Abstract
Infections are a major cause of morbidity and mortality in patients with chronic lymphocytic leukemia (CLL). These can be exacerbated by anti-leukemic treatments. In addition, the typical patients with CLL already have fragilities and background risk factors that apply to the general population for severe COVID-19. On these bases, patients with CLL may experience COVID-19 morbidity and mortality. Recurrent seasonal epidemics of SARS-CoV-2 are expected, and doctors taking care of patients with CLL must be prepared for the possibility of substantial resurgences of infection and adapt their approach to CLL management accordingly. In this Guideline Article, we aim at providing clinicians with a literature-informed expert opinion on the management of patients with CLL during SARS-CoV-2 epidemic.
Introduction
Many countries are following SARS-CoV-2 non-pharmaceutical mitigation policies, and, with the current data, it is impossible to determine how long such policies will be needed to establish sufficient herd immunity. Modeling suggests recurrent SARS-CoV-2 epidemic phases flaring up on the background of an endemic disease dictated by relaxation and reinstitution of the package of non-pharmaceutical interventions until an effective pharmacological treatment/prevention against COVID-19 will be available.1,2
The rapidly expanding SARS-CoV-2 pandemic and its threats require a quick reaction prior to the availability of (eagerly awaited) evidence on how to manage patients with chronic lymphocytic leukemia (CLL) during this pandemic. Accordingly, this document was prepared by adapting existing guidance and scientific evidence to the new scenario imposed by the SARS-CoV-2 epidemics.
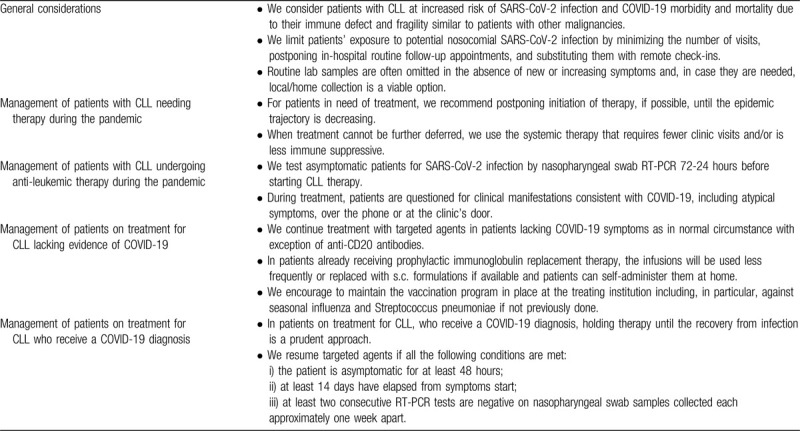
The aim of this document is to provide clinicians with a literature-informed expert opinion (Table 1) developed through a bottom-up information processing and based on incoming data from publications and the clinics in SARS-CoV-2 infection and related infectious conditions including other oncological diseases.
Table 1.
Summary of Recommendations About Management of Patients With CLL During the COVID-19 Pandemic.
Search strategy and selection criteria
A literature review was performed using PubMed to identify relevant English-language articles published through April 30, 2020 [search terms (coronavirus OR COVID OR SARS-CoV OR ∗nCoV∗) AND (immunodeficiency OR leukemia OR cancer)]. Recommendations on the general themes of SARS-CoV-2, COVID-19 and CLL or cancer provided by ASH, ASCO, ASTCT, CDC, EBMT, EHA, ERIC, ESMO, iwCLL, NCCN, NIH, SSC, and WHO were also reviewed (last search on April 30th, 2020).
General considerations
We consider patients with CLL at increased risk of SARS-CoV-2 infection and COVID-19 morbidity and mortality due to their immune defect and fragility similar to patients with other malignancies
Whether the prevalence of COVID-19 in patients with cancer, including CLL, is higher than in sex- and age-matched normal population is uncertain.3–5 However, there is evidence that cancer conveys a poorer outcome in patients with COVID-19 infection.3–10 In addition, the risk of COVID-19 morbidity and mortality is thought to be higher in CLL due to the detrimental effect of comorbidities frequently occurring in patients with this leukemia, though this aspect has not been specifically addressed.
CLL can result in one or more of the following risk factors for infection: hypogammaglobulinemia, qualitative and quantitative B and T cell defects including impaired response to vaccination and CD4+ lymphopenia, innate immune dysfunction, and neutropenia among others.11 These can be exacerbated by anti-leukemic treatments and are known risk factors for viral infections.12,13 Thus, we can speculate that this existing immune suppression might also prevent or delay CLL patient's ability to react against the SARS-CoV-2 virus or to cope with COVID-19.
In addition, the typical patient with CLL may already have background risk factors for life-threatening COVID-19 that apply to the general population. Notably male gender, age >65 years, and medical conditions such as cardiovascular disease, diabetes, chronic respiratory disease, hypertension, other cancers, chronic kidney disease, and >2 underlying diseases are known risk factors of morbidity and mortality from COVID-19.14–16 Accordingly, around 70% of patients with CLL are male, 70% are older than 65 years, 25% harbor >2 comorbidities, 21% have hypertension, 13% cardiovascular disease, 26% diabetes, and 5% chronic respiratory disease.17,18
Communication with patients can both mitigate emotional outcomes and improve adherence to public health, non-pharmaceutical interventions aiming at reducing the risk of infection.19
We limit patients’ exposure to potential nosocomial SARS-CoV-2 infection by minimizing the number of visits, postponing in-hospital routine follow-up appointments, and substituting them with remote check-ins. Routine lab samples are often omitted in the absence of new or increasing symptoms and, in case they are needed, local/home collection is a viable option
There is solid evidence supporting that, in the absence of a vaccine, the sole effective prevention of SARS-CoV-2 infection and COVID-19 is public health, non-pharmaceutical interventions aimed at reducing contact rates in the population and thereby reducing transmission of the virus.20–28 Nosocomial spread of SARS-CoV-2 across patients and health-care professionals is a serious concern.29–32 The final goal should be to have COVID-19 free environments for safely and routinely taking care of patients with CLL, also during both endemic and future epidemic outbreaks, particularly in institutions with dedicated cancer centers.33
Access to the hospital for investigations that are not iwCLL guideline recommended must be avoided to prevent nosocomial SARS-CoV-2 infection. Marrow aspirate and biopsy generally are not required for the diagnosis of CLL.34 The staging of CLL does not use CT scans but relies on physical examination and blood counts.34 The majority of relapses or progressions in CLL are detected by physical examination and blood counts, not by imaging studies.35 For patients enrolled in clinical trials, the patient's safety remains a priority and it is better to avoid all unnecessary visits, CT scans and lab tests requested per protocol, following regulatory agencies and/or sponsor ad hoc guidelines. Only those exams that will have a direct impact on the clinical management of patients should be performed and in-hospital visits should be replaced with remote consultations.
Management of patients with CLL needing therapy during the pandemic
For patients in need of treatment, we recommend postponing initiation of therapy, if possible, until the epidemic trajectory is decreasing
CLL is a chronic disease that very rarely poses an imminent risk of death even when it is in advanced stage. The risk of death from COVID-19 in patients with CLL has not yet been established, making it difficult to balance the risks of SARS-CoV-2 infection and those of starting, deferring, or halting treatment on life expectancy. Nevertheless, under an epidemic scenario, we estimate the risks of community and nosocomial infection by SARS-CoV-2 and of complicated COVID-19 higher than the risk of delaying CLL treatment. Under an endemic scenario (ie, Rτ <1, where Rτ is the average number of secondary infections produced when one infected individual is introduced into a host population where everyone is susceptible, Rτ >1 indicates that outbreak will lead to an epidemic, and Rτ <1 that the outbreak will become extinct),36 we estimate the benefit of a treatment known to prolong the survival of patients with CLL higher than the risks of community and nosocomial infection by SARS-CoV-2 and symptomatic COVID-19.
This reasoning is based on the following indirect evidence. First, in cancer patients, the COVID-19 case fatality rate is estimated to be 6% to 7%.6–8,10,37,38 Unadjusted statistics point to a higher mortality by COVID-19 among cancer patients than in the general population.4,5 Likewise, in a retrospective study during the 2009 influenza A (H1N1) virus pandemic, cancer patients had a higher incidence of 30-day mortality (18%) compared with the general population.39 Second, a pattern of decreasing risk of death was reported for the Middle East respiratory syndrome as the infection reproduction number declined toward a more endemic level (Rτ <1).40 Third, the introduction of chemo(immuno)therapy and targeted agents in the treatment of CLL led to a 6% relative survival improvement and to a 10% decrease of deaths per 100-patient/year compared to palliative therapies used in the 1980s.41,42
The decision about delivering treatment should be primarily influenced by the tempo of SARS-CoV-2 epidemiology, the local situation of the hospital and the potential therapeutic benefit of the anti-leukemic therapy. CLL rarely conveys the need for immediate, urgent therapy that cannot be postponed a few weeks while waiting for a decline of the outbreak and a safer delivery of the drugs. Therefore, during the rise and the peak of the SARS-CoV-2 epidemic, we strongly consider the possibility of delaying the start of a treatment even in advanced stage CLL. It is known that advanced stage CLL is seldom complicated by life-threatening end organ damage or profound, debilitating symptoms requiring immediate treatment. In addition, it is important to note that lymph node size and degree of cytopenia do not affect progression free survival of targeted treatment of CLL,43–61 and that cytopenias may remain stable over an extended period slightly below the suggested thresholds to initiate therapy.
Bulky disease, as per iwCLL guidelines, is defined as >10 cm lymph node size but this should not be axiomatically assumed to be synonymous with impending organ compression34 and should be carefully evaluated on an individualized basis. In both treatment naïve and relapsed CLL, bulky lymphadenopathy occurs in only 10% of patients.43–61
The iwCLL recommends starting therapy when the Hb level is <10 g/dL, as a proxy of lower quality of life and cardiovascular risk; in other conditions, symptomatic anemia rather than a defined cut-off is used to trigger intervention. Iron deficiency with or without anemia is a frequent complication in lymphoid malignancies and more in general in cancer, occurring in approximately 40% of cases and must be considered in the differential diagnosis of anemia.62,63
Decreased hemoglobin for autoimmune hemolytic anemia can be managed with a course of corticosteroids and it is not an indication for anti-CLL treatment. Corticosteroids have the largest evidence of activity in CLL-related autoimmune hemolytic anemia and are the guidelines-recommended first line treatment.34 It is not known whether corticosteroids increases the risk of SARS-CoV-2 infection or mitigates its severity.29,64–70 Clinical trials with novel agents excluded patients with uncontrolled autoimmune hemolytic anemia.43–46,54,56,58,59 However, treatment with BTK inhibitors facilitate withdrawal of ongoing immune suppressive agents in controlling hemolytic manifestations.71
For platelets, according to the 2018 update of the iwCLL guidelines, a count <100 × 109/l does not require immediate therapeutic intervention and can be tolerated, according to the bleeding risk, with regular monitoring.34 One should also remember that thrombocytopenia may be a feature of the initial presentation of COVID-19.72–74 Immune thrombocytopenia can be effectively treated with corticosteroids but also with agents that are not immunosuppressive, such as intravenous immunoglobulin and oral thrombopoietic (TPO) agents.75 Up to 78% of patients with CLL and immune thrombocytopenia respond to eltrombopag.76 Potential increased risk of thrombosis, which is also a concern in COVID-19,77 has been reported with the use of TPO agents and should be taken into account.75 While prophylactic anticoagulation is recommended for hospitalized COVID-19 patients, its use in the outpatient setting for COVID-19 thrombosis prevention is not supported by prospective clinical trial data.
Disease-related symptoms (ie, extreme fatigue; unintentional weight loss ≥10% within the previous 6 months; fever > 38.0°C for 2 or more weeks without evidence of infection; drenching night sweats for ≥1 month without evidence of infection) or short lymphocyte doubling time (LDT) are very infrequently (∼5%) the only reason to start therapy and we emphasize carefully excluding causes other than CLL.34,78 Prolonged observation can sometimes show improvement of systemic symptoms or LDT.
When treatment cannot be further deferred, we use the systemic therapy that requires fewer clinic visits and/or is less immune suppressive
The rationale of the recommendation is to reduce the risk of nosocomial SARS-CoV-2 infection by reducing hospital visits and to avoid chemo(immuno)therapy, idelalisib plus rituximab and duvelisib, due to the concern about a higher risk of infection. Based on these considerations, we suggest ibrutinib or acalabrutinib and, for logistical reasons, venetoclax for patients not fitting for BTK inhibitors. We use BTK inhibitors as monotherapies instead of rituximab or obinutuzumab combinations and delay combining anti-CD20 monoclonal antibodies with venetoclax until later in the course of treatment when safer.
Ibrutinib, acalabrutinib, and venetoclax prolong progression-free and overall survival with lower risk of infections and similar/lower need for hospital care when compared to chemo(immuno)therapy.43–46,54,56,58,59 The percentage of opportunistic infections reported for ibrutinib is low (4.1%) and similar to that reported for venetoclax (3.1%).79–82 Compared to chemo(immuno)therapy, ibrutinib and acalabrutinib do not produce lymphopenia, a known risk factor for severe COVID-19.79,83–85 The incidence of any ≥3 grade adverse events does not differ between ibrutinib (41%–77%), acalabrutinib (50%), and venetoclax (78%), indicating that the frequency of unplanned visits for adverse event management is likely to be similar for the 3 drugs.43–45,54,56,58 Venetoclax may require additional unplanned visits for tumor lysis management during the ramp up phase.
Ibrutinib treatment requires few routine treatment visits and lab assessments.54 It is associated with a low risk of neutropenia, and the immune reconstitution of T-cells, which in turns decreases the infection rate after the first 6 months of therapy.54,80,84,85 BTK inhibitors are also undergoing investigation (NCT04346199) as an anti-inflammatory therapy in COVID-19, based on a few reports from uncontrolled clinical cases.86,87 The disadvantage of ibrutinib treatment during SARS-CoV-2 outbreak is the continuous schedule not allowing treatment free intervals. However, if ibrutinib is discontinued because of an adverse event while CLL is in remission, the disease may continue being under control for a prolonged period of time before an alternative therapy is required.46,50,88–90
Venetoclax monotherapy preserves T-cells, and immunoglobulins, while transiently reducing the B-lymphocyte count. B-lymphocytes recover to normal levels within an average of 60 days from venetoclax discontinuation.83,91 The disadvantage of venetoclax treatment is the need for frequent access to the hospital during the ramp-up phase to prevent tumor lysis syndrome (TLS).58 In addition, venetoclax treatment has a relatively high risk of neutropenia during the first 3 months, though it does not translate into a high rate of infections and can be easily prevented through the use of G-CSF.79 There is no evidence to support if, and to what extent, neutropenia is predictive of a negative outcome in SARS-CoV-2 infection.
Idelalisib and other approved PI3K inhibitors cause hyper-activation of the immune system resulting in significant autoimmune adverse events, including pneumonitis, and increase the risk of opportunistic infections, particularly when given as front-line therapy or in combination with anti-CD20 monoclonal antibodies.92,93 In addition, in the relapsed setting, idelalisib plus rituximab treated patients have a shorter progression free survival and a higher drug discontinuation rate due to adverse events compared to acalabrutinib treated patients.59
Treatment with rituximab or obinutuzumab produces a marked decrease of B-lymphocytes that may persist for a long time after treatment discontinuation.94 Rituximab therapy may facilitate JC and hepatitis B viral reactivation.95,96 Humoral immunity appears to facilitate COVID-19 recovery.97
Management of patients with CLL undergoing anti-leukemic therapy during the pandemic
We test asymptomatic patients for SARS-CoV-2 infection by nasopharyngeal swab RT-PCR 72-24 hours before starting CLL therapy. During treatment, patients are questioned for clinical manifestations consistent with COVID-19, including atypical symptoms, over the phone or at the clinic's door
RT-PCR is the standard diagnostic test though its performance on nasopharyngeal swab for SARS-CoV-2 shows variable sensitivities ranging from 40% to 70%, but are consistently higher than RT-PCR of oropharyngeal swab.98–102 False negative RT-PCR tests have been reported in patients with CT findings of COVID-19 who were eventually tested positive on lower respiratory tract specimens or with serial upper respiratory tract samplings.103
We monitor closely symptoms and keep a high suspicion for COVID-19 during treatment. Typical symptoms of COVID-19 are fever, myalgia, chills, coryza, cough, shortness of breath or sore throat. Gastrointestinal symptoms, as diarrhea, nausea, anosmia and ageusia can precede the development of fever and lower respiratory tract symptoms.104–106 The specificity of such symptoms toward COVID-19 diagnosis is decreased because they may overlap with common adverse events of CLL therapies. In addition, sensitivity of infection-control strategies only based on symptoms triage is limited and these policies are not sufficient to prevent transmission of SARS-CoV-2, with up 50% of SARS-CoV-2 infections detected in an asymptomatic or pre-symptomatic condition in a skilled nursing facility.107,108
In patients developing symptoms consistent with COVID-19, we immediately isolate the patient and proceed to a comprehensive evaluation (SARS-CoV-2 RT-PCR on nasopharyngeal swabs, chest imaging studies, multiplex-nucleic antigen test including influenza, and other respiratory viruses and pathogens like pneumococci). We might offer imaging of the chest in patients without SARS-CoV-2 detected in the upper respiratory tract by RT-PCR but with clinical symptoms of lower respiratory infection.
Patients with CLL may have infectious diseases other than COVID-19, while COVID-19 symptoms are similar to other respiratory infections. Differential diagnoses must therefore include influenza and respiratory tract diseases. Indeed, even during the epidemic up to 50% of patients with fever and respiratory symptoms from the general population are positive for respiratory pathogens other than SARS-CoV-2, depending on the seasonal outbreaks and geographic location.9,109–111 In addition, approximately 10% to 50% of patients with COVID-19 have superinfections.9,111–113
Management of patients on treatment for CLL lacking evidence of COVID-19
We continue treatment with targeted agents in patients lacking COVID-19 symptoms as in normal circumstance with exception of anti-CD20 antibodies
We do not apply prophylactic interruption or dose reductions of ibrutinib, acalabrutinib or venetoclax based on the reasoning that once treatment has started, the dose intensity should be preserved to grant the maximum benefit. This is illustrated by the evidence that temporary ibrutinib dose interruptions associate with shorter progression free survival, suggesting that patients who are able to better adhere to treatment may derive more benefit.46,58,90,114–119
In patients already receiving prophylactic immunoglobulin replacement therapy, the infusions will be used less frequently or replaced with s.c. formulations if available and patients can self-administer them at home
Physicians need to be aware that immunoglobulins are not specifically effective against SARS-CoV-2 because of a lack of specific antibodies within the product, but can help in preventing additional infections. Bacterial secondary infection can complicate viral infections, a situation well known in influenza, and emerging in COVID-19.120,121 Immunoglobulin replacement therapy reduces the risk of major infection in patients with CLL and low serum IgG.122 Subcutaneous formulations are non-inferior to intravenous formulations with the advantage of being self-administered by patients at home after a short training.123 Given the higher risk of thromboembolic events with COVID-19, we recommend assessment of risks vs. benefits in each patient and close monitoring for thromboembolic symptoms.
We encourage to maintain the vaccination program in place at the treating institution including, in particular, against seasonal influenza and Streptococcus pneumoniae if not previously done
Due to the known susceptibility of patients with CLL to common infections, it is wise to protect them through vaccination including the common seasonal diseases such as influenza to limit diagnostic confusion in case of symptoms.121 In some institutions, anti-meningococcal vaccination is also included.
Management of patients on treatment for CLL who receive a COVID-19 diagnosis
In patients on treatment for CLL, who receive a COVID-19 diagnosis, holding therapy until the recovery from infection is a prudent approach
Patients with CLL may be already at increased risk of developing life threatening COVID-19 for multiple reasons, including the underlying cancer, disease-related immune suppression, age, concomitant medical conditions and the immune suppressive effect of most CLL therapies.117–119,124 Thus, if the patient is receiving CLL therapy, its continuation should be carefully considered against the risk of drug-related immune suppression even in cases with mild COVID-19 symptoms. Occasional patients on BTK inhibitors, particularly those recently started and in whom the disease is not yet well controlled, may develop tumor flare with drug hold, which usually resolves rapidly with resumption of the inhibitor. However, most patients with well-controlled disease will remain stable during drug hold.
Despite mild symptoms at the onset of COVID-19, clinicians should be aware that patients at risk of life threatening COVID-19 could sometimes rapidly deteriorate, 1 to 2 weeks after illness onset.117–119,124 We counsel the COVID-19 team to closely monitor these patients with remote 24/24 hours home health care and real time rapid evaluation of complications or with hospitalization. Remdesivir is the sole approved pharmaceutical agent effective at treating severe COVID-19. Use of investigational therapies for treatment of patients with CLL and with COVID-19 should ideally be done in the context of randomized controlled trials.117–119,124
We resume targeted agents if all the following conditions are met: (i) the patient is asymptomatic for at least 48 hours; (ii) at least 14 days have elapsed from symptoms start; (iii) at least two consecutive RT-PCR tests are negative on nasopharyngeal swab samples collected each approximately one week apart.
Beyond day 10 after symptom onset there is little residual risk of infectivity, based on cell culture of upper respiratory tract specimens, despite residual viral RNA shedding detected by RT-PCR.100 The median range of SARS-CoV-2 viral shedding among patients with COVID-19 may indeed be up to 20 days from symptoms and may persist over longer periods in older persons, in those who received immunosuppressive therapy, and in those who had severe illness requiring hospitalization.98–102,125–130
One single RT-PCR test on nasopharyngeal swab has up to 15% false negative results when performed at the time of COVID-19 recovery. It is likely that 2 negative RT-PCR tests on nasopharyngeal swab samples collected 24 hours apart may not be sufficient for viral clearance evaluation, since an average of 7 ± 3 days between two tests is required to exclude an initial false negative assessment.
Appearance of specific IgG might also be informative, keeping in mind that the immunosuppression of patients with CLL in particular under anti-leukemic treatments may hamper a robust response. Seroconversion coincides with a slow but steady decline of sputum viral load and clinical recovery from COVID-19.
We would be prudent in resuming chemoimmunotherapy and consider a longer delay.
Conclusion
If SARS-CoV-2 will transit from an epidemic to an endemic state, recurrent seasonal epidemics of SARS-CoV-2 are expected, and if immunity to SARS-CoV-2 wanes in the same manner as in related coronaviruses, recurrent wintertime outbreaks are likely to occur. The total incidence of SARS-CoV-2 through 2025 will depend crucially on the proportion of patients developing efficient immunity and its duration, as well as the availability of a vaccine and effective therapy. Doctors taking care of patients with CLL must be prepared for possible outbreaks of the infection and adapt the management of patients with CLL accordingly, by reintroducing strict preventive measures during SARS-CoV-2 reappearance, while relaxing them during the post-epidemic period until virus extinction. An expert opinion is the sole evidence that can be provided at the moment, given the lack of any specific data about COVID-19 in CLL. As understanding of SARS-CoV-2 and COVID-19 and the available information evolves, we expect the proposed approach will be modified in the future.
We hope that the comments and recommendations made in this paper are useful to the global medical community, patients with CLL and physicians looking after them. Also, that they serve as background for further refinement as our understanding of SARS-CoV-2 and COVID-19 infection unfolds, a process which requires a continued multidisciplinary and international collaboration.
Sources of Funding
DR received honoraria from Abbvie, AstraZeneca, Gilead, Janssen, Roche, Verastem, and research funding from Abbvie, Gilead, Janssen, Cellestia; MS received honoraria from Abbvie, Genentech, Astra Zeneca, Sound Biologics, Pharmacyclics, Verastem, ADC Therapeutics, Cellectar, Bristol Myers Squibb and Atara Biotherapeutics, and research funding from Mustang Bio, Celgene, Bristol Myers Squibb, Pharmacyclics, Gilead, Genentech, Abbvie, TG Therapeutics, Beigene, Astra Zeneca, Sunesis, Acerta Pharma, Beigene and Merck; JRB received honoraria from AbbVie, Acerta, AstraZeneca, BeiGene, Catapult Therapeutics, Dynamo Therapeutics, Genentech/Roche, Gilead, Juno/Celgene, Kite, Loxo, Novartis, Pfizer, Pharmacyclics, Sunesis, TG Therapeutics Janssen, Teva and Verastem, received research funding from Gilead, Loxo, Sun and Verastem, and is a member of the data safety monitoring board for Morphosys and Invectys; JCB received honoraria from Astra Zeneca, Acerta, Janssen Oncology, Pharmacyclics, and Verastem and research funding from Acerta, Pharmacyclics, and Celgene; GG received honoraria from Abbvie, Janssen, AstraZeneca, Sunesis. MH received honoraria from Roche, Gilead, Mundipharma, Janssen, Celgene, Pharmacyclics, Abbvie and research funding from Roche, Gilead, Mundipharma, Janssen, Celgene, Pharmacyclics, Abbvie; PH received honoraria from Acerta, Janssen, AbbVie; Pharmacyclics, Gilead and Roche; AM received honoraria from TG Therapeutics, Abbvie, Pharmacyclics, Johnson & Johnson, Regeneron, Astra Zeneca, Genentech, LOXO, and Celgene, and research funding from TG Therapeutics, Abbvie, Pharmacyclics, Johnson & Johnson, Regeneron, Genentech, LOXO, Portola, DTRM, and Acerta; PG received honoraria from AbbVie, Acerta/AstraZeneca, Adaptive, ArQule, BeiGene, CelGene/Juno, Dynamo, Gilead, Janssen, Sunesis, and research funding from AbbVie, Gilead, Janssen, Novartis, Sunesis.
Footnotes
Citation: Rossi D, Shadman M, Condoluci A, Brown JR, Byrd JC, Gaidano G, Hallek M, Hillmen P, Mato A, Montserrat E, Ghia P. How we Manage Patients with Chronic Lymphocytic Leukemia During the SARS-CoV-2 Pandemic. HemaSphere, 2020;4:4(e432). http://dx.doi.org/10.1097/HS9.0000000000000432
The authors have no conflicts of interest to disclose.
References
- 1.Leung K, Wu JT, Liu D, et al. First-wave COVID-19 transmissibility and severity in China outside Hubei after control measures, and second-wave scenario planning: a modelling impact assessment. Lancet. 2020;395:1382–1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kissler SM, Tedijanto C, Goldstein E, et al. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science. 2020;368:860–868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baumann T, Delgado J, Montserrat E. CLL and COVID-19 at the hospital Clinic of Barcelona: an interim report. Leukemia. 2020;34:1954–1956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dai M, Liu D, Liu M, et al. Patients with cancer appear more vulnerable to SARS-COV-2: a multi-center study during the COVID-19 outbreak. Cancer Discov. 2020;10:783–791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mehta V, Goel S, Kabarriti R, et al. Case Fatality Rate of Cancer Patients with COVID-19 in a New York Hospital System. Cancer Discov. 2020;10:935–941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yu J, Ouyang W, Chua MLK, et al. SARS-CoV-2 Transmission in Patients With Cancer at a Tertiary Care Hospital in Wuhan, China. JAMA Oncol. 2020;March 25. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Desai A, Sachdeva S, Parekh T, et al. COVID-19 and cancer: lessons from a pooled meta-analysis. JCO Glob Oncol. 2020;6:557–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liang W, Guan W, Chen R, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21:335–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.He W, Chen L, Chen L, et al. COVID-19 in persons with haematological cancers. Leukemia. 2020;34:1637–1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang L, Zhu F, Xie L, et al. Clinical characteristics of COVID-19-infected cancer patients: a retrospective case study in three hospitals within Wuhan, China. Ann Oncol. 2020;31:894–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Teh BW, Tam CS, Handunnetti S, et al. Infections in patients with chronic lymphocytic leukaemia: mitigating risk in the era of targeted therapies. Blood Rev. 2018;32:499–507. [DOI] [PubMed] [Google Scholar]
- 12.Chen G, Wu D, Guo W, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020;130:2620–2629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Russell CD, Millar JE, Baillie JK. Clinical evidence does not support corticosteroid treatment for 2019-nCoV lung injury. Lancet. 2020;395:473–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) Outbreak in China: summary of a report of 72,314 cases from the Chinese center for disease control and prevention. JAMA. 2020 February 24. [Epub ahead of print]. [DOI] [PubMed]
- 15.Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020;March 23. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 16.Chen R, Liang W, Jiang M, et al. Risk factors of fatal outcome in hospitalized subjects with coronavirus disease 2019 from a nationwide analysis in China. Chest. 2020;158:97–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stauder R, Eichhorst B, Hamaker ME, et al. Management of chronic lymphocytic leukemia (CLL) in the elderly: a position paper from an international Society of Geriatric Oncology (SIOG) Task Force. Ann Oncol. 2017;28:218–227. [DOI] [PubMed] [Google Scholar]
- 18.Goede V, Cramer P, Busch R, et al. Interactions between comorbidity and treatment of chronic lymphocytic leukemia: results of German Chronic Lymphocytic Leukemia Study Group trials. Haematologica. 2014;99:1095–1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pfefferbaum B, North CS. Mental Health and the Covid-19 Pandemic. N Engl J Med. 2020;April 13. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 20.Cowling BJ, Ali ST, Ng TWY, et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health. 2020;5:e279–e288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Health Organization. Country & Technical Guidance - Coronavirus disease (COVID-19). 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance. Accessed April 30, 2020.
- 22.Centers for Disease Control and Prevention. Infection Control Guidance for Healthcare Professionals about Coronavirus (COVID-19). 202. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control.html. Accessed April 30, 2020.
- 23.National Institutes of Health. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. 2020. https://www.covid19treatmentguidelines.nih.gov/. Accessed April 30, 2020. [PubMed]
- 24.European Centre for Disease Prevention and Control. COVID-19 2020. https://www.ecdc.europa.eu/en/covid-19-pandemic. Accessed April 30, 2020.
- 25.European Hematology Association. Frequently asked questions regarding SARS-CoV-2 in cancer patients: Recommendations for clinicians caring for patients with malignant diseases. 2020. https://ehaweb.org/assets/Uploads/01-EHA-SWB-Infect-Manuscript-FAQ-COVID19-25032020.pdf. Accessed April 30, 2020. [DOI] [PMC free article] [PubMed]
- 26.American Society of Clinical Oncology. ASCO Coronavirus Resources. 2020. https://www.asco.org/asco-coronavirus-information. Accessed April 30, 2020.
- 27.Hartley DM, Perencevich EN. Public Health Interventions for COVID-19: Emerging Evidence and Implications for an Evolving Public Health Crisis. JAMA. 2020;April 10. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 28.Pan A, Liu L, Wang C, et al. Association of Public Health Interventions With the Epidemiology of the COVID-19 Outbreak in Wuhan, China. JAMA. 2020;323:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.National University Cancer Institute of Singapore Workflow Team A Segregated-Team Model to Maintain Cancer Care During the COVID-19 Outbreak at an Academic Center in Singapore. Ann Oncol. 2020;31:840–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ueda M, Martins R, Hendrie PC, et al. Managing Cancer Care During the COVID-19 Pandemic: Agility and Collaboration Toward a Common Goal. J Natl Compr Canc Netw. 2020;1–4. [DOI] [PubMed] [Google Scholar]
- 32.He X, Lau EHY, Wu P, et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. 2020;26:672–675. [DOI] [PubMed] [Google Scholar]
- 33.Guo ZD, Wang ZY, Zhang SF, et al. Aerosol and surface distribution of severe acute respiratory syndrome coronavirus 2 in hospital Wards, Wuhan, China. Emerg Infect Dis. 2020;26:1583–1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hallek M, Cheson BD, Catovsky D, et al. iwCLL guidelines for diagnosis, indications for treatment, response assessment, and supportive management of CLL. Blood. 2018;131:2745–2760. [DOI] [PubMed] [Google Scholar]
- 35.Eichhorst BF, Fischer K, Fink AM, et al. Limited clinical relevance of imaging techniques in the follow-up of patients with advanced chronic lymphocytic leukemia: results of a meta-analysis. Blood. 2011;117:1817–1821. [DOI] [PubMed] [Google Scholar]
- 36.Anderson R, May R. Infectious Diseases of Humans: Oxford Science Publications; 1992.
- 37.van de Haar J, Holes LR, Coles CE, et al. Caring for patients with cancer in the COVID-19 era. Nat Med. 2020;26:665–671. [DOI] [PubMed] [Google Scholar]
- 38.Hanna TP, Evans GA, Booth CM, et al. Cancer, COVID-19 and the precautionary principle: prioritizing treatment during a global pandemic. Nat Rev Clin Oncol. 2020;17:268–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dignani MC, Costantini P, Salgueira C, et al. Pandemic 2009 Influenza A (H1N1) virus infection in cancer and hematopoietic stem cell transplant recipients; a multicenter observational study. F1000Res. 2014;3:221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yang YM, Hsu CY, Lai CC, et al. Impact of comorbidity on fatality rate of patients with middle east respiratory syndrome. Sci Rep. 2017;7:11307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brenner H, Gondos A, Pulte D. Recent trends in long-term survival of patients with chronic myelocytic leukemia: disclosing the impact of advances in therapy on the population level. Haematologica. 2008;93:1544–1549. [DOI] [PubMed] [Google Scholar]
- 42.Abrisqueta P, Pereira A, Rozman C, et al. Improving survival in patients with chronic lymphocytic leukemia (1980–2008): the Hospital Clinic of Barcelona experience. Blood. 2009;114:2044–2050. [DOI] [PubMed] [Google Scholar]
- 43.Shanafelt TD, Wang XV, Kay NE, et al. Ibrutinib-Rituximab or chemoimmunotherapy for chronic lymphocytic leukemia. N Engl J Med. 2019;381:432–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Woyach JA, Ruppert AS, Heerema NA, et al. Ibrutinib regimens versus chemoimmunotherapy in older patients with untreated CLL. N Engl J Med. 2018;379:2517–2528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Moreno C, Greil R, Demirkan F, et al. Ibrutinib plus obinutuzumab versus chlorambucil plus obinutuzumab in first-line treatment of chronic lymphocytic leukaemia (iLLUMINATE): a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2019;20:43–56. [DOI] [PubMed] [Google Scholar]
- 46.Kater AP, Seymour JF, Hillmen P, et al. Fixed duration of venetoclax-rituximab in relapsed/refractory chronic lymphocytic leukemia eradicates minimal residual disease and prolongs survival: post-treatment follow-up of the MURANO phase III study. J Clin Oncol. 2019;37:269–277. [DOI] [PubMed] [Google Scholar]
- 47.Burger JA, Sivina M, Jain N, et al. Randomized trial of ibrutinib vs ibrutinib plus rituximab in patients with chronic lymphocytic leukemia. Blood. 2019;133:1011–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Roberts AW, Ma S, Kipps TJ, et al. Efficacy of venetoclax in relapsed chronic lymphocytic leukemia is influenced by disease and response variables. Blood. 2019;134:111–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Byrd JC, Hillmen P, O’Brien S, et al. Long-term follow-up of the RESONATE phase 3 trial of ibrutinib vs ofatumumab. Blood. 2019;133:2031–2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Byrd JC, Furman RR, Coutre SE, et al. Ibrutinib treatment for first-line and relapsed/refractory chronic lymphocytic leukemia: Final analysis of the pivotal phase 1b/2 PCYC-1102 study. Clin Cancer Res. 2020;March 24. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Brown JR, Hillmen P, O’Brien S, et al. Extended follow-up and impact of high-risk prognostic factors from the phase 3 RESONATE study in patients with previously treated CLL/SLL. Leukemia. 2018;32:83–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.O’Brien S, Furman RR, Coutre S, et al. Single-agent ibrutinib in treatment-naive and relapsed/refractory chronic lymphocytic leukemia: a 5-year experience. Blood. 2018;131:1910–1919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Munir T, Brown JR, O’Brien S, et al. Final analysis from RESONATE: Up to six years of follow-up on ibrutinib in patients with previously treated chronic lymphocytic leukemia or small lymphocytic lymphoma. Am J Hematol. 2019;94:1353–1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Burger JA, Barr PM, Robak T, et al. Long-term efficacy and safety of first-line ibrutinib treatment for patients with CLL/SLL: 5 years of follow-up from the phase 3 RESONATE-2 study. Leukemia. 2020;34:787–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sharman JP, Coutre SE, Furman RR, et al. Final results of a randomized, phase III Study of rituximab with or without idelalisib followed by open-label idelalisib in patients with relapsed chronic lymphocytic leukemia. J Clin Oncol. 2019;37:1391–1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sharman JP, Egyed M, Jurczak W, et al. Acalabrutinib with or without obinutuzumab versus chlorambucil and obinutuzmab for treatment-naive chronic lymphocytic leukaemia (ELEVATE TN): a randomised, controlled, phase 3 trial. Lancet. 2020;395:1278–1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Flinn IW, Hillmen P, Montillo M, et al. The phase 3 DUO trial: duvelisib vs ofatumumab in relapsed and refractory CLL/SLL. Blood. 2018;132:2446–2455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fischer K, Al-Sawaf O, Bahlo J, et al. Venetoclax and obinutuzumab in patients with CLL and coexisting conditions. N Engl J Med. 2019;380:2225–2236. [DOI] [PubMed] [Google Scholar]
- 59.Ghia P. Acalabrutinib vs Rituximab Plus Idelalisib (IdR) or Bendamustine (BR) by Investigator Choice in Relapsed/Refractory (RR) chronic lymphocytic leukemia: phase 3 ASCEND Study. Hematol Oncol. 2019;37:86–87. [Google Scholar]
- 60.Byrd JC, Wierda WG, Schuh A, et al. Acalabrutinib monotherapy in patients with relapsed/refractory chronic lymphocytic leukemia: updated phase 2 results. Blood. 2020;135:1204–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Awan FT, Schuh A, Brown JR, et al. Acalabrutinib monotherapy in patients with chronic lymphocytic leukemia who are intolerant to ibrutinib. Blood Adv. 2019;3:1553–1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ludwig H, Muldur E, Endler G, et al. Prevalence of iron deficiency across different tumors and its association with poor performance status, disease status and anemia. Ann Oncol. 2013;24:1886–1892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hedenus M, Karlsson T, Ludwig H, et al. Intravenous iron alone resolves anemia in patients with functional iron deficiency and lymphoid malignancies undergoing chemotherapy. Med Oncol. 2014;31:302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Auyeung TW, Lee JS, Lai WK, et al. The use of corticosteroid as treatment in SARS was associated with adverse outcomes: a retrospective cohort study. J Infect. 2005;51:98–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chen RC, Tang XP, Tan SY, et al. Treatment of severe acute respiratory syndrome with glucosteroids: the Guangzhou experience. Chest. 2006;129:1441–1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ho JC, Ooi GC, Mok TY, et al. High-dose pulse versus nonpulse corticosteroid regimens in severe acute respiratory syndrome. Am J Respir Crit Care Med. 2003;168:1449–1456. [DOI] [PubMed] [Google Scholar]
- 67.Arabi YM, Mandourah Y, Al-Hameed F, et al. Corticosteroid therapy for Critically Ill patients with Middle East respiratory syndrome. Am J Respir Crit Care Med. 2018;197:757–767. [DOI] [PubMed] [Google Scholar]
- 68.Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with Coronavirus Disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;March 13. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Shang L, Zhao J, Hu Y, et al. On the use of corticosteroids for 2019-nCoV pneumonia. Lancet. 2020;395:683–684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Fang X, Mei Q, Yang T, et al. Low-dose corticosteroid therapy does not delay viral clearance in patients with COVID-19. J Infect. 2020;81:147–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Montillo M, O’Brien S, Tedeschi A, et al. Ibrutinib in previously treated chronic lymphocytic leukemia patients with autoimmune cytopenias in the RESONATE study. Blood Cancer J. 2017;7:e524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Terpos E, Ntanasis-Stathopoulos I, Elalamy I, et al. Hematological findings and complications of COVID-19. Am J Hematol. 2020;95:834–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yang X, Yang Q, Wang Y, et al. Thrombocytopenia and Its Association with Mortality in Patients with COVID-19. J Thromb Haemost. 2020;18:1469–1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zulfiqar AA, Lorenzo-Villalba N, Hassler P, et al. Immune thrombocytopenic purpura in a patient with Covid-19. N Engl J Med. 2020;382:e43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Neunert C, Terrell DR, Arnold DM, et al. American Society of Hematology 2019 guidelines for immune thrombocytopenia. Blood Adv. 2019;3:3829–3866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Visco C, Rodeghiero F, Romano A, et al. Eltrombopag for immune thrombocytopenia secondary to chronic lymphoproliferative disorders: a phase 2 multicenter study. Blood. 2019;134:1708–1711. [DOI] [PubMed] [Google Scholar]
- 77.Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020;135:2033–2040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mozas P, Rivas-Delgado A, Baumann T, et al. Analysis of criteria for treatment initiation in patients with progressive chronic lymphocytic leukemia. Blood Cancer J. 2018;8:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Davids MS, Hallek M, Wierda W, et al. Comprehensive safety analysis of venetoclax monotherapy for patients with relapsed/refractory chronic lymphocytic leukemia. Clin Cancer Res. 2018;24:4371–4379. [DOI] [PubMed] [Google Scholar]
- 80.Sun C, Tian X, Lee YS, et al. Partial reconstitution of humoral immunity and fewer infections in patients with chronic lymphocytic leukemia treated with ibrutinib. Blood. 2015;126:2213–2219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Varughese T, Taur Y, Cohen N, et al. Serious infections in patients receiving ibrutinib for treatment of lymphoid cancer. Clin Infect Dis. 2018;67:687–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Rogers KA, Mousa L, Zhao Q, et al. Incidence of opportunistic infections during ibrutinib treatment for B-cell malignancies. Leukemia. 2019;33:2527–2530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.de Weerdt I, Hofland T, de Boer R, et al. Distinct immune composition in lymph node and peripheral blood of CLL patients is reshaped during venetoclax treatment. Blood Adv. 2019;3:2642–2652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Long M, Beckwith K, Do P, et al. Ibrutinib treatment improves T cell number and function in CLL patients. J Clin Invest. 2017;127:3052–3064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Yin Q, Sivina M, Robins H, et al. Ibrutinib therapy increases T Cell repertoire diversity in patients with chronic lymphocytic leukemia. J Immunol. 2017;198:1740–1747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Treon SP, Castillo J, Skarbnik AP, et al. The BTK-inhibitor ibrutinib may protect against pulmonary injury in COVID-19 infected patients. Blood. 2020;135:1912–1915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Chong EA, Roeker LE, Shadman M, et al. BTK inhibitors in cancer patients with COVID19: “The winner will be the one who controls that chaos” (Napoleon Bonaparte). Clin Cancer Res. 2020;April 28. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Shanafelt TD, Wang XV, Kay NE, et al. Ibrutinib-rituximab or chemoimmunotherapy for chronic lymphocytic leukemia. N Engl J Med. 2019;381:432–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.O’Brien SM, Byrd JC, Hillmen P, et al. Outcomes with ibrutinib by line of therapy and post-ibrutinib discontinuation in patients with chronic lymphocytic leukemia: phase 3 analysis. Am J Hematol. 2019;94:554–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Parikh SA, Achenbach SJ, Call TG, et al. The impact of dose modification and temporary interruption of ibrutinib on outcomes of chronic lymphocytic leukemia patients in routine clinical practice. Cancer Med. 2020;9:3390–3399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Dave N, Gopalakrishnan S, Mensing S, et al. Model-informed dosing of venetoclax in healthy subjects: an exposure-response analysis. Clin Transl Sci. 2019;12:625–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Furman RR, Sharman JP, Coutre SE, et al. Idelalisib and rituximab in relapsed chronic lymphocytic leukemia. N Engl J Med. 2014;370:997–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lampson BL, Kim HT, Davids MS, et al. Efficacy results of a phase 2 trial of first-line idelalisib plus ofatumumab in chronic lymphocytic leukemia. Blood Adv. 2019;3:1167–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.McLaughlin P, Grillo-Lopez AJ, Link BK, et al. Rituximab chimeric anti-CD20 monoclonal antibody therapy for relapsed indolent lymphoma: half of patients respond to a four-dose treatment program. J Clin Oncol. 1998;16:2825–2833. [DOI] [PubMed] [Google Scholar]
- 95.Carson KR, Focosi D, Major EO, et al. Monoclonal antibody-associated progressive multifocal leucoencephalopathy in patients treated with rituximab, natalizumab, and efalizumab: a review from the research on adverse drug events and reports (RADAR) project. Lancet Oncol. 2009;10:816–824. [DOI] [PubMed] [Google Scholar]
- 96.Mozessohn L, Chan KK, Feld JJ, et al. Hepatitis B reactivation in HBsAg-negative/HBcAb-positive patients receiving rituximab for lymphoma: a meta-analysis. J Viral Hepat. 2015;22:842–849. [DOI] [PubMed] [Google Scholar]
- 97.Shen C, Wang Z, Zhao F, et al. Treatment of 5 critically Ill patients with COVID-19 with convalescent plasma. JAMA. 2020;323:1582–1589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wang W, Xu Y, Gao R, et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020;323:1843–1844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Zou L, Ruan F, Huang M, et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177–1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Wolfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients with COVID. Nature. 2020;581:465–469. [DOI] [PubMed] [Google Scholar]
- 101.Liu Y, Yan LM, Wan L, et al. Viral dynamics in mild and severe cases of COVID-19. Lancet Infect Dis. 2020;20:656–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Jin X, Lian JS, Hu JH, et al. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut. 2020;69:1002–1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Rubin GD, Ryerson CJ, Haramati LB, et al. The role of chest imaging in patient management during the COVID-19 pandemic: a multinational consensus statement from the Fleischner society. Chest. 2020;158:106–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Chow EJ, Schwartz NG, Tobolowsky FA, et al. Symptom screening at illness onset of health care personnel with SARS-CoV-2 infection in King County, Washington. JAMA. 2020;323:2087–2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Cheung KS, Hung IF, Chan PP, et al. Gastrointestinal manifestations of SARS-CoV-2 infection and virus load in fecal samples from the Hong Kong Cohort and systematic review and meta-analysis. Gastroenterology. 2020;April 3. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Benezit F, Le Turnier P, Declerck C, et al. Utility of hyposmia and hypogeusia for the diagnosis of COVID-19. Lancet Infect Dis. 2020;April 15. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kimball A, Hatfield KM, Arons M, et al. Asymptomatic and presymptomatic SARS-CoV-2 infections in residents of a long-term care Skilled Nursing Facility - King County, Washington, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Arons MM, Hatfield KM, Reddy SC, et al. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med. 2020;382:2081–2090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kong WH, Li Y, Peng MW, et al. SARS-CoV-2 detection in patients with influenza-like illness. Nat Microbiol. 2020;5:675–678. [DOI] [PubMed] [Google Scholar]
- 110.Bordi L, Nicastri E, Scorzolini L, et al. Differential diagnosis of illness in patients under investigation for the novel coronavirus (SARS-CoV-2), Italy, February 2020. Euro Surveill. 2020;25:2000170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Chu HY, Englund JA, Starita LM, et al. Early detection of Covid-19 through a citywide pandemic surveillance platform. N Engl J Med. 2020;May 1. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Sanità. ISd. Characteristics of SARS-CoV-2 patients dying in Italy. 2020. https://www.epicentro.iss.it/en/coronavirus/bollettino/Report-COVID-2019_20_april_2020.pdf. Accessed on April 30th, 2020.
- 113.Cox MJ. Co-infections: potentially lethal and unexplored in COVID-19. Lancet Microbe. 2020;Published online April 24, 2020. 10.1016/S2666-5247(20)30009-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Hampel PJ, Ding W, Call TG, et al. Rapid disease progression following discontinuation of ibrutinib in patients with chronic lymphocytic leukemia treated in routine clinical practice. Leuk Lymphoma. 2019;60:2712–2719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Thompson PA, Peterson CB, Strati P, et al. Serial minimal residual disease (MRD) monitoring during first-line FCR treatment for CLL may direct individualized therapeutic strategies. Leukemia. 2018;32:2388–2398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Burger JA, Tedeschi A, Barr PM, et al. Ibrutinib as initial therapy for patients with chronic lymphocytic leukemia. N Engl J Med. 2015;373:2425–2437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.World Health Organization. Clinical management of severe acute respiratory infection when COVID-19 is suspected. 2020, March 13. https://www.who.int/publications-detail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected. Accessed April 30th, 2020.
- 118.Sanders JM, Monogue ML, Jodlowski TZ, et al. Pharmacologic treatments for coronavirus disease 2019 (COVID-19): a review. JAMA. 2020;April 13. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 119.Bhimraj A, Morgan RL, Shumaker AH, et al. Infectious diseases society of america guidelines on the treatment and management of patients with COVID-19. Clin Infect Dis. 2020;April 27. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Morris DE, Cleary DW, Clarke SC. Secondary Bacterial Infections Associated with Influenza Pandemics. Front Microbiol. 2017;8:1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Mikulska M, Cesaro S, de Lavallade H, et al. Vaccination of patients with haematological malignancies who did not have transplantations: guidelines from the 2017 European Conference on Infections in Leukaemia (ECIL 7). Lancet Infect Dis. 2019;19:e188–e199. [DOI] [PubMed] [Google Scholar]
- 122.Raanani P, Gafter-Gvili A, Paul M, et al. Immunoglobulin prophylaxis in chronic lymphocytic leukemia and multiple myeloma: systematic review and meta-analysis. Leuk Lymphoma. 2009;50:764–772. [DOI] [PubMed] [Google Scholar]
- 123.Windegger TM, Lambooy CA, Hollis L, et al. Subcutaneous immunoglobulin therapy for hypogammaglobulinemia secondary to malignancy or related drug therapy. Transfus Med Rev. 2017;31:45–50. [DOI] [PubMed] [Google Scholar]
- 124.Alhazzani W, Moller MH, Arabi YM, et al. Surviving sepsis campaign: guidelines on the management of critically Ill adults with coronavirus disease 2019 (COVID-19). Crit Care Med. 2020;48:e440–e469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Yu F, Yan L, Wang N, et al. Quantitative detection and viral load analysis of SARS-CoV-2 in infected patients. Clin Infect Dis. 2020;ciaa345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.To KK, Tsang OT, Leung WS, et al. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study. Lancet Infect Dis. 2020;20:565–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Xu K, Chen Y, Yuan J, et al. Factors associated with prolonged viral RNA shedding in patients with COVID-19. Clin Infect Dis. 2020;ciaa351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Yuan J, Kou S, Liang Y, et al. PCR assays turned positive in 25 discharged COVID-19 patients. Clin Infect Dis. 2020;ciaa398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Lescure FX, Bouadma L, Nguyen D, et al. Clinical and virological data of the first cases of COVID-19 in Europe: a case series. Lancet Infect Dis. 2020;20:697–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Xiao AT, Tong YX, Zhang S. Profile of RT-PCR for SARS-CoV-2: a preliminary study from 56 COVID-19 patients. Clin Infect Dis. 2020;ciaa460. [DOI] [PMC free article] [PubMed] [Google Scholar]


