Abstract
The present investigation examined the role of mindful attention in regard to the relation between negative affect reduction smoking outcome expectancies and anxious arousal and anhedonic depression symptoms and difficulties with emotion regulation among 174 (46% women; Mage = 25.32 years, SD = 10.51) daily cigarette smokers. As predicted, there was a significant interaction for negative affect reduction smoking outcome expectancies and mindful attention in relation to anxious arousal symptoms and emotion regulation difficulties. Individuals endorsing both higher levels of negative affect reduction outcome expectancies and lower levels of mindful attention reported the greatest anxious arousal symptoms and difficulties with emotion regulation, while those reporting both lower levels of negative affect reduction expectancies and higher levels of mindful attention were associated with lesser anxious arousal symptoms and the least difficulties with emotion regulation. There was no interactive effect for anhedonic depression symptoms. Findings are discussed in relation to better understanding the clinically meaningful interplay between mindful attention and negative affect reduction outcome expectancies among cigarette smokers in terms of affective vulnerability.
Keywords: Smoking, Outcome expectancies, Mindful attention, Anxiety, Depression, Emotion regulation
Introduction
A large body of empirical work has documented an association between cigarette smoking and anxiety and depressive symptoms and their disorders (Grant et al. 2004; Morissette et al. 2007; Patton et al. 1998). Here, bi-directional effects between smoking and both anxiety and depressive symptoms have been documented (Morissette et al. 2007; Zvolensky et al. 2003). For example, some work suggests that smoking may increase and maintain anxiety (Breslau and Klein 1999; Breslau et al. 2004; Goodwin et al. 2005; Isensee et al. 2003; Johnson et al. 2000; McLeish et al. 2007) and depressive symptoms (Choi et al. 1997; Steuber and Banner 2006). Another body of work suggests current and/or recurrent anxiety and depressive symptoms are related to increased daily smoking rates and higher levels of nicotine dependence and can increase the risk of a return to smoking (lapse and relapse) following a quit attempt (Brown et al. 2001; Covey et al. 1997; Haas et al. 2004; Zvolensky et al. 2008a).
Although the nature of the precise relations between smoking and anxiety and depressive symptoms and their disorders remains a subject of active and sustained scientific inquiry (Kalman et al. 2005), it is noteworthy that there is an increasing degree of attention focused on the cognitive-based mechanisms underlying such associations. One promising explanatory candidate in this domain has been outcome expectancies for smoking behavior (beliefs about the putative effects of smoking; Brandon et al. 1999). Outcome expectancies reflect the perceived anticipated consequences of smoking (Brandon 1994; Brandon et al. 1999; Cohen et al. 2002; Cox and Klinger 1988; Niaura et al. 1991). Specifically, smoking outcome expectancies may include beliefs about positive reinforcement (e.g., “I enjoy the taste sensations while smoking”), negative reinforcement/negative affect reduction (referred to from hereafter as negative affect reduction; e.g., “Smoking helps me calm down when I feel nervous”), negative consequences (e.g., “The more I smoke, the more I risk my health”), and appetite control (e.g., “Smoking helps me control my weight”; Brandon and Baker 1991). Outcome expectancies have been helpful in explaining various aspects of smoking behavior (Kelemen and Kaighobadi 2007). For example, greater positive expectancies about the effects of smoking are related to smoking at higher rates (Ahijevych and Wewers 1993; Copeland et al. 1995; Downey and Kilbey 1995), whereas negative affect reduction expectancies are related to decreased rates of successful quit attempts (Wetter et al. 1994).
Of the smoking outcome expectancies, negative affect reduction expectancies may be particularly relevant in regard to better understanding smoking-anxiety/depressive symptom relations. Negative affect reduction outcome expectancies reflect beliefs about the role of smoking in negative mood management whereas negative mood vulnerability reflects the experience of negative affective states (e.g., greater degrees of emotional dysregulation). A central aspect of self-regulation and coping theories of substance use is that individuals may engage in smoking behavior because they believe it can help them cope with aversive emotional states (Abrams and Niaura 1987; Shiffman and Wills 1985). Although the objective mood dampening effects of smoking are complex (Kassel et al. 2003), emotionally vulnerable smokers, specifically, may expect tobacco use to help alleviate aversive or dysregulated affective states (Gonzalez et al. 2008; Gregor et al. 2008; Leyro et al. 2008; Zvolensky et al. 2004a) and may thus often be motivated to smoke for affect regulation purposes (Comeau et al. 2001; Novak et al. 2003; Stewart et al. 1997; Zvolensky et al. 2006b). Aside from the relationship between individual differences in emotional vulnerability and negative affect reduction outcome expectancies, simply believing smoking could be used as an effective response strategy for managing aversive emotional states may confer risk for negative emotional states (Kirsch 1985), thus promoting affective avoidance (e.g., smoking to manage difficult emotions) and decreasing the likelihood that more effective coping skills are used. That is, although an individual smoker may hold varied beliefs about the effects of smoking (Brandon and Baker 1991), those persons who hold the strongest beliefs that smoking will yield effective mood management benefits may be the most prone to affective disturbances. Consistent with this perspective, negative affect reduction outcome expectancies have been found to predict negative emotional reactivity to laboratory-induced stress (Zvolensky et al. 2008b), self-reported anxiety and depressive symptoms, and difficulties with regulating emotions (Johnson et al. 2008). It is noteworthy that these effects are not better accounted for by coping style, level of cigarette use, other substance use (alcohol or marijuana), comorbid psychopathology, or individual differences in negative emotional factors (e.g., neuroticism; Johnson et al. 2008).
Although negative affect reduction outcome expectancies for smoking may serve to enhance or mark risk for negative emotional vulnerability among smokers, there has not been scientific attention focused on other cognitive factors that could modify such effects. Given that these expectancies can shape smoking behavior (e.g., negative affect reduction oriented cigarette smoking; Ahijevych and Wewers 1993; Copeland et al. 1995; Downey and Kilbey 1995), one factor that may be a good candidate in altering the above noted relations between negative affect reduction expectancies and negative affective states is mindfulness. Although there are different operational definitions and theoretical conceptualizations of mindfulness (Grossman 2008; Kabat-Zinn et al. 1986, 1992; Linehan 1993; Parks et al. 2001; Segal et al. 2002; Walser and Westrup 2007), a particularly promising approach has been to conceptualize this construct as “attention to, and awareness of, what is occurring in the present moment” (p. 824; Brown and Ryan 2003; MacKillop and Anderson 2007; please note that from hereafter we refer to mindful attention and awareness as simply ‘mindful attention’ for ease of presentation). Brown and Ryan (2003) have developed a theoretically grounded and empirically driven measure entitled the Mindful Attention Awareness scale that putatively indexes individual differences in the frequency of mindful states over time. It should be noted that although some researchers have argued that the MAAS can be conceptualized as a direct measurement of attention lapses or lack of mindfulness (e.g., Cheyne et al. 2006), others have consistently interpreted and applied the measure as assessing mindful attention (Carlson and Brown 2005; Baer et al. 2006; Herndon 2008; Gonzalez et al. 2009; MacKillop and Anderson 2007; O’Loughlin and Zuckerman 2008). Thus, there is some overarching level of ambiguity related to the construct validity of the MAAS in terms of whether it measures a lack rather than the presence of mindful attention. Despite the lack of scientific consensus, higher levels of mindful attention (as indexed by the MAAS; Brown and Ryan 2003) have been related to both lower levels of anxious arousal (Vujanovic et al. 2007) and anhedonic depressive symptoms (Zvolensky et al. 2006c). Moreover, one study found that lower levels of mindful attention interacted with higher levels of fears of internal sensations (anxiety sensitivity) for greatest risk of anxious arousal symptoms (Vujanovic et al. 2007).
Given the aforementioned relations, higher levels of mindful attention may serve to lessen the established association between negative affect reduction smoking expectancies in regard to anxious arousal and anhedonic depression symptoms and emotion regulation difficulties, although this issue has not yet been empirically explored. Specifically, mindful attention may theoretically interact with negative affect reduction expectancies in a clinically-meaningful way regarding anxious arousal and anhedonic depression symptoms and difficulties with emotion regulation. Given the negative associations between mindful attention and anxiety and depressive symptoms (Brown and Ryan 2003; Vujanovic et al. 2007; Zvolensky et al. 2006c), higher levels of mindful attention may weaken the positive association between higher levels of negative affect reduction expectancies and negative emotional states. Similarly, lower levels of mindful attention and higher levels of negative affect reduction expectancies may be the combination associated with the highest levels of anxiety and depressive symptoms and difficulties with emotion regulation. Thus, mindful attention may serve at least one or several (related) theoretically-relevant functions in modulating the association between negative affect reduction expectancies for smoking and affective vulnerability. For example, smokers possessing higher levels of mindful attention may be more aware of their present-oriented, cognitive-affective experiences, and thus, may be less likely to smoke in an automated fashion for affect regulation purposes (expecting smoking to reduce negative affective states); thereby, lessening their risk for the exacerbation of anxiety and depressive symptoms and therefore bolstering their abilities to regulate negative emotions more adaptively. Conversely, smokers with lower levels of mindful attention and higher levels of negative affect reduction outcome expectancies may be more apt to smoke reactively to reduce negative affective states, without necessarily being cognizant of their current cognitive-affective experience; consequently reinforcing their smoking behavior and theoretically increasing emotional vulnerability/negative affective states. Here, higher levels of mindful attention among individuals with negative affect reduction outcome expectancies for smoking may serve a protective role, lessening the impact of such beliefs on smoking behavior, and thus, potentially ameliorating the deleterious effects of smoking for coping-oriented reasons on emotional well-being. Additionally, greater attention to, and awareness of, present-oriented internal experiences, including cognitions and affective experiences, may be associated with more adaptive coping strategies (e.g., observing, acting with awareness) that lessen an individual’s propensity for emotional vulnerability.
Together, the present investigation sought to examine the role of mindful attention in regard to the relation between negative affect reduction cigarette smoking outcome expectancies and negative emotional vulnerability, defined here as anxious arousal and anhedonic depression symptoms and difficulties with emotion regulation, among daily cigarette smokers. Both mindful attention and negative affect reduction outcome expectancies are theorized to be cognitive variables (Brandon and Baker 1991; Brown and Ryan 2003). It was hypothesized that mindful attention would interact with negative affect reduction expectancies in the prediction of negative emotional vulnerability (indexed by anxious arousal, anhedonic depression, and difficulties with emotion regulation) above and beyond the variance accounted for by the frequency of substance use (cigarettes, alcohol, and marijuana), and the individual main effects of mindful attention and negative affect reduction expectancies. Specifically, it was hypothesized that higher levels of mindful attention would weaken the associations between higher levels of negative affect reduction expectancies and greater degrees of negative emotional vulnerability (i.e., anxious arousal, anhedonic depression, and difficulties with emotion regulation). In a related fashion, it was hypothesized that lower levels of mindful attention and higher degrees of negative affect reduction expectancies would be associated with the highest levels of negative emotional vulnerability (i.e., anxious arousal, anhedonic depression, and difficulties with emotion regulation).
Method
Participants included 174 (46% women; Mage = 25.32 years, SD = 10.51; observed range = 18–60) persons who endorsed being daily (current) cigarette smokers. Participants were recruited from the community as part of a larger laboratory study on “emotion” via placement of specifically-tailored (i.e., “Are you a smoker?”) study flyers throughout various community settings as well as posting of printed advertisements in local newspapers. The racial distribution of the sample generally reflected that of the Vermont population (State of Vermont Department of Health 2007): 95% of the sample identified as Caucasian, 3% as African American, 1% as Hispanic and 1% as “other.” On average, participants reported smoking 16 cigarettes per day (M = 16.30, SD = 11.93; observed range = 1–100) in the last week, smoking their first cigarette at age 14 (M = 14.20, SD = 3.71), becoming a regular smoker by age 16 (M = 16.12, SD = 3.59), and smoking regularly for the past 9 years (M = 8.58, SD = 9.68). According to the Fagerström test for nicotine dependence (FTND; Fagerstrom 1978), the sample was mildly nicotine dependent (M = 2.68, SD = 1.64). Approximately 86% of the sample reported being a current drinker, consuming alcoholic beverages approximately 2–4 times per month at a rate of approximately 4–5 drinks per occasion. Sixty-nine percent of the sample reported using marijuana in the past 30 days. Current marijuana-using individuals reported smoking marijuana approximately once every week in the past 30 days. Participants were administered the Structured Clinical Interview for DSM-IV Axis I Disorders- Non-Patient Edition (SCID-NP; First et al. 1994) by trained interviewers, to assess for current Axis I disorders, and study exclusionary criteria (please see description of exclusionary criteria below). Overall, 20% of participants met criteria for a current Axis I disorder (12.6% major depressive disorder, 4.6% post-traumatic stress disorder, 1.7% social phobia, 1.1% general anxiety disorder). Reliability checks were conducted on a random sample of 20% of the interviews and no discrepancies were found.
Participants were eligible for this study if they were current cigarette smokers between 18 and 65 years of age. Exclusionary criteria for the investigation included: (1) current suicidality or homicidality; (2) limited mental competency (indexed by not being oriented to person, place, or time during the consenting process) or the inability to provide informed, written consent; (3) endorsement of current or past psychotic-spectrum symptoms; and (4) self-reported endorsement of a major medical illness (e.g., human immunodeficiency virus; cancer).
Measures
The Structured Clinical Interview for DSM-IV Axis I Disorders- Non-Patient Edition (SCID-NP).
The SCID-NP (First et al. 1994) is a well-established diagnostic interview for psychiatric problems. The interview was administered by trained interviewers to determine if participants had current or past psychotic-spectrum symptoms and other Axis I psychopathology.
The Smoking History Questionnaire (SHQ; Brown et al. 2002) is a self-report questionnaire used to assess smoking history and pattern. The SHQ has been successfully used in previous studies as a measure of smoking history, pattern, and symptom-based problems during quitting (Zvolensky et al. 2004b, c). The current investigation utilized the following variables from the SHQ: average number of cigarettes smoked per day, age at first cigarette, and age at onset of regular (daily) cigarette smoking.
The Fagerström Tolerance Questionnaire (FTQ; Fagerstrom 1978) was used as a continuous self-report measure of nicotine dependence. Specifically, the FTQ was administered and scored as the Fagerström test for nicotine dependence (FTND). The FTND is a 6-item scale designed to assess gradations in tobacco dependence (Heatherton et al. 1991). Two items are rated on a four-point Likert-style scale (0–3); and four items are rated dichotomously (yes/no). The FTND has shown good internal consistency, positive relations with key smoking variables (e.g., saliva cotinine; Heatherton et al. 1991; Payne et al. 1994), and high degrees of test-retest reliability (Pomerleau et al. 1994).
The Alcohol Use Disorders Identification Test (AUDIT; Babor et al. 1992) is a 10-item self-report screening measure developed by the World Health Organization to identify individuals with alcohol problems (Babor et al. 1992). There is a large body of literature attesting to the reliability and validity of the AUDIT (Saunders et al. 1993). In the present study, the frequency and quantity items from the AUDIT were used to index current alcohol consumption (an average frequency-by-quantity composite score; Stewart et al. 2001).
The Marijuana Smoking History Questionnaire (MSHQ; Bonn-Miller and Zvolensky 2005) was used to assess marijuana smoking use history and pattern. The MSHQ is a self-report instrument that includes items pertaining to marijuana smoking rate (scaled frequency of use in lifetime and past 30 days). The MSHQ has been employed successfully in past research (e.g., Bonn-Miller et al. 2005) and is available by contacting Dr. Zvolensky.
The Smoking Consequences Questionnaire (SCQ; Brandon and Baker 1991) is a 50-item self-report measure that assesses smoking expectancies on a 10-point Likert-type scale (0 = completely unlikely to 9 = completely likely). The measure and its constituent factors have excellent psychometric properties (Buckley et al. 2005; Brandon and Baker 1991; Downey and Kilbey 1995). The SCQ includes the following subscales: positive reinforcement (e.g., “I enjoy the taste sensations while smoking”), negative affect reduction (e.g., “Smoking helps me calm down when I feel nervous”), negative personal consequences (e.g., “The more I smoke, the more I risk my health”), and appetite control (e.g., “Smoking helps me control my weight”). The negative affect reduction sub-scale (SCQ-NARE), specifically employed in the current report, demonstrated high levels of internal consistency (Cronbach α = .95) in the present sample.
The Mindful Attention Awareness Scale (MAAS; Brown and Ryan 2003) is a 15-item questionnaire on which participants indicate, on a 6-point Likert-type scale (1 = almost always to 6 = almost never), their experience of present events. The items on the MAAS are worded such that they may appear to be measuring mindlessness or inattention (e.g., “I could be experiencing some emotion and not be conscious of it until some time later.”; “I find it difficult to stay focused on what’s happening in the present.”; “I rush through activities without being really attentive to them.”). However, they are rated and scored such that a higher score represents greater attention and awareness paid to present activities and experiences. The MAAS-total score was derived by averaging the ratings of all items. The MAAS has shown good internal consistency and construct validity across a wide range of samples (α = .80–.87; Brown and Ryan 2003; MacKillop and Anderson 2007; Vujanovic et al. 2007; Zvolensky et al. 2006c), and it has demonstrated good internal consistency in the present study (Cronbach α = .91).
The Mood and Anxiety Symptom Questionnaire (MASQ; Watson et al. 1995) is a 62-item measure of affective symptoms. Participants indicate how much they have experienced each symptom during the past week on a 5-point Likert-type scale (1 = not at all to 5 = extremely). Factor analysis indicates that this scale taps distinct anxiety-depression symptom domains. The anxious arousal scale (MASQ-AA.) measures symptoms of somatic tension and arousal (e.g., “felt dizzy”). The anhedonic depression scale (MASQ-AD) measures a loss of interest in life (e.g., “felt nothing was enjoyable”), and reverse-keyed items measure positive affect. The MASQ shows excellent convergence with other measures of anxiety and depression and good discriminative validity for anxious versus depressive symptoms via the MASQ-AA and MASQ-AD scales, respectively (Watson et al. 1995). The MASQ-AA and MASQ-AD subscales displayed good internal consistency (alpha coefficients: .87 and .91, respectively), and were utilized to index anxiety and depressive symptoms, respectively, in the present investigation.
The Difficulties in Emotion Regulation Scale (DERS; Gratz and Roemer 2004) was used to assess emotion dysregulation. This scale consists of 36 items, rated on a 5-point Likert-style scale (1 = almost never to 5 = almost always), which comprise six subscales: non-acceptance of emotional responses (e.g., “when I’m upset, I feel guilty for feeling that way.”), difficulties engaging in goal-directed behavior (e.g., “when I’m upset, I have difficulty getting work done.”), impulse control difficulties (e.g., “when I’m upset I have difficulty controlling my behaviors.”), lack of emotional awareness (e.g., “I pay attention to how I feel.”; reverse scored), limited access to emotion regulation strategies (e.g., “when I’m upset any emotions feel overwhelming.”), and lack of emotional clarity (e.g., “I have no idea how I am feeling.”). Consistent with past work (e.g., Gratz and Roemer 2004), the DERS-total score demonstrated good internal consistency in the present sample (Cronbach α = .93).
Procedure
Interested persons, responding to various community-based advertisements specifically targeting daily smokers, who contacted the research team were given a detailed description of the study over the phone and scheduled for an appointment. Upon arrival to the laboratory, each participant was greeted by a research assistant and provided verbal and written consent to participate in the research study. Next, participants were administered the SCID-NP (First First et al. 1994) by trained interviewers to assess for current or past psychotic-spectrum symptoms and other Axis I diagnoses. If deemed eligible, participants then completed a battery of self-report measures.1 At the end of the laboratory session, participants were debriefed and compensated $20 for their participation.
Data Analytic Strategy
Criterion variables in the hierarchical regression analyses included: (1) MASQ-AA, (2) MASQ-AD, and (3) DERS-total. The main effects of average number of cigarettes smoked per day, alcohol use (an average frequency-by-quantity composite score), and marijuana use in the past 30 days were entered as a block at step 1. These covariates were chosen on an a priori basis because prior work suggests that use of these substances is often related to negative affective states (Zvolensky et al. 2006a) and therefore could affect relations between the studied predictor and criterion variables. At step 2, the main effects (mean-centered) of negative affect reduction expectancies and mindful attention were simultaneously entered. At step 3, the interaction (mean-centered) term of negative affect reduction expectancies by mindful attention was entered.
Results
Descriptive Data and Correlations Among Theoretically-Relevant Variables
Means, standard deviations, the observed range, and zero-order (or bivariate) correlations of all studied variables are reported in Table 1. In general, the observed variability among the studied predictor and criterion variables were within the normal limits for nonclinical populations (see Table 1). Negative affect reduction expectancies were significantly related to mindful attention, sharing 4% of variance. Negative affect reduction expectancies were significantly and positively associated with anxious arousal and anhedonic depressive symptoms (r = .31 and r = .27, respectively) as well as emotional dysregulation (r = .36). Mindful attention was significantly and negatively related to anxious arousal and anhedonic depressive symptoms and emotional dysregulation (range of observed r’s:−.36 to −.51; see Table 1). In contrast, negative affect reduction expectancies and mindful attention were not significantly related to current cigarette, alcohol, or marijuana use (see Table 1).
Table 1.
Descriptive data and zero-order (or bi-variate) relations between variables
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | M | SD | Range |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cigarettes/daya | - | −.31** | −.15 | .06 | −.09 | .11 | .13 | .02 | −.17* | −.10 | 16.30 | 11.93 | 1–100 |
| Alcohol useb | - | .39** | .02 | .11 | .06 | −.17* | .08 | −.47** | .01 | 6.68 | 4.75 | 0–16 | |
| Marijuana usec | - | −.03 | .07 | .11 | −.12 | −.10 | −.44** | .07 | 3.71 | 3.23 | 0–8 | ||
| Negative affect reduction expectanciesd |
- | −.20** | .31** | .27** | .36** | .02 | .13 | 5.41 | 2.03 | 0–9 | |||
| Mindful attentione | - | −.37** | −.36** | −.51** | −.04 | −.09 | 3.87 | 1.01 | 1–6 | ||||
| Anxious arousalf | - | .40** | .56** | .05 | .19* | 26.87 | 9.46 | 17–59 | |||||
| Anhedonic depressiong | - | .55** | .21** | .14 | 57.75 | 15.47 | 16–104 | ||||||
| Emotional dysregulationh | - | −.02 | .19* | 80.78 | 22.76 | 40–153 | |||||||
| Age | - | −.14 | 25.32 | 10.51 | 18–60 | ||||||||
| Genderi | - | N/a | N/a | N/a |
p < .05,
p < .01
Average number of cigarettes smoked per day
Alcohol use (number of drinks per occasion × number of occasions)
Average scaled number of times marijuana used in the past 30 days
Negative affect reduction expectancies sub-scale, smoking consequences questionnaire (Brandon and Baker 1991)
Mindful attention and awareness scale (Brown and Ryan 2003)
Mood and anxiety symptoms questionnaire-anxious arousal (Watson et al. 1995)
Mood and anxiety symptoms questionnaire-anhedonic depression (Watson et al. 1995)
Difficulties in emotion regulation scale (Gratz and Roemer 2004)
Gender coded as 1 = male and 2 = female
In exploratory analyses, it should be noted that gender was not significantly related to either predictor variable and relatively modestly associated with the dependent variables (see Table 1). Here, females relative to males reported significantly higher levels of emotional dysregulation and anxious arousal symptoms. In terms of exploratory analyses for age, there was a consistent negative relation with concurrent substance use (cigarettes per day, alcohol use, and marijuana use; see Table 1). Also, a significant positive relation was evident for age and anhedonic depressive symptoms (r = .21).
Hierarchical Regression Analyses
Please see Table 2 for a summary of hierarchical regression analyses. For anxious arousal symptoms, substance use variables entered at step 1 of the model did not account for a significant amount of the variance. At step 2, the main effects of negative affect reduction expectancies and mindful attention accounted for a significant 20% of the variance, with both predictors making significant contributions (β = .25, p = .001 and β = −.32, p < .001, respectively). At step 3, the negative affect reduction expectancies by mindful attention interactive effect accounted for an additional 3% of the variance (p < .05).
Table 2.
Predictors of anxious arousal, anhedonic depression, and emotional dysregulation
| ΔR2 | t (Each predictor) | β | sr2 | p | |
|---|---|---|---|---|---|
| Dependent variable: anxious arousala | |||||
| Step 1 | .02 | ns | |||
| Cigarettes/dayb | .97 | .08 | .01 | ns | |
| Alcohol usec | .34 | .03 | .00 | ns | |
| Marijuana used | 1.56 | .13 | .01 | ns | |
| Step 2 | .20 | <.001 | |||
| Negative affect reduction expectanciese | 3.46 | .25 | .07 | .001 | |
| Mindful attentionf | −4.50 | −.32 | .11 | <001 | |
| Step 3 | .03 | <05 | |||
| SCQ-NARE × MAAS-total score | −2.42 | −.17 | .04 | <05 | |
| Dependent variable: anhedonic depressiong | |||||
| Step 1 | .06 | <.05 | |||
| Cigarettes/day | 2.16 | .17 | .03 | <.05 | |
| Alcohol use | −1.10 | −.10 | .01 | ns | |
| Marijuana use | −.64 | −.05 | .00 | ns | |
| Step 2 | .15 | <001 | |||
| Negative affect reduction expectancies | 2.55 | .18 | .04 | <.05 | |
| Mindful attention | −4.23 | −.30 | .10 | <001 | |
| Step 3 | .00 | ns | |||
| SCQ-NARE × MAAS-total score | −.67 | −.05 | .00 | ns | |
| Dependent variable: emotional dysregulationh | |||||
| Step 1 | .02 | ns | |||
| Cigarettes/day | .74 | .06 | .00 | ns | |
| Alcohol use | 1.66 | .15 | .02 | ns | |
| Marijuana use | −1.51 | −.13 | .01 | ns | |
| Step 2 | .32 | <001 | |||
| Negative affect reduction expectancies | 3.58 | .24 | .08 | <.001 | |
| Mindful attention | −7.07 | −.48 | .25 | <001 | |
| Step 3 | .04 | <.01 | |||
| SCQ-NARE × MAAS-total score | −2.96 | −.19 | .05 | <01 |
Note: β = Standardized beta weights
Mood and anxiety symptoms questionnaire-anxious arousal (Watson et al. 1995)
Average number of cigarettes smoked/day
Alcohol use (number of drinks per occasion × number of occasions)
Average scaled number of times marijuana used in the past 30 days
Negative affect reduction expectancies sub-scale, smoking consequences questionnaire (SCQ-NARE; Brandon and Baker 1991)
Mindful attention and awareness scale (MAAS-total score; Brown and Ryan 2003)
Mood and anxiety symptoms questionnaire-anhedonic depression (Watson et al. 1995)
Difficulties in emotion regulation scale (Gratz and Roemer 2004)
Regarding anhedonic depressive symptoms, substance use variables at step 1 accounted for a significant portion of variance (R2 = .06, p < .05), with cigarettes smoked per day being the only significant contributor (β = .17, p < .05). At step 2, the main effects of negative affect reduction expectancies and mindful attention accounted for an additional 15% of unique variance, with both predictors making significant contributions (β = .18, p < .05 and β = −.30, p < .001, respectively). At step 3, the interactive effect did not account for any additional variance (ΔR2 = .00).
For emotional dysregulation, substance use variables entered at step 1 of the model did not account for a significant portion of the variance. At step 2, the main effects of negative affect reduction expectancies and mindful attention accounted for an additional 32% of the variance, with both predictors making significant contributions (β = .24 and β = −.48, p’s < .001, respectively). At step 3, the negative affect reduction expectancies by mindful attention interactive effect contributed an additional 4% of unique variance (p < .01) to the model.2
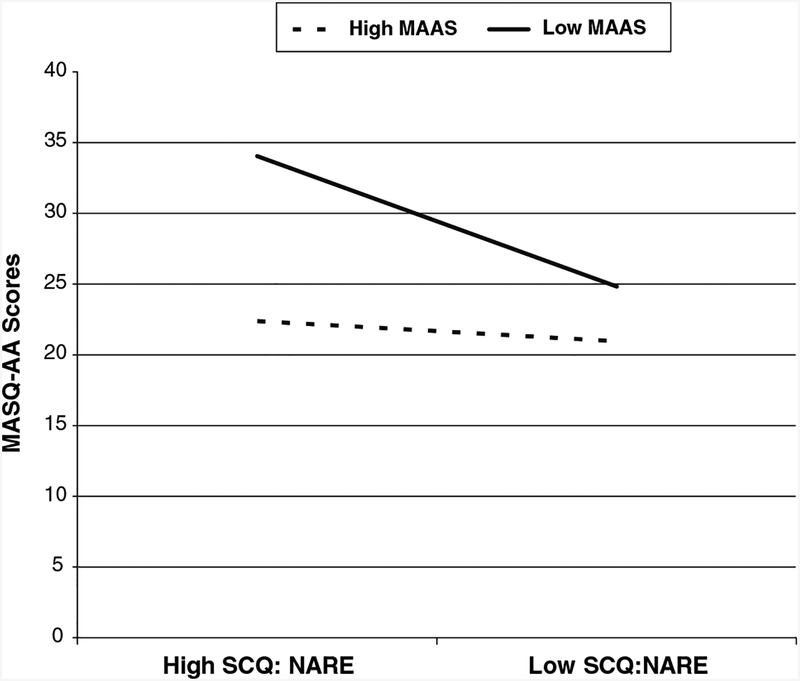
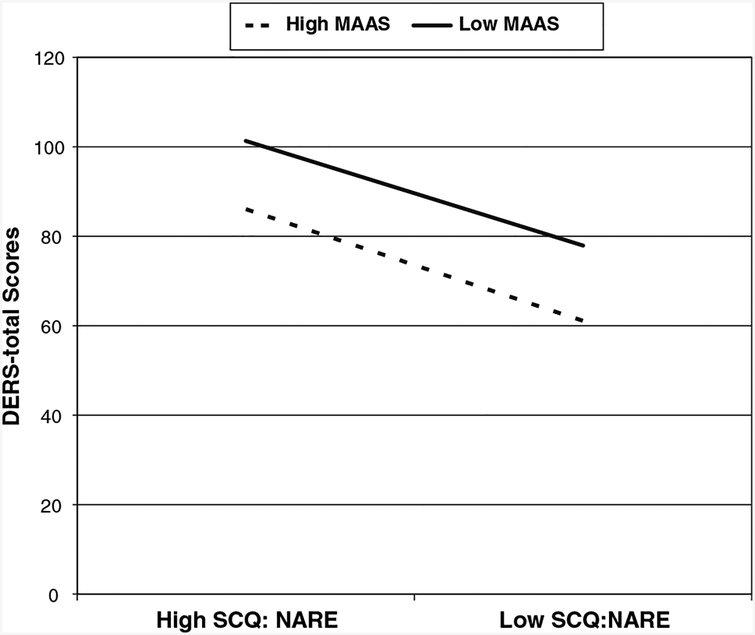
Mapping the Form of the Observed Significant Interactions
The form of the significant interactions were then examined for each criterion variable by plotting the mean value among participants scoring 0.5 standard deviation above and/or below the mean, consistent with the recommendations of Cohen and Cohen (1983, p. 323). As is evident in Fig. 1, the form of the interaction for anxious arousal symptoms indicates that co-occurring high levels of negative affect reduction expectancies and low mindful attention yield the greatest levels of anxious arousal symptoms. High levels of negative affect reduction expectancies and high levels of mindful attention were largely comparable to low negative affect reduction expectancies and low mindful attention. Individuals with low levels of negative affect reduction expectancies and high levels of mindful attention evidenced the lowest levels of anxious arousal symptoms. A generally similar, but not fully identical, pattern of findings was evident for levels of emotional dysregulation (see Fig. 2); here, mindful attention was associated with lower emotional dysregulation scores throughout the observed range of variability.
Fig. 1.
Anxious arousal (MASQ-AA) scores as a function of the interaction of negative affect reduction expectancies (SCQ-NARE) and mindful attention (MAAS-Total) among participants 0.5 SD above and/or below the mean
Fig. 2.
Emotional dysregulation (DERS-total) scores as a function of the interaction of negative affect reduction expectancies (SCQ-NARE) and mindful attention (MAAS-Total) among participants 0.5 SD above and/or below the mean
Discussion
Although empirical investigations have begun to examine the effects of cigarette smoking outcome expectancies in relation to the experience of negative affective symptoms and difficulties with regulating emotions (Zvolensky et al. 2008b; Johnson et al. 2008), work has not yet focused on factors that may serve to impact these negative effects. The present investigation sought to address this gap in the existing literature by examining the role of mindful attention in regard to the relationship between negative affect reduction outcome expectancies and anxious arousal, anhedonic depressive symptoms, and difficulties with emotion regulation.
Consistent with hypotheses, the interactive effect of negative affect reduction expectancies by mindful attention was significantly associated with levels of anxious arousal and emotion regulation difficulties. The size of the observed interactive effects was 3% and 4% of unique variance (respectively) above and beyond the variance accounted for by substance use variables and the significant main effects (see Table 2). Inspection of the form of the interactions was in accord with the a priori theoretical formulation. Specifically, higher levels of negative affect reduction outcome expectancies and lower levels of mindful attention were associated with the greatest degrees of anxious arousal symptoms and difficulties with emotion regulation (see Figs. 1 and 2). Similarly, lower levels of negative affect reduction outcome expectancies and higher levels of mindful attention were associated with the lowest levels of anxious arousal symptoms and emotion regulation difficulties (see Figs. 1 and 2). Overall, this novel pattern of findings highlights the possible clinically-relevant interplay between an established smoking-relevant cognitive vulnerability (negative reinforcement/negative affect reduction outcome expectancies) and promising self-regulatory behaviors (mindful attention) in regard to anxious arousal and difficulties with emotion regulation among daily adult cigarette smokers.
Contrary to prediction, the negative affect reduction outcome expectancies and mindful attention interaction term was not significantly related to anhedonic depressive symptoms. However, there were significant and robust main effects for negative affect reduction outcome expectancies and mindful attention (18% and 30%, respectively) in regard to anhedonic depressive symptoms. These effects were apparent above and beyond the significant portion of variance (6%) accounted for by substance use variables. Incremental associations were in the expected directions, with negative affect reduction outcome expectancies incrementally positively related to anhedonic depressive symptoms, and mindful attention incrementally negatively related to anhedonic depressive symptoms. Other non-smoking focused work in this area has failed to document significant mindful attention-relevant interactive effects in terms of anhedonic depressive symptoms (Vujanovic et al. 2007). This may suggest a unique interplay of vulnerability factors for anhedonic depressive symptoms among smokers, distinct from that for anxious arousal symptoms and difficulties in emotion regulation, broadly defined. Before any definitive conclusions can be made, further work is necessary to replicate and extend the current findings.
In terms of main effects, it is noteworthy that both negative affect reduction outcome expectancies and mindful attention also were incrementally related to anxious arousal and difficulties with emotion regulation, contributing 20% and 32% of unique variance, respectively. As expected, negative affect reduction outcome expectancies were positively related to each of the emotional vulnerability variables. That is, adult smokers reporting greater beliefs that smoking will facilitate affect management reported higher negative emotional vulnerability indexed by the three criterion variables; thus, negative affect reduction outcome expectancies may mark risk for negative mood vulnerability. Also as expected, mindful attention was significantly negatively associated with each of the criterion variables, such that higher levels of mindful attention were related to lower levels of anxious arousal, anhedonic depression, and emotional dysregulation. These findings are consistent with past work related to both smoking-relevant outcome expectancies (e.g., Johnson et al. 2008; Zvolensky et al. 2008b) and mindful attention (e.g., Vujanovic et al. 2007). Notably, negative affect reduction outcome expectancies and mindful attention were significantly negatively correlated with each other at the zero-order level (r = .20, p < .01), indicating that these two variables are distinct, though associated, constructs. It also should be noted that the substance use variables (cigarette use, marijuana use, and alcohol use) were weakly associated with the studied affective variables (dependent measures). These findings are perhaps not surprising given the younger age of the sample and their relative drug using careers (i.e., years of use) in terms of substance use. It would be useful to extend the present tests over time and further evaluate the relations between uni-and poly substance use patterns and affective vulnerability in future work.
The current findings need to be considered in light of several limitations that might be addressed by future work relevant to this line of inquiry. First, the current findings were based on a community sample of relatively homogeneous participants in terms of race/ethnicity and age, limiting the generalizability of the findings. Future work might extend this line of inquiry to more diverse samples. Second, smokers in the current study reported relatively low levels of nicotine dependence, and given documented associations between higher levels of nicotine dependence and anxious and depressive symptoms and affective vulnerability (e.g., Goodwin et al. 2008), future work might wish to sample more highly nicotine dependent smokers. Furthermore, our sample was comprised of young adult smokers who endorsed high levels of marijuana use. Future work may benefit from discerning the singular and interactive effects of concurrent substance use on affect vulnerability among cigarette smokers. Third, the current study tested the associations between smoking-relevant negative affect reduction outcome expectancies and mindful attention, as indexed by the MAAS (Brown and Ryan 2003). To continue to build upon the extant literature and to empirically better understand distinctions between various mindfulness perspectives, it may be advantageous to examine the interplay between alternative smoking-relevant cognitions (e.g., reasons for smoking questionnaire: Ikard et al. 1969), and other mindfulness-based constructs (see Baer et al. 2006). Additionally, it may be advantageous for future work involving the MAAS to include measures of inattentiveness in order to better parse apart the putative effects of the MAAS as a measurement of mindful attention, but not attention lapses. More generally, there may be value in terms of directing future study on the construct validity using the MAAS. This type of work could help more definitely clarify whether the MAAS measures mindful attention, perceived mindlessness, or absentmindedness.
Fourth, the present investigation utilized established self-report instruments as the principal assessment strategy. Though this approach was prudent at this stage of research development, future work might build upon the present findings and incorporate multi-method approaches to index the variables of interest. For example, emotion evocation laboratory paradigms might be used to more rigorously assess anxious and depressive symptoms as well as affect regulation skills in real time. Furthermore, ecological momentary assessments might be implemented to track smoking-relevant outcome expectancies and corresponding affective reactivity in real world settings. Fifth, due to the cross-sectional and correlational nature of the present research design, it is not possible to make causal statements concerning any of the relevant constructs. One important next step in this line of inquiry would therefore be to use prospective research methodologies and evaluate the consistency of the present findings over time. For instance, smokers might be tracked over time so that the evolution of smoking-relevant beliefs and expectancies, clinical symptoms, and affect regulation skills could be monitored longitudinally. Sixth, the present study, as an initial step in this line of inquiry, was focused on individually evaluating the present research hypotheses using a general linear model. Although useful, it is possible future work could benefit from using multivariate approaches such as structural equation modeling to replicate and extend this line of inquiry. Finally, negative affect reduction/negative reinforcement outcome expectancies were conceptualized a priori as a cognitive factor worthy of empirical attention due to the emerging empirical evidence suggesting associations with emotional vulnerability factors (e.g., Zvolensky et al. 2008b). Future work might further extend this line of inquiry by examining other potentially relevant cognitive-affective coping styles as relevant to smoking behavior to better understand affective vulnerability among smokers.
Despite the noted limitations, the documented interactive effect between mindful attention and negative affect reduction outcome expectancies may ultimately have translational implications for clinical intervention among smokers. Specifically, if the current results were replicated and extended through other research designs (as described in the foregoing section), it may suggest that targeting mindful attention may offer a therapeutic avenue to clinically address affective vulnerability among smokers. To explore the potential utility of this translational idea, future treatment-oriented studies could target mindful attention in the context of expectancies about negative affect reduction expectancies to hasten reductions in emotional vulnerability. Here, recent work suggests that mindful attention, as measured by the MAAS, can be cultivated through meditation and mindfulness-based practices (Shapiro et al. 2008). This type of work may be directly relevant to smoking cessation given negative affect and emotional dysregulation are important risk factors for poor cessation outcome (Ziedonis et al. 2008). Accordingly, by decreasing emotional vulnerability, it may be possible to promote greater degrees of success in quitting.
Overall, the current study documented significant interactive effects between negative affect reduction outcome expectancies and mindful attention in regard to anxious arousal and difficulties in emotion regulation, but not anhedonic depressive symptoms. These effects provide preliminary evidence for using facets of mindfulness to moderate the relationship between specific cognitive smoking processes (negative reinforcement/negative affect reduction outcome expectancies) and aspects of emotional vulnerability. Furthermore, both negative affect reduction expectancies and mindful attention were incrementally related to each of the emotional vulnerability variables, underscoring the clinical and theoretical utility in further exploring this line of inquiry so as to better inform relevant clinical advances among smokers.
Footnotes
The present data were a subset of a larger project that involved a laboratory challenge component. The present data have not been published previously and represent a novel heretofore un-examined aspect of the larger data set.
It is noteworthy that the pattern of results and significance levels do not change with addition of levels of nicotine dependence as a covariate (as assessed by the Fagerström test for nicotine dependence; Heatherton et al. 1991).
References
- Abrams DB, & Niaura RS (1987). Social learning theory In Blane HT & Leonard KE (Eds.), Psychological theories of drinking and alcoholism (pp. 131–178). New York: Guilford Press. [Google Scholar]
- Ahijevych K, & Wewers ME (1993). Factors associated with nicotine dependence among African American women cigarette smokers. Research in Nursing and Health, 16(4), 283–292. doi: 10.1002/nur.4770160407. [DOI] [PubMed] [Google Scholar]
- Babor TF, de la Fuente JR, Saunders J, & Grant M (1992). AUDIT-alcohol use disorders identification test: Guidelines for use in primary health care. Geneva: World Health Organization. [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, & Toney L (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13, 27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller MO, & Zvolensky MJ(2005). The Marijuana smoking history questionnaire. Unpublished manuscript, The anxiety and health research laboratory, University of Vermont. [Google Scholar]
- Bonn-Miller MO, Zvolensky MJ, Leen-Feldner EW, Feldner MT, & Yartz AR (2005). Marijuana use among daily tobacco smokers: Relationship to anxiety-related factors. Journal of Psychopathology and Behavioral Assessment, 27, 279–289. [Google Scholar]
- Brandon TH (1994). Negative affect as motivation to smoke. Current Directions in Psychological Science, 3, 33–37. [Google Scholar]
- Brandon TH, & Baker TB (1991). The smoking consequences questionnaire: The subjective expected utility of smoking in college students. Psychological Assessment, 3, 484–491. [Google Scholar]
- Brandon TH, Juliano LM, & Copeland AL (1999). How expectancies shape experience. Washington, DC, US: American Psychological Association. [Google Scholar]
- Breslau N, & Klein DF (1999). Smoking and panic attacks: An epidemiologic investigation. Archives of General Psychiatry, 56, 1141–1147. [DOI] [PubMed] [Google Scholar]
- Breslau N, Novak SP, & Kessler RC (2004). Daily smoking and the subsequent onset of psychiatric disorders. Psychological Medicine, 34, 323–333. [DOI] [PubMed] [Google Scholar]
- Brown RA, Kahler CW, Niaura R, Abrams DB, Sales SD, Ramsey SE, et al. (2001). Cogntive-behavioral treatment for depression in smoking cessation. Journal of Consulting and Clinical Psychology, 69, 471–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Lejuez CW, Kahler CW, & Strong DR (2002). Distress tolerance and duration of past smoking cessation attempts. Journal of Abnormal Psychology, 111, 180–185. [PubMed] [Google Scholar]
- Brown KW, & Ryan RM (2003). The benefits of being present: Mindful attention and its role in psychological well-being. Journal of Personality and Social Psychology, 84, 822–848. [DOI] [PubMed] [Google Scholar]
- Buckley TC, Kamholz BW, Mozley SL, Gulliver SB, Holohan DR, Helstrom AW, et al. (2005). A psychometric evaluation of the smoking consequences questionnaire-adult in smokers with psychiatric conditions. Nicotine & Tobacco Research, 7, 739–745. [DOI] [PubMed] [Google Scholar]
- Carlson LE, & Brown KW (2005). Validation of the mindful attention awareness scale in a cancer population. Journal of Psychosomatic Research, 58, 29–33. [DOI] [PubMed] [Google Scholar]
- Cheyne JA, Carriere JSA, & Smilek D (2006). Absent-mindedness: Lapses of conscious awareness and everyday cognitive failures. Consciousness and Cognition, 15, 578–592. [DOI] [PubMed] [Google Scholar]
- Choi WS, Patten CA, Gillin JC, Kaplan RM, & Pierce JP (1997). Cigarette smoking predicts development of depressive symptoms among US adolescents. Annuals of Behavioral Medicine, 19(4), 2–50. [DOI] [PubMed] [Google Scholar]
- Cohen J, & Cohen P (1983). Applied multiple regression/correlation analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ, US: Erlbaum. [Google Scholar]
- Cohen LM, McCarthy DM, Brown SA, & Myers MG (2002). Negative affect combines with smoking outcome expectancies to predict smoking behavior over time. Psychology of Addictive Behaviors, 16(2), 91–97. [DOI] [PubMed] [Google Scholar]
- Comeau N, Stewart SH, & Loba P (2001). The relations of trait anxiety, anxiety sensitivity, and sensation seeking to adolescents’ motivations for alcohol, cigarette, and marijuana use. Addictive Behaviors, 26, 803–825. [DOI] [PubMed] [Google Scholar]
- Copeland AL, Brandon TH, & Quinn EP (1995). The smoking consequences questionnaire-adult: Measurement of smoking outcome expectancies of experienced smokers. Psychology Assessment, 7(4), 484–494. [Google Scholar]
- Covey LS, Glassman AH, & Stetner F (1997). Major depression following smoking cessation. American Journal of Psychiatry, 154, 263–265. [DOI] [PubMed] [Google Scholar]
- Cox WM, & Klinger E (1988). A motivational model of alcohol use. Journal of Abnormal Psychology, 97(2), 168–180. [DOI] [PubMed] [Google Scholar]
- Downey KK, & Kilbey MM (1995). Relationship between nicotine dependence and alcohol expectancies and substance dependence. Experimental & Clinical Psychopharmacology, 3, 174–182. [Google Scholar]
- Fagerstrom KO (1978). Measuring degree of physical dependence to tobacco smoking with reference to individualization of treatment. Addictive Behaviors, 3, 235–241. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (1994). Structured clinical interview for DSM-IV patient edition (SCID-N/P, Version 2.0). New York: Biometrics Research Department. [Google Scholar]
- Gonzalez A, Solomon SE, Zvolensky MJ, & Miller CT (2009). The interaction of mindful-based attention and awareness and disengagement coping with HIV/AIDS-related stigma in regard to concurrent anxiety and depressive symptoms. Journal of Health Psychology, 14, 403–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez A, Zvolensky MJ, Vujanovic AA, Leyro TM, & Marshall EC (2008). An evaluation of anxiety sensitivity, emotional dysregulation, and negative affectivity among daily cigarette smokers: Relation to smoking motives and barriers to quitting. Journal of Psychiatric Research, 43, 138–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin RD, Lewinsohn PM, & Seeley JR (2005). Cigarette smoking and panic attacks among young adults in the community: The role of parental smoking and anxiety disorders. Biological Psychiatry, 58(9), 686–693. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Zvolensky MJ, & Keyes K (2008). Nicotine dependence and mental disorders among adults in the US: Evaluating the role of mode of administration. Psychological Medicine, 38, 1277–1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Chou SP, Stinson FS, & Dawson DA (2004). Nicotine dependence and psychiatric disorders in the US: Results from the national epidemiologic survey on alcohol and related conditions. Archives of General Psychiatry, 61(11), 1107–1115. [DOI] [PubMed] [Google Scholar]
- Gratz KL, & Roemer L (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26, 41–54. [Google Scholar]
- Gregor K, Zvolensky MJ, McLeish AC, Bernstein A, & Morissette S (2008). Anxiety sensitivity and perceived control over anxiety-related events: Associations with smoking outcome expectancies and perceived cessation barriers among daily smokers. Nicotine & Tobacco Research, 10, 627–635. [DOI] [PubMed] [Google Scholar]
- Grossman J (2008). On measuring mindfulness in psychosomatic and psychological research. Journal of Psychosomatic Research, 64, 405–408. [DOI] [PubMed] [Google Scholar]
- Haas AL, Munoz RF, Humfleet GL, Reus VI, & Hall SM (2004). Influences of mood, depression history, and treatment modality outcomes in smoking cessation. Journal of Consulting and Clinical Psychology, 72, 563–570. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, & Fagerstrom KO (1991). The Fagerstrom test for nicotine dependence: A revision of the Fagerstrom tolerance questionnaire. British Journal of Addiction, 86, 1119–1127. [DOI] [PubMed] [Google Scholar]
- Herndon F (2008). Testing mindfulness with perceptual and cognitive factors: External verses internal encoding, and the cognitive failures questionnaire. Personality and Individual Differences, 3, 2–41. [Google Scholar]
- Ikard FF, Green DE, & Horn D (1969). A scale to differentiate between types of smoking as related to the management of affect. The International Journal of Addictions, 4, 649–659. [Google Scholar]
- Isensee B, Wittchen HU, Stein MB, Höfler M, & Lieb R (2003). Smoking increases the risk of panic: Findings from a prospective community study. Archives of General Psychiatry, 60, 692–700. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Pine DS, Klein DF, Kasen S, & Brook JS (2000). Association between cigarette smoking and anxiety disorders during adolescence and early adulthood. Journal of the American Medical Association, 284, 2348–2351. [DOI] [PubMed] [Google Scholar]
- Johnson KA, Zvolensky MJ, Marshall EC, Gonzalez A, Abrams K, & Vujanovic AA (2008). Linkages between cigarette smoking outcome expectancies and negative emotional vulnerability. Addictive Behaviors, 33, 1416–1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J, Lipworth L, Burney R, & Sellers W (1986). Four-year follow-up of a meditation-based stress reduction program for the self-regulation of chronic pain: Treatment outcomes and compliance. Clinical Journal of Pain, 2, 159–173. [Google Scholar]
- Kabat-Zinn J, Massion AO, Kristeller J, Peterson LG, Fletcher KE, Pbert L, et al. (1992). Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. American Journal of Psychiatry, 149, 936–943. [DOI] [PubMed] [Google Scholar]
- Kalman D, Morissette SB, & George TP (2005). Co-morbidity of smoking in patients with psychiatric and substance use disorders. The American Journal on Addictions, 14, 106–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassel JD, Stroud LR, & Paronis CA (2003). Smoking, stress and negative affect: Correlation, causation, and context across stages of smoking. Psychological Bulletin, 129, 270–304. [DOI] [PubMed] [Google Scholar]
- Kelemen WL, & Kaighobadi F (2007). Expectancy and pharmacology influence the subjective effects of nicotine in a balanced-placebo design. Experimental and Clinical Psychopharmacology, 15(1), 93–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirsch I (1985). Self-efficacy and expectancy: Old wine with new labels. Journal of Personality and Social Psychology, 49(3), 824–830. [Google Scholar]
- Leyro TM, Zvolensky MJ, Vujanovic A, & Bernstein A (2008). Anxiety sensitivity and smoking motives and outcome expectancies among adult daily smokers: Replication and extension. Nicotine & Tobacco Research, 10, 985–994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM (1993). Skills training manual for treating borderline personality disorder In Linehan MM (Ed.), Diagnosis and treatment of mental disorders. New York, NY, US: Guilford Press. [Google Scholar]
- MacKillop J, & Anderson EJ (2007). Further psychometric validation of the mindful attention and awareness scale. Journal of Psychopathology and Behavioral Assessment, 29, 289–293. [Google Scholar]
- McLeish AC, Zvolensky MJ, & Bucossi MM (2007). Interaction between smoking rate and anxiety sensitivity: Relation to anticipatory anxiety and panic-relevant avoidance among daily smokers. Journal of Anxiety Disorders, 21(6), 849–859. [DOI] [PubMed] [Google Scholar]
- Morissette SB, Tull MT, Gulliver SB, Kamholz BW, & Zimering RT (2007). Anxiety, anxiety disorders, tobacco use, and nicotine: A critical review of interrelationships. Psychological Bulletin, 133(2), 245–272. [DOI] [PubMed] [Google Scholar]
- Niaura R, Goldstein M, & Abrams D (1991). A bioinformational systems perspective on tobacco dependence. British Journal of Addiction, 86(5), 593–597. [DOI] [PubMed] [Google Scholar]
- Novak A, Burgess ES, Clark M, Zvolensky MJ, & Brown RA (2003). Anxiety sensitivity, self-reported motives for alcohol and nicotine use and level of consumption. Journal of Anxiety Disorders, 17(2), 165–180. [DOI] [PubMed] [Google Scholar]
- O’Loughlin RE, & Zuckerman M (2008). Mindfulness as a moderator of the relationship between dehydroepiandrosterone and reported physical symptoms. Personality and Individual Differences, 119, 3–1202. [Google Scholar]
- Parks GA, Anderson BK, & Marlatt GA (2001). Relapse prevention therapy In Heather N, Peters TJ, & Stockwell T (Eds.), International handbook of alcohol dependence and problems (pp. 575–592). New York, NY, US: John Wiley & Sons Ltd. [Google Scholar]
- Patton GC, Carlin JB, Coffey C, Wolfe R, Hibbert M, & Bowes G (1998). Depression, anxiety, and smoking initiation: A prospective study over 3 years. American Journal of Public Health, 88, 1518–1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Payne TJ, Smith PO, McCracken LM, McSherry WC, & Antony M (1994). Assessing nicotidependence: A comparison of the Fagerstrom tolerance questionnaire (FTQ) with the Fagerstrom test for nicotine dependence (FTND) in a clinical sample. Addictive Behaviors, 19, 307–317. [DOI] [PubMed] [Google Scholar]
- Pomerleau CS, Carton SM, Lutzke ML, Flessland KA, & Pomerleau OF (1994). Reliability of the Fagerstrom tolerance questionnaire and the Fagerstrom test for nicotine dependence. Addictive Behaviors, 19, 33–39. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, & Grant M (1993). Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction, 88, 791–804. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Williams JMG, & Teasdale JD (2002). Mindful attention-based cognitive therapy for depression: A new approach to preventing relapse. New York, NY, US: Guilford Press. [Google Scholar]
- Shapiro SL, Oman D, Thoresen CE, Plante TG, & Flinders T (2008). Cultivating mindfulness: Effects on well-being. Journal of Clinical Psychology, 64, 840–862. [DOI] [PubMed] [Google Scholar]
- Shiffman S, & Wills TA (1985). Coping and cessation of substance use In Shiffman S & Wills TA (Eds.), Coping and substance use (pp. 221–240). New York: Academic. [Google Scholar]
- State of Vermont department of health. (2007). Retrieved June 30, 2007, from http://www.healthyvermonters.info/.
- Steuber TL, & Banner F (2006). Adolescent smoking and depression: Which comes first? Addictive Behaviors, 31, 133–136. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Karp J, Pihl RO, & Peterson RA (1997). Anxiety sensitivity and self-reported reasons for drug use. Journal of Substance Abuse, 9, 223–240. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Zvolensky MJ, & Eifert GH (2001). Negative-reinforcement drinking motives mediate the relation between anxiety sensitivity and increased drinking behavior. Personality and Individual Differences, 31, 157–171. [Google Scholar]
- Vujanovic AA, Zvolensky MJ, Bernstein A, Feldner M, & McLeish AC (2007). A test of the interactive effects of anxiety sensitivity and mindful attention in the prediction of anxious arousal, agoraphobic cognitions, and body vigilance. Behaviour Research and Therapy, 45, 1393–1400. [DOI] [PubMed] [Google Scholar]
- Walser RD, & Westrup D (2007). Acceptance & commitment therapy for the treatment of post-traumatic stress disorder and trauma-related problems: A practitioner’s guide to using mindful attention and acceptance strategies. Oakland, CA, US: New Harbinger Publications. [Google Scholar]
- Watson D, Weber K, Assenheimer JS, Clark LA, Strauss O, & McCormick J (1995). Testing a tripartite model I. Evaluating the convergent and discriminant validity of anxiety and depression symptom scales. Journal of Abnormal Psychology, 104, 3–14. [DOI] [PubMed] [Google Scholar]
- Wetter DW, Smith SS, Kenford SL, Jorenby DE, Fiore MC, Hurt RD, et al. (1994). Smoking outcome expectancies: Factor structure, predictive validity, and discriminant validity. Journal of Abnormal Psychology, 103(4), 801–811. [DOI] [PubMed] [Google Scholar]
- Ziedonis D, Hitsman B, Beckham J, Zvolensky MJ, Adler L, Audrain-McGovern J, et al. (2008). Tobacco use and cessation in psychiatric disorders: National institute of mental health (NIMH) report. Nicotine & Tobacco Research, 10, 1691–1715. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Bernstein A, Marshall EC, & Feldner MT (2006a). Panic attacks, panic disorder, and agoraphobia: Associations with substance use, abuse, and dependence. Current Psychiatry Reports, 8, 279–285. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Bonn-Miller MO, Bernstein A, & Marshall EC (2006b). Anxiety sensitivity and abstinence duration to smoking. Journal of Mental Health, 15, 659–670. [Google Scholar]
- Zvolensky MJ, Feldner MT, Leen-Feldner E, Bonn-Miller MO, McLeish AC, & Gregor K (2004a). Evaluating the role of anxiety sensitivity in smoking outcome expectancies among regular smokers. Cognitive Therapy and Research, 28, 473–486. [Google Scholar]
- Zvolensky MJ, Gibson LE, Vujanovic AA, Gregor K, Bernstein A, Kahler C, et al. (2008a). Impact of posttraumatic stress disorder on early smoking lapse and relapse during a self-guided quit attempt among community-recruited daily smokers. Nicotine & Tobacco Research, 10, 1415–1427. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Gonzalez A, Bonn-Miller MO, Bernstein A, & Goodwin RD (2008b). Negative reinforcement/negative affect reduction cigarette smoking outcome expectancies: Incremental validity for anxiety focused on bodily sensations and panic attack symptoms among daily smokers. Experimental and Clinical Psychopharmacology, 16(1), 66–76. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Leen-Feldner EW, Feldner MT, Bonn-Miller MO, Lejuez CW, Kahler CW, et al. (2004b). Emotional responding to biological challenge as a function of panic disorder and smoking. Journal of Anxiety Disorders, 18, 19–32. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Lejuez CW, Kahler CW, & Brown RA (2004c). Nonclinical panic attack history and smoking cessation: An initial examination. Addictive Behaviors, 29, 825–830. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Schmidt NB, & Stewart SH (2003). Panic disorder and smoking. Clinical Psychology: Science and Practice, 10, 29–51. [Google Scholar]
- Zvolensky MJ, Solomon SE, McLeish AC, Cassidy D, Bernstein A, Bowman CJ, et al. (2006c). Incremental validity of mindful-based attention in relation to the concurrent prediction of anxiety and depressive symptomatology and perceptions of health. Cognitive Behaviour Therapy, 35, 148–158. [DOI] [PubMed] [Google Scholar]