while they are acquiring specialization, were higher than those of consultants in a statistically significant manner (60 (65%) out of 99 vs 57 (52%) out of 109; OR 1.75; 95% CI 1.00 to 3.04; p = 0.049) (Fig. 1b).
Associations between physicians’ communication skills and burnout
Single-item analysis
In our single-item analysis, the following variables were related to high levels of burnout: 1) physicians believing that BBN means discussing a poor prognosis (p = 0.039); 2) physicians self-assessing BBN to be a stressful task for themselves (p = 0.001); 3) discussing prognosis only including the rates for cure (p = 0.036); 4) feeling unskilled at patient-physician relationship (p = 0.029) and 5) being a resident (p = 0.049). On the contrary, the following variables were found to be related to low levels of burnout: 1) considering BBN an emotionally engaging task (p = 0.042); 2) having a consistent plan for communicating with patients (p = 0.040); 3) responding to patients’ emotions with empathic responses (p = 0.017); 4) discussing prognosis with the goal of promoting awareness of illness trajectory, therapeutic choices and to optimize patients’ coping (p = 0.010); 5) sharing decisions with patients (p = 0.019); 6) developing CS by using textbooks and scientific literature (p = 0.011); 7) feeling to be good or very good at CS (p = 0.000); 8) graduation within the last 6 to 16 years (p = 0.003) (Table 3).
Table 3.
Associations between communication patterns and burnout: single-item analysis
| Variables | All physicians (n = 211) N (%) |
Physicians with burnout (n = 124) N (%) |
OR | 95% CI | P value |
|---|---|---|---|---|---|
| Factors associated with high risk of burnout | |||||
| Breaking bad news means discussing a poor prognosis | |||||
| Yes | 136 (64%) | 86 (69%) | 1.94 | 1.03–3.64 | 0.039 |
| No | 75 (36%) | 38 (31%) | |||
| Breaking bad news is stressful | |||||
| Yes | 78 (37%) | 57 (46%) | 2.92 | 1.49–5.73 | 0.001 |
| No | 133 (63%) | 67 (54%) | |||
| Discussing prognosis is talking about the success of treatment options | |||||
| Yes | 75 (36%) | 52 (42%) | 2.12 | 1.05–4.28 | 0.036 |
| No | 136 (64%) | 72 (58%) | |||
| Self-evaluating as unskilled at patient-physician communication | |||||
| Yes | 44 (22%) | 31 (27%) | 2.27 | 1.04–4.75 | 0.029 |
| No | 156 (78%) | 85 (73%) | |||
| Professional Role | |||||
| Resident | 93 (46%) | 60 (51%) | 1.75 | 1.00–3.04 | 0.049 |
| Consultant | 109 (54%) | 57 (49%) | |||
| Factors associated with low risk of burnout | |||||
| Having a consistent plan for communication | |||||
| Yes | 80 (38%) | 40 (32%) | 0.37 | 0.14–0.96 | 0.040 |
| No | 130 (62%) | 84 (68%) | |||
| Breaking bad news only considered as emotionally engaging | |||||
| Yes | 158 (75%) | 89 (72%) | 0.56 | 0.31–0.98 | 0.042 |
| No | 53 (25%) | 35 (28%) | |||
| Addressing patients’ emotions with empathic responses | |||||
| Yes | 137 (66%) | 71 (58%) | 0.39 | 0.18–0.85 | 0.017 |
| No | 72 (34%) | 51 (42%) | |||
| Discussing prognosis with the goal of promoting awareness of illness trajectory, therapeutic choices and to optimize patients’ adjustment | |||||
| Yes | 119 (69%) | 65 (63%) | 0.44 | 0.24–0.82 | 0.010 |
| No | 53 (31%) | 38 (37%) | |||
| Sharing decisions with patients | |||||
| Yes | 86 (41%) | 42 (34%) | 0.46 | 0.24–0.88 | 0.019 |
| No | 125 (59%) | 82 (66%) | |||
| Mastering communication skills by using textbooks and scientific literature | |||||
| Yes | 13 (6%) | 3 (2%) | 0.18 | 0.01–0.68 | 0.011 |
| No | 198 (94%) | 121 (98%) | |||
| Self-evaluating communication skills as good or very good | |||||
| Yes | 74 (35%) | 30 (24%) | 0.31 | 0.17–0.56 | 0.000 |
| No | 136 (75%) | 93 (76%) | |||
| Years from graduation | |||||
| 6–16 | 60 (52%) | 29 (23%a) | 0.29 | 0.13–0.67 | 0.003 |
| 0–3 | 55 (48%) | 37 (30%a) | |||
aThe sum of these fractions is < 1 as the two compared covariates represent only a part of the whole responders cohort
Shown are only statistically significant associations. Percentages are calculated as fractions of responders to each item
Abbreviations: OR Odds Ratio, CI Confidence Interval
Multivariable analysis
The multivariable logistic regression model confirmed that physicians self-assessing BBN to be a stressful task for themselves (OR 3.01; 95% CI 1.26 to 7.19; p = 0.013) were associated with high levels of burnout; whereas a) physicians referring to plan in advance before communicating with patients (OR 0.43; 95% CI 0.21 to 0.89; p = 0.023), b) physicians reporting to have learnt CS from textbooks and scientific literature (OR 0.21; 0.05 to 0.93; p = 0.039) and c) physicians self-evaluating their ability to break bad news as good or very good (OR 0.32; 0.15 to 0.71; p = 0.005) were associated with low levels of burnout (Table 4). All other independent variables included in the multivariable model were not significantly associated to the presence of burnout. Goodness-of-fit of our multivariable model was good, as the c-statistic was equal to 0.78.
Table 4.
Associations between communication patterns and burnout: multivariable analysis
| Variables | OR | 95% CI | P value |
|---|---|---|---|
| Factors associated with high risk of burnout | |||
| Breaking bad news is stressful | 3.01 | 1.26–7.19 | 0.013 |
| Factors associated with low risk of burnout | |||
| Having a consistent plan for communication | 0.43 | 0.21–0.89 | 0.023 |
| Mastering communication skills by using textbooks and scientific literature | 0.21 | 0.05–0.93 | 0.039 |
| Self-evaluating communication skills as good or very good | 0.32 | 0.15–0.71 | 0.005 |
Shown are only statistically significant associations
Abbreviations: OR Odds Ratio, CI Confidence Interval
Discussion
This study collects descriptions and opinions of a sample of Italian hospital medical doctors on their own HC, including specific behaviours, thoughts, and feelings they might experience while getting ready for and performing difficult communication tasks. Moreover, it informs some of the factors and how they might relate to burnout metrics.
Results are consistent with those of previous surveys, mainly focused on the disclosure of the diagnosis, such as that from the American Society of Clinical Oncology [14, 16, 19, 22]. The majority of our respondents believed that BBN mainly equals discussing a poor prognosis, that discussing prognosis is the most difficult communication task, and that BBN is very emotionally engaging or stressful. Most clinicians admitted not using a consistent evidence-based framework for BBN encounter, not asking the patients the amount of information they want to receive, and checking for understanding only if they think this may be impaired. Fear is generally reported as the most frequently emotion raised in patients while discussing such topics. Respondents rated themselves good or at least fair in BBN and mostly reported acquiring CS empirically by observing colleagues. Of note, they reported very low rates of CS training both at medical school and beyond.
Also the frequency of burnout in our population is similar to that reported in US practising physicians, where nearly 60% of them experience the syndrome at some point in their career [2, 23, 24]. In Europe, similar rates were documented among French and Swiss physicians, 49 and 70%, respectively [25, 26]. Present data also confirm that younger medical doctors or residents have been reported to be exposed to an even higher risk [27].
The other important finding of our study is that, for the first time, it documents significant associations between some self-efficacy patterns regarding communication to patients and the risk of burnout. This study shows that physicians self-assessing BBN as a stressful task are exposed to a higher risk of burnout, up to three folds.
Previous researches have so far reported that BBN to patients have always been challenging for clinicians, either because many of them are concerned that honest information can damage patients’ hope or because they feel uncertain in managing patients’ emotion and estimating patients’ survival [28]. Indeed, by demonstrating the increase of several physiological indices (e.g. heart rate, blood pressure, skin conductance, cortisol levels, etc. …) during BBN encounters, other studies have empirically confirmed that physicians perceive BBN as a stressful task [9–11].
Our report supported by quantitative data suggests that these areas of self-efficacy, related to the distress, deriving from the uncertainty and the emotional burden, are linked to burnout.
Interestingly, clinicians for whom BBN means discussing a poor prognosis and who disclose prognosis only by talking about the success rate of therapies find themselves at a higher risk of burnout - although those were detected only in the single-item analysis. These findings suggest that the physicians’ uneasiness in discussing prognosis and the sole conscious positive estimate of treatment efficacy may have unintended consequences not only for patients, who may be led to seek life-sustaining therapies even in phases where active treatments will not be helpful, but also for physicians, who expose themselves to burnout, by risking losing patients’ trust when things get worse [29]. In the last few years, while new therapeutic technologies have progressively enabled patients to live longer with their disease than ever before, this has become even more complex [30].
Our data show that an evidence-based theoretical framework for the encounter may be protective of burnout in a statistically significant manner. This is even more important if we consider that the majority of our interviewed physicians admit not to plan a BBN encounter because of lack of time or because they consider this approach to be worthless. Previous qualitative studies found evidence that simple behavioral training has potential to positively affect physician-patient relationship and are felt beneficial by physician in terms of reducing BBN-related stress [31]. Our findings supported by quantitative data the effectiveness of this approach, and, together with the data that physicians who delay serious news discussions may experience high levels of burnout, further validate the importance of planning difficult communication tasks as a burnout prevention strategy. Furthermore, we found that physicians who are aware of communication skills by means of textbooks and scientific literature and those evaluating their ability to BBN at least good are exposed to low levels of burnout, in a statistically significant manner. Indeed, although understanding what patients want to know and delivering worrisome information may be stressful for clinicians, it has been reported that standard communication protocol may increase the confidence, the ability of physicians to disclose unfavourable medical information, eventually reducing the BBN related-stress, and may also increase patients’ rating of medical professionalism [32]. These findings, associated with the results of the single-item analysis, reporting low levels of burnout for physicians addressing patients’ emotions with empathy and fostering shared decision making, further support the relevance of acquiring, practising and improving basic CS as burnout prevention strategy [20].
Our study has several limitations. First, it was conducted on a sample of physicians who work in Modena, therefore the results we describe could not represent the entire national or international population. However, it should be recognised that a measurable rate of the interviewed physicians attended medical schools in different Italian regions, increasing at least in part the generalizability of the results. Second, the design of our study does not allow to establish an undoubted cause-effect association between the communication patterns and burnout metrics. Repeated monitoring of the same population over time would have consolidated the results. However, it has been recognised that the use of multiple assessments impairs similarly the reliability of the studies by increasing the likelihood of finding results. An ad-hoc survey was used and we acknowledge that objective measures of CST efficacy including the use of audio-recording of the medical encounters, for example, would provide more objective information about their communication habits. However, our data are consistent with the results of other surveys about communication and burnout rates in different countries and in different historical periods.
Conclusions
In conclusion, our study suggests that physicians’ attitudes and practices about and during difficult communication tasks may influence their risk of burnout. These results support the relevance of embedding evidence-based communication skill training at all levels of professional medical development. Given the potential burnout impact for doctors it may be worth considering priority areas such as BBN and prognostication integrated with core CST to ensure they have mastered the foundation skills. Further studies on large number of physicians of different background and in different Countries are needed to confirm our results.
Acknowledgements
Not applicable.
Abbreviations
- BBN
Breaking bad news
- PEE
Physical and emotional exhaustion
- CD
Cynicism and depersonalization
- PA
Personal accomplishment
- HC
Healthcare communication
- CS
Communication skills
- MBI-HSS
Maslach Burnout Inventory - Human Services Survey
- OR
Odds ratio
- CI
Confidence interval
- CST
Communication skill training
Authors’ contributions
LP, ML, FB, EmBa and AM conceived and designed the study; SF, ElBa and GMG designed the study; AM, EC, VP, DG, HC, MM, RD’A, FB, EmBa, ElBo and FF acquired and analyzed data; SB, PM, FE, ML and LP interpreted the data, FE, PM, EmBa, ML and LP drafted the manuscript and revised it. All authors read and approved the final manuscript.
Funding
This work was supported by grants of the Associazione Italiana Lotta alle Leucemie, Linfoma e Mieloma (AIL) – Sezione “Luciano Pavarotti”-Modena-ONLUS (Gold Charity Dinner Show “Inno alla Vita” initiative, by Dr. Alberto Fontana) and is also part of Programma di Ricerca Regione Emilia Romagna-Università, Ricerca per il Governo Clinico, 2010–2012 (3b211–19 to M.L.).
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This study was conducted in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the local Ethical Committee (CE protocol n° 244/16).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Peter Martin, Fabio Efficace, Mario Luppi and Leonardo Potenza contributed equally to this work.
References
- 1.Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 2.West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388:2272–2281. doi: 10.1016/S0140-6736(16)31279-X. [DOI] [PubMed] [Google Scholar]
- 3.Hlubocky FJ, Back AL, Shanafelt TD. Addressing Burnout in Oncology: Why Cancer Care Clinicians Are At Risk, What Individuals Can Do, and How Organizations Can Respond. Am Soc Clin Oncol Educ Book. 2016;35:271–279. doi: 10.14694/EDBK_156120. [DOI] [PubMed] [Google Scholar]
- 4.van Vliet LM, Epstein AS. Current state of the art and science of patient-clinician communication in progressive disease: patients’ need to know and need to feel known. J Clin Oncol. 2014;32:3474–3478. doi: 10.1200/JCO.2014.56.0425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. doi: 10.1037/0033-295X.84.2.191. [DOI] [PubMed] [Google Scholar]
- 6.Ammentorp J, Sabroe S, Kofoed PE, Mainz J. The effect of training in communication skills on medical doctors' and nurses' self-efficacy. A randomized controlled trial. Patient Educ Couns. 2007;66:270–277. doi: 10.1016/j.pec.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 7.Kissane DW, Bylund CL, Banerjee SC, et al. Communication skills training for oncology professionals. J Clin Oncol. 2012;30:1242–1247. doi: 10.1200/JCO.2011.39.6184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fallowfield L, Jenkins V. Communicating sad, bad, and difficult news in medicine. Lancet. 2004;363:312–319. doi: 10.1016/S0140-6736(03)15392-5. [DOI] [PubMed] [Google Scholar]
- 9.Brown R, Dunn S, Byrnes K, Morris R, Heinrich P, Shaw J. Doctors’ stress responses and poor communication performance in simulated bad-news consultations. Acad Med J Assoc Am Med Coll. 2009;84:1595–1602. doi: 10.1097/ACM.0b013e3181baf537. [DOI] [PubMed] [Google Scholar]
- 10.Shaw JM, Brown RF, Dunn SM. A qualitative study of stress and coping responses in doctors breaking bad news. Patient Educ Couns. 2013;91:243–248. doi: 10.1016/j.pec.2012.11.006. [DOI] [PubMed] [Google Scholar]
- 11.Shaw J, Brown R, Dunn S. The impact of delivery style on doctors’ experience of stress during simulated bad news consultations. Patient Educ Couns. 2015;98:1255–1259. doi: 10.1016/j.pec.2015.08.023. [DOI] [PubMed] [Google Scholar]
- 12.Bousquet G, Orri M, Winterman S, Brugière C, Verneuil L, Revah-Levy A. Breaking bad news in oncology: a Metasynthesis. J Clin Oncol. 2015;33:2437–2443. doi: 10.1200/JCO.2014.59.6759. [DOI] [PubMed] [Google Scholar]
- 13.Arnold RM, Back AL, Baile WF, Edwards KA, Tulsky JA. In: Oxford textbook communication in oncology and palliative care. 2. Kissane DW, Bultz BD, Butow PN, Bylund CL, Noble S, Wilkinson S, editors. Oxford: Oxford University Press; 2017. pp. 363–368. [Google Scholar]
- 14.Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP. SPIKES-A six-step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5:302–311. doi: 10.1634/theoncologist.5-4-302. [DOI] [PubMed] [Google Scholar]
- 15.Gilligan T, Coyle N, Frankel RM, et al. Patient-clinician communication: American Society of Clinical Oncology consensus guideline. J Clin Oncol. 2017;35:3618–3632. doi: 10.1200/JCO.2017.75.2311. [DOI] [PubMed] [Google Scholar]
- 16.Grassi L, Giraldi T, Messina EG, Magnani K, Valle E, Cartei G. Physicians’ attitudes to and problems with truth-telling to cancer patients. Support Care Cancer. 2000;8:40–45. doi: 10.1007/s005209900067. [DOI] [PubMed] [Google Scholar]
- 17.Gorniewicz J, Floyd M, Krishnan K, Bishop TW, Tudiver F, Lang F. Breaking bad news to patients with cancer: a randomized control trial of a brief communication skills training module incorporating the stories and preferences of actual patients. Patient Educ Couns. 2017;100:655–666. doi: 10.1016/j.pec.2016.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Daugherty CK, Hlubocky FJ. What terminally ill cancer patients told about their expected death? A study of cancer physicians' self-reports of prognosis disclosure. J Clin Oncol. 2008;26:5988–5993. doi: 10.1200/JCO.2008.17.2221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Voorhees J, Rietjens J, Onwuteaka-Philipsen B, Deliens L, Cartwright C, Faisst K, et al. Discussing prognosis with terminally ill cancer patients and relatives: a survey of physicians’ intentions in seven countries. Patient Educ Couns. 2009;77:430–436. doi: 10.1016/j.pec.2009.09.013. [DOI] [PubMed] [Google Scholar]
- 20.Curtis JR, Wenrich MD, Carline JD, Shannon SE, Ambrozy DM, Ramsey PG. Understanding physicians' skills at providing end-of-life care perspectives of patients, families, and health care workers. J Gen Intern Med. 2001;16:41–49. doi: 10.1111/j.1525-1497.2001.00333.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grunfeld E, Whelan TJ, Zitzelsberger L, Willan AR, Montesanto B, Evans WK. Cancer care workers in Ontario: prevalence of burnout, job stress and job satisfaction. CMAJ Can Med Assoc J. 2000;163:166–169. [PMC free article] [PubMed] [Google Scholar]
- 22.Christakis NA, Iwashyna TJ. Attitude and self-reported practice regarding prognostication in a national sample of internists. Arch Intern Med. 1998;158:2389–2395. doi: 10.1001/archinte.158.21.2389. [DOI] [PubMed] [Google Scholar]
- 23.Shanafelt TD, Hasan O, Dyrbye LN, Sinsky C, Satele D, Sloan J, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90:1600–1613. doi: 10.1016/j.mayocp.2015.08.023. [DOI] [PubMed] [Google Scholar]
- 24.Rotenstein LS, Torre M, Ramos MA, et al. Prevalence of burnout among physicians: a systematic review. JAMA. 2018;320:1131–1150. doi: 10.1001/jama.2018.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kansoun Z, Boyer L, Hodgkinson M, Villes V, Lançon C, Fond G. Burnout in French physicians: a systematic review and meta-analysis. J Affect Disord. 2019;246:132–147. doi: 10.1016/j.jad.2018.12.056. [DOI] [PubMed] [Google Scholar]
- 26.Hamming O. Explaining burnout and the intention to leave the profession among health professionals - a cross-sectional study in hospital setting in Switzerland. BMC Health Serv Rev. 2018;18:785–796. doi: 10.1186/s12913-018-3556-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jovanović N, Podlesek A, Volpe U, et al. Burnout syndrome among psychiatric trainees in 22 countries: risk increased by long working hours, lack of supervision, and psychiatry not being first career choice. Eur Psychiatry. 2016;32:34–41. doi: 10.1016/j.eurpsy.2015.10.007. [DOI] [PubMed] [Google Scholar]
- 28.Back AL, Arnold RM. Discussing prognosis: “how much do you want to know?” talking to patients who are prepared for explicit information. J Clin Oncol. 2006;24:4209–4213. doi: 10.1200/JCO.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 29.Fallowfield LJ, Jenkins VA, Beveridge HA. Truth may hurt but deceit hurts more: communication in palliative care. Palliat Med. 2002;16:297–303. doi: 10.1191/0269216302pm575oa. [DOI] [PubMed] [Google Scholar]
- 30.Temel JS, Shaw AT, Greer JA. Challenge of prognostic uncertainty in the modern era of Cancer therapeutics. J Clin Oncol. 2016;34:3605–3608. doi: 10.1200/JCO.2016.67.8573. [DOI] [PubMed] [Google Scholar]
- 31.Rodriguez HP, Anastario MP, Frankel RM, Odigie EG, Rogers WH, von Glahn T, et al. Can teaching agenda-setting skills to physicians improve clinical interaction quality? A controlled intervention. BMC Med Educ. 2008;8:3. doi: 10.1186/1472-6920-8-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Back AL, Deignan PF, Potter PA. Compassion, compassion fatigue, and burnout: key insights for oncology professionals. Am Soc Clin Oncol Educ Book. 2014:e454–9. 10.14694/EdBook_AM.2014.34.e454. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.