Abstract
Objectives
Lockdown measures in response to the coronavirus disease 2019 (COVID-19) pandemic can have serious mental health effects on the population, especially in vulnerable groups, such as those living in poor socio-economic conditions, those who are homeless, migrant workers and asylum seekers/refugees. In addition, these vulnerable groups frequently have greater difficulty accessing health services and in treatment adherence. The aim of this study is to estimate the impact of the COVID-19–related lockdown on service utilisation and follow-up adherence in an Italian mental health outpatient service for migrants and individuals in socio-economic difficulties.
Study design
The design of this study is a retrospective cross-sectional study.
Methods
All patients who visited the mental health outpatient service in the months of February and March in the years 2017–2020 were included in the study. To compare service utilisation before and after the lockdown, the number of patients who visited the mental health outpatient service for psychiatric interview were recorded. Follow-up adherence was calculated as the percentage of patients who visited in February and subsequently attended a follow-up visit in March of the same year.
Results
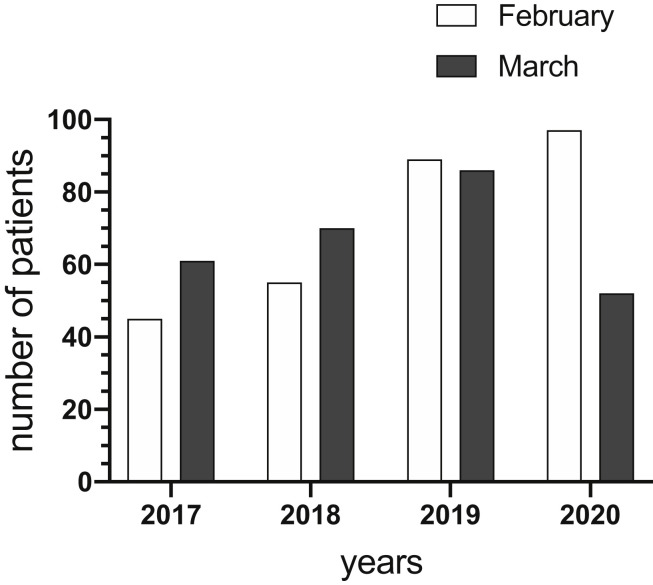
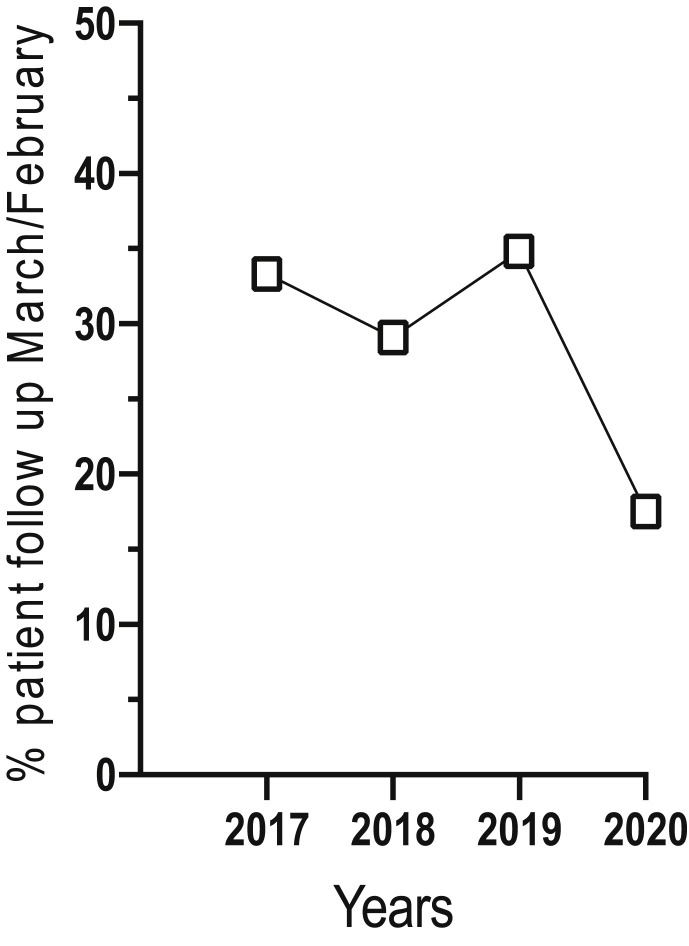
The number of patients who visited the outpatient service between February 2017 and February 2020 was continuously increasing. In March 2020, fewer patients visited the service for psychiatric interview, in line with the introduction of lockdown measures. In addition, the number of the patients who visited in February 2020 and returned for their follow-up visits in March 2020 declined from approximately 30% over the same months in 2017–2019 to 17.53% in March 2020.
Conclusions
The lockdown-related reduction in numbers of patients accessing the mental health service makes it difficult to help vulnerable populations during a period of time in which their mental health needs are expected to increase. Moreover, the reduction seen in follow-up compliance increases the risk of treatment discontinuation and possible relapse. Proactive alternative strategies need to be developed to reach these vulnerable populations.
Keywords: Coronavirus, Mental health, Service utilisation, Immigrants, Refugees, Homeless
Highlights
-
•
Lockdown can have serious mental health effects on vulnerable groups.
-
•
These population subgroups also have greater difficulties in accessing health services and maintaining treatment adherence.
-
•
Access to mental health services and follow-up compliance dramatically dropped as a consequence of lockdown.
-
•
Vulnerable groups are at risk of unmet mental health needs, treatment discontinuation and possible relapse.
-
•
Proactive alternative strategies need to be developed to reach these vulnerable populations.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic, as a result of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, has led to a public health emergency, thousands of deaths, generalised economic depression, unemployment and worldwide quarantines. Italy was the first European country to be severely impacted by the disease, with the total number of cases currently being 238,499, with 34,634 deaths.1 On 8 March 2020, in response to the growing pandemic of COVID-19 in the country, the Italian government imposed a national restriction of movements of the population, with the exceptions of buying food and other necessary items (e.g. drugs, disinfectants), essential work and health emergencies.2 The national lockdown ended in June 2020 and proved to be useful in reducing the spread of SARS-CoV-2 infection.
However, such restrictive measures will likely have serious mental health effects on the population.3, 4, 5, 6 In particular, there are certain subgroups of the population that are particularly at risk in this situation due to their precrisis vulnerability. Among them, there are those who live in poor socio-economic conditions,7 , 8 those who are homeless,9 migrant workers,10 , 11 asylum seekers and refugees12 , 13 and patients with existing mental health disorders.14 , 15 In addition, some individuals will fall into several of these subgroups, thus increasing their risk.16 For example, asylum seekers whose request of international protection has been rejected are often homeless, without documents, without jobs, live in poverty and also have symptoms of post-traumatic stress disorder (PTSD) due to their migratory experience, as well as depressive and adjustment disorders related to their present poor living conditions. This is not an unusual problem in Italy, and it has actually worsened over the last year due to a law removing the ‘humanitarian’ forms of permission of stay in the country and consequently the right for those people to be hosted in reception centres and get a job.17
Previous research has shown that migrants in poor sociocultural conditions have an increased risk of mental health problems, including the worsening of PTSD,18 higher rates of psychoses19 and difficultly in access and/or inadequate treatment in some mental health services of the Italian National Health Service.20 , 21
There is evidence that the COVID-19 crisis has had a negative impact on the mental health of vulnerable populations through different mechanisms.22 , 23 Unfortunately, no data are currently available in specific populations, such as those investigated in this study; however, the authors recently performed a phone-based data collection survey (personal data, article in preparation) showing that there are several pathways leading to mental distress. For example, participants reported intrinsic effects related to anxieties of being infected; consequences of the quarantine, both on living experience (e.g. sense of imprisonment reminding traumatic experiences, intolerance to inactivity, boredom, depression) and interpersonal relationships (e.g. forced and conflictual cohabitation in reception centres); fears for the health of relatives living in their home countries; increased social marginalisation (e.g. homeless remained without food, clothing, furniture, laundry and washing facilities or without acceptance in public dormitories); job loss and additional economic difficulties; reduction of the activities in the mental health outpatient services, with increased difficulty in accessing them; increased fears of being taken by the police in the cases of undocumented migrants (the reduction of people around the city made them more visible in the streets) and inability to obtain necessary medications.
The aim of this study is to evaluate the impact of the COVID-19–related lockdown on two specific problems possibly faced by mental health patients with a history of immigration and/or socio-economic difficulties: that is, difficulties in mental health service utilisation and follow-up adherence. In particular, the study was conducted in an Italian public health outpatient service that was specifically dedicated to migrants and individuals with socio-economic difficulties. The authors believe that this study is necessary because problems at this level have been predicted on the basis of theoretical considerations but, to the authors’ knowledge, no evidence measuring this effect is currently available. Moreover, centres dedicated to migrants are frequently based on volunteers, and their reports often remain in the grey literature, thus remain difficult to access by the scientific community.
Methods
This retrospective study was conducted by the Mental Health Unit of the Italian National Institute for Health, Migration and Poverty (INMP), based in Rome. To facilitate access of migrants and homeless people, the INMP uses a low-threshold setting with a transcultural approach model. Information routinely and systematically collected in medical records was used, and all patients signed an informed consent form to use their data for study and research purposes.
The study included all patients who received at least one psychiatric interview in February (286 patients) and March (269 patients) in the years 2017–2020. Patients who visited the service in February were considered as the baseline population. Their sociodemographic data and diagnoses were considered in the sample description. Psychiatric disorders were categorised into eleven groups, reflecting the frequency of International Classification of Diseases (ICD)-9 disorders diagnosed in the healthcare unit (the ICD-9 diagnostic system is currently for official statistical recording used in Italy).
The number of patients who visited in February was also compared with those who visited in March for each particular year group. For 2020, the number of patients who visited in February and March was divided into three time periods of about ten days for each month (1-10th, 11-20th and 21-end of the month) to highlight the fact that the change started after the lockdown was established. Furthermore, to assess follow-up compliance, we used, as proxy, the number of patients who visited the service in February and then attended at least one follow-up visit the following month.
Data analysis
The sociodemographic characteristics and psychiatric categories of the study population are reported, and trends in the number of patients attending interviews are shown graphically. Continuous variables were computed as means ± standard deviations (SDs), and categorical variables were calculated as frequencies. Trend differences were reported as absolute numbers or percentage change when appropriate. In addition, the 95% confidence interval (CI) of percentage change was calculated and significance reported.
Results
Table 1 summarises the characteristics of the 286 patients who visited the mental health outpatient service in February. Participants were mainly men (75.17%) and had a mean age (±SD) of 37.37 (±13.43) years. Patient age and gender did not differ significantly between the study years. Geopolitical areas of provenance and diagnostic groups changed each year depending on unpredictable pathways of access related to the population dynamics, although the main provenance of Africa (above all Western/Central Africa) remained, and a prevalence for PTSD and depressive, adjustment and psychotic conditions was maintained. The proportion of Italians in poor socio-economic conditions who visited the outpatient service fluctuated between 5% and 10%.
Table 1.
Characteristics of patients who visited the mental health outpatient service in February 2017–2020.
| Characteristic | Year |
|||
|---|---|---|---|---|
| 2017 | 2018 | 2019 | 2020 | |
| No. of patient visits in February | 45 | 55 | 89 | 97 |
| Age in years (mean ± SD) | 33.58 (±10.57) | 38.55 (±14.94) | 36.11 (±13.24) | 39.61 (±13.57) |
| Women [n (%)] | 14 (31.11%) | 13 (23.64%) | 17 (19.10%) | 27 (27.84%) |
| Geopolitical area of provenance [n (%)] | ||||
| Western/Central Africa | 21 (46.67%) | 21 (38.18%) | 47 (52.81%) | 33 (34.02%) |
| South/Central Asia | 6 (13.33%) | 4 (7.27%) | 1 (1.12%) | 11 (11.34%) |
| East Africa | 5 (11.11%) | 2 (3.64%) | 4 (4.49%) | 6 (6.19%) |
| Europe | 4 (8.89%) | 13 (23.64%) | 4 (4.49%) | 18 (18.56%) |
| Italy | 3 (6.67%) | 4 (7.27%) | 9 (10.11%) | 5 (5.15%) |
| South/Central America | 3 (6.67%) | 2 (3.64%) | 10 (11.24%) | 11 (11.34%) |
| East Asia | 2 (4.44%) | 1 (1.82%) | 1 (1.12%) | 0 (0%) |
| Middle East | 1 (2.22%) | 1 (1.82%) | 5 (5.62%) | 7 (7.22%) |
| North Africa | 0 (0%) | 7 (12.73%) | 8 (8.99%) | 6 (6.19%) |
| Diagnosis [n (%)] | ||||
| PTSD | 11 (24.44%) | 12 (21.82%) | 28 (31.46%) | 29 (29.90%) |
| Psychosis | 7 (15.56%) | 8 (14.55%) | 19 (21.35%) | 9 (9.28%) |
| Depression | 5 (11.11%) | 13 (23.64%) | 10 (11.24%) | 20 (20.62%) |
| Anxiety | 4 (8.89%) | 2 (3.64%) | 3 (3.37%) | 2 (2.06%) |
| Adjustment disorder | 3 (6.67%) | 8 (14.55%) | 3 (3.37%) | 7 (7.22%) |
| Somatization | 3 (6.67%) | 4 (7.27%) | 3 (3.37%) | 5 (5.15%) |
| Personality disorder | 2 (4.44%) | 1 (1.82%) | 10 (11.24%) | 5 (5.15%) |
| Bipolar disorder | 1 (2.22%) | 1 (1.82%) | 1 (1.12%) | 3 (3.09%) |
| Alcoholism | 0 (0%) | 3 (5.45%) | 1 (1.12%) | 6 (6.19%) |
| Other mental disorder | 4 (8.89%) | 3 (5.45%) | 9 (10.11%) | 10 (10.31%) |
| No mental disorder | 5 (11.11%) | 0 (0%) | 2 (2.25%) | 1 (1.03%) |
PTSD, post-traumatic stress disorder; SD, standard deviation.
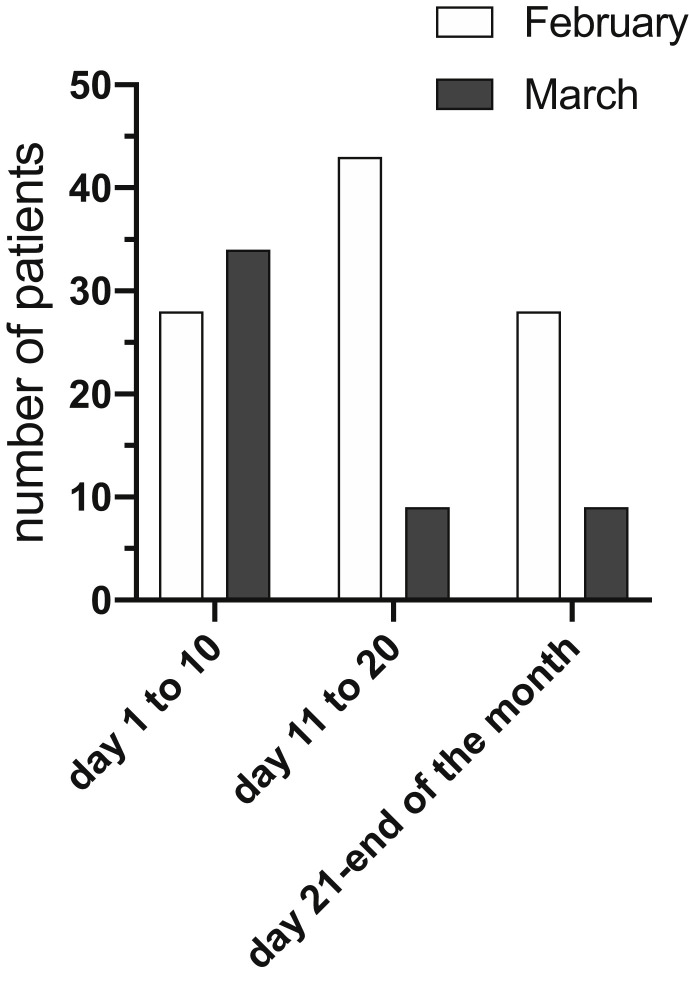
As shown in Fig. 1 , there was a trend of increasing numbers of patients who visited the service between 2017 and 2020, until February 2020. Subsequently, a drop of the number of patients who visited in March was registered (Fig. 1) and, more specifically, a reduction in the number of psychiatric interviews after the 10th of March 2020, which corresponds with the period in which the lockdown was established in Italy (Fig. 2 ).
Fig. 1.
The total number of patients who visited in February compared with those who visited in March (2017–2020).
Fig. 2.
The number of patient visits in February and March 2020 (10-day periods compared).
In addition, whereas in the period 2017–2019, at least 30% of the patients who visited in February attended a follow-up visit in March of the same year; only 17.53% of patients accessing the mental health outpatient service in February 2020 came back for the scheduled follow-up appointment in March 2020 (Fig. 3 ), showing a significant decrease of 46.57% (95% CI: 19.80 to 71.03; P < 0.001).
Fig. 3.
Percentage of patients who visited in February with at least one follow-up visit in March in the years 2017–2020.
Discussion
As a result of the COVID-19 pandemic and consequent lockdown, migrants and, more generally, individuals in poor socio-economic conditions can experience a greater negative impact than the general population.
The first key factor is the psychopathological reaction to the situation (i.e. the COVID-19 pandemic). Indeed, in these subgroups of the population, difficult living conditions, together with previous experience of severe traumas and mental distress, are expected to increase levels of anxiety and consequently negatively impact mental health.10 , 12 , 24 To the authors’ knowledge, this feared effect on the mental health of migrants, refugees and homeless people has not yet been quantified, so further research on this issue is needed.
The second key factor is the difficulty in access to treatment if mental conditions are deteriorating, as expected. Theoretically, lockdown measures should not hamper the ability of receiving medical care,2 and the Italian National Mental Health Service has modified its organisation and procedures to enable treatment of emergent needs.25 However, factors such as insufficient information,10 total quarantine in reception centres that report COVID-19 cases among their asylum seekers and other barriers to the access to mental health services26 can limit the possibility of receiving adequate psychiatric help. To the authors’ knowledge, this study is the first evaluation of the effect of the COVID-19 lockdown measures on the accessibility and follow-up use of public mental health services for immigrants and individuals with poor socio-economic conditions. It should be noted that, in some outpatient services, after the start of lockdown measures, appointments for psychiatric interviews were not available or were restricted only to emergencies. However, even during this period, the psychiatric service in the present study continued regular interviews on a free-access model; accordingly, the effects registered here are not due to changes in the organisation of the outpatient service but due to possible external factors (e.g. information about available facilities, movement restrictions).
This study shows a relevant reduction in the total number of patients who visited the mental health outpatient service after the lockdown, with the risk that new mental health needs are neglected in a period when they are expected to increase. Moreover, a significant reduction in the number of follow-up visits has also been demonstrated, which has potential negative effects on therapeutic compliance and increases the risk of relapse.
This study is limited by that fact that it is a retrospective single-centre study, so the findings cannot be directly generalised to other services. However, it has been reported that mental health services such as the one in this study, specifically oriented to migrants and individuals in poor socio-economic conditions, usually perform better than general mental health services in terms of both accessibility and patient satisfaction.20 , 21 Consequently, it is highly probable that the situation described in this study can be an indication of a more general issue for the entire National Health Service.
Owing to the relevance of these problems of accessibility and continuity of treatment for the mental health of the most vulnerable individuals in the population, proactive strategies should be implemented to monitor emergent needs and provide territorial assistance, with online assistance where feasible.27 , 28
Author statements
Ethical approval
This study has been performed in accordance with the Helsinki declaration. The research design and ethical considerations were reviewed and approved by the Italian National Institute for Health, Migration and Poverty Review Board.
Funding
None declared.
Competing interests
None declared.
References
- 1.Italian Ministry of Health . 2020. Coronavirus: La situazione in Italia [coronavirus, the situation in Italy]http://www.salute.gov.it/portale/nuovocoronavirus/dettaglioContenutiNuovoCoronavirus.jsp?area=nuovoCoronavirus&id=5351&lingua=italiano&menu=vuoto [Google Scholar]
- 2.Conte G. Ulteriori disposizioni attuative del decreto-legge 23 febbraio 2020, n. 6, recante misure urgenti in materia di contenimento e gestione dell’emergenza epidemiologica da COVID-19. [Further dispositions to put in act the law-decree 23 February 2020, n.6, with urgent measures to circumscribe and manage the COVID-19 epidemiological emergency]. Gazzetta Ufficiale della Repubblica Italiana 2020;59:1-6.
- 3.Jakovljevic M., Bjedov S., Jaksic N., Jakovljevic I. Covid-19 pandemia and public and global mental health from the perspective of global health security. Psychiatr Danub. 2020;32:6–14. doi: 10.24869/psyd.2020.6. [DOI] [PubMed] [Google Scholar]
- 4.Sani G., Janiri D., Di Nicola M., Janiri L., Ferretti S., Chieffo D. Mental health during and after the COVID-19 emergency in Italy. Psychiatr Clin Neurosci. 2020 doi: 10.1111/pcn.13004. Apr 4. [DOI] [PubMed] [Google Scholar]
- 5.Tian F., Li H., Tian S., Yang J., Shao J., Tian C. Psychological symptoms of ordinary Chinese citizens based on SCL-90 during the level I emergency response to COVID-19. Psychiatr Res. 2020;288:112992. doi: 10.1016/j.psychres.2020.112992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang J., Lu H., Zeng H., Zhang S., Du Q., Jiang T., Du B. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain Behav Immun. 2020 doi: 10.1016/j.bbi.2020.04.031. Apr 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chung R.Y., Dong D., Li M.M. Socioeconomic gradient in health and the covid-19 outbreak. BMJ. 2020;369 doi: 10.1136/bmj.m1329. m1329. [DOI] [PubMed] [Google Scholar]
- 8.Wang Z., Tang K. Combating COVID-19: health equity matters. Nat Med. 2020;26:458. doi: 10.1038/s41591-020-0823-6. [DOI] [PubMed] [Google Scholar]
- 9.Lima N.N.R., de Souza R.I., Feitosa P.W.G., Moreira J.L.S., da Silva C.G.L., Neto M.L.R. People experiencing homelessness: their potential exposure to COVID-19. Psychiatr Res. 2020;288:112945. doi: 10.1016/j.psychres.2020.112945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liem A., Wang C., Wariyanti Y., Latkin C.A., Hall B.J. The neglected health of international migrant workers in the COVID-19 epidemic. Lancet Psychiatr. 2020;7:e20. doi: 10.1016/S2215-0366(20)30076-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Page K.R., Venkataramani M., Beyrer C., Polk S. Undocumented U.S. Immigrants and covid-19. N Engl J Med. 2020 doi: 10.1056/NEJMp2005953. Mar 27. [DOI] [PubMed] [Google Scholar]
- 12.Kluge H.H.P., Jakab Z., Bartovic J., D'Anna V., Severoni S. Refugee and migrant health in the COVID-19 response. Lancet. 2020;395:1237–1239. doi: 10.1016/S0140-6736(20)30791-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.UNHCR COVID-19 will not leave behind refugees and migrants. Lancet. 2020;395:1090. doi: 10.1016/S0140-6736(20)30758-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chevance A., Gourion D., Hoertel N., Llorca P.M., Thomas P., Bocher R. Assurer les soins aux patients souffrant de troubles psychiques en France pendant l’épidémie à SARS-CoV-2. [Ensuring mental health care during the SARS-CoV-2 epidemic in France: a narrative review] Encephale. 2020 doi: 10.1016/j.encep.2020.03.001. pii:S0013-7006(20)30064-30066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yao H., Chen J.H., Xu Y.F. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatr. 2020;7:e21. doi: 10.1016/S2215-0366(20)30090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bhopal R.S. COVID-19: immense necessity and challenges in meeting the needs of minorities, especially asylum seekers and undocumented migrants. Publ Health. 2020;182:161–162. doi: 10.1016/j.puhe.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Law n.132 Conversione in legge, con modificazioni, del decreto legge 4 ottobre 2018, n. 113, recante disposizioni urgenti in materia di protezione internazionale e immigrazione, sicurezza pubblica, (omissis). [Conversion in law, with changes, of the law decree 4 October 2018, n.113, with urgent measures regarding international protection and migration, public security (omissis)] Gazzetta Ufficiale della Repubblica Italiana. 2018;281:1–17. [Google Scholar]
- 18.Aragona M., Pucci D., Mazzetti M., Geraci S. Post-migration living difficulties as a significant risk factor for PTSD in immigrants: a primary care study. Ital J Publ Health. 2012;9 doi: 10.2427/7525. 67-4. [DOI] [Google Scholar]
- 19.Jongsma H.E., Gayer-Anderson C., Lasalvia A., Quattrone D., Mulè A., Szöke A. Treated incidence of psychotic disorders in the multinational EU-GEI study. JAMA Psychiatr. 2018;75:36–46. doi: 10.1001/jamapsychiatry.2017.3554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Griffiths G., Tarricone I., Study Group The provision of mental health services to immigrants and refugees in Italy: the barriers and facilitating factors experienced by mental health workers. J Psychopathol. 2017;23:79–86. [Google Scholar]
- 21.Petta A.M. Crossing Dialogues; Rome: 2019. Indagine sui bisogni sanitari e di salute mentale dei rifugiati e richiedenti asilo ospiti dei centri di accoglienza nel territorio di Roma. [Inquiry about the sanitary and mental health needs of refugees and asylum seekers hosted in the reception centers of the territory of Rome] [Google Scholar]
- 22.Júnior J.G., de Sales J.P., Moreira M.M., Pinheiro W.R., Lima C.K.T., Neto M.L.R. A crisis within the crisis: the mental health situation of refugees in the world during the 2019 coronavirus (2019-nCoV) outbreak. Psychiatr Res. 2020;288:113000. doi: 10.1016/j.psychres.2020.113000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatr Res. 2020;288:112954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kar S.K., Arafat S.M.Y., Marthoenis M., Kabir R. Homeless mentally ill people and COVID-19 pandemic: the two-way sword for LMICs. Asian J Psychiatr. 2020;51:102067. doi: 10.1016/j.ajp.2020.102067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Percudani M., Corradin M., Moreno M., Indelicato A., Vita A. Mental health services in lombardy during COVID-19 outbreak. Psychiatr Res. 2020;288:112980. doi: 10.1016/j.psychres.2020.112980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bartolomei J., Baeriswyl-Cottin R., Framorando D., Kasina F., Premand N., Eytan A. What are the barriers to access to mental healthcare and the primary needs of asylum seekers? A survey of mental health caregivers and primary care workers. BMC Psychiatr. 2016;16:336. doi: 10.1186/s12888-016-1048-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kannarkat J.T., Smith N.N., McLeod-Bryant S.A. Mobilization of telepsychiatry in response to COVID-19-moving toward 21st century access to care. Adm Policy Ment Health. 2020 doi: 10.1007/s10488-020-01044-z. Apr 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu S., Yang L., Zhang C., Xiang Y.T., Liu Z., Hu S. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatr. 2020;7:e17–e18. doi: 10.1016/S2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]