Supplemental Digital Content is available in the text
Keywords: Japan, overtime working, psychological distress, Stress Check Program, Work Style Reform
Abstract
Objective:
The study aims to examine the association between overtime-working environment (OWE) and individual psychological distress among Japanese workers.
Methods:
Data of 7786 workers from 101 companies in Japan were analyzed. Psychological distress was assessed through a 29-item questionnaire. The OWE was evaluated by calculating the proportion of workers whose monthly overtime was 45 hours or more in a workplace. Multilevel logistic regression was used.
Results:
As 10% increase in the OWE was associated with a 16% higher risk of individual psychological distress after adjustment of individual covariates, including overtime working hours. Cross-level interaction showed that the risk was varied depending on individual overtime working hours.
Conclusions:
OWE was associated with the psychological distress of workers. It is necessary to create a non-OWE at workplaces to prevent psychological distress for workers.
The impact of long working hours on employees’ health is a classic but crucial global health issue. Japanese are known for working long hours but low productivity, and to address the situation, the Japanese government enacted the Work Style Reform Law in 2019. At the same time, the Japanese government recommend the health and productivity management as a policy to promote contextual workers wellbeing and organizational profit synergistically through intervention to psycho-social work environment.1
Essentially, the objective of the management of working hours is not for the promotion of health, like stress reduction, but for compliance and productivity. On the other hand, it has been hypothesized that long working hours affect workers’ health status, both psychologically and physiologically, owing to a variety of occupational factors, particularly job stress. Previous studies have associated long working hours to adverse health outcomes such as heart disease, stroke, diabetes, alcohol consumption, and depression.2–9 One of the possible pathways between long working hours and adverse health outcomes could be short sleeping hours.10–13 The effects of long working hours on psychological distress might be mediated by short sleeping hours as the Korean study, however, there was no consistent association between working hours and psychological distress as the Japanese systemic review.14,15 One study showed no change in psychological distress in relation to overtime work periods, the other suggested that high job control impacted on the reduction of psychological distress in relation to overtime work hours in Japanese employees.16,17 Several factors besides sleeping hours may have contributed to the mixed findings on the relationship between long working hours and psychological distress. That is, the job stress as psycho-social poor health could be confounded by workplace environment.18,19 The overtime-working environment might induce not only longer working hours but also psychological distress of employees directly as a contextual effect regardless of their working hours.
Japanese are so sensitive to feeling shame and guilt that the common reason for working overtime is the difficulty of leaving the workplace alone while the rest, especially their supervisors, are still working.20 The overtime environment may also affect workers who do not or work fewer hours in overtime through this feeling of guilt and shame. Emotions, such as guilt and shame, are central to the development of posttraumatic stress disorder (PTSD), and the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) recognized the pathological role of negative emotions, such as guilt and shame.21 In the literature, however, there are no studies that have investigated the contextual effect of overtime-working environment on individual psychological distress.
The hypothesis of the contextual effect might suggest that the appropriate time management could simultaneously lead to the contextual positive health outcomes of workers. In addition, if social supportive environment, where workers could easily access to appropriate support from supervisors as needed, could remedy the contextual impact of psychological distress, then the development of leadership could also promote workers’ health.22 This is the way of the health and productivity management that is recommended by the government of Japan.
In 2015, the Japanese government launched the Stress Check Program based on the amended Industrial Safety and Health Act for companies with 50 or more employees.23 The mandatory program mainly aims to facilitate each employee's mental health by nurturing one's own recognition of psychological stress levels at the workplace.24 Furthermore, the improvement of the occupational environment in accordance with the results of group analysis to promote the psychosocial health of the entire organization is expected as obligation to make effort. The government recommended the use of the Brief Job Stress Questionnaire (BJSQ) in the Stress Check Program to assess workers’ job stressors, stress reactions, and social support as buffering factors.25,26 The simultaneous assessment of BJSQ and overtime working hours would help investigate both the contextual effect of the overtime-working environment on psychological distress using multilevel modeling adjusted for individual-level working hours and the contextual effect of social supportive environment on individual psychological distress using multilevel modeling adjusted for individual-level social support. This study was specifically conducted for such a purpose.
METHODS
Study Sample
The data from the Stress Check Program belonged to 14,348 workers from 101 companies between April 2016 and June 2017. The companies were clients of one vendor that addressed the program's compliance with the Stress Check Program. Companies that comprised less than 50 workers were excluded because the Industry Safety and Health Act required the respective program to target companies with 50 or more employees. Hence, all excluded departments composed of less than 50 workers (N = 5980), and had missing values on the BJSQ (N = 582), yielding an analytic sample size of 7786 (Fig. 1). Data were provided to the researchers anonymously. This study was approved by the Teikyo University Review Board.
FIGURE 1.
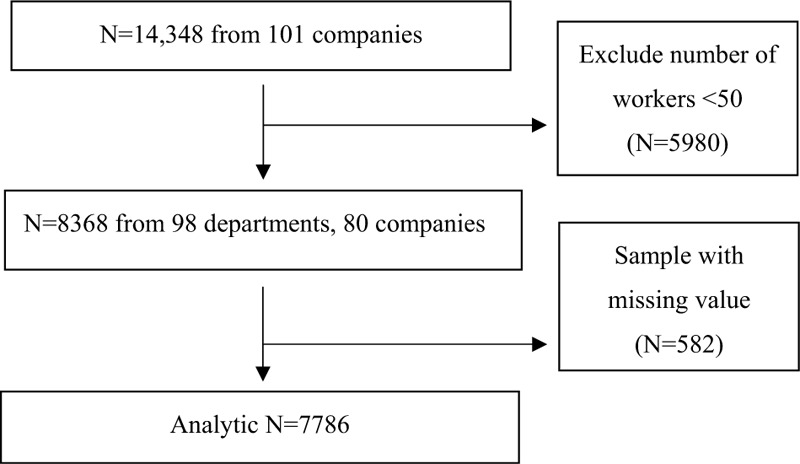
Sampling flow.
Measurements
Psychological Distress
The BJSQ includes three subscales of stressor, stress reaction, and social support. Psychological distress was assessed using the questionnaire for stress reactions that is a part of BJSQ and composed of 29 items rated on a four-point Likert scale (range 29 to 116). The 29 items include mental reactions like emotions (eg, irritability, anger) or attitudes (eg, concentration, exhaustion) and physical symptoms like diarrhea and sleep disorder. The four-point Likert scale consists of “Almost never,” “Sometimes,” “Often,” and “Almost always.” Psychological distress was defined as having the highest level of stress reaction (ie, stress reaction score 77 or higher) based on the governmental guideline for the Stress Check Program.27
Overtime-Working Environment
The overtime working hours are extra working hours on top of scheduled working hours in the labor contract of each worker. The overtime working hours in the preceding month and average monthly overtime hours were self-reported using the following categorized response items: “0 to less than 20 hours,” “20 to less than 45 hours,” “45 to less than 80 hours,” “80 to less than 100 hours,” and “100+ hours.” As for the overtime-working environment, we calculated the proportion of workers who accumulated overtime work of 45 hours or more in the preceding month under the principles of the amended Labor Standards Act.
Covariates
Following previous studies, gender, age, marital status (“married” or “unmarried”), working years (by category), job position (“managers,” “general,” or “other”), employment status (“regular,” “part-time,” “dispatched,” or “other”), and overtime working hours were included as for the individual level covariates.24,28 Thus, being male, young, unmarried, and having high seniority, a higher job position, and regular employment status can be associated with both working hours and psychological distress. As for the covariates of the workplace, the proportion of regular workers and mean social support from supervisors and colleagues were calculated.
Statistical Analysis
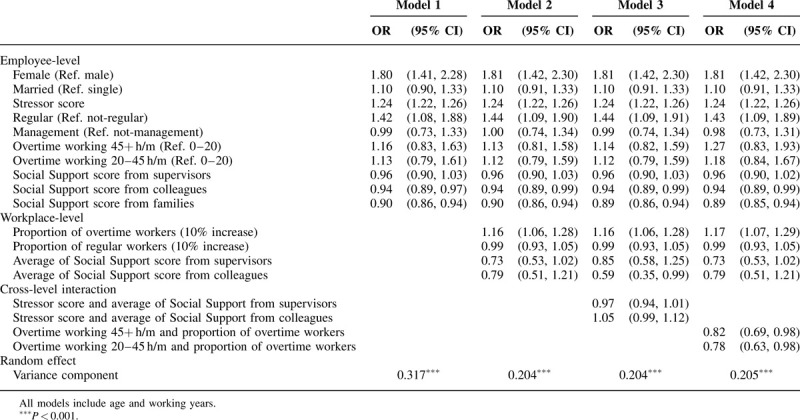
This study used four models of multilevel analysis for 7786 individuals nested with 98 workplaces (departments or companies). First, in Model 1, we estimated the odds ratio of individual-level variables, that is, the preceding month's overtime working hours, in addition to sex, age, marital status, working years, employment status, job position, scores from BJSQ including Stressor score, and Social Support score from supervisors, colleagues, and families for high-stress workers. Next, in Model 2, we included the contextual effects of workplace variables, including the proportion of preceding month's overworked employees, the proportion of regular workers, the average Social Support Score of supervisors, and the average Social Support Score of colleagues, adjusted for individual-level covariates. As Model 3 and 4, cross-level interaction was checked to confirm effect modifiers between: (a) Stressor score and the average Social Support of supervisors or colleagues (Model 3) and (b) the preceding month's overtimeworking hours and the proportion of that month's overtime workers (Model 4). The result that 0.82 (0.69, 0.98) and 0.78 (0.63, 0.98) have to move the next row of Model 4 in Table 3. HLM7 (Scientific Software International, Inc., Skokie, IL) was used for the analysis. As a sensitivity analysis, multiple imputations for missing data were employed to minimize the potential bias associated with item nonresponse. In particular, 10 complete datasets were imputed by IBM SPSS 23 (IBM Corp., Armonk, NY).
TABLE 3.
Results of Multilevel Logistic Regression: Odds Ratio (OR) of Having High Job Stress
RESULTS
Table 1 shows the sample characteristics. The proportion of males and females was almost equal (53.4% and 46.6%), and the mean age was 41.8 (standard deviation [SD] = 12.1) years. More than 80% were non-management positions, 62% were married, and 82% were regular workers. The proportion of those who worked overtime over 45 hours preceding month was 7.1%. Workers who marked psychological distress made up 11.2%.
TABLE 1.
Characteristics of Study Subjects
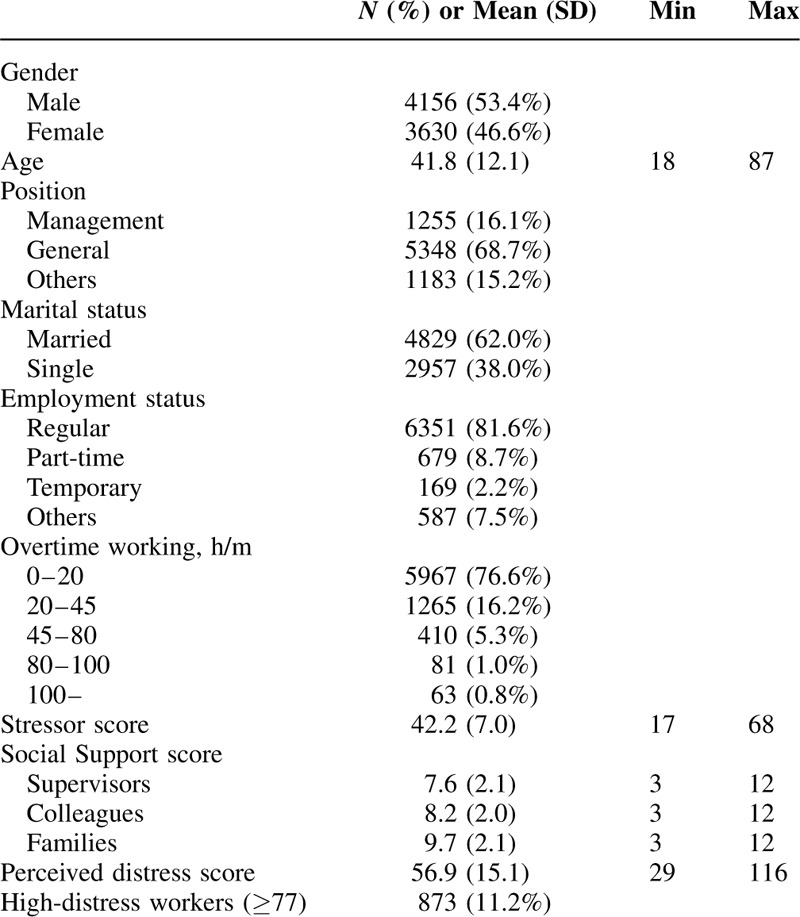
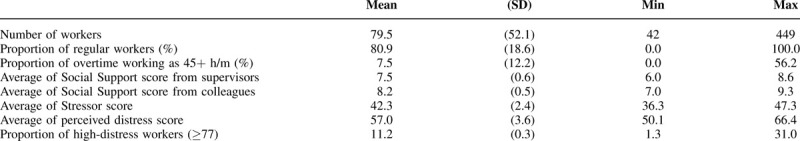
Table 2 shows the characteristics of the workplace (N = 98). The mean number of workers was 79.5, ranging from 42 to 449. As for the proportion of regular workers, the average was 80%. The mean proportion of overtime workers as for the overtime-environment among workplaces was 7.5% (SD = 12.2%), ranging from 0% to 56.2%.
TABLE 2.
Characteristics of Workplaces (N = 98)
Odds ratios (ORs) of the psychologically distressed workers, according to individual and workplace factors, are shown in Table 3. In Model 2, a 10% increase in the proportion of workers whose preceding monthly overtime was 45 hours or more showed a significant independent risk factor for psychologically distressed workers (OR: 1.16, 95% confidence interval: 1.06 to 1.28), even after adjusting for individual-level factors, including the average monthly overtime working hours, working status, Stressor score, and Social Support scores.
In Model 3, the interaction of Stressor score with the average Social Support of supervisors and colleagues was not statistically significant. However, in Model 4, we found a significant interaction between the preceding month's overtime working hours (ie, 20 to 45 and 45+ hours per month) and the proportion of that month's overtime workers. For a sensitivity analysis, multiple imputations for missing data were performed which confirmed similar results (OR: 1.15, 95% confidence interval: 1.05 to 1.26) (Supplemental Table 1, Supplemental Digital Content). To clarify this significant cross-level interaction, we conducted the stratified analysis by the preceding month's overtime working hours (ie, 0 to 20, 20 to 45, and 45+ hours per month) (Supplemental Table 2, Supplemental Digital Content). Even though it was not statistically significant, the directions of the association between the proportion of overtime workers and psychological distress varied depending on overtime working hours: ORs were 1.10, 0.98, and 0.92 for 0 to 20, 20 to 45, and 45+ hours per month, respectively. Figure 2 graphically shows the interaction between the preceding month's overtime working hours and the proportion of that month's overtime workers.
FIGURE 2.
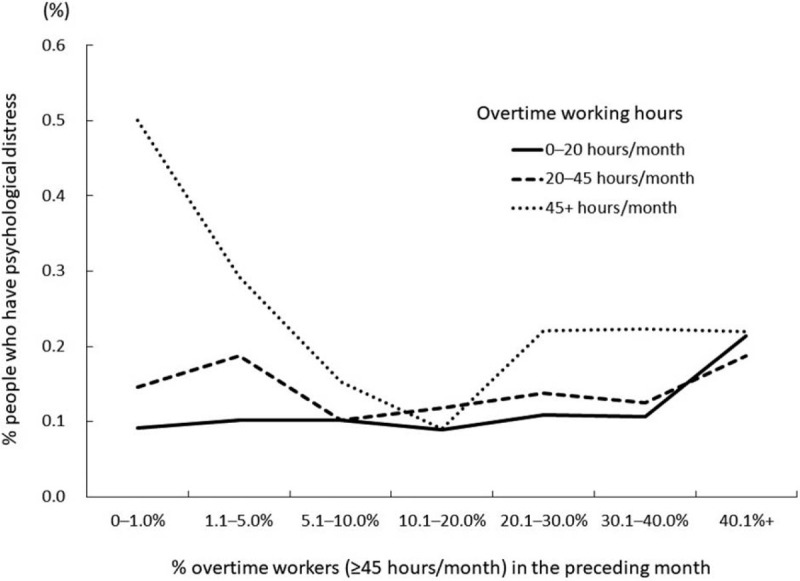
The interaction effect of overtime working hours per month on the association between percentage of overtime workers in the preceding month and percentage of people who have psychological distress.
DISCUSSION
As hypothesized, we found the contextual effect of overtime-working environment on psychological distress among workers, more specifically, the nature of the contextual effect depending on the overtime working hours: for example, the most harmful contextual effect of long-working environment among the less overworked workers, and the rather positive contextual effect among the most overworked workers. To the best of our knowledge, this is the first study to find the contextual effect of overtime-working environment on individual psychological distress.
The current study added new evidence to the debate on the association between overtime working and psychological distress. Previous studies reported inconclusive evidence; for example, one study showed the significant association of overtime working hours with doctor-diagnosed depression among females only.29 It was also reported that a decrease in overtime working hours showed a protective effect on depressive symptoms, while other studies showed no significant association between long working hours and depression.9,30–34 In the current study, although we did not find a significant association between overtime working hours and psychological distress, we did find a contextual effect of the proportion of overtime workers on psychological distress, suggesting that inconsistent findings might be due to unmeasured contextual effect of overtime working. Hence, a positive association between overtime working and depressive symptoms in previous studies might be confounded by the overtime-working environment.
The mechanisms regulating the overtime-working environment and its contextual effect on psychological distress at the individual level remains unknown. However, based on cross-level interaction, it can be speculated that workers who accumulated less than 20 hours of overtime per month may feel shame and guilt in an overtime-working environment. Japanese are too accustomed to overtime working and tend to feel more shame and guilt if they complete their task within the scheduled working hours. That is, workers leaving at the official end-of-work time, while their colleagues were still working, may experience feelings of shame and guilt because they would feel that their colleagues would judge them as lazy, although it may be not true. Most Japanese agree that people who work till late at workspaces are diligent. Notably, the emotions of shame and guilt are often involved in psychopathological risks, including suicide.35
In addition, previous studies showed the association between organizational justice or psychological safety climate and psychological health.36–39 The less overtime workers might lose their trust and psychosocial health because they saw that their managers could neither effectively manage the human resources nor schedule and that their companies tolerated disparities without organizational justice nor psychosocial safety climate. The low level of organizational justice included the risk of workers’ psychological health even after adjustment for workload.40 Thus, the organizational justice and psychosocial safety climate may explain the current positive contextual effect among the most overworked workers. In other words, the disparities in the work environment can more negatively affect the psychological health of each worker than one's overtime working hours. Needless to say, excessive overtime is not recommended; however, Fig. 2 suggests that it is better to share tasks than to assign them to some specific workers. Moreover, the buffering by social support from supervisors was most effective and significant in the medium overtime-working environment. For both organizational compliance and all workers’ psychological health, the proper management to create a trusting environment without disparities is required even if it increases the average overtime. We recommend companies to control the impartial time management as the improvement of the occupational environment after the Stress Check Program.
Several limitations of this study need to be addressed before concluding the findings. First, the current sample is not randomly selected from companies in Japan, and the proportion of regular workers at 81.2% was relatively higher than 62.1%, the proportion in Japan.41 Hence, the collected sample might be biased in the aspect of higher socioeconomic status. Further, small companies with less than 50 workers were excluded, and thus the current findings could not be applied to small companies. Second, because the current study was cross-sectional in nature, causality remains unknown because workers with psychological distress may perform poorly, leading them to work longer hours or requesting other workers to cover their work, which can induce a higher proportion of overtime workers. A further longitudinal study is needed to confirm the contextual effect of the overtime-working environment on psychological distress. Third, we used psychological distress from stress reactions of BJSQ; however, psychological distress screened by BJSQ may not capture potential psychological distress measured by K6.42 Nevertheless, a previous study confirmed the predictability of long-term sickness absence.43 A further study assessing the contextual effect of overtime-working environment on absenteeism, presenteeism, turnover, or accidents among workers is warranted. In addition, we dichotomized the BJSQ score, which may reduce the statistical power due to information loss.44 However, since dichotomization by the 77 cut-off was based on the governmental guideline, our results could be practically implemented.
Nonetheless, we found the harmful effect of overtime-working environment on psychological distress even among workers who did less overtime work, suggesting that more efficient working reforms are needed to protect the health of workers. That is, in addition to limiting the average overtime working hours at the individual level, the proportion of overtime workers needs to be controlled, and eventually, a psychosocial safety climate needs to be created to protect the mental health and safety of all workers.45 Notably, it is insufficient for an individual to be cautious of overtime working hours if other workers in the same workplace do not care about lengthy overtime working hours.
In conclusion, an overtime-working environment had a contextual effect on psychological distress for all workers. It is necessary for companies to create a non-overtime-working environment without disparity at workplaces to prevent psychological distress for workers.
Supplementary Material
Acknowledgments
The authors would like to thank Digit Inc. (www.digit.co.jp) for supplying data.
Footnotes
Funding Sources: None declared.
Conflict of Interest: None declared.
Acknowledgments, including all sources of support: None declared.
Ethical Considerations & Disclosure: None declared.
Clinical significance: By analyzing mandatory program for companies in Japan to promote workers’ psychological health, we found the contextual effect of overtime-working environment on individual psychological distress and the trend of the contextual effect. A working environment without overtime disparity is required not only for compliance but as workplace psychological health promotion.
REFERENCES
- 1. Healthcare Industries Division, Ministry of Economy, Trade and Industry. Enhancing Health and Productivity Management; 2020. Available at: https://www.meti.go.jp/policy/mono_info_service/healthcare/downloadfiles/180717health-and-productivity-management.pdf. Accessed March 13, 2020. [Google Scholar]
- 2.Bannai A, Tamakoshi A. The association between long working hours and health: a systematic review of epidemiological evidence. Scand J Work Environ Health 2014; 40:5–18. [DOI] [PubMed] [Google Scholar]
- 3.Kivimaki M, Nyberg ST, Batty GD, et al. Long working hours as a risk factor for atrial fibrillation: a multi-cohort study. Eur Heart J 2017; 38:2621–2628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Virtanen M, Kivimaki M. Long working hours and risk of cardiovascular disease. Curr Cardiol Rep 2018; 20:123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kivimaki M, Jokela M, Nyberg ST, et al. Long working hours and risk of coronary heart disease and stroke: a systematic review and meta-analysis of published and unpublished data for 603,838 individuals. Lancet 2015; 386:1739–1746. [DOI] [PubMed] [Google Scholar]
- 6.Kivimaki M, Virtanen M, Kawachi I, et al. Long working hours, socioeconomic status, and the risk of incident type 2 diabetes: a meta-analysis of published and unpublished data from 222 120 individuals. Lancet Diabetes Endocrinol 2015; 3:27–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Virtanen M, Jokela M, Nyberg ST, et al. Long working hours and alcohol use: systematic review and meta-analysis of published studies and unpublished individual participant data. BMJ 2015; 350:g7772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Watanabe K, Imamura K, Kawakami N. Working hours and the onset of depressive disorder: a systematic review and meta-analysis. Occup Environ Med 2016; 73:877–884. [DOI] [PubMed] [Google Scholar]
- 9.Virtanen M, Jokela M, Madsen IE, et al. Long working hours and depressive symptoms: systematic review and meta-analysis of published studies and unpublished individual participant data. Scand J Work Environ Health 2018; 44:239–250. [DOI] [PubMed] [Google Scholar]
- 10.Nakata A. Work hours, sleep sufficiency, and prevalence of depression among full-time employees: a community-based cross-sectional study. J Clin Psychiatry 2011; 72:605–614. [DOI] [PubMed] [Google Scholar]
- 11.Liu Y, Tanaka H. Fukuoka, Heart Study Group Overtime work, insufficient sleep, and risk of non-fatal acute myocardial infarction in Japanese men. Occup Environ Med 2002; 59:447–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Virtanen M, Ferrie JE, Gimeno D, et al. Long working hours and sleep disturbances: the Whitehall II prospective cohort study. Sleep 2009; 32:737–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nakashima M, Morikawa Y, Sakurai M, et al. Association between long working hours and sleep problems in white-collar workers. J Sleep Res 2011; 20 (1 pt 1):110–116. [DOI] [PubMed] [Google Scholar]
- 14.Kim TK, Lee HC, Lee SG, et al. The combined effect of sleep duration and quality on mental health among Republic of Korea Armed Forces. Mil Med 2016; 181:e1581–e1589. [DOI] [PubMed] [Google Scholar]
- 15.Fujino Y, Horie S, Hoshuyama T, et al. A systematic review of working hours and mental health burden. Sangyo Eiseigaku Zasshi 2006; 48:87–97. [DOI] [PubMed] [Google Scholar]
- 16.Steptoe A, Wardle J, Lipsey Z, et al. A longitudinal study of work load and variations in psychological well-being, cortisol, smoking, and alcohol consumption. Ann Behav Med 1998; 20:84–91. [DOI] [PubMed] [Google Scholar]
- 17.Hino A, Inoue A, Kawakami N, et al. Buffering effects of job resources on the association of overtime work hours with psychological distress in Japanese white-collar workers. Int Arch Occup Environ Health 2015; 88:631–640. [DOI] [PubMed] [Google Scholar]
- 18.Virtanen M, Stansfeld SA, Fuhrer R, et al. Overtime work as a predictor of major depressive episode: a 5-year follow-up of the Whitehall II study. PLoS One 2012; 7:e30719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pattussi MP, Olinto MT, Canuto R, et al. Workplace social capital, mental health and health behaviors among Brazilian female workers. Soc Psychiatry Psychiatr Epidemiol 2016; 51:1321–1330. [DOI] [PubMed] [Google Scholar]
- 20. Ministry of Health, Labour and Welfare, Japan. A labor and social research for understanding the actual situation of Karoshi; 2017. Available at: https://www.mhlw.go.jp/file/06-Seisakujouhou-11200000-Roudoukijunkyoku/0000174210.pdf. Accessed November 3, 2019. [Google Scholar]
- 21. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®), 5th ed.; 2013. [Google Scholar]
- 22.Tsuboya T, Tsutsumi A, Kawachi I. Change in psychological distress following change in workplace social capital: results from the panel surveys of the J-HOPE study. Occup Environ Med 2015; 72:188–194. [DOI] [PubMed] [Google Scholar]
- 23. Ministry of Health, Labour and Welfare, Japan. The Stress Check Program; 2015. Available at: http://www.mhlw.go.jp/bunya/roudoukijun/anzeneisei12/. Accessed November 3, 2019. [Google Scholar]
- 24.Kawakami N, Tsutsumi A. The Stress Check Program: a new national policy for monitoring and screening psychosocial stress in the workplace in Japan. J Occup Health 2016; 58:1–6. [DOI] [PubMed] [Google Scholar]
- 25.Shimomitsu T, Nakamura K, Kawakami N, et al. The Final Development of the Brief Job Stress Questionnaire Mainly Used for Assessment of the Individuals. 1999 Report. 2000; Tokyo:Tokyo Medical University, 126–164. [Google Scholar]
- 26. The National Institute for Occupational Safety and Health (NIOSH). Stress…At Work. Available at: https://www.cdc.gov/niosh/docs/99-101/default.html and https://www.cdc.gov/niosh/docs/99-101/pdfs/99-101.pdf?id=10.26616/NIOSHPUB99101. Accessed March 13, 2020. [Google Scholar]
- 27. Ministry of Health, Labour and Welfare, Japan, Guideline for implementing a stress check program based on the Industrial Safety and Health Act. [Available at: https://www.mhlw.go.jp/bunya/roudoukijun/anzeneisei12/pdf/150507-1.pdf. Accessed March 13, 2020]. [Google Scholar]
- 28. Ministry of Health, Labour and Welfare, Japan. A Health and Labor Sciences Research Grant; 2016. Available at: https://mental.m.u-tokyo.ac.jp/jstress/H27_29%E3%82%B9%E3%83%88%E3%83%AC%E3%82%B9%E3%83%81%E3%82%A7%E3%83%83%E3%82%AF%E7%8F%AD%E7%B7%8F%E5%90%88%E5%A0%B1%E5%91%8A%E6%9B%B8.pdf. Accessed November 3, 2019. [Google Scholar]
- 29.Shields M. Long working hours and health. Health Rep 1999; 11:33–48. [PubMed] [Google Scholar]
- 30.Hino A, Inoue A, Mafune K, et al. The effect of changes in overtime work hours on depressive symptoms among Japanese white-collar workers: a 2-year follow-up study. J Occup Health 2019; 61:320–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kawakami N, Araki S, Kawashima M. Effects of job stress on occurrence of major depression in Japanese industry: a case-control study nested in a cohort study. J Occup Med 1990; 32:722–725. [PubMed] [Google Scholar]
- 32.Ogasawara K, Nakamura Y, Aleksic B, et al. Depression associated with alcohol intake and younger age in Japanese office workers: a case-control and a cohort study. J Affect Disord 2011; 128:33–40. [DOI] [PubMed] [Google Scholar]
- 33.Wang J, Patten SB, Currie S, et al. A population-based longitudinal study on work environmental factors and the risk of major depressive disorder. Am J Epidemiol 2012; 176:52–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Niedhammer I, Malard L, Chastang JF. Occupational factors and subsequent major depressive and generalized anxiety disorders in the prospective French national SIP study. BMC Public Health 2015; 15:200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Crowder MK, Kemmelmeier M. Cultural. Differences in Shame and Guilt as Understandable Reasons for Suicide. Psychol Rep 2018; 121:396–429. [DOI] [PubMed] [Google Scholar]
- 36.Hayashi T, Shimomitsu T, Ohya Y, et al. Organizational justice, willingness to work, and psychological distress: results from a Private Japanese Company. JOEM 2011; 53:174–181. [DOI] [PubMed] [Google Scholar]
- 37.Kivimäki M, Elovainio M, Vahtera J, et al. Organisational justice and health of employees: prospective cohort study. Occup Environ Med 2003; 60:27–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hayashi T, Odagiri Y, Ohya Y, et al. Organizational justice, willingness to work, and psychological distress: results from a Private Japanese Company. JOEM 2011; 53:174–181. [DOI] [PubMed] [Google Scholar]
- 39.Dollard MF, Bakker AB. Psychosocial safety climate as a precursor to conducive work environments, psychological health problems, and employee engagement. J Occup Organ Psych 2010; 83:579–599. [Google Scholar]
- 40.Elovainio M, Kivimäki M, Vahtera J. Organizational justice: evidence of a new psychosocial predictor of health. Am J Public Health 2002; 92:105–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Ministry of Internal Affairs and Communications, Japan. Labor force survey 2018; 2019. Available at: https://www.stat.go.jp/data/roudou/sokuhou/nendo/pdf/2018nd.pdf. Accessed November 3, 2019. [Google Scholar]
- 42.Tsutsumi A, Inoue A, Eguchi H. How accurately does the Brief Job Stress Questionnaire identify workers with or without potential psychological distress? J Occup Health 2017; 59:356–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tsutsumi A, Shimazu A, Eguchi H, et al. A Japanese Stress Check Program screening tool predicts employee long-term sickness absence: a prospective study. J Occup Health 2018; 60:55–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Walraven CV, Hart RG. Leave‘em alone - why continuous variables should be analyzed as such. Neuroepidemiology 2008; 30:138–139. [DOI] [PubMed] [Google Scholar]
- 45.Dollard MF, McTernan W. Psychosocial safety climate: a multilevel theory of work stress in the health and community service sector. Epidemiol Psychiatr Sci 2011; 20:287–293. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


