Abstract
For all the spine surgeons, thoracic disc herniations (TDHs) entrust a real challenge in terms of patient diagnosis, proper selection, surgical technique, and potential adverse events. TDHs are relatively uncommon compared to the lumbar and cervical levels. Literature reports a variable prevalence of TDHs around 6% to 40%, but less than 1% of all disk herniations are symptomatic TDHs, evidencing as a relatively unusual condition. Nowadays, transforaminal endoscopic thoracic discectomy (TETD) has been implemented as an alternative to classic open procedures with results that are as good as and, in some situations, better than those in traditional discectomy. However, the surgeon must be familiar with endoscopic lumbar spine surgery before opting to perform a TETD, considering that the learning curve is much harder. We describe all the steps and safety considerations during TETD based on the anatomic differences compared to lumbar endoscopic procedures. TETD is an effective and safe method that yields more benefits, provides a direct route to the lesion with less morbidity, and is performed in a minimally invasive way. Many severe complications related to the thoracic region could be avoided having the proper knowledge, adequate technique, and safety routes and considerations.
Keywords: Endoscopic thoracic discectomy, Complications, Technique
INTRODUCTION
For all the spine surgeons, thoracic disc herniations (TDHs) entrust a real challenge in terms of patient diagnosis, proper selection, surgical technique, and potential adverse events. Percutaneous endoscopic thoracic discectomy is recently renamed as transforaminal endoscopic thoracic discectomy (TETD) by AO (Arbeitsgemeinschaft für Osteosynthesefragen; German for “Association for the Study of Internal Fixation”) minimally invasive task force.
Nowadays, TETD has been implemented as an alternative to classic open procedures with results that are as good as and, in some situations, better than those in traditional open discectomy. TETD is routinely performed under local sedation, and anesthesia, postoperative pain is very minimal, paraspinal muscles ,and thoracic structures are well preserved. The risk of epidural scar formation and instability during the postoperative period, can be minimized [1,2]. However, the surgeon must be familiar with endoscopic lumbar spine surgery before deciding to perform a TETD since the learning curve is harder compared to other endoscopic procedures.
EPIDEMIOLOGY AND CLINICAL FEATURES
TDHs are relatively uncommon compared to the lumbar and cervical levels. Literature reports a variable prevalence of TDHs around 6% to 40%, but less than 1% of all disk herniations are symptomatic TDHs, evidencing as a relatively unusual condition [3,4]. It is more common between the fourth and sixth decades of life and tends to occur more frequently in males than females [3]. The lower thoracic spine is the most commonly affected, being T8–9, the most affected level. In the majority of cases, TDHs are located centrally (around 66%), and the rest are located in paramedian fashion (around 33%) [3]. Greater number of such cases are asymptomatic, and a very few parts require surgical management [3].
One of the unique concerns and features of TDH is its high frequency of calcification or even ossification. Quint et al. [5], in a study of 168 patients with TDHs, found that 58% were soft herniations and 42% calcified herniations. The calcification mechanism has not been elucidated yet. In singular cases, it is reported that calcified herniations are an extension of a calcified nucleus pulposus [6].
The debut of TDHs varies according to the affected level. In most of the cases, thoracic back pain is the main complaint. Neck pain may be seen in some cases affecting levels above T4–5. Myelopathic symptoms and girdle pain might be present in cases of cord and root compression, respectively. Occasionally, the presentation might be a combination of motor deficit in lower limbs, ataxia, paresthesias, and bladder and bowel symptoms [3].
SURGICAL INDICATIONS AND CONTRAINDICATIONS
The most important indication for TETD is the soft TDH confirmed by computed tomography (CT) and magnetic resonance imaging (MRI). The proper level is confirmed by clinical findings, images and with the help, in some cases, of selective root blocks. These findings should be accompanied by back pain (axial type) with or without radicular pain, including that may include thoracolumbar pain, anterior radiating chest pain, interscapular pain, and intercostal pain [2]. Also, a mild degree of myelopathy due to soft disk herniation without a favorable response to conservative therapy [1,4,5,7,8].
On the other hand, TETD is contraindicated in patients with hard or calcified disc herniation, thoracic ossification of the posterior longitudinal ligament and severe disk narrowing, as well as, severe cord compression and documentation of acute or progressive degenerative spinal cord disease.
SURGICAL CONSIDERATIONS AND ENDOSCOPIC PROCEDURE
1. Anatomical Review
An exhaustive understanding of spinal anatomy is imperative for global evaluation and conscious treatment of a patient with TDH. The relative rigidity of the thoracic cage decreases flexion, extension, and rotation movements compared with other segments of the spine. This fact is, fairly, the main cause of the low incidence of symptomatic TDH [1,4].
Several considerations of the thoracic spinal anatomy must be taken into consideration before opting to perform an endoscopic procedure: the thoracic vertebrae size increases running down the spine, the spinal canal has less free space for the spinal cord than cervical and lumbar regions, and the foramen is larger and more oval from cephalic to caudal direction, in a very similar way compared to the upper lumbar spine.
The pedicles are oriented dorsally from the vertebral bodies to the laminae. The superior articular facet is oval, practically flat, and it is directed dorsally upwards, arising at the pedicle and lamina junction. Similarly, the inferior articular process is oriented in a medially and downward fashion and constitutes the facet joint in association with the superior articulate process (SAP) of the inferior vertebra. This junction provides an important landmark and docking place for facet releasing procedures, along with transpedicular discectomies. The joint line is also part of the intervertebral foramen (dorsal wall) and gives access to the exiting nerve root and lateral thecal sac. Due to thoracic foramen is much smaller than the lumbar foramen; a widening procedure is usually required to introduce the cannula when we execute a transforaminal approach for a TDH. Only when we remove the costal process of rib heads; the pedicles and the total extension intervertebral foramen could be completely identified [4,9].
The costotransverse joint works as an important landmark for far-lateral discectomies; as we explained before, most often, this joint needs to be drilled to access, laterally, into the intervertebral disc. In lateral view, the rib head partially covers the transverse process. The intercostal and segmental vessels run around the vertebral body into its middle part (concavity) and provide an important landmark. In anterolateral discectomy procedures, those vessels do not need to be divided. However, in corpectomy procedures, they should be ligated at the beginning of the procedure.
Also, the intradural component at thoracic levels differs from others because it has many rootlets and less amount of cerebrospinal fluid (CSF), that plays an important role as a buffer, making this region more susceptible to heat injury in relation with the use of laser (Fig. 1) [1,2].
Fig. 1.
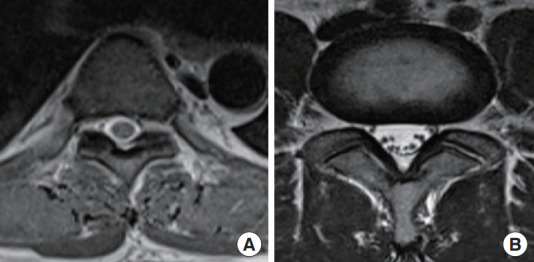
Magnetic resonance imaging pictures comparing the thoracic vertebra (A) and lumbar vertebra (B). Note the difference in size and the distribution of the rootlets and the amount of cerebrospinal fluid, which makes thoracic levels more susceptible to heat injury (less buffer).
2. Preoperative Planning, Position, and Anesthesia
For preoperative planning, to determine if the patient is a candidate for a percutaneous thoracic procedure and also, to design the needle trajectory CT scan and MRI are always required. These images are used to calculate the proper skin entry point. The desired trajectory is determined by extending a line from the mid-pedicular annulus to the lateral margin of the facet and up to the skin surface, taking as a point of reference the posterior border of the rib head (Fig. 2) [2].
Fig. 2.

Skin entry point and safe route of a needle. Measurements on computed tomography scan to determine skin entry point considering anatomical marks such posterior border of rib, the facet, and the midpedicular line.
The patient is placed in a prone position on a radiolucent operating table, the surgeon facing the affected side, and the arms above the patient as well as the endoscopic and fluoroscopic monitors are positioned in front of the surgeon to simplify viewing.
Local anesthesia with lidocaine 1% is used to infiltrate the pathway from the skin to the facet. Conscious sedation with midazolam (dose of 0.05 mg/kg intramuscularly 30 minutes before surgery followed by another dose intravenously if required), and fentanyl allows continuous feedback from the patient during the entire procedure avoiding any potential injury to neural structures.
3. Needle Insertion Techniques
As we mentioned before, the appropriate operative level must be precisely located using lateral and anteroposterior (AP) fluoroscopy and extrapolating the measures obtained in MRI/CT. One of the first steps is counting the level from the sacrum or C1 (requiring continuous fluoroscopic guidance). Nowadays, however, there are many methods for aiding the surgeon to locate more accurately the proper level in thoracic spine [10-12].
Another important fact: since the thoracic disk is more concave than the lumbar disks, lumbar fluoroscopic landmarks cannot be used for thoracic disks (Fig. 1). Because of this concavity, TDHs can only be addressed through the foraminal region. Deeper approaches have the risk of dural penetration and lesion.
The skin entry point is determined with a preoperative image based on an imaginary line projected toward the skin from the target area (between the rib and facet) and using the posterior rib edge as the limit and protection of the thoracic cavity. Routinely, the skin entry point is around 7 to 9 cm lateral to the midline (Fig. 2), and it is more separated from midline due to inclination degree based on the posterior rib edge. The path between the rib head and the thoracic facet is the safest route for the needle into the thoracic disk [1,4,7,8,13] (Fig. 2).
For larger patients and to reduce the manipulation of the spinal cord, a more lateral approach is needed during discectomy. Also, since the pleura is located anterior to the ribs, we always must be careful to keep the needle posterior to the rib head [2]. Using oblique views can help to identify and confirm the safe placement of needle: we use the principle of coaxial view, in which the needle orientation and C-arm orientation are the same. In that case, the needle position has to be between the rib head and the pedicle shadow (Fig. 3). Figs. 3 and 4 adequately detail the precise position in this projection: the needle must be medial to the edge of the head of the rib, superior and slightly lateral to the midline of the pedicle and centered on the discligament complex. Also, the oblique angle is related to the angle obtained in the preoperative planning; thus, an adequate coaxial view might be achieved with the C-arm. Otherwise, any other position could lead to an adverse event; additionally, with this projection, we can minimize the risk of dural puncture as well as thoracic and vascular complications. Concluding this step, the final position of needle ought to be located at the midpedicular line and posterior vertebral line on the AP and lateral view (Fig. 5) [1,4].
Fig. 3.
(A) C-arm oblique orientation using a coaxial method for needle placement. The oblique angle can be obtained according to the preoperative planning. (B) Zoomed image of oblique projection and its relationship with the rib head (blue dotted circle) and the pedicle (white dotted circle). The zone marked in yellow is the safest zone for docking the needle and always has to be centered in the disc complex. (C) C-arm oblique projection of the previous image. Note the safety point in between the rib head and the shadow of the pedicle, as described in panel B.
Fig. 4.
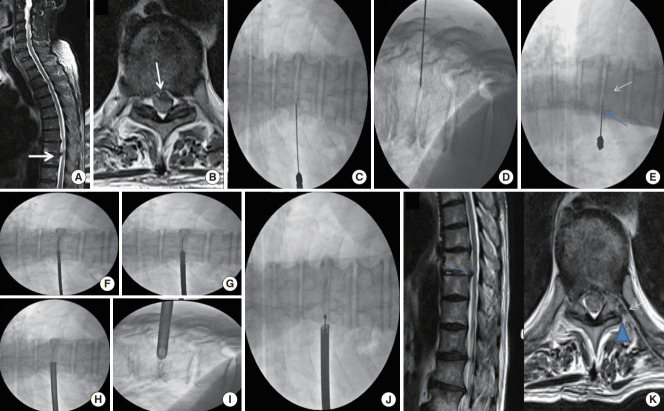
Case example: a 67-year-old male patient presented with dorsal pain (visual analogue scale [VAS] 6/10) radiated to the left leg (VAS 8/10) and associated paresthesias. Initial magnetic resonance imaging (MRI) sagittal (A) and axial views (B) showed a central to left disc herniation at T9–10 (white arrows). Proper and safe needle placement is shown in C-arm anteroposterior (C), lateral (D), and oblique projections (E), in this latter projection we pointed out the needle’s accurate target between the rib head (blue arrow) and the pedicle (white arrow). We used these safe projections to perform foraminoplasty with manual reamers (F, G) and to dock the working sleeve (H, I). During the procedure, we needed to extend the initial foraminoplasty using endoscopic burr (J). Postoperative MRI confirmed findings of disc herniation removal and endoscopic left foraminoplasty (K; the blue arrow shows the level operated in sagittal view; white arrow indicates a postoperative hemovac drain and the blue arrowhead indicates left foraminoplasty).
Fig. 5.
(A) C-arm anteroposterior view showing the needle tip placed at the midpedicular line. (B) Lateral view showing the needle tip in the posterior vertebral line.
Once the needle is confirmed at this level, we proceed to advance it a little further (inside the disc), and a mixture of 2–3 mL of indigo carmine and radiopaque dye is used to perform the discography to stain the herniated fragment.
4. Obturator and Working Channel Positioning
A blunt-tipped guide wire (0.8 mm) is placed through the needle, and, consequently, the needle is withdrawn. A skin incision of 7–10 mm in length is made, and the subcutaneous tract is developed by passing serial dilators of increasing size (from 1 to 5 mm) in a gentle twisting motion. After removing the dilators, a blunt-tapered obturator is passed over the guidewire by a gentle twisting motion again and using the fluoroscopic guidance, until attaining the posterolateral margin of the facet (Fig. 6).
Fig. 6.
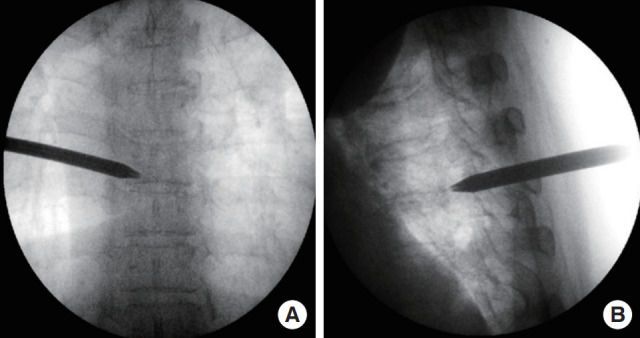
(A, B) The obturator is shown, and it is advanced over the guidewire.
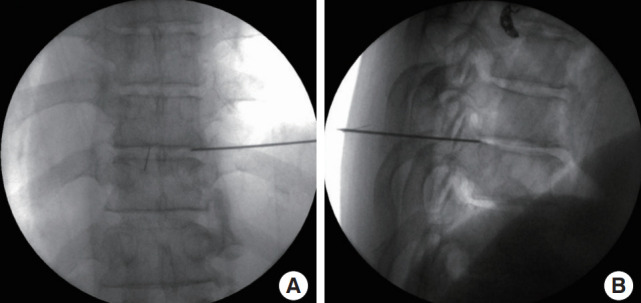
Then, to accommodate the working cannula, the path is further dilated until the beveled opening is facing medially and inferiorly, and the cannula’s tip compresses the annulus just lateral to the mid-pedicular line. After reaching this final position, the endoscope is passed over (Fig. 7).
Fig. 7.
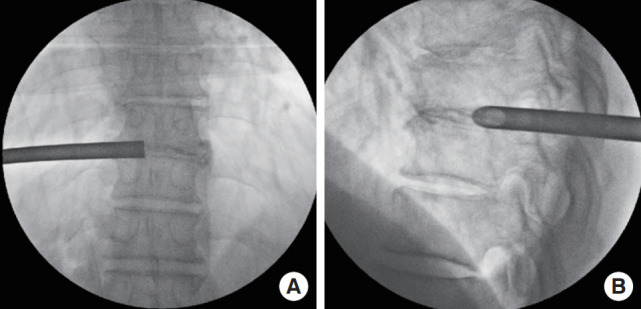
Final working channel positioning on anteroposterior (A) and lateral views (B).
5. Endoscopic Procedure
To prevent unintended entry into the spinal canal with potential damage to neural structures, it is mandatory to keep the right orientation.
After the endoscope is placed, the soft tissue obstructing the view is removed with the aid of radiofrequency or laser. The exposure should encompass the proximal transverse process and lateral facet. To reduce the manipulation of the spinal cord laterally, the position of the instruments must be essential.
At the upper thoracic levels, foraminoplasty procedure might be required to widen the foramen and to facilitate the insertion of the cannula. Technically, the lateral aspect of the superior facet (SAP)can be removed by using a long, tapered, high-speed drill or manual reamers at the beginning of the procedure [2,14] (Figs. 4 and 8).
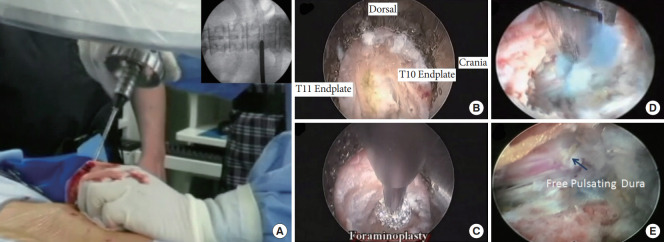
Fig. 8.
Endoscopic procedure for transforaminal endoscopic thoracic discectomy. (A) The ventral and lateral aspect of the superior facet is cut using progressive round manual cutters (reamers). C-arm controlled is showed in the right corner. Initially, this maneuver will help us to enlarge the foramen. (B) Using the endoscope, we can identify anatomic marks for orientation. (C) The ventral and lateral border of the superior articular process is drilled again to allow better visualization of structures. (D) After dissection and correct identification of anatomical marks, we perform a discectomy. (E) At the end of the procedure, we can observe the dural sac moving freely
Once the disk space is visualized, we perform the annulotomy. Initially, we create a space in the posterior subannular region using holmium: yttrium-aluminum-garnet laser ablation.
Once we finished the initial decompression using forceps, the cannula is tilted posteriorly to expose the foraminal epidural space, and then the remaining extruded disc could be removed with the aid of laser and forceps. At the end of the procedure, one of the signs that help us to confirm the proper decompression is the free movement of the thecal sac by changing the irrigation pressure.
A sterile strip was applied on the small wound, after a single subcutaneous suture.
DISCUSSION
With the advancement and improvement of diagnostic techniques, currently, the findings of thoracic herniations that agree or explain the symptoms of the patients have presented a significant increase in its incidence and prevalence.
Unfortunately, many of the techniques described for the management of symptomatic herniated discs require a great approach in open surgery, often generating significant morbidity and, in some unfortunate cases, associated mortality.
Minimally invasive spine surgery, in particular, thoracic spine endoscopy, has become more popular due to the possibility of managing cases with local anesthesia and even on an outpatient basis, reducing complications and adequately treating pathology.
Proper and previous training and experience with open thoracic surgery and familiarity with percutaneous spinal endoscopic procedures (lumbar endoscopic procedures, etc.) should be the base of this procedure. Moreover, conscious surgical planning and deep detailing of the diagnosis can surely prevent undesirable complications.
Currently, there are no articles in the literature that report complications or adverse events in TETD. Fessler and Sturgill [15] and McCormick et al. [16], have published in their respective works, the most frequently observed complications in open surgery for TDH, both for anterior and posterior approaches [17]. Some of these complications can also be extrapolated from thoracic open procedures and from lumbar endoscopic procedures as well.
We should always remember that surgical treatment of TDHs may present potentially devastating complications: the thoracic spinal cord has special features concerning its vascular supply. The upper thoracic region has a watershed region of the spinal vascular supply and might be susceptible to ischemic complications [2]. In the thoracic spine, root injury does not carry the same morbidity and neurological deficit that it does in other regions (cervical or lumbar); on the other hand, injury to the thoracic cord with its particular blood supply can impart a patient severe and disabling outcomes.
Dural tear and nerve injury have been reported with an incidence of 0% to 5.6% and 0% to 1.5%, respectively, in lumbar endoscopic procedures [18-20]. The former can go unnoticed, presenting symptoms of intracranial hypotension in the postoperative period. Tears noted during the surgical procedure can be managed with hard patches and packing, since most of them are small defects (< 5 mm). Major defects may be refractory to management and may require future open reoperations for definitive management. Nerve injury could be monitored in a much more efficient way with the patient awake and managed with local anesthesia during the whole procedure.
Knowing the anatomical characteristics that differentiate the thoracic segments from the whole spine and also analyzing the anatomical features of each patient as well as proper surgical planning are some key points to avoid this kind of complication.
Vascular complications such as puncture of the aorta or vena cava can be fatal for the patient [1]. These findings for endoscopic procedures have not been reported in the literature to date. However, findings of important bleeding due to radicular or segmental arteries have been reported in lumbar endoscopic procedures [21-23]. The hemothorax secondary to that arterial puncture (in thoracic cases: intercostal or segmental artery) is the most feared complication and depending on the size, and clinical compromise may require observation or surgical management.
Pulmonary complications, in descending order, are the second most worrisome after vascular complications. McCormick et al. [17] describe that for open procedures, pneumonia, atelectasis, and pleural effusions have been described. Also, inadvertent pleural tears in posterior approaches and extracavitary lateral approaches occur in approximately 13% of cases.
The strategies employed in the prevention of those most feared complications are related, mainly, to the needle placement at the beginning of the procedure. At the skin entry point of the needle, the posterior aspect of the rib, corresponding to the segment to be treated, can be used as a “shield” to protect the structures of the chest from inadvertent entry by the surgeon and thus, guide the needle to the intervertebral foramen. Also, the oblique projection will provide safety to continue the procedure. Hence, the needle, as we explained previously, has to be positioned medial to the rib head and superior and lateral concerning mid pedicular line and centered in the disc complex.
Incomplete decompression or residual fragment is defined as the clinical persistence of symptoms in the 2 weeks following the postoperative period, without a period of relief of symptoms and, also, with fragment findings in control images [24]. This has been described by Dickman et al. [25] in 15 patients in open surgery: most of the cases due to the absence of a correct visualization of the fragment. In endoscopic procedures, it can also occur due to said lack of visualization of the entire fragment or due to the surgeon’s fear of the surrounding nerve structures that prevent the deepening of the dissection and the position of the working canal.
The heat injury related to the use of laser or radiofrequency is a concern for the surgeon and that mainly occurs in the thoracic region, due to an anatomical fact: the higher density of the spinal cord compared to the multiple roots in the lumbar region. This means that the amount of CSF, which acts as a buffer against heat, is less in the thoracic segments, generating a greater probability of the occurrence of this type of injury.
The infection rate in these kinds of procedures is very low compared with traditional open procedures [20]. However, some advice could be given in this apart: besides the prophylaxis with proper antibiotics and according to the experience of the senior author, the saline solution mixed with antibiotics (aminoglycosides) during the whole procedure could help to prevent infections. And second, once the needle has entered into the skin, any need to withdraw and reposition the needle to change the trajectory or to perform another new skin puncture should be accompanied with the change of the needle for a new one. Thus, contamination and inoculation of microorganisms into the thoracic spine are prevented.
In summary, extrapolating the various complications presented in open surgeries and also considering the most frequent complications in lumbar endoscopic approaches, the authors consider the following as the most frequent and feared complications: vascular and pulmonary complications when the position of the needle locates more towards lateral, in oblique projections. Oppositely, complications such as nerve injuries, intercostal neuralgias, and dural tears might happen when the needle moves very medially, in the same projections. Other complications such as recurrence of herniations, residual fragments of discs, and heat injury might also occur; the latter, more frequently related to the use of laser and radiofrequency. Strategies and advice were given during the discussion to prevent such complications.
CONCLUSION
TETD is an effective and safe method that yields more benefits, provides a direct route to the lesion with less morbidity, and is performed in a minimally invasive way. Many severe complications related to the thoracic region could be avoided having the proper knowledge, adequate technique, and safety routes and considerations.
Footnotes
The authors have nothing to disclose.
SUPPLEMENTARY MATERIALS
Supplementary video clip 1 can be found via https://doi.org/10.14245/ns.2040250.125.v.1.
REFERENCES
- 1.Choi G, Pophale CS, Patel B, et al. Endoscopic spine surgery. J Korean Neurosurg Soc. 2017;60:485–97. doi: 10.3340/jkns.2017.0203.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim DH, Choi G, Lee SH. Endoscopic spine procedures. New York: Thieme Medical Publishers; 2011. [Google Scholar]
- 3.Sharma SB, Kim JS. A review of minimally invasive surgical techniques for the management of thoracic disc herniations. Neurospine. 2019;16:24–33. doi: 10.14245/ns.1938014.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choi KY, Eun SS, Lee SH, et al. Percutaneous endoscopic thoracic discectomy; transforaminal approach. Minim Invasive Neurosurg. 2010;53:25–8. doi: 10.1055/s-0029-1246159. [DOI] [PubMed] [Google Scholar]
- 5.Quint U, Bordon G, Preissl I, et al. Thoracoscopic treatment for single level symptomatic thoracic disc herniation: a prospective followed cohort study in a group of 167 consecutive cases. Eur Spine J. 2012;21:637–45. doi: 10.1007/s00586-011-2103-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gong M, Liu G, Guan Q, et al. Surgery for giant calcified herniated thoracic discs: a systematic review. World Neurosurg. 2018;118:109–17. doi: 10.1016/j.wneu.2018.06.232. [DOI] [PubMed] [Google Scholar]
- 7.Bae J, Chachan S, Shin SH, et al. Percutaneous endoscopic thoracic discectomy in the upper and midthoracic spine: a technical note. Neurospine. 2019;16:148–53. doi: 10.14245/ns.1836260.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shen J. Fully endoscopic transforaminal discectomy under local anesthesia for thoracic disc herniations: a case series. J Spine. 2018;7:013. doi: 10.4172/2165-7939.s7-013. [DOI] [Google Scholar]
- 9.Kim JS, Lee JH, Ahn Y. Endoscopic procedures on the spine. Singapore: Springer; 2020. [DOI] [Google Scholar]
- 10.Binning MJ, Schmidt MH. Percutaneous placement of radiopaque markers at the pedicle of interest for preoperative localization of thoracic spine level. Spine (Phila Pa 1976) 2010;35:1821–5. doi: 10.1097/BRS.0b013e3181c90bdf. [DOI] [PubMed] [Google Scholar]
- 11.Anaizi AN, Kalhorn C, McCullough M, et al. Thoracic spine localization using preoperative placement of fiducial markers and subsequent CT. A technical report. J Neurol Surg A Cent Eur Neurosurg. 2015;76:66–71. doi: 10.1055/s-0034-1371512. [DOI] [PubMed] [Google Scholar]
- 12.Upadhyaya CD, Wu JC, Chin CT, et al. Avoidance of wrong-level thoracic spine surgery: intraoperative localization with preoperative percutaneous fiducial screw placement. J Neurosurg Spine. 2012;16:280–4. doi: 10.3171/2011.3.SPINE10445. [DOI] [PubMed] [Google Scholar]
- 13.Nie HF, Liu KX. Endoscopic transforaminal thoracic foraminotomy and discectomy for the treatment of thoracic disc herniation. Minim Invasive Surg. 2013;2013:264105. doi: 10.1155/2013/264105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wagner R, Telfeian AE, Iprenburg M, et al. Transforaminal endoscopic foraminoplasty and discectomy for the treatment of a thoracic disc herniation. World Neurosurg. 2016;90:194–8. doi: 10.1016/j.wneu.2016.02.086. [DOI] [PubMed] [Google Scholar]
- 15.Fessler RG, Sturgill M. Review: complications of surgery for thoracic disc disease. Surg Neurol. 1998;49:609–18. doi: 10.1016/s0090-3019(97)00434-5. [DOI] [PubMed] [Google Scholar]
- 16.McCormick WE, Will SF, Benzel EC. Surgery for thoracic disc disease. Complication avoidance: overview and management. Neurosurg Focus. 2000;9:e13. doi: 10.3171/foc.2000.9.4.13. [DOI] [PubMed] [Google Scholar]
- 17.Jain A, Menga EN, Hassanzadeh H, et al. Thoracic disc disorders with myelopathy: treatment trends, patient characteristics, and complications. Spine (Phila Pa 1976) 2014;39:E1233–8. doi: 10.1097/BRS.0000000000000511. [DOI] [PubMed] [Google Scholar]
- 18.Chen X, Chamoli U, Lapkin S, et al. Complication rates of different discectomy techniques for the treatment of lumbar disc herniation: a network meta-analysis. Eur Spine J. 2019;28:2588–601. doi: 10.1007/s00586-019-06142-7. [DOI] [PubMed] [Google Scholar]
- 19.Xie TH, Zeng JC, Li ZH, et al. Complications of lumbar disc herniation following full-endoscopic interlaminar lumbar discectomy: a large, single-center, retrospective study. Pain Physician. 2017;20:E379–87. [PubMed] [Google Scholar]
- 20.Shriver MF, Xie JJ, Tye EY, et al. Lumbar microdiscectomy complication rates: a systematic review and meta-analysis. Neurosurg Focus. 2015;39:E6. doi: 10.3171/2015.7.FOCUS15281. [DOI] [PubMed] [Google Scholar]
- 21.Sen RD, White-Dzuro G, Ruzevick J, et al. Intra- and perioperative complications associated with endoscopic spine surgery: a multi-institutional study. World Neurosurg. 2018;120:e1054–60. doi: 10.1016/j.wneu.2018.09.009. [DOI] [PubMed] [Google Scholar]
- 22.Wang Y, Ai P, Zhan G, et al. Lumbar artery injury during transforaminal percutaneous endoscopic lumbar discectomy: successful treatment by emergent transcatheter arterial embolization. Ann Vasc Surg. 2018;53:267.e11–267.e14. doi: 10.1016/j.avsg.2018.05.032. [DOI] [PubMed] [Google Scholar]
- 23.Bae DH, Eun SS, Lee SH, et al. Two cases of retroperitoneal hematoma after transforaminal percutaneous endoscopic lumbar discectomy. Interdiscip Neurosurg. 2020;20:100649. doi: 10.1016/j.inat.2019.100649. [DOI] [Google Scholar]
- 24.Lee SH, Kang BU, Ahn Y, et al. Operative failure of percutaneous endoscopic lumbar discectomy: a radiologic analysis of 55 cases. Spine (Phila Pa 1976) 2006;31:E285–90. [PubMed] [Google Scholar]
- 25.Dickman CA, Rosenthal D, Regan JJ. Reoperation for herniated thoracic discs. J Neurosurg. 1999;91(2 Suppl):157–62. doi: 10.3171/spi.1999.91.2.0157. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.