Abstract
Objective:
To establish a procedural sedation (PS) time line for patients in the pediatric emergency department (PED) with orthopedic injuries.
Methods:
Retrospective review of patients requiring PS for orthopedic injuries. Process times were collected. Ten percent of encounters were co-reviewed. Interrater reliability and descriptive statistics were calculated.
Results:
A total of 189 patients were included. Co-abstracted data demonstrated excellent agreement. The median time to PS and length of stay (LOS) were 214 (interquartile range [IQR]: 160-282) and 320 (IQR: 257-402) minutes, respectively.
Conclusion:
Patients with orthopedic injuries requiring PS experience prolonged PED visits. Interventions should target safely reducing the time to PS and LOS.
Keywords: pediatric, orthopedic injury, procedural sedation
Introduction
Patients presenting to the pediatric emergency department (PED) with orthopedic injuries often require interventions prior to discharge (1). This may necessitate procedural sedation (PS) in order to maintain patient comfort, procedure tolerance, and success (2). Procedural sedation produces an altered level of consciousness that allows patients to tolerate unpleasant procedures (3). In most institutions, the process of PS for orthopedic injuries requires the coordination of several members of the care team, including orthopedics and emergency medicine or pediatrics residents, pediatric emergency medicine (PEM) fellows and attendings, nurses, and respiratory therapists.
This coordination occurs within busy academic emergency departments, in which the frequency of interruptions is high, leading to potential delays, overcrowding, and increased wait times (4,5). This is associated with patient dissatisfaction and increased morbidity and mortality (6 -8). Patient satisfaction influences future health-care utilization, compliance with treatment plans, and willingness to return to the same provider or facility (8 -10).
Streamlining processes in the PED is important for reduced wait times, efficient patient care, and resource allocation. Inefficiencies associated with PS have an effect on the remainder of the PED, as resources are often shared among patients presenting for a variety of complaints. The goal of this investigation was to establish a process time line for patients presenting to the PED for orthopedic injuries in which PS is required.
Methods
Study Design
We performed a retrospective review of all patients presenting to the PED who required PS for orthopedic injuries between November 2, 2017, and June 20, 2018. Data were collected by chart review. This study was reviewed and approved by our institutional review board (protocol #180951).
Study Setting and Population
This study was performed in a high-volume, academic PED with approximately 53 000 visits annually, serving as a major referral source for regional pediatric orthopedic injuries. The majority of patients are initially evaluated by trainees (residents or fellows) or nurse practitioners prior to assessment by attending physicians. Orthopedic surgery consults are placed, when indicated, and patients are evaluated by a resident from this team prior to PS and their performance of the indicated procedure. Our institution has 24-hour, in-house orthopedic coverage. Procedural sedations are performed by PEM attending physicians who are present through the entirety of the procedure. Representatives from nursing and respiratory therapy are present through the entire procedure. It is a policy at our institution that all patients have nothing by mouth (NPO) at least 4 hours prior to nonemergent PS.
Patients were eligible for inclusion if they had PS performed in the PED for an orthopedic procedure. These procedures included fracture reduction, joint aspiration, and hand laceration repair. Patients were excluded from the study if they underwent PS for procedures performed by PEM providers or consultants other than orthopedic surgery, for patients in whom any additional consultants were involved in the patients’ care, or when no PS was ultimately performed in the PED.
Study Protocol
A list of patients in whom PS was performed was generated utilizing billing codes applied to patient visits during the study period. Investigators developed a data dictionary and source hierarchy for review of the electronic medical record (EMR). Before study commencement, investigators jointly reviewed 5 patient charts, during which the source hierarchy was refined. These patients were included in the final study sample.
The list of potentially eligible patients was divided among 3 investigators. Patient charts were evaluated for inclusion eligibility and data were abstracted through a structured review of the patient encounter for eligible patients. In patients deemed ineligible for inclusion in this study, the reason for exclusion as well as discharge diagnosis was recorded. Data were abstracted from the EMR and input directly into a Research Electronic Data Capture (REDCap) database hosted at Vanderbilt University Medical Center (11). If a data element was unavailable in the EMR, it was considered missing for that patient.
To further increase the reliability of our data collection, each of the 3 investigators additionally performed an independent review and data abstraction of 10% of the other investigators’ assigned records. This data abstraction was also recorded in the REDCap database.
Measures
Data collection consisted of times of specific events during the patient’s PED visit, including date and time of patient arrival, patient placement into a room in the PED, first provider evaluation (defined as the time any physician first examined the patient), initial X-ray order, start of initial X-ray, end of initial X-ray, initial X-ray interpretation, orthopedics consult order placement, NPO time, the start of sedation documentation, the start of procedure, first dose of sedative, the end of procedure, the end of sedation documentation, order for postprocedure imaging, completion of postprocedure imaging, patient disposition order, patient discharge, and patient disposition. In patients who were admitted, a discharge time was not recorded. The primary outcome measure was an assessment of the time spent in various phases of care throughout the PED visit for patients with orthopedic injuries undergoing PS.
Data Analysis
Descriptive statistics were generated for continuous variables. To measure interrater reliability, an intraclass correlation coefficient (ICC) for absolute agreement was calculated using 2-way analysis of variance. Data analysis was performed with SPSS (IBM Corp. Released 2017, IBM SPSS Statistics for Macintosh, Version 25.0; IBM Corp, Armonk, New York).
Results
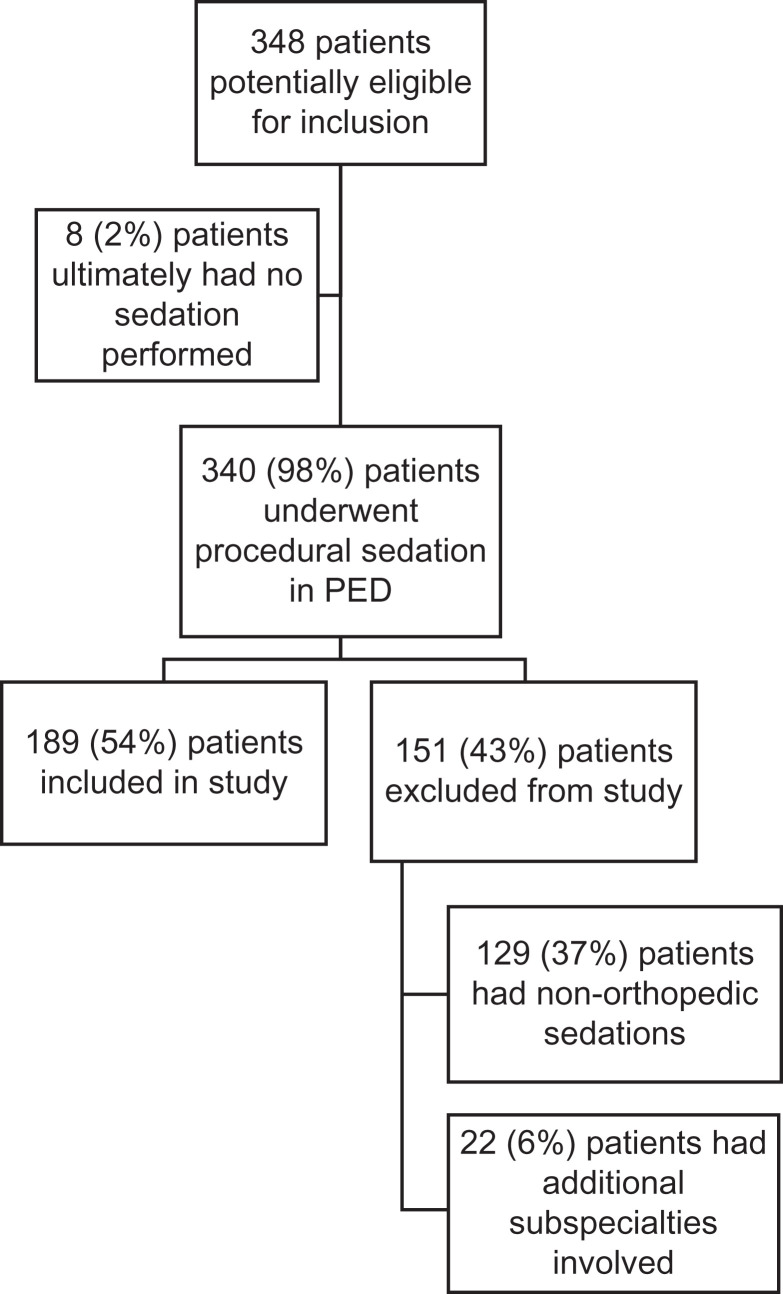
There were 348 potentially eligible patients identified through billing queries of patient encounters between November 2, 2017, and June 20, 2018; 189 (54%) of these patients made up the final study sample (Figure 1). Thirty-five charts were co-reviewed; the ICC was 0.969 (95% confidence interval: 0.959-0.967), indicating excellent agreement between raters.
Figure 1.
Patient inclusion and exclusion flowchart.
For all patients with orthopedic injuries requiring PS, the median time to PS was 214 minutes (interquartile range [IQR]: 160-282). The median time to disposition was 320 minutes (IQR: 257-402). For those patients discharged from the PED (n = 154), the median visit duration was 375 minutes (IQR: 312-456). This included all but 1 case in which a procedure start time was not recorded. The median NPO time was 443 minutes (IQR: 332-593), and 41% were ready for sedation by NPO time on arrival to the PED. Four cases were missing from this measure, in which no NPO time was recorded. Figure 2 depicts the overall PED visit for these patients, broken down by phases of care during the process.
Figure 2.
Time line for patients presenting to the pediatric emergency department with orthopedic injuries requiring procedural sedation.
Discussion
This study was an effort to better understand the process of PS for patients with orthopedic injuries in the PED. We chose to focus on orthopedic injuries, as more than half of PSs in the PED require orthopedic consultation. Process improvement is iterative, and we chose to focus our attention on a specific group of patients, providers, and conditions (12). Half of the patients in this study waited 5 or more hours for PS for their orthopedic injuries, and the total time spent in the PED was more than 6 hours in greater than half of patients who were ultimately discharged. While few other studies have evaluated this process in the PED, these results are similar to those reported by Bawden et al for adult patients with either orthopedic injuries or in whom cardioversion was required (13).
Inefficiencies are likely related to problems with communication and coordination occurring within a busy, academic PED. The traditional flow of the PED and nature of providers to multitask while caring for multiple patients lends itself to breakdown in both communication and care coordination. This is reflected in the time between orthopedic consult and procedure start, with an interquartile range of 78 to 170 minutes suggesting a high degree of variation for patients in this study. These inefficiencies contribute to PED overcrowding, prolonged patient wait times, and reduced patient satisfaction with care delivery (4,8,13). The knowledge gained from this study has additionally offered the opportunity to reexamine policies around patient monitoring (14) and NPO status (15).
In summary, there are many processes contributing to the length of stay for patients presenting to the PED with orthopedic injuries requiring PS. Our next steps will utilize quality improvement methodology focused on process standardization, improved communication, and reduced variation to evaluate the effects of targeted interventions on the process of PS for orthopedic injuries in the PED and patient experience during the process.
Limitations
We have identified several limitations in this study. First, this is a retrospective chart review, and the limitations inherent to this type of study are present here. We attempted to mitigate this by adhering to quality standards of retrospective reviews as well as perform measures of interrater agreement, finding excellent agreement between raters on co-abstracted data. Second, this study was performed over nearly 8 months at a high-volume academic PED, and the results may not be generalizable across all institutions in which pediatric patients present with orthopedic injuries. Additionally, this study focused specifically on PS in which orthopedic injuries required intervention. Thus, we have a cohort of patients who are sedated in the PED in whom we have not studied. This was intentional, as our improvement efforts are focused on orthopedic injuries prior to generalization to other patient populations. Still, these data may not be reflective of patient presenting to the PED requiring sedation for nonorthopedic complaints.
Author Biographies
Adam A Vukovic obtained his medical degree from University of Cincinnati College of Medicine and completed his Pediatrics residency, chief residency, and Pediatric Emergency Medicine fellowship at Cincinnati Children's Hospital Medical Center. He is board certified in both Pediatrics and Pediatric Emergency Medicine. His interests lie in the management of acutely ill or injured child as well as improvement science.
Elizabeth Keiner obtained her medical degree from Florida State University. She is currently completing her Pediatrics residency and will pursue a fellowship in Pediatric Emergency Medicine, both at Vanderbilt University Medical Center.
Holly R Hanson obtained her medical degree from Northeastern Ohio Medical College and completed her Pediatrics residency and Pediatric Emergency Medicine fellowship at Cincinnati Children's Hospital Medical Center. She is board certified in both Pediatrics and Pediatric Emergency Medicine. Her interests include acute kidney injury and the management of acutely ill and injured children.
Footnotes
Authors’ Note: Adam A Vukovic is now affiliated with Department of Pediatrics, University of Cincinnati, College of Medicine and Division of Emergency Medicine, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, USA.
A.A.V. and H.R.H. conceived the study and designed the trial. A.A.V., H.R.H., and E.K. performed data collection. A.A.V. and H.R.H. performed statistical analysis. A.A.V. drafted the manuscript, while H.R.H. and E.K. contributed substantially to its revision. A.A.V. takes responsibility for the paper as a whole.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by UL1 TR000445 from NCATS/NIH (Vanderbilt CTSA).
References
- 1. Joeris A, Lutz N, Wicki B, Slongo T, Audige L. An epidemiological evaluation of pediatric long bone fractures—a retrospective cohort study of 2716 patients from two Swiss tertiary pediatric hospitals. BMC Pediatr. 2014;14:314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hartling L, Milne A, Foisy M, Lang ES, Sinclair D, Klassen TP, et al. What works and what’s safe in pediatric emergency procedural sedation: an overview of reviews. Acad Emerg Med. 2016;23:519–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. American College of Emergency Physicians (physicians ACoE). Procedural sedation in the emergency department. 2017, https://www.acep.org/Content.aspx?id=75479#sm.00001c2nkdojscohyhk1651y6sat2.
- 4. Schull MJ, Slaughter PM, Redelmeier DA. Urban emergency department overcrowding: defining the problem and eliminating misconceptions. CJEM. 2002;4:76–83. [DOI] [PubMed] [Google Scholar]
- 5. Canadian Association of Emergency Physicians and National Emergency Nurses Affiliation. Emergency department overcrowding—position statement. 2003, http://caep.ca/resources/position-statements-and-guidelines/ed-overcrowding-2003.
- 6. Hoot NR, Aronsky D. Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008;52:126–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Nichol JR, Fu R, French K, Momberger J, Handel DA. Association between patient and emergency department operational characteristics and patient satisfaction scores in a pediatric population. Pediatr Emerg Care. 2016;32:139–41. [DOI] [PubMed] [Google Scholar]
- 8. McCarthy ML, Ding R, Zeger SL, Agada NO, Bessman SC, Chiang W, et al. A randomized controlled trial of the effect of service delivery information on patient satisfaction in an emergency department fast track. Acad Emerg Med. 2011;18:674–85. [DOI] [PubMed] [Google Scholar]
- 9. Wartman SA, Morlock LL, Maylitz FE, Palm EA. Patient understanding and satisfaction as predictors of compliance. Med Care. 2010;21:886–91. [DOI] [PubMed] [Google Scholar]
- 10. Mack JL, File KM, Horwitz JE, Prince RA. Factors associated with emergency room choice among Medicare patients. J Ambul Care Mark. 1995;6:45–9. [DOI] [PubMed] [Google Scholar]
- 11. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research Electronic Data Capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Provost LP, Murray SK. The Health Care Data Guide: Learning from Data for Improvement. 1st ed San Francisco, CA: Jossey-Bass; 2011. [Google Scholar]
- 13. Bawden J, Villa-Roel C, Singh M, Fabris G, Bond K, Boyko D, et al. Procedural sedation and analgesia in a Canadian ED: a time-in-motion study. Am J Emerg Med. 2011;29:1083–8. [DOI] [PubMed] [Google Scholar]
- 14. Josephy CP, Vinson DR. Feasibility of single- vs two-physician procedural sedation in a small community emergency department. Am J Emerg Med. 2018;36:977–82. [DOI] [PubMed] [Google Scholar]
- 15. Beach ML, Cohen DM, Gallagher SM, Cravero JP. Major adverse events and relationship to nil per os status in pediatric sedation/anesthesia outside the operating room: a report of the pediatric sedation research consortium. Anesthesiology. 2016;124:80–8. [DOI] [PubMed] [Google Scholar]