Objective
In response to the coronavirus disease 2019 (COVID-19) pandemic, and to control viral spread among patients and staff, delivery of healthcare rapidly adjusted by reducing in-person patient interactions.1 , 2 Worldwide and for a variety of specialties, healthcare protocols were tailored to allow for expansion of telehealth services. For vulnerable populations, such as pregnant women with opioid use disorder (OUD), this shift in practice represented an abrupt transition and compounded the significant barriers to care that already exist for this population.3 , 4 Here, we report our experience with implementation of telehealth services for a cohort of pregnant women with OUD.
Study Design
In our practice, maternal fetal medicine and addiction specialists care for pregnant women with OUD in a colocated office-based outpatient program. A major component of this program is weekly in-person psychotherapeutic/psychoeducational/supportive interventions group therapy. As part of our response to the COVID-19 pandemic, weekly group therapy services transitioned from in-person to virtual meetings between April 1, 2020 and May 26, 2020 to reduce potential COVID-19 exposure among patients and to comply with social distancing as recommended by the Centers for Disease Control and Prevention (CDC). Patients who received individual counseling sessions were also transitioned to virtual sessions. The group prenatal care model transitioned to individual care visits based on a department-developed algorithm for providing prenatal care during the COVID-19 pandemic, considering the patient’s gestational age and acuity of additional medical complications. Visits to obtain urine drug screens (UDS) and prescriptions for medication-assisted therapy (MAT) remained in-person and were adjusted from weekly to biweekly visits on the basis of patient compliance history and availability.
During the reopening phase (after May 27, 2020), a combined approach was adapted in which patients chose either in-person (limited to <10 patients per session in compliance with CDC recommendations for social distancing) or virtual group sessions. Patients attending group care visits in person received a temperature and symptom screen before arrival; visitors, including children, were not allowed to accompany the patient to any outpatient prenatal visit or ultrasound. For this study, patient data on group attendance, UDS results, emergency department (ED) and/or obstetrical triage visits, at-home assaults, overdoses, uptitration of MAT, and opiate craving scores were collected. The opiate craving score is based on a 10-point Likert craving score composed of 3 questions: (1) How much do you currently crave opiates? (2) In the past week, please rate how strong your desire to use opiates has been when something in the environment has reminded you of opiates. (3) Imagine yourself in the environment in which you previously used opiates. If you were in this environment today and if it were that time of day that you typically used opiates, what is the likelihood that you would use opiates today?
The Impact of Event Scale-Revised (IES-R) was administered after resumption of in-person groups to assess distress because of the pandemic. Data were collected by obstetrical physicians providing care within the OUD pregnancy colocated clinic. After verification by the authors, these variables were then compared among 3 periods representing the immediate pre- and postperiods as well as the virtual group therapy–only period.
To meet the inclusion criteria for this analysis, a patient should have enrolled in the obstetrical OUD treatment program with stable MAT dosing 4 weeks before the first case of COVID-19 in Ohio and continued prenatal care through virtual-only and combined in-person and virtual care periods. Postpartum participants, those entering care after the transition to virtual visits, or those demonstrating instability before the changes related to the pandemic were excluded from analysis. A total of 13 patients met inclusion criteria and were included in this study.
Continuous variables were compared using repeated measures analysis of variance and categorical variables using Fisher exact or chi-square tests. The study was deemed exempt by the institutional review board.
Results
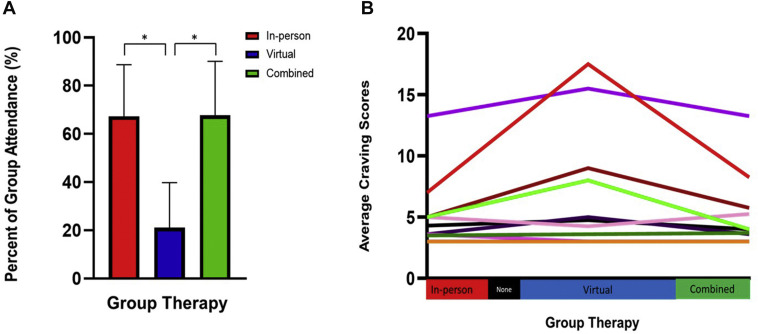
When compared with in-person sessions, attendance to group therapy sessions virtually was significantly lower by more than 3-fold (Figure A). Common reasons cited for not attending virtual sessions were unavailability of technology, technological malfunction or poor digital literacy, unreliable internet connection, or inability to access virtual sessions in a location meeting appropriate per the Health Insurance Portability and Accountability Act regulations for patient privacy (such as for patients residing in shelters or other multiresident living situations).
Figure.
Group attendance and total craving scores during each period
A, The bar graph represents the percent of group therapy sessions attended during each period. In the combined group, 75% of total attended group sessions were in-person sessions. ∗ denotes statistical significance, P<.05. B, Spaghetti plot, (n=13) each line represents 1 participant’s average total craving score during each period.
McKiever. Telehealth transition for OUD pregnancies during the COVID-19 pandemic. Am J Obstet Gynecol 2020.
Although there was no significant difference in the number of positive UDS results between periods, the data are notable for a relapse and overdose in 1 previously stable patient in addition to a significant increase in the total number of patients requiring uptitration in MAT dosage because of intensified cravings during the period of virtual-only sessions. Furthermore, there was a notable trend toward higher ED and/or obstetrical triage visits, reported assaults, and craving scores (Table ). Craving scores peaked for 6 (46%) patients during the virtual-only period (Figure B). Furthermore, 2 (15%) women reported IES-R scores of >34, which is concerning for COVID-19–specific distress.
Table.
Outcomes for women with opioid use disorder
|
Number of participants (n=13) |
In-person (before virtual-only meetings) | Virtual-only | Combined (after virtual-only meetings) | P value |
|---|---|---|---|---|
| Period | Feb. 19–March 11 | April 1–May 26 | May 27–June 25 | |
| Number of group therapy sessions offered over defined period | 4 | 8 | 5 | |
| Percentage of group therapy sessions attended | 67±21.4 | 21±18.7 | 68±22.4 | <.001a |
| Positive UDS tests for illicit substances | 9 (21) | 8 (13) | 2 (5) | .12 |
| ED or triage visitsb | 1 (8) | 4 (30) | 1 (8) | .17 |
| Reported assaultsb | 0 (0) | 2 (15) | 0 (0) | .08 |
| Overdosesb | 0 (0) | 1 (8) | 0 (0) | .39 |
| Uptitration of MAT dosage during defined periodb | 0 (0) | 5 (38) | 1 (8) | .02a |
| Average number of craving questionnaires completed per participant | 2.8±0.8 | 3.2±1.2 | 3.4±0.9 | .47 |
| Total craving scores | 3.6 [3–5] | 4.3 [3–8.5] | 3.7 [3–5.5] | .15 |
Data are presented as number (percentage), mean±standard deviation, or median [interquartile range], as applicable.
ED, emergency department, MAT, medication-assisted therapy; UDS, urine drug screen.
McKiever. Telehealth transition for OUD pregnancies during the COVID-19 pandemic. Am J Obstet Gynecol 2020.
Statistically significant (P<.05)
The number of ED or triage visits, reported assaults, and uptitration of MAT dosage visits were only counted once per participant in each specific period.
Conclusion
To protect patients and staff and minimize exposure to COVID-19, care models shifted toward fewer in-person visits during the peak of the pandemic. Although this model has public health benefits, transitioning to primarily telehealth healthcare administration also has unintended consequences, and some patient subgroups may be at risk of harm. One example of an at-risk group is pregnant women with OUD. These patients frequently have social vulnerabilities, significant barriers to care,3 history of trauma, and psychiatric illnesses that are exacerbated in times of uncertainty such as during the COVID-19 pandemic. Compounding the general atmosphere of uncertainty and anxiety because of the pandemic, the shift toward telehealth removed the consistency of care and support provided during in-person group visits. Although changes associated with the pandemic, including social distancing measures, closure of conveniences, and food and work insecurity largely affected the population as a whole, these changes compounded an already vulnerable population working to overcome addiction. Patients within this population are often limited in their social support groups, are frequently isolated from family, and have limited abilities to set up contingencies for childcare and work-related changes. Our study suggests that the switch from in-person to virtual-only group visits compounded change within this population and led to decreased attendance of therapy sessions and uptitration of MAT secondary to cravings. The small sample size is a limitation of this study; however, it is strengthened by its longitudinal design. As we continue to navigate care through the continually evolving pandemic and as healthcare moves into a paradigm where telehealth has a more permanent place, we need to consider the impact of that transition on our most vulnerable populations.
Footnotes
The authors report no conflict of interest.
References
- 1.Uscher-Pines L., Huskamp H.A., Mehrotra A. Treating patients with opioid use disorder in their homes: an emerging treatment model. JAMA. 2020 doi: 10.1001/jama.2020.3940. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aziz A., Zork N., Aubey J.J. Telehealth for high-risk pregnancies in the setting of the COVID-19 pandemic. Am J Perinatol. 2020;37:800–808. doi: 10.1055/s-0040-1712121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dunlop A., Lokuge B., Masters D. Challenges in maintaining treatment services for people who use drugs during the COVID-19 pandemic. Harm Reduct J. 2020;17:26. doi: 10.1186/s12954-020-00370-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peahl A.F., Smith R.D., Moniz M.H. Prenatal care redesign: creating flexible maternity care models through virtual care. Am J Obstet Gynecol. 2020 doi: 10.1016/j.ajog.2020.05.029. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]