Abstract
Spinal epidural abscess is a rare disease that is less likely to occur in the cervical region. When it occurs here, cervical spondylodiscitis can develop. Surgical treatment is recommended because of possible life-threatening septic and neurological complications. We present a case of an 81-year-old man who suffered from right side paralysis and was subsequently diagnosed with a C4 to C7 epidural abscess. We utilized full endoscopic surgery for patient management. The traditional surgical methods for treating cervical epidural abscesses may cause spinal instability. There has only been one previous case report on the endoscopic-assisted method. Minimal invasive surgery by a full endoscopic method can be done with a small incision and is associated with minimal blood loss and muscle damage. This is the first report on cervical epidural abscess drainage utilization a full endoscopic method. We recommend this alternative minimally invasive method to manage cervical epidural abscess.
Keywords: Spinal epidural abscess, Endoscopic surgery, Cervical spondylodiscitis
INTRODUCTION
Spinal epidural abscess (SEA) is a spinal pyogenic infection that generally localizes between the spinal dura mater and vertebral periosteum [1].
Infections in the cervical spine are uncommon compared to lumbar and thoracic regions [2]. When SEA presents with neurologic deficits or becomes refractory to antibiotics, surgical intervention is indicated; surgical treatments reduce risk of motor dysfunction, paralysis, and death [3]. The standard operative method is laminectomy for spinal decompression with abscess evacuation [4]. However, SEA is not limited to 1 or 2 vertebral levels, as most extend to multiple levels. Minimal invasive techniques for managing extended SEA are of value for vertebral stabilization and older patients [5]. We report a case of cervical SEA treated by full endoscopic surgery.
CASE REPORT
This 81-year-old man with a history of type 2 diabetes mellitus, hypertension, and benign prostatic hyperplasia presented with a fever and right upper quadrant pain for 1 day and was admitted due to suspected cholangitis. Acute right limb weakness was noted on hospital admission day 2. Physical examination revealed decreased right-sided muscle power (grade 0 for the right upper limb and grade 1 for the right lower limb). Laboratory data indicated bacteremia (cause by Staphylococcus aureus) and bacteriuria (also caused by S. aureus). Empiric intravenous antibiotics with Cefoxitin 2,000 mg per 8 hours (second cephalosporin generation) had been prescribed since he was admitted. Spinal magnetic resonance imaging (MRI) revealed extradural hypersignal lesions 54 mm in length in the right posterior region of the spinal canal at level C4 to C7 (Fig. 1A, B). Because considering old age, underlying disease, multiple level involvement but limited on posterior right side, and there was no structure deformity and instability, we decided to performed minimally invasive surgery with full endoscopic surgery to manage the cervical epidural abscess.
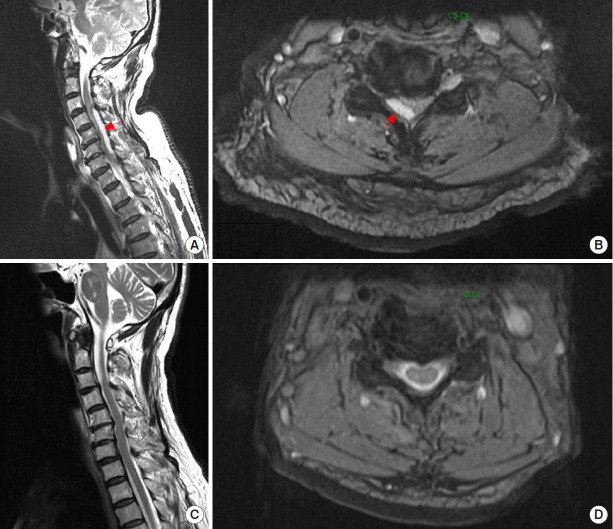
Fig. 1.
(A) Sagittal T2-weighted magnetic resonance imaging (MRI) showing a hypersignal lesion (red arrow), located posterior to spinal cord at the level of C4 to C7. (B) Axial T2-weighted MRI showing the lesion located right posterior epidural space at C5–6 level. Two-month lateral MRI follow-up sagittal T2-weighted MRI (C) showing no residual lesions or residual epidural abscess compressing the spinal cord at axial T2-weighted MRI (D).
1. Operative Method
The patient was positioned prone on a radiolucent table with Mayfield holder fixation while keeping the neck flexed (Fig. 2A). Operative access was determined based on anatomic landmarks under posteroanterior fluoroscopic guidance (Fig. 2B). After the skin entry point was determined at the 0.5-cm para-midline at the C5–6 level and the puncture incision was made, the dilator was inserted under posteroanterior and lateral fluoroscopic guidance. The working sleeve with a beveled opening was advanced toward the C5–6 level (the thickest level of the abscess) via the dilator and subsequently, the dilator was removed. The endoscope (SPINENDOS GmbH, Munich, Germany) was passed through the working sleeve (Fig. 3A). The operation was performed via the intraendoscopic working channel using alternating sets of instruments under full visual control and with continuous irrigation by gravity pressure. The irrigation pressure depended on gravity which was designed with 1,000-mL normal saline bag hanging on infusion stand and elevated 100 cm higher than operating table. To prevent from deteriorated myelopathy, intraoperative neuromonitoring was also equipped in this operation.
Fig. 2.
(A) The patient is placed in the prone position. His head is fixed with Mayfield holder fixation with his neck flexed as much as possible. (B) Localization with fluoroscopy (the lateral view and posteroanterior view) to confirm the level at C5–6 and the trajectory for percutaneous endoscopy.
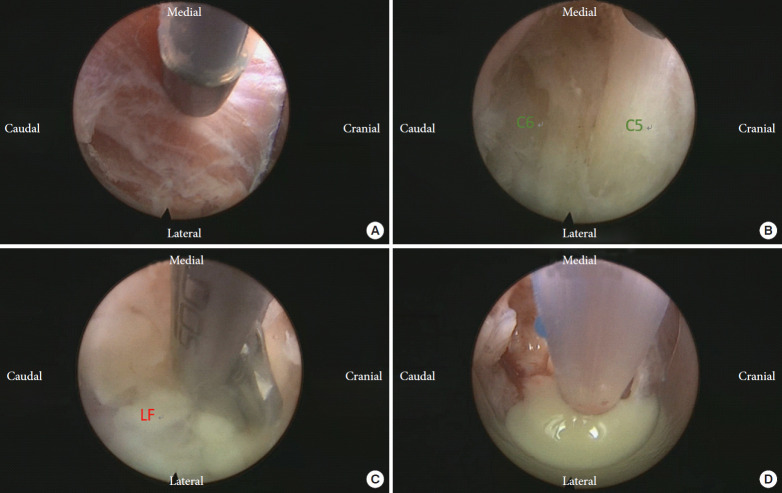
Fig. 3.
(A) A percutaneous endoscope was inserted at the level of C5–6 and was passed through the trapezius, splenius capitis, and semispinal capitus muscles. The muscular fibers were coagulated by endoscopic bipolar cautery and dissected by endoscopic scissor punch or cup forceps. (B) The interlaminar space between right C5 and C6 (V-point) was exposed after dissected muscles and periosteum. (C) Ligamentum flavum was removed by endoscopic scissor punch. (D) Yellowish pus was drained using an 8F. Nasogastric tube.
The V-point inter-laminal space between C5 and C6 was exposed (Fig. 3B). A laminotomy was performed over the right inferior lamina of C5 and a right superior lamina of C6 was performed by an endoscopic diamond burr (SPINENDOS GmbH).
As the ligamentum flavum was removed (Fig. 3C), turbid fluid was drained immediately. Hemostasis was completed by endoscopic bipolar cautery (SPINENDOS GmbH). An 8F nasogastric tube was inserted to collect the fluid (Fig. 3D). After the turbid fluid was drained, the abscess capsule was removed by a nerve hook. Active bleeding was then checked. A Hemovac drain (Zimmer Biomet, Swindon, UK) was placed under the endoscope (Fig. 4).
Fig. 4.
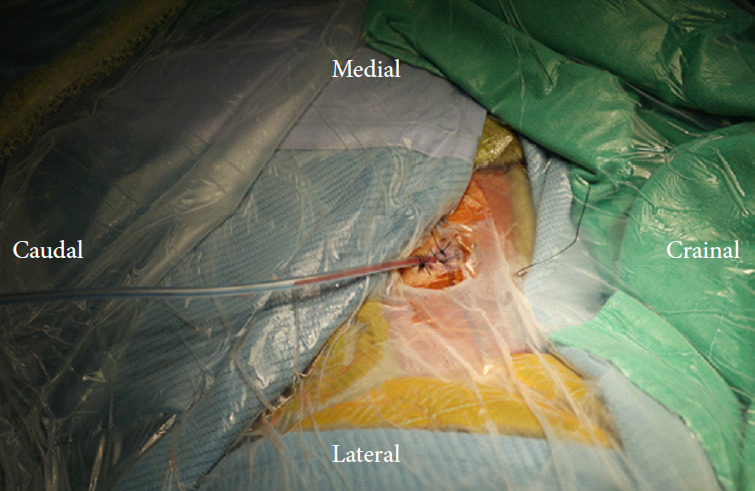
Drainage with a Hemovac was fixed and the wound was closed by 3-0 nylon sutures.
The wound was then closed with interrupted sutures of 3-0 nylon (1671H, Ethicon, Bridgewater, NJ). Operative time was 1 hour and 16 minutes. There was no significant change at somatosensory evoked potential and motor evoked potential intraoperatively.
The specimen was sent for pathological study.
2. Follow-Up
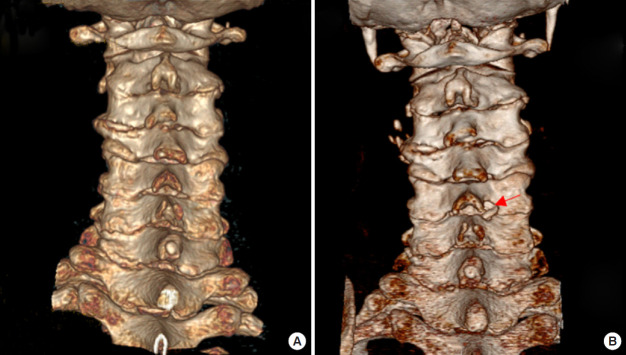
The patient’s right-sided muscle resumed to grade 3 on the day following the operation. However, the abscess was not cultured. A pathological report indicated inflammatory exudate with fibrin, neutrophils, and histiocytes as well as granulation tissue formation. The follow-up MRI was administered 2 months later which revealed no residual abscess and no cord compression (Fig. 1C, D). Preoperative and 6-month follow-up cervical spinal computed tomography disclosed the minimal laminotomy keyhole at the right lamina between C5 and C6 (Fig. 5A, B). The postoperative empiric antibiotics was adjusted to Oxacillin 2 g per 6 hours after consulting infection specialist for methicillin-resistant Staphylococcus aureus according to Staphylococcus aureus cultured in blood and urine. The duration of intravenous antibiotics had been used for 4 weeks and shifted to oral 3rd generation cephalosporins with Ceftibuten 200 mg per 12 hours. Oral antibiotics were discontinued until 9 weeks postoperatively due to resuming to the normal level of erythrocyte sedimentation rate and the improving follow-up MRI. At the 3-month outpatient follow-up, the patient’s right-sided muscle power remained at grade 3. Finally, the muscle power resumed to grade 5 in the postoperative 6 months.
Fig. 5.
(A) The coronal view of preoperative cervical spinal computed tomography (CT) reconstruction. (B) Six-month follow-up image reconstruction in cervical spinal CT. Compared to preoperative CT (A), a laminotomy keyhole is located between right-sided lamina of C5 and C6 (red arrow).
DISCUSSION
SEA is a surgical emergency due to possible neurologic deficits [6]. Cervical spine infections are less common than thoracic and lumbar localization; however, cervical infections are more often associated with epidural abscess formation [5].
Principles of SEA surgery are drainage of pus, cord decompression, and debridement of granulation tissue. Early decompression avoids possible ischemic change to the spinal cord due to vascular compression [7]. Roselli et al. [8] treated an anterior cervical epidural abscess by endoscopy-assisted posterior minimally invasive microsurgery using “keyhole microsurgery’’ and placed a ventricular catheter by endoscope for abscess drainage and irrigation.
Muzii et al. [2] performed microsurgery for a cervical epidural abscess with an anterior approach; a single-level discectomy with curettage of the disc plates at the level of the discitis and drainage of the epidural abscess via a silicone catheter was performed. Yang et al. [9] retrospectively assessed the advantage of percutaneous endoscopic lavage and drainage (PELD) for 21 patients with lumbar infectious spondylitis to help determine whether minimally invasive surgery (PELD) would suffice and whether open surgery could be avoided. Kang et al. [10] managed lumbar SEAs via biportal endoscopic surgery and obtained good results in 13 patients.
To the best of our knowledge, this is the first published case demonstrating a full endoscopic method to drain and decompress a cervical epidural abscess. Because of the risk and instability after a traditional laminectomy (with fusion added or not) for those old in age, minimally invasive surgery should also be considered. After reviewing the MRI, the well-defined border of the abscess without bony destruction or discitis enhanced our confidence in total drainage by a full endoscopic method.
The need for continuous irrigation by gravity pressure during the operation might dilute the bacterial count and lead to absence of the abscess culture. The intravenous empiric antibiotics, which are injected for days, also decreased the number of bacteria in a culture. This might become a disadvantage as it may prevent acquiring a specific culture for the following target antibiotics. Lin et al. [11] demonstrated a that the rate of cultured pathogens was 57% in 14 patients and Haaker et al. [12] found a 45% culture rate in 16 patients; both these studies selected patients who underwent percutaneous endoscopic discectomy or drainage due to thoracic or lumbar spondylodiscitis. However, we could recognize the obvious pyogenic abscess via the endoscope.
The advantages of endoscopic spinal surgery include minimal blood loss and small incisions. The smaller incision provides rapid postoperative recovery, early ambulation, and optimal cosmetic outcomes. Less muscle damage and limited bony deconstruction also provide an opportunity to wean the patient from mechanical ventilation, especially those in old age.
CONCLUSION
We performed minimally invasive surgery using a full endoscopic approach for drainage and decompression of a cervical SEA. This method can be an option for full endoscopic drainage, irrigation, and decompression.
Footnotes
The authors have nothing to disclose.
SUPPLEMENTARY MATERIALS
Supplementary video clip 1 can be found via https://doi.org/10.14245/ns.2040218.109.v.1.
REFERENCES
- 1.Arko L, 4th, Quach E, Nguyen V, et al. Medical and surgical management of spinal epidural abscess: a systematic review. Neurosurg Focus. 2014;37:E4. doi: 10.3171/2014.6.FOCUS14127. [DOI] [PubMed] [Google Scholar]
- 2.Muzii VF, Mariottini A, Zalaffi A, et al. Cervical spine epidural abscess: experience with microsurgical treatment in eight cases. J Neurosurg Spine. 2006;5:392–7. doi: 10.3171/spi.2006.5.5.392. [DOI] [PubMed] [Google Scholar]
- 3.Johnson KG. Spinal epidural abscess. Crit Care Nurs Clin North Am. 2013;25:389–97. doi: 10.1016/j.ccell.2013.04.002. [DOI] [PubMed] [Google Scholar]
- 4.Löhr M, Reithmeier T, Ernestus RI, et al. Spinal epidural abscess: prognostic factors and comparison of different surgical treatment strategies. Acta Neurochir (Wien) 2005;147:159–66. doi: 10.1007/s00701-004-0414-1. discussion 166. [DOI] [PubMed] [Google Scholar]
- 5.Panagiotopoulos V, Konstantinou D, Solomou E, et al. Extended cervicolumbar spinal epidural abscess associated with paraparesis successfully decompressed using a minimally invasive technique. Spine (Phila Pa 1976) 2004;29:E300–3. doi: 10.1097/01.brs.0000131215.46119.dd. [DOI] [PubMed] [Google Scholar]
- 6.Al-Hourani K, Al-Aref R, Mesfin A. Upper cervical epidural abscess in clinical practice: diagnosis and management. Global Spine J. 2016;6:383–93. doi: 10.1055/s-0035-1565260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Feldenzer JA, McKeever PE, Schaberg DR, et al. The pathogenesis of spinal epidural abscess: microangiographic studies in an experimental model. J Neurosurg. 1988;69:110–4. doi: 10.3171/jns.1988.69.1.0110. [DOI] [PubMed] [Google Scholar]
- 8.Roselli R, Iacoangeli M, Pompucci A, et al. Anterior cervical epidural abscess treated by endoscopy-assisted minimally invasive microsurgery via posterior approach. Minim Invasive Neurosurg. 1998;41:161–5. doi: 10.1055/s-2008-1052034. [DOI] [PubMed] [Google Scholar]
- 9.Yang SC, Chen WJ, Chen HS, et al. Extended indications of percutaneous endoscopic lavage and drainage for the treatment of lumbar infectious spondylitis. Eur Spine J. 2014;23:846–53. doi: 10.1007/s00586-013-3157-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kang T, Park SY, Lee SH, et al. Spinal epidural abscess successfully treated with biportal endoscopic spinal surgery. Medicine (Baltimore) 2019;98:e18231. doi: 10.1097/MD.0000000000018231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lin GX, Kim JS, Sharma S, et al. Full endoscopic discectomy, debridement, and drainage for high-risk patients with spondylodiscitis. World Neurosurg. 2019;127:e202–11. doi: 10.1016/j.wneu.2019.02.206. [DOI] [PubMed] [Google Scholar]
- 12.Haaker RG, Senkal M, Kielich T, et al. Percutaneous lumbar discectomy in the treatment of lumbar discitis. Eur Spine J. 1997;6:98–101. doi: 10.1007/BF01358740. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.